What Can One Minute of the Day Tell about Physical Activity?
Abstract
:1. Introduction
2. Materials and Methods
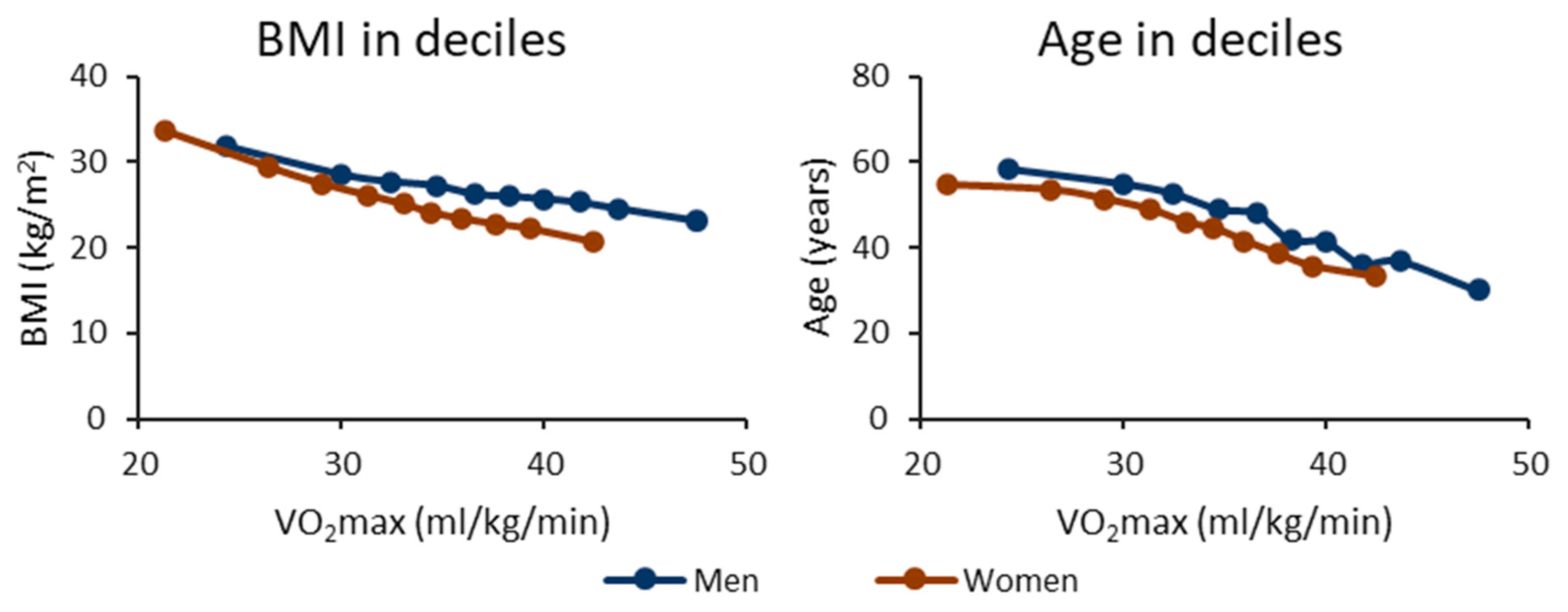
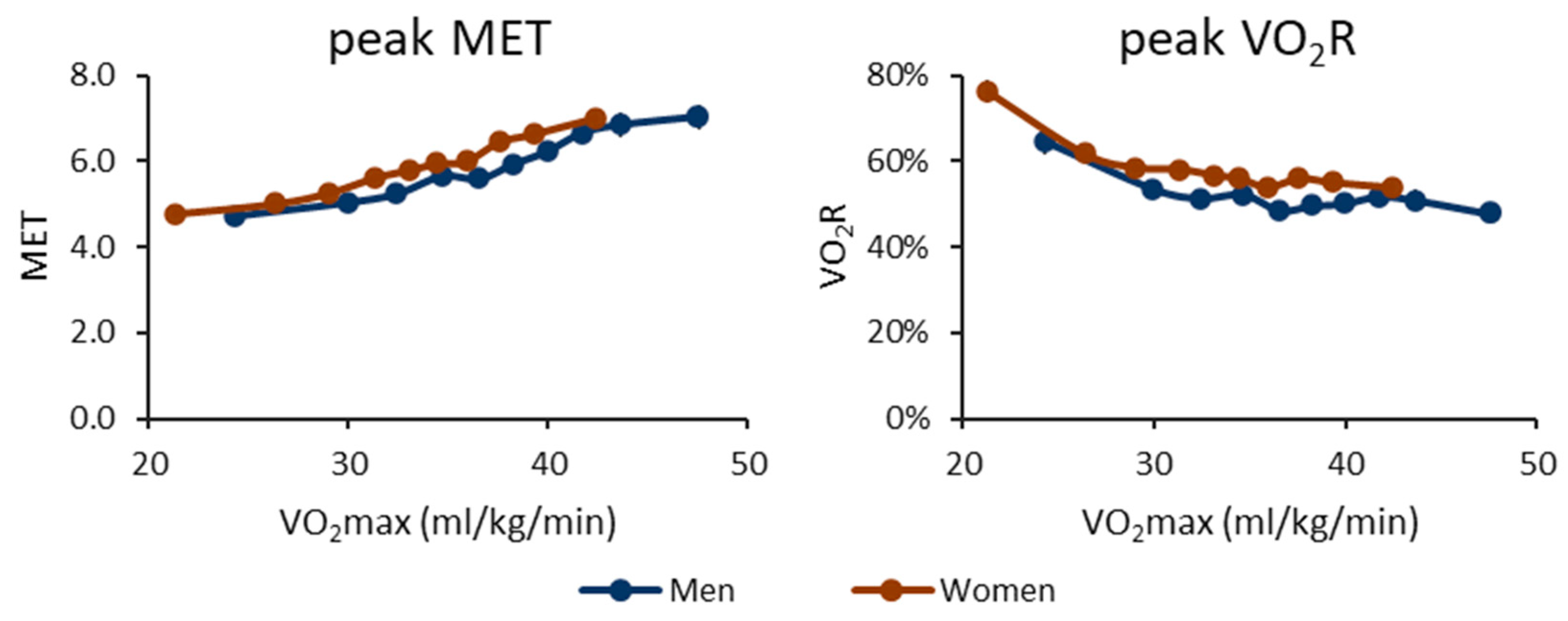
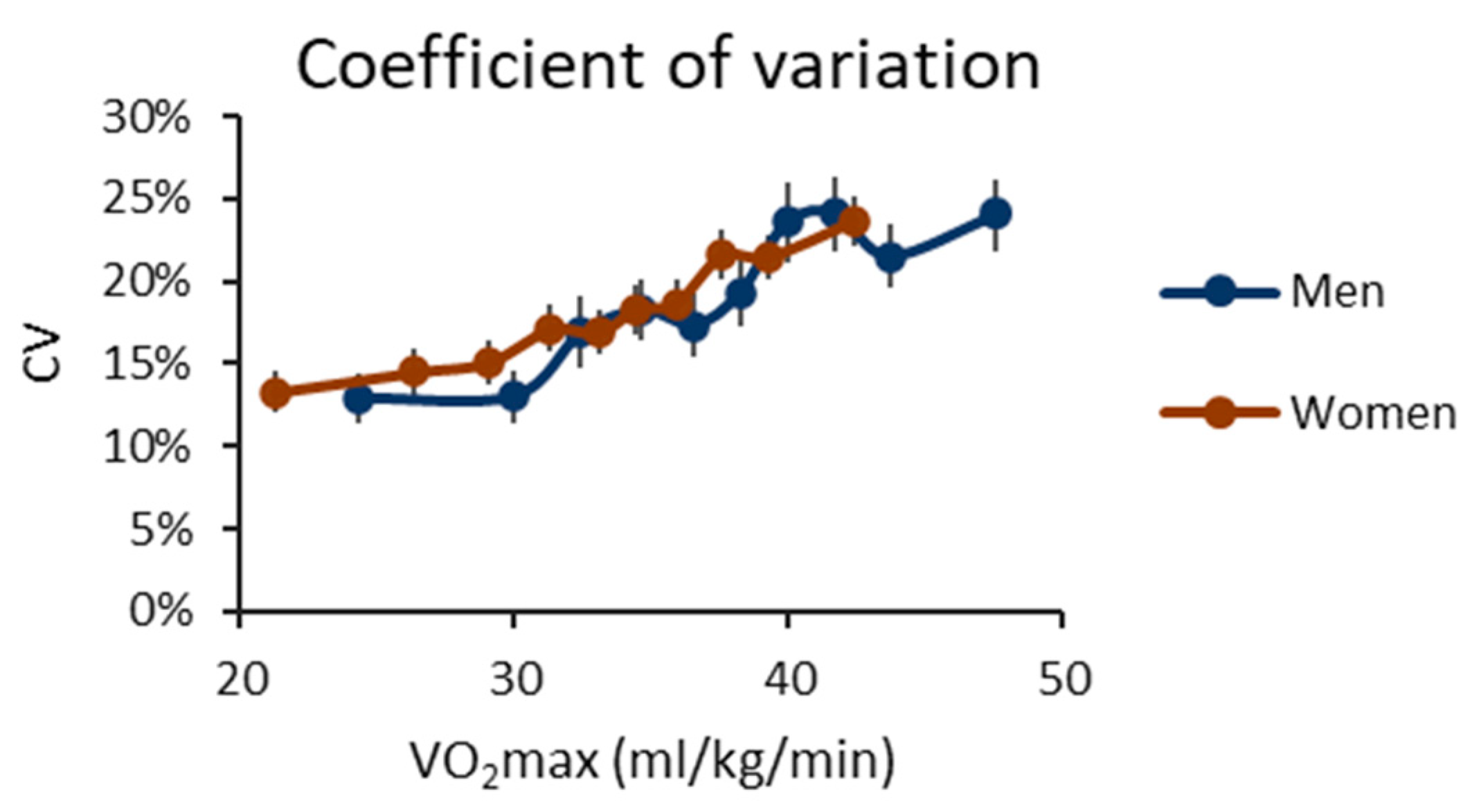
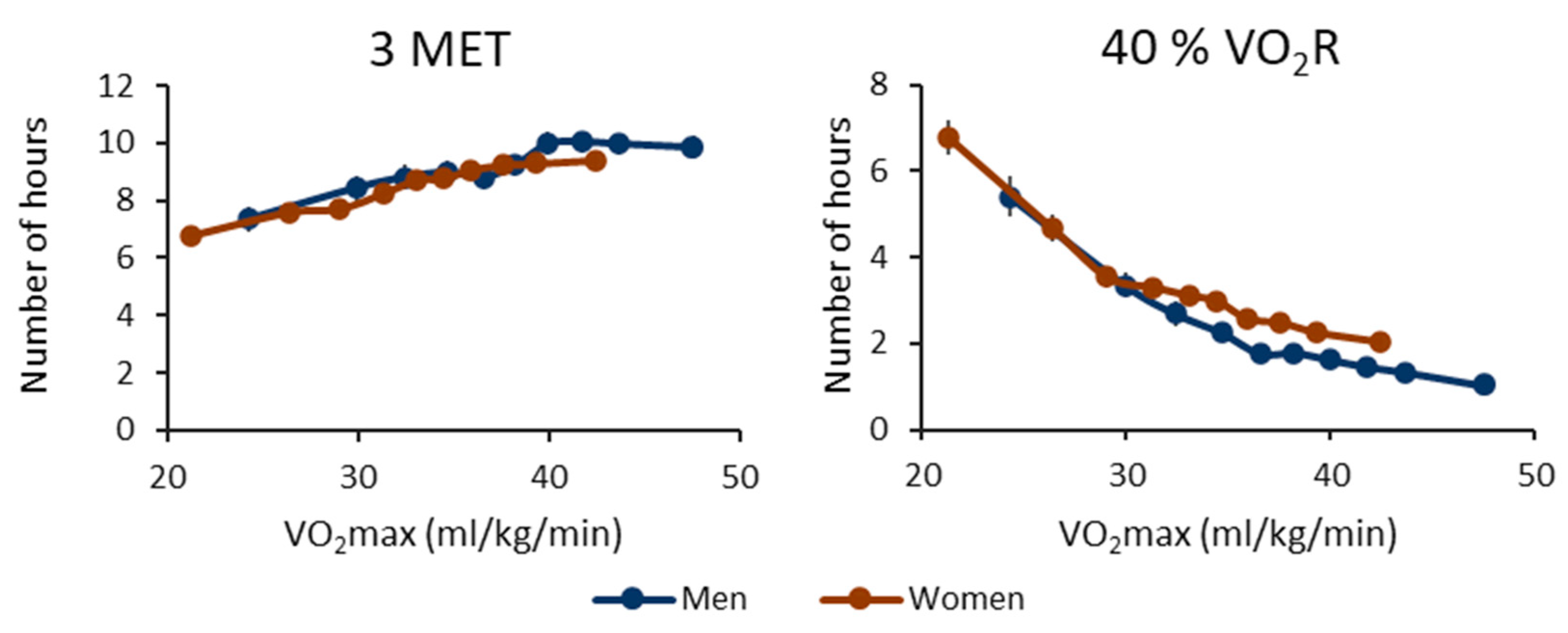
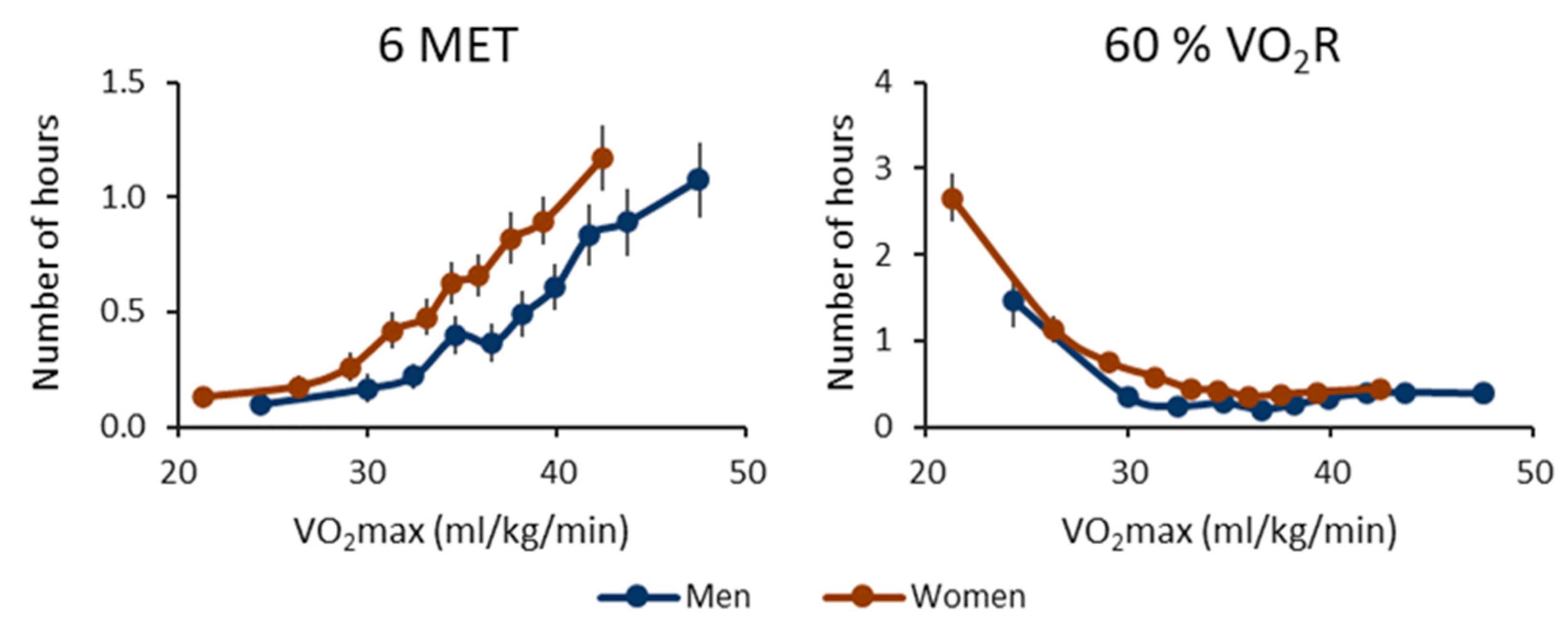
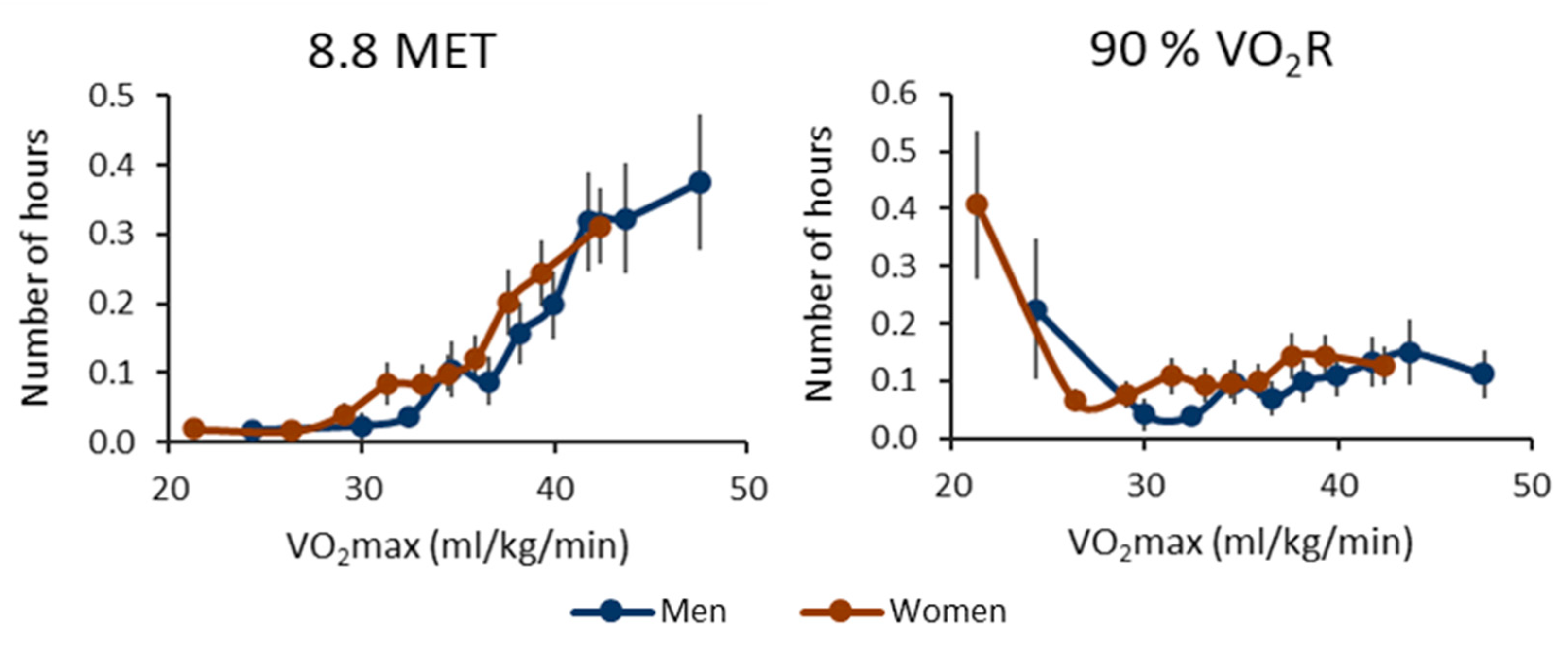
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Myers, J.; Kokkinos, P.; Arena, R.; LaMonte, M.J. The impact of moving more, physical activity, and cardiorespiratory fitness: Why we should strive to measure and improve fitness. Prog. Cardiovasc. Dis. 2021, 64, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Kaminsky, L.A.; Arena, R.; Ellingsen, Ø.; Harber, M.P.; Myers, J.; Ozemek, C.; Ross, R. Cardiorespiratory fitness and cardiovascular disease-the past, present, and future. Prog. Cardiovasc. Dis. 2019, 62, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Mandsager, K.; Harb, S.; Cremer, P.; Phelan, D.; Nissen, S.E.; Jaber, W. Association of Cardiorespiratory Fitness With Long-term Mortality Among Adults Undergoing Exercise Treadmill Testing. JAMA Netw. Open 2018, 1, e183605. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.; Durstine, J.L. Physical activity, exercise, and chronic diseases: A brief review. Sports Med. Health Sci. 2019, 1, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Gallo-Villegas, J.A.; Calderón, J.C. Epidemiological, mechanistic, and practical bases for assessment of cardi-orespiratory fitness and muscle status in adults in healthcare settings. Eur. J. Appl. Physiol. 2023, 123, 945–964. [Google Scholar] [CrossRef]
- Taherkhani, S.; Suzuki, K.; Castell, L. A Short Overview of Changes in Inflammatory Cytokines and Oxidative Stress in Response to Physical Activity and Antioxidant Supplementation. Antioxidants 2020, 9, 886. [Google Scholar] [CrossRef]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Despres, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement From the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef]
- Siddique, J.; Aaby, D.; Montag, S.E.; Sidney, S.; Sternfeld, B.; Welch, W.A.; Carnethon, M.R.; Liu, K.; Craft, L.L.; Gabriel, K.P.; et al. Individualized Relative-Intensity Physical Activity Accelerometer Cut Points. Med. Sci. Sports Exerc. 2020, 52, 398–407. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.-M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Orme, M.W.; Lloyd-Evans, P.H.; Jayamaha, A.R.; Katagira, W.; Kirenga, B.; Pina, I.; Kingsnorth, A.P.; Maylor, B.; Singh, S.J.; Rowlands, A.V. A Case for Unifying Accelerometry-Derived Movement Behaviors and Tests of Exercise Capacity for the Assessment of Relative Physical Activity Intensity. J. Phys. Act. Health 2023, 20, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Vähä-Ypyä, H.; Sievänen, H.; Husu, P.; Tokola, K.; Vasankari, T. Intensity Paradox—Low-Fit People Are Physically Most Active in Terms of Their Fitness. Sensors 2021, 21, 2063. [Google Scholar] [CrossRef] [PubMed]
- Vähä-Ypyä, H.; Sievänen, H.; Husu, P.; Tokola, K.; Mänttäri, A.; Heinonen, O.J.; Heiskanen, J.; Kaikkonen, K.M.; Savonen, K.; Kokko, S.; et al. How adherence to the updated physical activity guidelines should be assessed with accelerometer? Eur. J. Public Health 2022, 32, i50–i55. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Williams, P.T. Physical fitness and activity as separate heart disease risk factors: A meta-analysis. Med. Sci. Sports Exerc. 2001, 33, 754–761. [Google Scholar] [CrossRef]
- Trost, S.G. Population-level physical activity surveillance in young people: Are accelerometer-based measures ready for prime time? Int. J. Behav. Nutr. Phys. Act. 2020, 17, 28. [Google Scholar] [CrossRef]
- Fridolfsson, J.; Arvidsson, D.; Andersen, L.B.; Thorsson, O.; Wollmer, P.; Rosengren, B.; Karlsson, M.K.; Dencker, M. Physical activity spectrum discriminant analysis—A method to compare detailed patterns between groups. Scand. J. Med. Sci. Sports 2021, 31, 2333–2342. [Google Scholar] [CrossRef]
- Vasankari, V.; Halonen, J.; Vasankari, T.; Anttila, V.; Airaksinen, J.; Sievänen, H.; Hartikainen, J. Physical activity and sedentary behaviour in secondary prevention of coronary artery disease: A review. Am. J. Prev. Cardiol. 2021, 5, 100146. [Google Scholar] [CrossRef]
- Husu, P.; Tokola, K.; Vähä-Ypyä, H.; Sievänen, H.; Suni, J.; Heinonen, O.J.; Heiskanen, J.; Kaikkonen, K.M.; Savonen, K.; Kokko, S.; et al. Physical activity, sedentary behavior, and time in bed among finnish adults measured 24/7 by triaxial accelerometry. J. Meas. Phys. Behav. 2021, 4, 163–173. [Google Scholar] [CrossRef]
- Husu, P.; Vähä-Ypyä, H.; Tokola, K.; Sievänen, H.; Mänttäri, A.; Kokko, S.; Kaikkonen, K.M.; Savonen, K.; Vasankari, T. Measurement of Physical Fitness and 24/7 Physical Activity, Standing, Sedentary Behavior, and Time in Bed in Working-Age Finns: Study Protocol for FINFIT 2021. Methods Protoc. 2022, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Mänttäri, A.; Suni, J.; Sievänen, H.; Husu, P.; Vähä-Ypyä, H.; Valkeinen, H.; Tokola, K.; Vasankari, T. Six-minute walk test: A tool for predicting maximal aerobic power (VO 2 max) in healthy adults. Clin. Physiol. Funct. Imaging 2018, 38, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Vähä-Ypyä, H.; Bretterhofer, J.; Husu, P.; Windhaber, J.; Vasankari, T.; Titze, S.; Sievänen, H. Performance of Different Accelerometry-Based Metrics to Estimate Oxygen Consumption during Track and Treadmill Locomotion over a Wide In-tensity Range. Sensors 2023, 23, 5073. [Google Scholar] [CrossRef] [PubMed]
- Kruk, J.; Aboul-Enein, H.Y.; Kładna, A.; Bowser, J.E.; Jacquelyn, E. Bowser Oxidative stress in biological systems and its relation with pathophysiological functions: The effect of physical activity on cellular redox homeostasis. Free Radic. Res. 2019, 53, 497–521. [Google Scholar] [CrossRef]
- Gupta, N.; Dencker-Larsen, S.; McGregor, D.; Rasmussen, C.D.N.; Thorsen, S.V.; Jørgensen, M.B.; Chastin, S.; Holtermann, A. The physical activity paradox revisited: A prospective study on compositional accelerometer data and long-term sickness absence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 93. [Google Scholar] [CrossRef]
- Ketels, M.; Rasmussen, C.L.; Korshøj, M.; Gupta, N.; De Bacquer, D.; Holtermann, A.; Clays, E. The Relation between Domain-Specific Physical Behaviour and Cardiorespiratory Fitness: A Cross-Sectional Compositional Data Analysis on the Physical Activity Health Paradox Using Accelerometer-Assessed Data. Int. J. Environ. Res. Public Health 2020, 17, 7929. [Google Scholar] [CrossRef]
- Arvidsson, D.; Fridolfsson, J.; Börjesson, M. Measurement of physical activity in clinical practice using accelerom-eters. J. Intern. Med. 2019, 286, 137–153. [Google Scholar] [CrossRef]
- Holtermann, A.; Schnohr, P.; Nordestgaard, B.G.; Marott, J.L. The physical activity paradox in cardiovascular disease and all-cause mortality: The contemporary Copenhagen General Population Study with 104 046 adults. Eur. Hear. J. 2021, 42, 1499–1511. [Google Scholar] [CrossRef]
- Väisänen, D.; Kallings, L.V.; Andersson, G.; Wallin, P.; Hemmingsson, E.; Ekblom-Bak, E. Cardiorespiratory Fitness in Occupational Groups—Trends over 20 Years and Future Forecasts. Int. J. Environ. Res. Public Health 2021, 18, 8437. [Google Scholar] [CrossRef]
- Holtermann, A.; Rasmussen, C.L.; Hallman, D.M.; Ding, D.; Dumuid, D.; Gupta, N. 24-Hour Physical behavior balance for better health for all:“The sweet-spot hypothesis”. Sports Med.-Open 2021, 7, 98. [Google Scholar] [CrossRef]
- Zeiher, J.; Ombrellaro, K.J.; Perumal, N.; Keil, T.; Mensink, G.B.; Finger, J.D. Correlates and determinants of car-diorespiratory fitness in adults: A systematic review. Sports Med.-Open 2019, 5, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, P.; Faselis, C.; Samuel, I.B.H.; Lavie, C.J.; Zhang, J.; Vargas, J.D.; Pittaras, A.; Doumas, M.; Karasik, P.; Moore, H.; et al. Changes in Cardiorespiratory Fitness and Survival in Patients With or Without Cardiovascular Disease. J. Am. Coll. Cardiol. 2023, 81, 1137–1147. [Google Scholar] [CrossRef] [PubMed]
- Franklin, B.A.; Eijsvogels, T.M.; Pandey, A.; Quindry, J.; Toth, P.P. Physical activity, cardiorespiratory fitness, and cardiovascular health: A clinical practice statement of the ASPC Part I: Bioenergetics, contemporary physical activity rec-ommendations, benefits, risks, extreme exercise regimens, potential maladaptations. Am. J. Prev. Cardiol. 2022, 12, 100424. [Google Scholar] [CrossRef]
- Medrano-Ureña MD, R.; Ortega-Ruiz, R.; Benítez-Sillero, J.D.D. Physical fitness, exercise self-efficacy, and quality of life in adulthood: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 6343. [Google Scholar] [CrossRef] [PubMed]
| Sex and Age Group | N | CRF Group | VO2max (mL/kg/min) | BMI (kg/m2) | Peak MET | Peak VO2R |
|---|---|---|---|---|---|---|
| Men | ||||||
| 20–29 | 80 | low | 35.2 (5.1) MH | 28.0 (5.4) H | 5.9 (0.9) H | 55% (11%) H |
| med | 42.4 (0.9) LH | 25.4 (3.2) H | 6.8 (1.5) | 52% (13%) | ||
| high | 47.4 (2.2) LM | 22.9 (2.4) LM | 7.0 (1.8) L | 47% (13%) L | ||
| 30–39 | 205 | low | 35.1 (2.9) MH | 29.1 (4.3) MH | 5.5 (0.9) MH | 51% (11%) |
| med | 39.9 (1.1) LH | 25.7 (2.7) LH | 6.4 (1.6) L | 52% (15%) | ||
| high | 45.0 (2.3) LM | 24.5 (2.7) LM | 6.9 (1.9) L | 49% (16%) | ||
| 40–49 | 288 | low | 31.4 (3.8) MH | 29.8 (4.8) MH | 5.5 (1.2) MH | 58% (18%) MH |
| med | 38.1 (1.5) LH | 26.3 (2.9) LH | 6.0 (1.2) LH | 50% (12%) L | ||
| high | 43.4 (2.3) LM | 24.4 (2.4) LM | 6.9 (1.8) LM | 51% (15%) L | ||
| 50–59 | 357 | low | 28.1 (3.8) MH | 29.9 (4.0) MH | 4.9 (0.8) MH | 57% (12%) MH |
| med | 34.7 (1.4) LH | 26.5 (2.6) LH | 5.6 (1.2) LH | 51% (13%) L | ||
| high | 40.0 (2.2) LM | 25.6 (2.3) LM | 5.9 (1.2) LM | 48% (11%) L | ||
| 60–69 | 517 | low | 25.1 (3.9) MH | 29.5 (4.1) MH | 4.7 (0.7) MH | 61% (15%) MH |
| med | 31.3 (1.2) LH | 27.2 (3.0) LH | 5.0 (0.7) LH | 51% (9%) LH | ||
| high | 36.8 (2.4) LM | 24.8 (3.1) LM | 5.6 (1.2) LM | 48% (12%) LM | ||
| Women | ||||||
| 20–29 | 188 | low | 33.3 (4.4) MH | 26.9 (4.6) MH | 6.1 (1.1) H | 61% (14%) MH |
| med | 39.3 (2.7) LH | 23.8 (2.9) LH | 6.6 (1.4) H | 55% (14%) L | ||
| high | 44.0 (3.5) LM | 21.7 (2.4) LM | 6.9 (1.5) LM | 51% (12%) L | ||
| 30–39 | 326 | low | 31.4 (4.6) MH | 29.1 (4.4) MH | 5.6 (1.0) MH | 60% (16%) MH |
| med | 37.5 (2.4) LH | 24.9 (2.6) LH | 6.3 (1.3) LH | 55% (14%) L | ||
| high | 42.5 (3.0) LM | 22.8 (2.8) LM | 6.8 (1.7) LM | 53% (15%) L | ||
| 40–49 | 448 | low | 28.8 (4.3) MH | 30.7 (4.7) MH | 5.5 (1.0) MH | 64% (19%) MH |
| med | 35.8 (2.3) LH | 25.2 (2.7) LH | 5.9 (1.1) LH | 53% (12%) L | ||
| high | 40.9 (2.9) LM | 23.0 (2.3) LM | 6.8 (1.7) LM | 54% (15%) L | ||
| 50–59 | 515 | low | 26.1 (3.9) MH | 30.5 (3.9) MH | 4.9 (0.8) MH | 62% (16%) MH |
| med | 32.7 (2.2) LH | 26.4 (2.7) LH | 5.5 (1.0) LH | 54% (12%) L | ||
| high | 37.7 (2.9) LM | 24.3 (2.6) LM | 6.0 (1.2) LM | 51% (12%) L | ||
| 60–69 | 663 | low | 23.5 (3.8) MH | 30.3 (4.3) MH | 4.6 (0.6) MH | 65% (16%) MH |
| med | 30.1 (1.6) LH | 26.2 (3.0) LH | 5.0 (0.7) LH | 53% (9%) LH | ||
| high | 35.6 (2.5) LM | 23.7 (2.9) LM | 5.5 (1.0) LM | 49% (11%) LM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vähä-Ypyä, H.; Husu, P.; Sievänen, H.; Vasankari, T. What Can One Minute of the Day Tell about Physical Activity? Int. J. Environ. Res. Public Health 2023, 20, 6852. https://doi.org/10.3390/ijerph20196852
Vähä-Ypyä H, Husu P, Sievänen H, Vasankari T. What Can One Minute of the Day Tell about Physical Activity? International Journal of Environmental Research and Public Health. 2023; 20(19):6852. https://doi.org/10.3390/ijerph20196852
Chicago/Turabian StyleVähä-Ypyä, Henri, Pauliina Husu, Harri Sievänen, and Tommi Vasankari. 2023. "What Can One Minute of the Day Tell about Physical Activity?" International Journal of Environmental Research and Public Health 20, no. 19: 6852. https://doi.org/10.3390/ijerph20196852
APA StyleVähä-Ypyä, H., Husu, P., Sievänen, H., & Vasankari, T. (2023). What Can One Minute of the Day Tell about Physical Activity? International Journal of Environmental Research and Public Health, 20(19), 6852. https://doi.org/10.3390/ijerph20196852









