Effects of COVID-19 Financial and Social Hardships on Infants’ and Toddlers’ Development in the ECHO Program
Abstract
1. Introduction
2. Materials and Methods
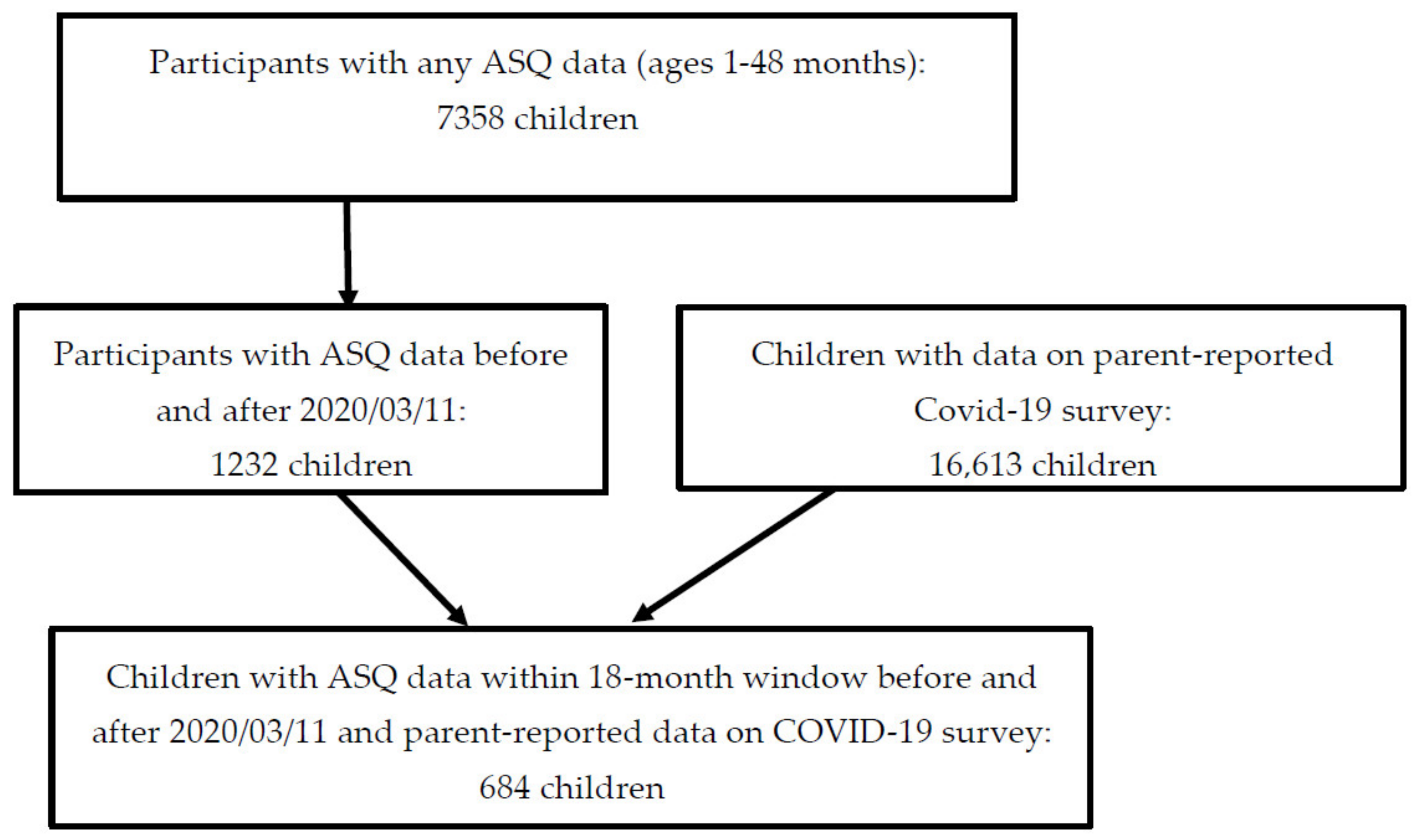
2.1. Study Population
2.2. Measures
2.3. Statistical Analyses
3. Results
3.1. Preliminary Results
3.2. Pandemic-Related Hardships by Pre-Pandemic Characteristics
3.3. Associations between Pandemic-Related Hardships and Change in ASQ Z-Scores
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moreland, A.; Herlihy, C.; Tynan, M.A.; Sunshine, G.; McCord, R.F.; Hilton, C.; Poovey, J.; Werner, A.K.; Jones, C.D.; Fulmer, E.B.; et al. Timing of State and Territorial COVID-19 Stay-at-Home Orders and Changes in Population Movement—United States, March 1–May 31, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1198–1203. [Google Scholar] [CrossRef] [PubMed]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef] [PubMed]
- Connell, C.M.; Strambler, M.J. Experiences with COVID-19 stressors and parents’ use of neglectful, harsh, and positive parenting practices in the northeastern United States. Child. Maltreat. 2021, 26, 255–266. [Google Scholar] [CrossRef]
- Perez, A.; Gobel, A.; Stuhrmann, L.Y.; Schepanski, S.; Singer, D.; Bindt, C.; Mudra, S. Born under COVID-19 Pandemic Conditions: Infant Regulatory Problems and Maternal Mental Health at 7 Months Postpartum. Front. Psychol. 2021, 12, 805543. [Google Scholar] [CrossRef]
- Werchan, D.M.; Hendrix, C.; Hume, A.; Zhang, M.; Thomason, M.O.; Brito, N.H. Cognitive and socioemotional development in infants exposed to SARS-CoV-2 in utero: A moderating role of prenatal psychosocial stress on infant outcomes. PsyArXiv 2022. [Google Scholar] [CrossRef]
- Karunathilake, K. Positive and negative impacts of COVID-19, an analysis with special reference to challenges on the supply chain in South Asian countries. J. Soc. Econ. Dev. 2021, 23, 568–581. [Google Scholar] [CrossRef]
- Gupta, S.; Jawanda, M.K. The impacts of COVID-19 on children. Acta Paediatr. 2020, 109, 2181–2183. [Google Scholar] [CrossRef]
- Brooks-Gunn, J.; Han, W.J.; Waldfogel, J. Maternal employment and child cognitive outcomes in the first three years of life: The NICHD Study of Early Child Care. National Institute of Child Health and Human Development. Child. Dev. 2002, 73, 1052–1072. [Google Scholar] [CrossRef]
- Deoni, S.C.; Beauchemin, J.; Volpe, A.; Da Sa, V.; Consortium, R. Impact of the COVID-19 Pandemic on Early Child Cognitive Development: Initial Findings in a Longitudinal Observational Study of Child Health. medRxiv 2021. [Google Scholar] [CrossRef]
- Shuffrey, L.C.; Firestein, M.R.; Kyle, M.H.; Fields, A.; Alcantara, C.; Amso, D.; Austin, J.; Bain, J.M.; Barbosa, J.; Bence, M.; et al. Association of Birth during the COVID-19 Pandemic with Neurodevelopmental Status at 6 Months in Infants with and without In Utero Exposure to Maternal SARS-CoV-2 Infection. JAMA Pediatr. 2022, 176, e215563. [Google Scholar] [CrossRef]
- Squires, J.; Bricker, D.; Potter, L. Revision of a parent-completed development screening tool: Ages and Stages Questionnaires. J. Pediatr. Psychol. 1997, 22, 313–328. [Google Scholar] [CrossRef] [PubMed]
- Blaisdell, C.J.; Park, C.; Hanspal, M.; Roary, M.; Arteaga, S.S.; Laessig, S.; Luetkemeier, E.; Gillman, M.W.; Program Collaborators for Environmental influences on Child Health Outcomes. The NIH ECHO Program: Investigating how early environmental influences affect child health. Pediatr. Res. 2021, 92, 1215–1216. [Google Scholar] [CrossRef] [PubMed]
- Goldfeld, S.; O’Connor, E.; Sung, V.; Roberts, G.; Wake, M.; West, S.; Hiscock, H. Potential indirect impacts of the COVID-19 pandemic on children: A narrative review using a community child health lens. Med. J. Aust. 2022, 216, 364–372. [Google Scholar] [CrossRef] [PubMed]
- PhenX Toolkit ECHO COVID-19 Questionnaires PhenX Toolkit: 2020. Available online: https://www.phenxtoolkit.org/covid19 (accessed on 12 July 2022).
- Blackwell, C.K.; Mansolf, M.; Sherlock, P.; Ganiban, J.; Hofheimer, J.A.; Barone, C.J.; Bekelman, T.A.; Blair, C.; Cella, D.; Collazo, S.; et al. Youth Well-being during the COVID-19 Pandemic. Pediatrics 2022, 149, e2021054754. [Google Scholar] [CrossRef] [PubMed]
- Enlow, P.T.; Phan, T.T.; Lewis, A.M.; Hildenbrand, A.K.; Sood, E.; Canter, K.S.; Vega, G.; Alderfer, M.A.; Kazak, A.E. Validation of the COVID-19 Exposure and Family Impact Scales. J. Pediatr. Psychol. 2022, 47, 259–269. [Google Scholar] [CrossRef]
- Chen, D.; Yang, H.; Cao, Y.; Cheng, W.; Duan, T.; Fan, C.; Fan, S.; Feng, L.; Gao, Y.; He, F.; et al. Expert consensus for managing pregnant women and neonates born to mothers with suspected or confirmed novel coronavirus (COVID-19) infection. Int. J. Gynaecol. Obstet. 2020, 149, 130–136. [Google Scholar] [CrossRef]
- Farewell, C.V.; Jewell, J.; Walls, J.; Leiferman, J.A. A Mixed-Methods Pilot Study of Perinatal Risk and Resilience during COVID-19. J. Prim. Care Community Health 2020, 11, 1–8. [Google Scholar] [CrossRef]
- Zamarro, G.; Prados, M.J. Gender differences in couples’ division of childcare, work and mental health during COVID-19. Rev. Econ. Househ. 2021, 19, 11–40. [Google Scholar] [CrossRef]
- Basurto-Davila, R.; Garza, R.; Meltzer, M.I.; Carlino, O.L.; Albalak, R.; Orellano, P.W.; Uez, O.; Shay, D.K.; Santandrea, C.; del Carmen Weis, M.; et al. Household economic impact and attitudes toward school closures in two cities in Argentina during the 2009 influenza A (H1N1) pandemic. Influenza Other Respir. Viruses 2013, 7, 1308–1315. [Google Scholar] [CrossRef]
- Bayham, J.; Fenichel, E.P. Impact of school closures for COVID-19 on the US health-care workforce and net mortality: A modelling study. Lancet Public Health 2020, 5, e271–e278. [Google Scholar] [CrossRef]
- Cauchemez, S.; Van Kerkhove, M.D.; Archer, B.N.; Cetron, M.; Cowling, B.J.; Grove, P.; Hunt, D.; Kojouharova, M.; Kon, P.; Ungchusak, K.; et al. School closures during the 2009 influenza pandemic: National and local experiences. BMC Infect. Dis. 2014, 14, 207. [Google Scholar] [CrossRef] [PubMed]
- Chin, E.T.; Huynh, B.Q.; Lo, N.C.; Hastie, T.; Basu, S. Projected geographic disparities in healthcare worker absenteeism from COVID-19 school closures and the economic feasibility of child care subsidies: A simulation study. MedRxiv 2020. [Google Scholar] [CrossRef]
- Kavanagh, A.M.; Mason, K.E.; Bentley, R.J.; Studdert, D.M.; McVernon, J.; Fielding, J.E.; Petrony, S.; Gurrin, L.; LaMontagne, A.D. Leave entitlements, time off work and the household financial impacts of quarantine compliance during an H1N1 outbreak. BMC Infect. Dis. 2012, 12, 311. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Lee, S.; Han, H.; Jung, J.; Yang, S.J.; Shin, Y. Parental Mental Health and Children’s Behaviors and Media Usage during COVID-19-Related School Closures. J. Korean Med. Sci. 2021, 36, e184. [Google Scholar] [CrossRef] [PubMed]
- Kuhfeld, M.; Soland, J.; Lewis, K. Test Score Patterns across Three COVID-19-Impacted School Years; Annenberg Institute at Brown University: Providence, RI, USA, 2022. [Google Scholar]
- Domingue, B.W.; Hough, H.J.; Lang, D.; Eatman, J. Changing Patterns of Growth in Oral Reading Fluency during the COVID-19 Pandemic; Policy Analysis for California Education (PACE): Stanford, CA, USA, 2021. [Google Scholar]
- Pier, L.; Christian, M.; Tymeson, H.; Meyer, R.H. COVID-19 Impacts on Student Learning; Policy Analysis for California Education (PACE): Stanford, CA, USA, 2021; p. 49. [Google Scholar]
| Influence of Job Loss/Change | Less Contact with Household Members | Less Contact with Family/Friends Outside the Home | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | No | Yes | p | No | Yes | p | No | Yes | p | |
| N | 684 | 247 | 279 | 580 | 96 | 76 | 600 | |||
| Maternal Characteristics | ||||||||||
| Maternal race (%) | <0.001 | <0.001 | 0.016 | |||||||
| White | 348 (50.9) | 150 (54.7) | 124 (45.3) | 314 (90.8) | 32 (9.2) | 30 (8.7) | 316 (91.3) | |||
| Black | 27 (3.9) | 7 (28) | 18 (72) | <28 | <5 | 5 (18.5) | 22 (81.5) | |||
| Asian | 84 (12.3) | 35 (57.4) | 26 (42.6) | 67 (81.7) | 15 (18.3) | 8 (9.8) | 74 (90.2) | |||
| Native Hawaiian or Pacific Islander | 7 (1) | <5 | <7 | 7 (100) | 0 (0.0) | 0 (0.0) | 7 (100) | |||
| American Indian/Alaska Native | 57 (8.3) | 26 (53.1) | 23 (46.9) | 33 (60) | 22 (40) | 12 (21.8) | 43 (78.2) | |||
| Multiple race | 33 (4.8) | 15 (60) | 10 (40) | 27 (81.8) | 6 (18.2) | 7 (21.2) | 26 (78.8) | |||
| Other race | 111(16.2) | 9 (12.5) | 63 (87.5) | 97 (89) | 12 (11) | 9 (8.3) | 100 (91.7) | |||
| Missing | 17 (2.5) | <5 | <13 | |||||||
| Maternal ethnicity (%) | <0.001 | 0.392 | 1 | |||||||
| Hispanic or Latino | 214 (31.3) | 33(22.1) | 116 (77.9) | 186 (87.7) | 26 (12.3) | 24 (11.3) | 188 (88.7) | |||
| Not Hispanic or Latino | 470 (68.7) | 214 (56.8) | 163 (43.2) | 394 (84.9) | 70 (15.1) | 52 (11.2) | 412 (88.8) | |||
| Maternal education (%) | <0.001 | 0.001 | 0.009 | |||||||
| Less than high school | 40 (5.8) | <5 | <20 | <36 | <5 | 5 | 34 | |||
| High school degree | 82 (12) | 9 (15) | 51 (85) | 71 (86.6) | 11 (13.4) | 14 (17.1) | 68 (82.9) | |||
| Some college | 126 (18.4) | 37 (36.3) | 65 (63.7) | 94 (75.2) | 31 (24.8) | 23 (18.4) | 102 (81.6) | |||
| Bachelor’s (BA,BS) | 187 (27.3) | 88 (61.5) | 55 (38.5) | 158 (84.9) | 28 (15.1) | 17 (9.1) | 169 (90.9) | |||
| Graduate degree | 237 (34.6) | 107 (56) | 84 (44) | 214 (91.5) | 20 (8.5) | 17 (7.3) | 217 (92.7) | |||
| Missing | 12 (1.8) | <5 | <7 | <10 | <5 | |||||
| Maternal employment | 0.708 | 0.114 | 0.011 | |||||||
| Employed | 484 (70.8) | 186 (50) | 186 (50) | 426 (89.1) | 52 (10.9) | 45 (9.4) | 433 (90.6) | |||
| Not employed | 26 (3.8) | 11 (44) | 14 (56) | 20 (76.9) | 6 (23.1) | 7 (26.9) | 19 (73.1) | |||
| Missing | 174 (25.4) | |||||||||
| Household income (%) | <0.001 | 0.593 | <0.001 | |||||||
| <$30,000 | 92 (13.5) | 8 (11.6) | 61 (88.4) | 78 (85.7) | 13 (14.3) | 15 (16.5) | 76 (83.5) | |||
| $30,000–49,999 | 45 (6.6) | 9 (29) | 22 (71) | <44 | <5 | 6 (13.3) | 39 (86.7) | |||
| $50,000–74,999 | 52 (7.6) | 22 (45.8) | 26 (54.2) | 44 (84.6) | 8 (15.4) | 12 (23.1) | 40 (76.9) | |||
| $75,000–99,999 | 48 (7) | 18 (47.4) | 20 (52.6) | 38 (82.6) | 8 (17.4) | 7 (15.2) | 39 (84.8) | |||
| $100,000 or more | 326 (47.7) | 156 (61.2) | 99 (38.8) | 288 (88.9) | 36 (11.1) | 18 (5.6) | 306 (94.4) | |||
| Missing | 121 (17.7) | |||||||||
| Marital status | 0.222 | 0.25 | 0.004 | |||||||
| Married/living with partner | 607 (88.7) | 226 (47.9) | 246 (52.1) | 519 (86.4) | 82 (13.6) | 61 (10.1) | 540 (89.9) | |||
| Not married | 66 (9.6) | 18 (37.5) | 30 (62.5) | 53 (80.3) | 13 (19.7) | 15 (22.7) | 51 (77.3) | |||
| Missing | 11 (1.6) | |||||||||
| Child Characteristics | ||||||||||
| Preterm | 1 | 1 | 1 | |||||||
| 37+ wks | 620 (90.6) | 223 (46.4) | 258 (53.6) | 528 (86) | 86 (14) | 66 (10.7) | 548 (89.3) | |||
| <37 wks | 53 (7.7) | 17 (47.2) | 19 (52.8) | 45 (86.5) | 7 (13.5) | 6 (11.5) | 46 (88.5) | |||
| Missing | 11 (1.6) | |||||||||
| Children sex (%) | 0.451 | 0.506 | 0.72 | |||||||
| Female | 324 47.4) | 110 (44.9) | 135 (55.1) | 278 (86.9) | 42 (13.1) | 38 (11.9) | 282 (88.1) | |||
| Male | 359 (52.5) | 136 (48.6) | 144 (51.4) | 301 (84.8) | 54 (15.2) | 38 (10.7) | 317 (89.3) | |||
| Children ethnicity (%) | <0.001 | 0.249 | 0.798 | |||||||
| Hispanic or Latino | 229 (33.5) | 42 (25.8) | 121 (74.2) | 199 (87.7) | 28 (12.3) | 25 (11) | 202 (89) | |||
| Not Hispanic or Latino | 430 (62.9) | 195 (56.9) | 148 (43.1) | 356 (84) | 68 (16) | 51 (12) | 373 (88) | |||
| Missing | 25 (3.7) | |||||||||
| Children race (%) | 0.5 | 0.4 | 0.8 | |||||||
| White | 349 (51) | 135 (50) | 135 (50) | 312 (89.9) | 35 (10.1) | 30 (8.6) | 317 (91.4) | |||
| Black | 23 (3.4) | <5 | <16 | <23 | <5 | <5 | <23 | |||
| Asian | 63 (9.2) | 28 (59.6) | 19 (40.4) | 49 (80.3) | 12 (19.7) | 8 (13.1) | 53 (86.9) | |||
| Native Hawaiian/Pacific Islander | 5 (0.7) | <5 | <5 | 8 (13.1) | 0 (0.0) | 0 (0.0) | 5 | |||
| American Indian | 59 (8.6) | 27 (54) | 23 (46) | 35 (61.4) | 22 (38.6) | 13 (22.8) | 44 (77.2) | |||
| Multiple race | 75 (11) | 33 (56.9) | 25 (43.1) | 64 (85.3) | 11 (14.7) | 9 (12) | 66 (88) | |||
| Other race | 0 (0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| Missing | 110 (16.1) | |||||||||
| Gestational age/birth weight (ga/bw) | ||||||||||
| Birth_ ga (mean (SD)) | 38.77 (1.59) | 38.63 (2.78) | 0.489 | 38.61 (2.27) | 38.82 (1.47) | 0.398 | 38.58 (1.96) | 38.65 (2.20) | 0.815 | |
| Birth_ bw (mean (SD)) | 3371.52 (509.87) | 3332.98 (520.79) | 0.405 | 3306.40 (518.48) | 3379.07 (509.01) | 0.221 | 3320.47 (619.27) | 3315.80 (504.49) | 0.944 | |
| Children Pre-pandemic Life Stage (%) | 684 (100) | 1 | 0.086 | 0.6 | ||||||
| Early childhood | 356 (52) | 129 (46.9) | 146 (53.1) | 292 (83.4) | 58 (16.6) | 42 (12) | 308 (88) | |||
| Infancy | 328 (48) | 118 (47) | 133 (53.0) | 288 (88.3) | 38 (11.7) | 34 (10.4) | 292 (89.6) | |||
| Ages and Stages Questionnaire (ASQ) | ||||||||||
| Communication (%) | 0.075 | 0.243 | 0.679 | |||||||
| On-track | 197 (45.2) | 239 (54.8) | 476 (85.2) | 83 (14.8) | 63 (11.3) | 496 (88.7) | ||||
| Needs monitoring | 33 (50.8) | 32 (49.2) | <80 | <11 | <9 | 78 (100) | ||||
| At-risk for delay | 14 (70) | 6 (30) | <23 | <5 | <5 | 22 (100) | ||||
| Gross motor (%) | 0.819 | 0.896 | 0.988 | |||||||
| On-track | 202 (47) | 228 (53) | 478 (86.1) | 77 (13.9) | 62 (11.2) | 493 (88.8) | ||||
| Needs monitoring | 27 (45) | 33 (55) | 67 (87) | 10 (13) | <10 | 68 | ||||
| At-risk for delay | 12 (41.4) | 17 (58.6) | 31 (83.8) | 6 (16.2) | <5 | 33 | ||||
| Fine motor (%) | 0.186 | 0.347 | 0.059 | |||||||
| On-track | 167 (47.7) | 183 (52.3) | 368 (84.6) | 67 (15.4) | 46 (10.6) | 389 (89.4) | ||||
| Needs monitoring | 20 (37.7) | 33 (62.3) | 61 (88.4) | 8 (11.6) | 11 (15.9) | 58 (84.1) | ||||
| At-risk for delay | 19 (57.6) | 14 (42.4) | 32 (78) | 9 (22) | 9 (22) | 32 (78) | ||||
| Problem solving (%) | 0.744 | 0.846 | 0.965 | |||||||
| On-track | 162 (46.3) | 188 (53.7) | 372 (84.4) | 69 (15.6) | 54 (12.2) | 387 (87.8) | ||||
| Needs monitoring | 30 (51.7) | 28 (48.3) | 55 (85.9) | 9 (14.1) | 8 (12.5) | 56 (87.5) | ||||
| At-risk for delay | 15 (46.9) | 17 (53.1) | 36 (81.8) | 8 (18.2) | 6 (13.6) | 38 (86.4) | ||||
| Personal social (%) | 0.063 | 0.213 | 0.126 | |||||||
| On-track | 164 (46.7) | 187 (53.3) | 376 (85.1) | 66 (14.9) | 48 (10.9) | 394 (89.1) | ||||
| Needs monitoring | 34 (56.7) | 26 (43.3) | 55 (77.5) | 16 (22.5) | 13 (18.3) | 58 (81.7) | ||||
| At-risk for delay | 8 (29.6) | 19 (70.4) | 27 (79.4) | 7 (20.6) | 6 (17.6) | 28 (82.4) | ||||
| Communication | Personal-Social | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposure Variables | Parents’ Job Loss/Change | Less Contact with Household Members | Less Contact with Family/Friends Outside Home | Parents’ Job Loss/Change | Less Contact with Household Members | Less Contact with Family/Friends Outside Home | ||||||
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Parents’ job loss/change | 0.66 (0.37,1) | 0.14 | 1.15 (0.63,2) | 0.66 | ||||||||
| less contact with household members | 0.92 (0.49,2) | 0.80 | 0.67 (0.34,1) | 0.26 | ||||||||
| Less contact with family/friends outside home | 2.03 (0.91,5) | 0.08 | 1.23 (0.58,3) | 0.59 | ||||||||
| Pre-pandemic ASQ | 0.72 (0.54,1) | 0.02 | 0.98 (0.81,1) | 0.82 | 0.97 (0.81,1) | 0.76 | 0.87 (0.64,1) | 0.39 | 1.12 (0.92,1) | 0.24 | 1.13 (0.93,1) | 0.21 |
| Maternal/family characteristics | ||||||||||||
| American Indian or Alaskan Native | 0.56 (0.17,2) | 0.33 | 0.55 (0.21,1) | 0.22 | 0.56 (0.22,1) | 0.23 | 1.49 (0.52,4) | 0.46 | 1.22 (0.48,3) | 0.68 | 1.08 (0.43,3) | 0.87 |
| Asian | 0.6 (0.23,2) | 0.29 | 0.84 (0.43,2) | 0.62 | 0.83 (0.41,2) | 0.58 | 1.41 (0.6,3) | 0.44 | 1.55 (0.76,3) | 0.23 | 1.48 (0.72,3) | 0.29 |
| Black | 0.88 (0.19,4) | 0.87 | 0.97 (0.29,3) | 0.96 | 0.95 (0.27,3) | 0.94 | 1.43 (0.37,5) | 0.60 | 1.21 (0.35,4) | 0.76 | 1.21 (0.35,4) | 0.76 |
| Multiple Race | 0.97 (0.31,3) | 0.96 | 1.28 (0.51,3) | 0.59 | 1.34 (0.53,3) | 0.53 | 1.32 (0.37,5) | 0.67 | 1.48 (0.51,4) | 0.47 | 1.47 (0.51,4) | 0.48 |
| Native Hawaiian or other Pacific Islander | 1.3 (0.28,6) | 0.74 | 1.64 (0.38,7) | 0.51 | 1.53 (0.36,7) | 0.56 | 6.1 (0.62,60) | 0.12 | 1.84 (0.22,16) | 0.58 | 1.86 (0.22,16) | 0.57 |
| Other Race | 1.05 (0.39,3) | 0.92 | 1.02 (0.47,2) | 0.97 | 0.98 (0.46,2) | 0.97 | 0.94 (0.4,2) | 0.89 | 0.94 (0.48,2) | 0.84 | 0.93 (0.48,2) | 0.84 |
| Maternal ethnicity | 0.73 (0.31,2) | 0.46 | 0.85 (0.45,2) | 0.60 | 0.87 (0.46,2) | 0.67 | ||||||
| <$30,000 | 1.85 (0.52,7) | 0.34 | 1.97 (0.82,5) | 0.13 | 2.04 (0.85,5) | 0.11 | ||||||
| $30,000–49,999 | 0.98 (0.31,3) | 0.98 | 1.1 (0.43,3) | 0.84 | 1.13 (0.44,3) | 0.79 | ||||||
| $50,000–74,999 | 2.16 (0.9,5) | 0.09 | 1.8 (0.82,4) | 0.14 | 1.97 (0.89,4) | 0.09 | ||||||
| $75,000–99,999 | 1.08 (0.38,3) | 0.88 | 0.95 (0.39,2) | 0.90 | 0.98 (0.41,2) | 0.97 | ||||||
| Less than high school | 2.61 (0.73,9) | 0.14 | 1.9 (0.72,5) | 0.20 | 2.05 (0.77,5) | 0.15 | ||||||
| High school degree, GED or equivalent | 2.89 (0.92,9) | 0.07 | 1.81 (0.74,4) | 0.19 | 1.92 (0.77,5) | 0.16 | ||||||
| Some college, no degree, or AA | 1.18 (0.46,3) | 0.73 | 1.07 (0.5,2) | 0.87 | 1.12 (0.51,2) | 0.78 | ||||||
| Master’s degree, professional or doctorate degree | 0.79 (0.41,2) | 0.48 | 0.72 (0.41,1) | 0.26 | 0.73 (0.41,1) | 0.28 | ||||||
| Child characteristics | ||||||||||||
| Children sex | 3.03 (1.75,5) | 0.00 | 2.55 (1.65,4) | 0.00 | 2.54 (1.64,4) | 0.00 | 2.23 (1.22,4) | 0.01 | 2.25 (1.35,4) | 0.00 | 2.24 (1.34,4) | 0.00 |
| Gestational age | 0.97 (0.84,1) | 0.65 | 1.05 (0.87,1) | 0.59 | 1.05 (0.87,1) | 0.63 | ||||||
| Preterm status | 6.18 (0.68,56) | 0.10 | 1.67 (0.45,6) | 0.44 | 1.61 (0.45,6) | 0.46 | ||||||
| Children pre-pandemic life stage | −0.69 (−0.38,−1) | .22 | −0.72 (−0.43,−1) | 0.22 | −0.71 (−0.43,−1) | .20 | ||||||
| Communication | Personal-Social | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Parents’ Job Loss/Change | Less Contact with Household Members | Less Contact with Family/Friends Outside Home | Parents’ Job Loss/Change | Less Contact with Household Members | Less Contact with Household Members | ||||||
| Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | Estimate (95% CI) | p Value | |
| Parents’ job loss/change | 0.12 (−0.04,0.27) | 0.15 | −0.02 (–0.2,0.17) | 0.85 | ||||||||
| Less contact with household members | 0.1 (−0.11,0.31) | 0.36 | 0.15 (−0.06,0.36) | 0.17 | ||||||||
| Less contact with family/friends outside home | −0.14 (−0.37,0.09) | 0.22 | −0.18 (−0.43,0.08) | 0.17 | ||||||||
| Baseline ASQ | −0.65 (−0.75,−0.54) | 0.00 | −0.63 (−0.72,−0.54) | 0.00 | −0.63 (−0.72,−0.54) | 0.00 | −0.56 (−0.67,−0.46) | 0.00 | −0.56 (−0.67,−0.46) | 0.00 | −0.57 (−0.67,−0.46) | 0.00 |
| Maternal/family characteristics | ||||||||||||
| American Indian or Alaska Native | 0.25 (−0.17,0.67) | 0.24 | 0.22 (−0.15,0.59) | 0.25 | 0.24 (−0.12,0.59) | 0.19 | −0.07 (−0.48,0.35) | 0.75 | 0.01 (−0.39,0.4) | 0.96 | 0.05 (−0.33,0.43) | 0.79 |
| Asian | 0.06 (−0.16,0.28) | 0.57 | −0.02 (−0.22,0.19) | 0.87 | −0.01 (−0.22,0.2) | 0.93 | 0.02 (−0.27,0.31) | 0.89 | −0.06 (−0.33,0.21) | 0.68 | −0.04 (−0.31,0.23) | 0.77 |
| Black | −0.01 (−0.46,0.45) | 0.98 | −0.01 (−0.43,0.41) | 0.98 | −0.01 (−0.43,0.42) | 0.98 | −0.26 (−0.8,0.28) | 0.35 | −0.15 (−0.69,0.4) | 0.60 | −0.14 (−0.69,0.42) | 0.63 |
| Multiple race | −0.07 (−0.46,0.31) | 0.70 | 0 (−0.32,0.32) | 0.99 | −0.01 (−0.33,0.31) | 0.96 | −0.23 (−0.65,0.19) | 0.29 | −0.12 (−0.48,0.23) | 0.50 | −0.13 (−0.49,0.23) | 0.48 |
| Native Hawaiian or other Pacific Islander | −0.51 (−0.25,0.22) | 0.17 | −0.46 (−0.14,0.22) | 0.18 | −0.44 (−0.12,0.23) | 0.20 | −0.85 (−1.78,0.09) | 0.07 | −0.76 (−1.71,0.19) | 0.11 | −0.73 (−1.68,0.22) | 0.13 |
| Other Race | −0.07 (−0.47,0.34) | 0.75 | −0.06 (−0.4,0.27) | 0.70 | −0.05 (−0.38,0.28) | 0.77 | −0.17 (−0.56,0.23) | 0.40 | −0.09 (−0.44,0.26) | 0.60 | −0.08 (−0.43,0.27) | 0.67 |
| Maternal ethnicity | 0.02 (−0.25,0.28) | 0.89 | 0.1 (−0.13,0.33) | 0.38 | 0.1 (−0.12,0.33) | 0.37 | ||||||
| Marital status | 0.18 (−0.15,0.51) | 0.29 | 0.06 (−0.23,0.34) | 0.69 | 0.05 (−0.23,0.34) | 0.71 | ||||||
| Less than high school | −0.56 (−1.14,0.02) | 0.06 | −0.34 (−0.78,0.09) | 0.12 | −0.36 (−0.79,0.08) | 0.11 | −0.03 (−0.57,0.51) | 0.91 | 0.07 (−0.38,0.51) | 0.77 | 0.05 (−0.4,0.49) | 0.83 |
| High school degree, GED or equivalent | −0.53 (−0.96,−0.1) | 0.02 | −0.43 (−0.8,−0.06) | 0.02 | −0.45 (−0.82,−0.08) | 0.02 | 0.06 (−0.38,0.49) | 0.80 | 0.14 (−0.29,0.57) | 0.53 | 0.11 (−0.32,0.53) | 0.62 |
| Some college/no degree/AA | −0.21 (−0.51,0.08) | 0.16 | −0.15 (−0.41,0.1) | 0.23 | −0.16 (−0.41,0.1) | 0.22 | 0.21 (−0.1,0.52) | 0.18 | 0.18 (−0.1,0.46) | 0.20 | 0.18 (−0.1,0.46) | 0.22 |
| Mater’s, Professional or Doctorate Degree | 0.03 (−0.15,0.2) | 0.75 | 0.05 (−0.11,0.21) | 0.52 | 0.05 (−0.11,0.21) | 0.56 | 0.11 (−0.11,0.33) | 0.32 | 0.09 (−0.11,0.29) | 0.38 | 0.08 (−0.12,0.28) | 0.42 |
| <$30,000 | −0.18 (−0.62,0.26) | 0.42 | −0.2 (−0.56,0.17) | 0.29 | −0.2 (−0.56,0.16) | 0.27 | −0.15 (−0.56,0.26) | 0.46 | −0.17 (−0.55,0.2) | 0.36 | −0.18 (−0.55,0.19) | 0.34 |
| $30,000–49,999 | −0.1 (−0.43,0.24) | 0.57 | 0.02 (−0.3,0.34) | 0.88 | 0.01 (−0.31,0.33) | 0.94 | −0.21 (−0.57,0.15) | 0.24 | −0.05 (−0.44,0.35) | 0.81 | −0.06 (−0.45,0.33) | 0.75 |
| $50,000–74,999 | −0.25 (−0.59,0.09) | 0.15 | −0.25 (−0.57,0.07) | 0.12 | −0.27 (−0.6,0.05) | 0.10 | −0.12 (−0.5,0.26) | 0.53 | −0.1 (−0.49,0.28) | 0.60 | −0.12 (−0.5,0.27) | 0.55 |
| $75,000–99,999 | −0.01 (−0.28,0.26) | 0.97 | −0.04 (−0.31,0.22) | 0.74 | −0.05 (−0.31,0.21) | 0.69 | −0.06 (−0.42,0.3) | 0.75 | 0.03 (−0.31,0.37) | 0.85 | 0.02 (−0.32,0.36) | 0.90 |
| Child Characteristics | ||||||||||||
| Children sex | −0.34 (−0.5,−0.18) | 0.00 | −0.36 (−0.5,−0.21) | 0.00 | −0.36 (−0.5,−0.21) | 0.00 | ||||||
| Birth weight | 0 (0,0) | 0.69 | 0 (0,0) | 0.79 | 0 (0,0) | 0.83 | 0 (0,0) | 0.30 | 0 (0,0) | 0.66 | 0 (0,0) | 0.62 |
| Children pre-pandemic life stage | −0.23 (−0.07,−0.39) | 0.00 | −0.23 (−0.09,−0.38) | 0.00 | −0.23 (−0.09,−0.38) | 0.00 | −0.23 (−0.06,−0.41) | 0.01 | −0.14 (−0.03,−0.31) | 0.11 | −0.14 (−0.03,−0.31) | 0.10 |
| Preterm status | −0.48 (−0.81,−0.15) | 0.00 | −0.25 (−0.55,0.05) | 0.10 | −0.24 (−0.54,0.06) | 0.11 | ||||||
| Gestational age | −0.01 (−0.04,0.02) | 0.52 | −0.02 (−0.06,0.02) | 0.27 | −0.02 (−0.06,0.02) | 0.28 | ||||||
| Children’s ethnicity | −0.16 (−0.41,0.09) | 0.20 | 0.03 (−0.2,0.27) | 0.79 | 0.03 (−0.21,0.26) | 0.82 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nozadi, S.S.; Li, X.; Kong, X.; Rennie, B.; Kanda, D.; MacKenzie, D.; Luo, L.; Posner, J.; Blackwell, C.K.; Croen, L.A.; et al. Effects of COVID-19 Financial and Social Hardships on Infants’ and Toddlers’ Development in the ECHO Program. Int. J. Environ. Res. Public Health 2023, 20, 1013. https://doi.org/10.3390/ijerph20021013
Nozadi SS, Li X, Kong X, Rennie B, Kanda D, MacKenzie D, Luo L, Posner J, Blackwell CK, Croen LA, et al. Effects of COVID-19 Financial and Social Hardships on Infants’ and Toddlers’ Development in the ECHO Program. International Journal of Environmental Research and Public Health. 2023; 20(2):1013. https://doi.org/10.3390/ijerph20021013
Chicago/Turabian StyleNozadi, Sara S., Ximin Li, Xiangrong Kong, Brandon Rennie, Deborah Kanda, Debra MacKenzie, Li Luo, Jonathan Posner, Courtney K. Blackwell, Lisa A. Croen, and et al. 2023. "Effects of COVID-19 Financial and Social Hardships on Infants’ and Toddlers’ Development in the ECHO Program" International Journal of Environmental Research and Public Health 20, no. 2: 1013. https://doi.org/10.3390/ijerph20021013
APA StyleNozadi, S. S., Li, X., Kong, X., Rennie, B., Kanda, D., MacKenzie, D., Luo, L., Posner, J., Blackwell, C. K., Croen, L. A., Ferrara, A., O’Connor, T. G., Zimmerman, E., Ghassabian, A., Leve, L. D., Elliott, A. J., Schmidt, R. J., Sprowles, J. L. N., & Lewis, J. L. (2023). Effects of COVID-19 Financial and Social Hardships on Infants’ and Toddlers’ Development in the ECHO Program. International Journal of Environmental Research and Public Health, 20(2), 1013. https://doi.org/10.3390/ijerph20021013








