Predicting Unmet Healthcare Needs in Post-Disaster: A Machine Learning Approach
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Measurement of Unmet Healthcare Needs
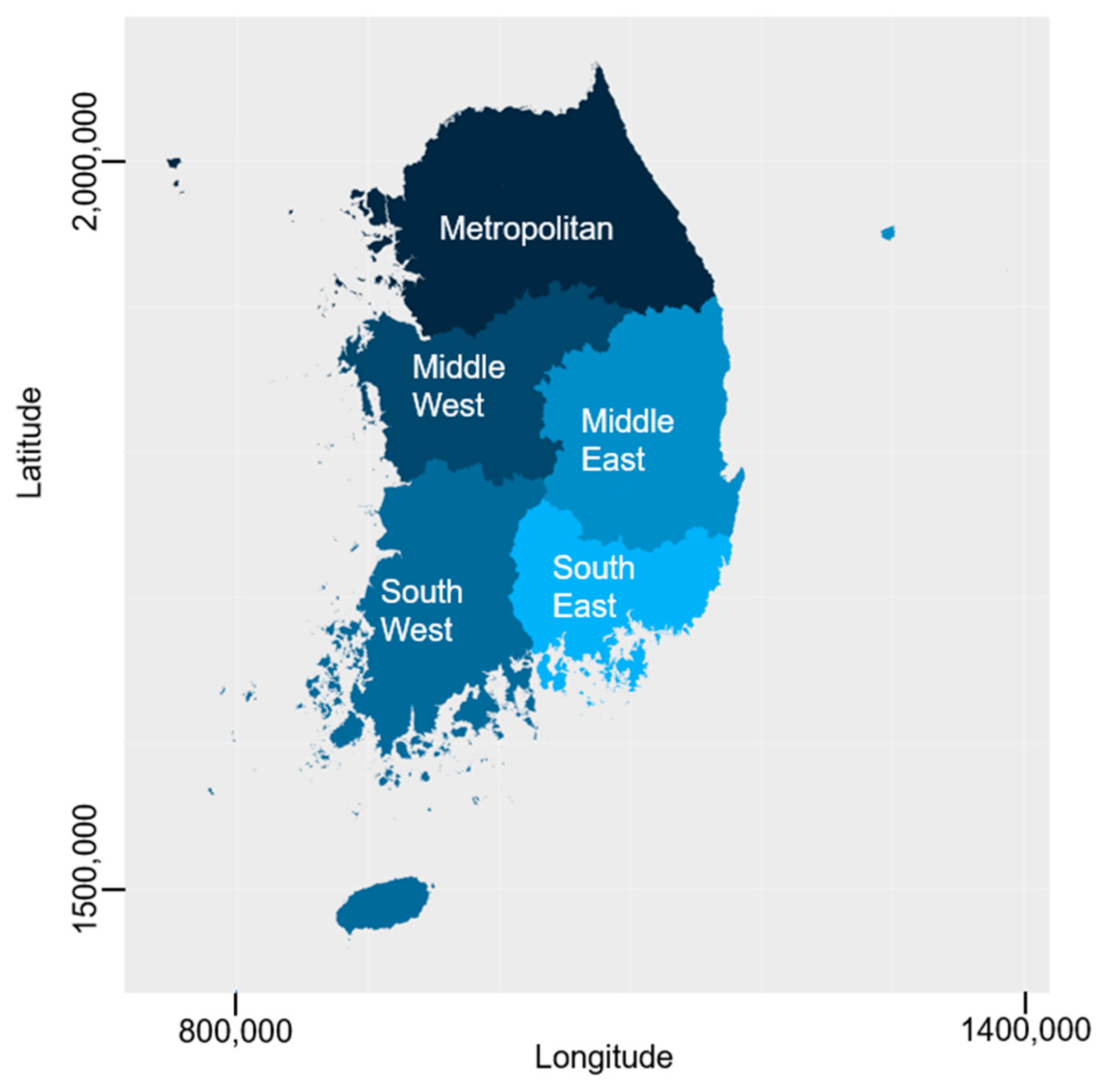
2.3. Variables for Prediction Algorithms
2.4. Machine Learning and Statistical Analyses
3. Results
3.1. Study Population
3.2. Estimating Unmet Healthcare Needs Related to Disasters
3.3. Predictive Model for Unmet Healthcare Needs
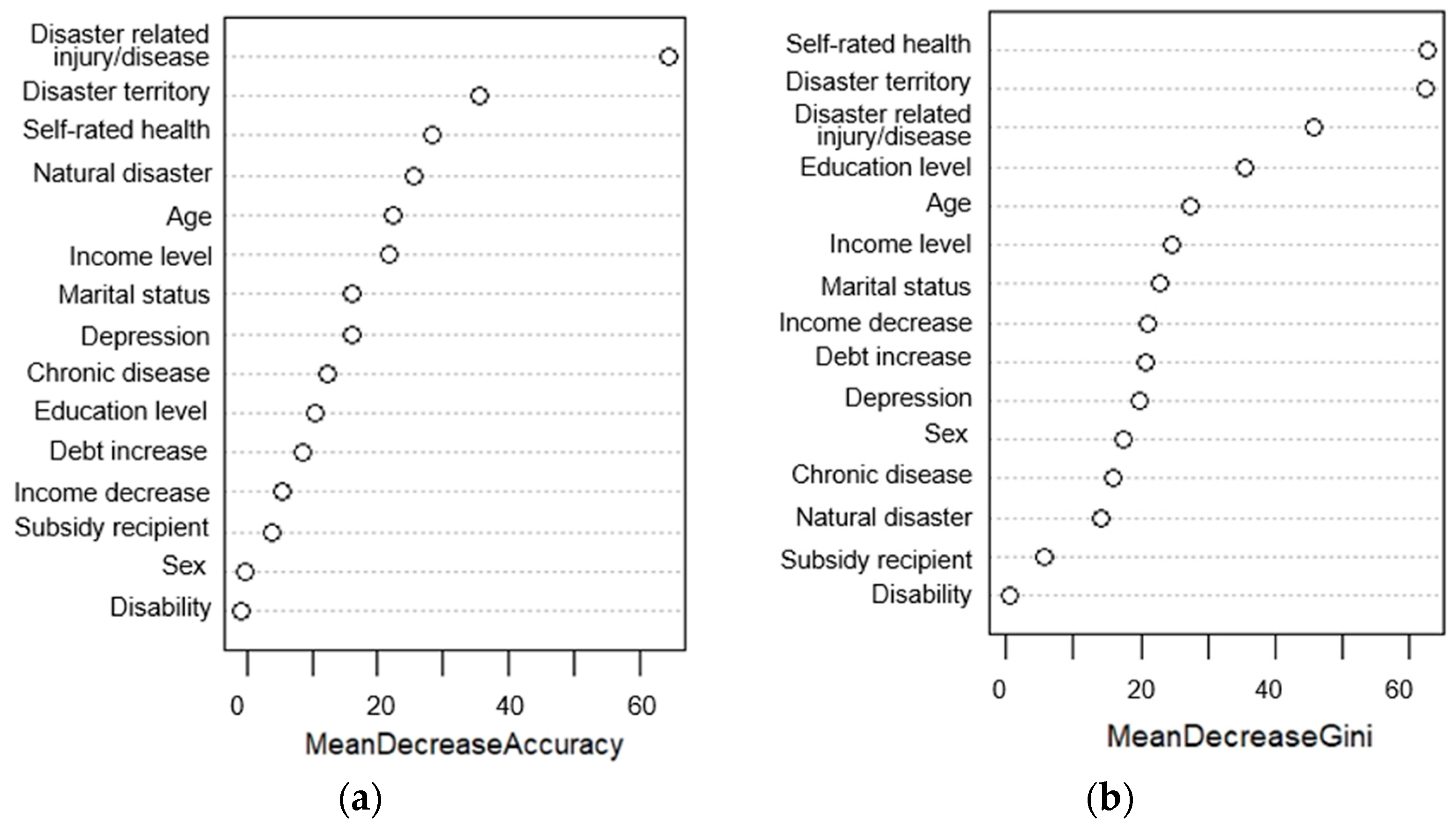
3.4. Important Variables in the Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Davis, J.R.; Wilson, S.; Brock-Martin, A.; Glover, S.; Svendsen, E.R. The impact of disasters on populations with health and health care disparities. Disaster Med. Public Health Prep. 2010, 4, 30–38. [Google Scholar] [CrossRef]
- Fonseca, V.A.; Smith, H.; Kuhadiya, N.; Leger, S.M.; Yau, C.L.; Reynolds, K.; Shi, L.; McDuffie, R.H.; Thethi, T.; John-Kalarickal, J. Impact of a natural disaster on diabetes: Exacerbation of disparities and long-term consequences. Diabetes Care 2009, 32, 1632–1638. [Google Scholar] [CrossRef] [PubMed]
- Finch, C.; Emrich, C.T.; Cutter, S.L. Disaster disparities and differential recovery in New Orleans. Popul. Environ. 2010, 31, 179–202. [Google Scholar] [CrossRef]
- Collins, T.W.; Jimenez, A.M.; Grineski, S.E. Hispanic health disparities after a flood disaster: Results of a population-based survey of individuals experiencing home site damage in El Paso (Texas, USA). J. Immigr. Minor. Health 2013, 15, 415–426. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.B.; Collins, T.W.; Grineski, S.E.; Chakraborty, J. Social vulnerability to Hurricane Harvey: Unmet needs and adverse event experiences in Greater Houston, Texas. Int. J. Disaster Risk Reduct. 2020, 46, 101521. [Google Scholar] [CrossRef]
- Runkle, J.D.; Zhang, H.; Karmaus, W.; Martin, A.B.; Svendsen, E.R. Prediction of unmet primary care needs for the medically vulnerable post-disaster: An interrupted time-series analysis of health system responses. Int. J. Environ. Res. Public Health 2012, 9, 3384–3397. [Google Scholar] [CrossRef]
- Brackbill, R.M.; Stellman, S.D.; Perlman, S.E.; Walker, D.J.; Farfel, M.R. Mental health of those directly exposed to the World Trade Center disaster: Unmet mental health care need, mental health treatment service use, and quality of life. Soc. Sci. Med. 2013, 81, 110–114. [Google Scholar] [CrossRef]
- Mack, D.; Brantley, K.M.; Bell, K.G. Mitigating the health effects of disasters for medically underserved populations: Electronic health records, telemedicine, research, screening, and surveillance. J. Health Care Poor Underserved 2007, 18, 432–442. [Google Scholar] [CrossRef]
- Enarson, E. Through women’s eyes: A gendered research agenda for disaster social science. Disasters 1998, 22, 157–173. [Google Scholar] [CrossRef]
- Smith, G.S.; Anjum, E.; Francis, C.; Deanes, L.; Acey, C. Climate change, environmental disasters, and health inequities: The underlying role of structural inequalities. Curr. Environ. Health Rep. 2022, 9, 80–89. [Google Scholar] [CrossRef]
- Phibbs, S.; Kenney, C.; Severinsen, C.; Mitchell, J.; Hughes, R. Synergising public health concepts with the Sendai framework for disaster risk reduction: A conceptual glossary. Int. J. Environ. Res. Public Health 2016, 13, 1241. [Google Scholar] [CrossRef]
- Carr, W.; Wolfe, S. Unmet Needs as Sociomedical Indicators. Int. J. Health Serv. 1976, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Sanmartin, C.; Houle, C.; Tremblay, S.; Berthelot, J.-M. Changes in unmet health care needs. Health Rep. 2002, 13, 15–21. [Google Scholar]
- Allin, S.; Grignon, M.; Le Grand, J. Subjective unmet need and utilization of health care services in Canada: What are the equity implications? Soc. Sci. Med. 2010, 70, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Reinhardt, U.E.; Cheng, T.-M. The world health report 2000-Health systems: Improving performance. Bull. World Health Organ. 2000, 78, 1064. [Google Scholar]
- Ju, Y.J.; Kim, T.H.; Han, K.-T.; Lee, H.J.; Kim, W.; Lee, S.A.; Park, E.-C. Association between unmet healthcare needs and health-related quality of life: A longitudinal study. Eur. J. Public Health 2017, 27, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Ronksley, P.E.; Sanmartin, C.; Quan, H.; Ravani, P.; Tonelli, M.; Manns, B.; Hemmelgarn, B.R. Association between perceived unmet health care needs and risk of adverse health outcomes among patients with chronic medical conditions. Open Med. 2013, 7, e21. [Google Scholar]
- Stuber, J.; Galea, S.; Boscarino, J.A.; Schlesinger, M. Was there unmet mental health need after the September 11, 2001 terrorist attacks? Soc. Psychiatry Psychiatr. Epidemiol. 2006, 41, 230–240. [Google Scholar] [CrossRef]
- Allin, S.; Masseria, C. Unmet need as an indicator of health care access. Eurohealth 2009, 15, 7–9. [Google Scholar]
- Koyama, Y.; Fujiwara, T.; Yagi, J.; Mashiko, H.; Great East Japan Earthquake Follow-up; Children Study Team. Association of parental dissatisfaction and perceived inequality of post-disaster recovery process with child mental health. Soc. Sci. Med. 2022, 296, 114723. [Google Scholar] [CrossRef]
- Kammerbauer, M.; Wamsler, C. Social inequality and marginalization in post-disaster recovery: Challenging the consensus? Int. J. Disaster Risk Reduct. 2017, 24, 411–418. [Google Scholar] [CrossRef]
- Sovacool, B.K.; Tan-Mullins, M.; Abrahamse, W. Bloated bodies and broken bricks: Power, ecology, and inequality in the political economy of natural disaster recovery. World Dev. 2018, 110, 243–255. [Google Scholar] [CrossRef]
- Ray-Bennett, N.S.; Collins, A.; Bhuiya, A.; Edgeworth, R.; Nahar, P.; Alamgir, F. Exploring the meaning of health security for disaster resilience through people’s perspectives in Bangladesh. Health Place 2010, 16, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Reid, M. Disasters and social inequalities. Sociol. Compass 2013, 7, 984–997. [Google Scholar] [CrossRef]
- Jenkins, J.; Hsu, E.; Sauer, L.; Hsieh, Y.-H.; Kirsch, T. Prevalence of Unmet Health Care Needs and Description of Health Care-seeking Behavior Among Displaced People After the 2007 California Wildfires. Disaster Med. Public Health Prep. 2009, 3, S24–S28. [Google Scholar] [CrossRef]
- Aitsi-Selmi, A.; Murray, V. The Sendai framework: Disaster risk reduction through a health lens. SciELO Public Health 2015, 93, 362. [Google Scholar] [CrossRef]
- Zagorecki, A.T.; Johnson, D.E.; Ristvej, J. Data mining and machine learning in the context of disaster and crisis management. Int. J. Emerg. Manag. 2013, 9, 351–365. [Google Scholar] [CrossRef]
- Arinta, R.R.; WR, E.A. Natural disaster application on big data and machine learning: A review. In Proceedings of the 2019 4th International Conference on Information Technology, Information Systems and Electrical Engineering (ICITISEE), Yogyakarta, Indonesia, 20–21 November 2019; pp. 249–254. [Google Scholar]
- Abid, S.K.; Sulaiman, N.; Chan, S.W.; Nazir, U.; Abid, M.; Han, H.; Ariza-Montes, A.; Vega-Muñoz, A. Toward an integrated disaster management approach: How artificial intelligence can boost disaster management. Sustainability 2021, 13, 12560. [Google Scholar] [CrossRef]
- Khouj, M.; López, C.; Sarkaria, S.; Marti, J. Disaster management in real time simulation using machine learning. In Proceedings of the 2011 24th Canadian Conference on Electrical and Computer Engineering (CCECE), Niagara Falls, ON, Canada, 8–11 May 2011; pp. 1507–1510. [Google Scholar]
- Linardos, V.; Drakaki, M.; Tzionas, P.; Karnavas, Y.L. Machine Learning in Disaster Management: Recent Developments in Methods and Applications. Mach. Learn. Knowl. Extr. 2022, 4, 446–473. [Google Scholar] [CrossRef]
- Park, S.C.; Jung, T.; Lee, Y.S.; Jang, E.J.; Yoo, E.J. Research of the Factors of Life Change in Disaster Victims and Development of Technology for Relief Services; National Disaster Management Research Institute: Seoul, Korea, 2016; p. 157. [Google Scholar]
- Jalali-Najafabadi, F.; Stadler, M.; Dand, N.; Jadon, D.; Soomro, M.; Ho, P.; Marzo-Ortega, H.; Helliwell, P.; Korendowych, E.; Simpson, M.A. Application of information theoretic feature selection and machine learning methods for the development of genetic risk prediction models. Sci. Rep. 2021, 11, 1–14. [Google Scholar] [CrossRef]
- Andersen, R. A behavioral model of families’ use of health services. In Research Series; Center for Health Administration Studies: Chicago, IL, USA, 1968. [Google Scholar]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Kumar, S.; Luo, C. US adults with unmet mental health treatment needs: Profiling and underlying causes using machine learning techniques. IISE Trans. Healthc. Syst. Eng. 2019, 9, 186–199. [Google Scholar] [CrossRef]
- Yoo, S.H.; Park, I.S.; Kim, Y.M. A Decision-Tree Analysis of Influential Factors and Reasons for Unmet Dental Care in Korean Adults. Health Soc. Welf. Rev. 2017, 37, 294–335. [Google Scholar] [CrossRef]
- Christodoulou, E.; Ma, J.; Collins, G.S.; Steyerberg, E.W.; Verbakel, J.Y.; Van Calster, B. A systematic review shows no performance benefit of machine learning over logistic regression for clinical prediction models. J. Clin. Epidemiol. 2019, 110, 12–22. [Google Scholar] [CrossRef]
- Watson, D.S.; Krutzinna, J.; Bruce, I.N.; Griffiths, C.E.; McInnes, I.B.; Barnes, M.R.; Floridi, L. Clinical applications of machine learning algorithms: Beyond the black box. BMJ 2019, 364, I886. [Google Scholar] [CrossRef]
- James, G.; Witten, D.; Hastie, T.; Tibshirani, R. An Introduction to Statistical Learning; Springer: Berlin/Heidelberg, Germany, 2013; Volume 112. [Google Scholar]
- Thabtah, F.; Abdelhamid, N.; Peebles, D. A machine learning autism classification based on logistic regression analysis. Health Inf. Sci. Syst. 2019, 7, 12. [Google Scholar] [CrossRef] [PubMed]
- Lemon, S.C.; Roy, J.; Clark, M.A.; Friedmann, P.D.; Rakowski, W. Classification and regression tree analysis in public health: Methodological review and comparison with logistic regression. Ann. Behav. Med. 2003, 26, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, M.; Johnson, K. Applied Predictive Modeling; Springer: Berlin/Heidelberg, Germany, 2013; Volume 26. [Google Scholar]
- Pandya, R.; Pandya, J. C5. 0 algorithm to improved decision tree with feature selection and reduced error pruning. Int. J. Comput. Appl. 2015, 117, 18–21. [Google Scholar] [CrossRef]
- Biau, G.; Scornet, E. A random forest guided tour. Test 2016, 25, 197–227. [Google Scholar] [CrossRef]
- Zhu, Z.; Zhang, Y. Flood disaster risk assessment based on random forest algorithm. Neural Comput. Appl. 2022, 34, 3443–3455. [Google Scholar] [CrossRef]
- Choi, C.; Kim, J.; Kim, J.; Kim, H.S. Development of combined heavy rain damage prediction models with machine learning. Water 2019, 11, 2516. [Google Scholar] [CrossRef]
- Li, M.; Hou, H.; Yu, J.; Geng, H.; Zhu, L.; Huang, Y.; Li, X. Prediction of power outage quantity of distribution network users under typhoon disaster based on random forest and important variables. Math. Probl. Eng. 2021, 2021, 6682242. [Google Scholar] [CrossRef]
- Bruce, P.C.; Shmueli, G.; Patel, N.R. Data Mining for Business Analytics: Concepts, Techniques, and Applications with XLMiner; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Kim, T.H.; Shin, Y.J.; Kwon, R.A. Multi-Level Analysis of Factors Affecting Unmet Medical Needs by Medical Security Type. J. Crit. Soc. Welf. 2020, 67, 41–69. [Google Scholar] [CrossRef]
- Jeon, B.; Kwon, S. Access Barriers To Health Care Among Persons With Physical Disabilities: Using Three Reasons For Unmet Need As Indicators Of Access. Korean Soc. Secur. Stud. 2015, 31, 145–171. [Google Scholar]
- Huh, S.-I.; Lee, H.-J. Unmet Health Care Needs and Attitudes towards Health Care System in Korea. Korean J. Health Econ. Policy 2016, 22, 59–89. [Google Scholar]
- Anderson, G.V. Universal health care coverage in Korea. Health Aff. 1989, 8, 24–34. [Google Scholar] [CrossRef]
- Kwon, S. Thirty years of national health insurance in South Korea: Lessons for achieving universal health care coverage. Health Policy Plan. 2009, 24, 63–71. [Google Scholar] [CrossRef]
- Hwang, J. Understanding reasons for unmet health care needs in Korea: What are health policy implications? BMC Health Serv. Res. 2018, 18, 557. [Google Scholar] [CrossRef]
- Choi, J.W.; Park, E.C.; Yoo, K.B.; Lee, S.G.; Jang, S.I.; Kim, T.H. The effect of high medical expenses on household income in South Korea: A longitudinal study using propensity score matching. BMC Health Serv. Res. 2015, 15, 369. [Google Scholar] [CrossRef]
- Kim, Y.-S.; Lee, J.; Moon, Y.; Kim, K.J.; Lee, K.; Choi, J.; Han, S.-H. Unmet healthcare needs of elderly people in Korea. BMC Geriatr. 2018, 18, 98. [Google Scholar] [CrossRef]
- Chen, J.; Hou, F. Unmet needs for health care. Health Rep. 2002, 13, 23–34. [Google Scholar] [PubMed]
- Shin, Y.; Shon, J. The prevalence and association factors of unmet medical need-using the 1st and 2nd Korea welfare panel data. Health Soc. Welf. Rev. 2009, 29, 111–142. [Google Scholar]
- Chen, W.; Xie, X.; Wang, J.; Pradhan, B.; Hong, H.; Bui, D.T.; Duan, Z.; Ma, J. A comparative study of logistic model tree, random forest, and classification and regression tree models for spatial prediction of landslide susceptibility. Catena 2017, 151, 147–160. [Google Scholar] [CrossRef]
- Brackbill, R.M.; Hadler, J.L.; DiGrande, L.; Ekenga, C.C.; Farfel, M.R.; Friedman, S.; Perlman, S.E.; Stellman, S.D.; Walker, D.J.; Wu, D. Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack. JAMA 2009, 302, 502–516. [Google Scholar] [CrossRef]
- Holman, E.A.; Silver, R.C. Health status and health care utilization following collective trauma: A 3-year national study of the 9/11 terrorist attacks in the United States. Soc. Sci. Med. 2011, 73, 483–490. [Google Scholar] [CrossRef]
- Eberhardt, M.S.; Pamuk, E.R. The importance of place of residence: Examining health in rural and nonrural areas. Am. J. Public Health 2004, 94, 1682–1686. [Google Scholar] [CrossRef]
- Ahern, J.; Galea, S. Social context and depression after a disaster: The role of income inequality. J. Epidemiol. Community Health 2006, 60, 766–770. [Google Scholar] [CrossRef]

| Variables | Total | Unmet Healthcare Need | p-Value | |
|---|---|---|---|---|
| No | Yes | |||
| N | 1659 | 1136 | 523 | |
| Gender | <0.000 * | |||
| Male | 806 (48.6) | 595 (52.4) | 211 (40.3) | |
| Female | 853 (51.4) | 541 (47.6) | 312 (59.7) | |
| Age (in years) | <0.000 * | |||
| 13–18 | 41 (2.5) | 39 (3.4) | 2 (0.4) | |
| 19–39 | 222 (13.7) | 169 (14.9) | 53 (10.1) | |
| 40–64 | 725 (44.0) | 525 (46.2) | 200 (38.2) | |
| 65 and over | 671 (32.7) | 403 (35.5) | 268 (51.2) | |
| Marital status | <0.000 * | |||
| Unmarried | 252 (15.2) | 198 (17.4) | 54 (10.3) | |
| Married | 1129 (68.1) | 779 (68.6) | 350 (66.9) | |
| Divorced, separated, or widowed | 278 (16.8) | 159 (14.0) | 119 (22.8) | |
| Education level | <0.000 * | |||
| Elementary school or less | 517 (31.2) | 313 (27.6) | 204 (39.0) | |
| Middle school | 297 (17.9) | 195 (17.2) | 102 (19.5) | |
| High school | 619 (37.3) | 447 (39.3) | 172 (32.9) | |
| University or higher | 226 (13.6) | 181 (15.9) | 45 (8.6) | |
| Monthly household income (KRW) | <0.000 * | |||
| Less than 1 M | 341 (20.6) | 196 (17.3) | 145 (27.7) | |
| 1 M~less than 5 M | 1188 (71.6) | 838 (73.8) | 350 (66.9) | |
| 5 M~less than 9 M | 120 (7.2) | 94 (8.3) | 26 (5.0) | |
| 9 M or higher | 10 (0.6) | 8 (0.7) | −0.4 | |
| Residential area | <0.000 * | |||
| Metropolitan | 248 (14.9) | 176 (15.5) | 72 (13.8) | |
| Middle west | 215 (13) | 155 (13.6) | 60 (11.5) | |
| South west | 550 (33.2) | 403 (35.5) | 147 (28.1) | |
| Middle east | 187 (11.3) | 86 (7.6) | 101 (19.3) | |
| South east | 459 (27.7) | 316 (27.8) | 143 (27.3) | |
| Self-rated heath, mean (SD) | 4.4 (1.4) | 4.6 (1.4) | 3.8 (1.4) | <0.000 † |
| Chronic disease | <0.000 * | |||
| Yes | 527 (31.8) | 311 (27.4) | 216 (41.3) | |
| No | 1132 (68.2) | 825 (72.6) | 307 (58.7) | |
| Disability | 0.023 * | |||
| Yes | 9 (0.5) | 3 (0.3) | 6 (1.1) | |
| No | 1650 (99.5) | 1133 (99.7) | 517 (98.9) | |
| Depression | <0.000 * | |||
| Yes | 959 (59.2) | 585 (51.5) | 374 (71.5) | |
| No | 660 (40.8) | 551 (48.5) | 149 (28.5) | |
| Type of disaster experience | <0.000 * | |||
| Natural disaster | 1549 (93.4) | 1086 (95.6) | 463 (88.5) | |
| Social disaster | 110 (6.6) | 50 (4.4) | 60 (11.5) | |
| Precision | Accuracy | Misclassification Rate | AUC-ROC 1 | F-1 Score | |
|---|---|---|---|---|---|
| Logistics regression | 70.00% | 75.20% | 24.8% | 0.774 | 70.59% |
| C5.0 | 65.40% | 76.60% | 17.1% | 0.805 | 73.62% |
| Random forest | 79.20% | 77.59% | 23.71% | 0.830 | 76.51% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, H.J.; Suh, H.S. Predicting Unmet Healthcare Needs in Post-Disaster: A Machine Learning Approach. Int. J. Environ. Res. Public Health 2023, 20, 6817. https://doi.org/10.3390/ijerph20196817
Han HJ, Suh HS. Predicting Unmet Healthcare Needs in Post-Disaster: A Machine Learning Approach. International Journal of Environmental Research and Public Health. 2023; 20(19):6817. https://doi.org/10.3390/ijerph20196817
Chicago/Turabian StyleHan, Hyun Jin, and Hae Sun Suh. 2023. "Predicting Unmet Healthcare Needs in Post-Disaster: A Machine Learning Approach" International Journal of Environmental Research and Public Health 20, no. 19: 6817. https://doi.org/10.3390/ijerph20196817
APA StyleHan, H. J., & Suh, H. S. (2023). Predicting Unmet Healthcare Needs in Post-Disaster: A Machine Learning Approach. International Journal of Environmental Research and Public Health, 20(19), 6817. https://doi.org/10.3390/ijerph20196817






