Design of Innovative Clothing for Pressure Injury Prevention: End-User Evaluation in a Mixed-Methods Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Participants and Recruitment
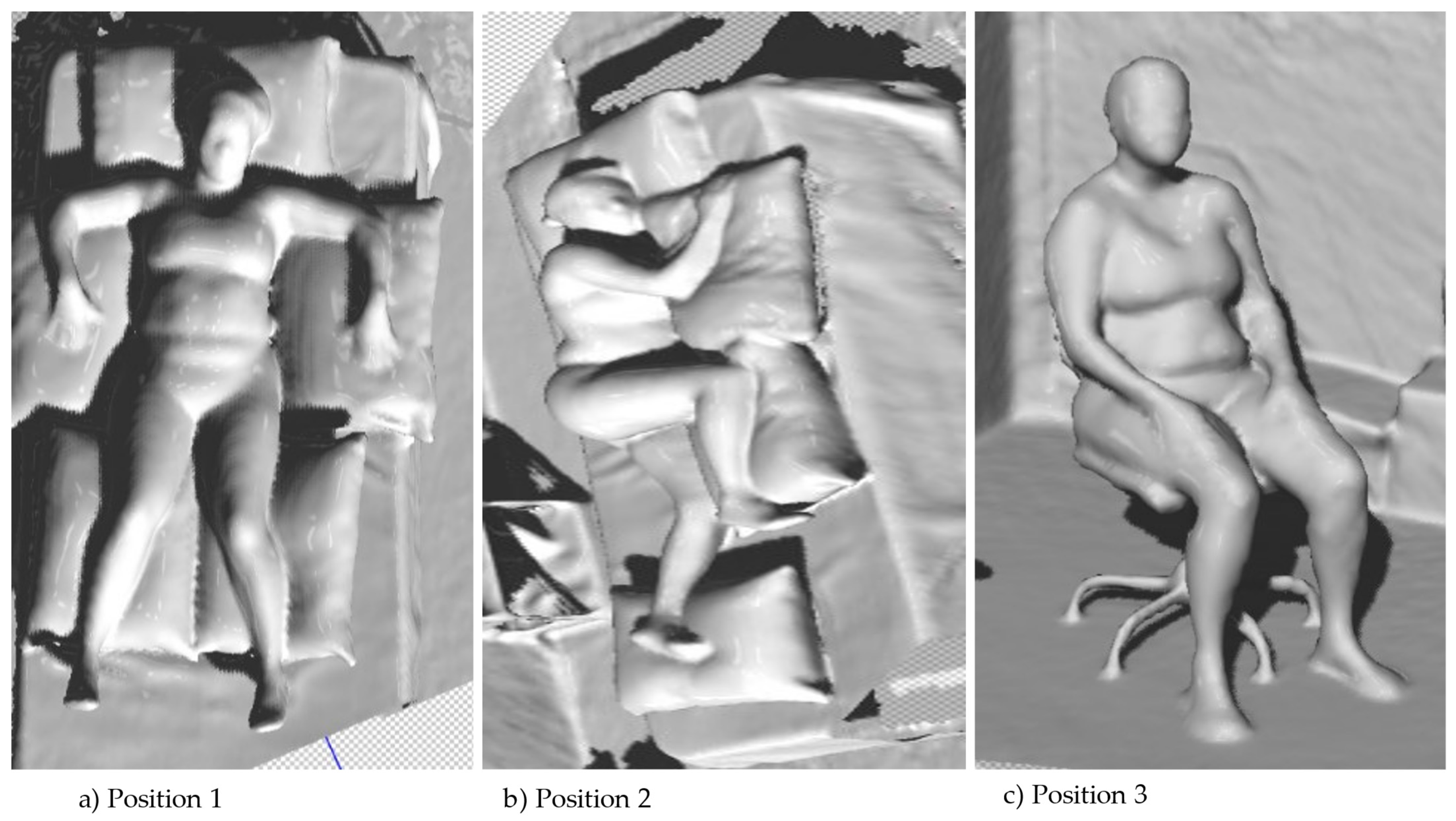
2.4. Description of the Prototype
2.5. Data Collection Instruments and Procedures
- -
- How likely are you to adopt the prototype of pajamas for PI prevention in home environments, residential facilities for the elderly, long-term care units, or hospitals?
- -
- About the characteristics of the presented prototype pajamas, what aspects should be improved and why?
- -
- What should be the number of openings and the distance between the pieces composing the pajamas? What are the reasons behind these choices?
- -
- What are the advantages and disadvantages of each of the presented prototypes?
- -
- How do you perceive the safety of the presented pajama prototypes for individuals with reduced mobility?
2.6. Data Analysis and Treatment Procedure
3. Results
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gefen, A.; Brienza, D.M.; Cuddigan, J.; Haesler, E.; Kottner, J. Our Contemporary Understanding of the A etiology of Pressure Ulcers/Pressure Injuries. Int. Wound J. 2022, 19, 692–704. [Google Scholar] [CrossRef]
- European Pressure Ulcer Advisory Panel/National Pressure Injury Advisory Panel/Pan Pacific Pressure Injury Alliance. Prevenção e Tratamento de Lesões/Úlceras por Pressão GUIA de Consulta Rápida (Brazilian edition); Haesler, E., Ed.; EPUAP/NPIAP/PPPIA: Prague, Czech Republic, 2019. [Google Scholar]
- Awoke, N.; Tekalign, T.; Arba, A.; Lenjebo, T.L. Pressure Injury Prevention Practice and Associated Factors among Nurses at Wolaita Sodo University Teaching and Referral Hospital, South Ethiopia: A Cross-Sectional Study. BMJ Open 2022, 12, e047687. [Google Scholar] [CrossRef]
- Parvizi, A.; Haddadi, S.; Mollaei, A.; Ghorbani Vajargah, P.; Takasi, P.; Firooz, M.; Hosseini, S.J.; Farzan, R.; Karkhah, S. A Systematic Review of Nurses’ Knowledge and Related Factors towards the Prevention of Medical Device-related Pressure Ulcers. Int. Wound J. 2023, 20, 2843–2854. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, C.; Nelson, E.A.; Nixon, J.; Vargas-Palacios, A.; McGinnis, E. Comparative Effectiveness of Heel-Specific Medical Devices for the Prevention of Heel Pressure Ulcers: A Systematic Review. J. Tissue Viability 2022, 31, 579–592. [Google Scholar] [CrossRef]
- Mamom, J.; Daovisan, H. Repositioning Mattress: How a Lateral Tilt Position Reshapes the Prevention of Pressure Ulcers in Bedridden Patients. J. Med. Eng. Technol. 2022, 46, 658–669. [Google Scholar] [CrossRef] [PubMed]
- Jeerapan, I.; Khumngern, S. Printed Devices for Wearable Biosensors: Laboratory to Emerging Markets. IEEE J. Flex. Electron. 2023, 1. [Google Scholar] [CrossRef]
- Sikka, M.P.; Garg, S. Functional Textiles for Prevention of Pressure Ulcers—A Review. Res. J. Text. Appar. 2020, 24, 185–198. [Google Scholar] [CrossRef]
- Imbesi, S.; Scataglini, S. A User Centered Methodology for the Design of Smart Apparel for Older Users. Sensors 2021, 21, 2804. [Google Scholar] [CrossRef]
- Arfah, A.; Yusuf, S.; Syam, Y. The Role of Textiles in Controlling Microclimate to Prevent Pressure Injury. Media Keperawatan Indones. 2020, 3, 81. [Google Scholar] [CrossRef]
- Baskan, A.; Goncu-Berk, G. User Experience of Wearable Technologies: A Comparative Analysis of Textile-Based and Accessory-Based Wearable Products. Appl. Sci. 2022, 12, 11154. [Google Scholar] [CrossRef]
- Kan, C.-W.; Lam, Y.-L. Future Trend in Wearable Electronics in the Textile Industry. Appl. Sci. 2021, 11, 3914. [Google Scholar] [CrossRef]
- Brickwood, K.-J.; Watson, G.; O’Brien, J.; Williams, A.D. Consumer-Based Wearable Activity Trackers Increase Physical Activity Participation: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2019, 7, e11819. [Google Scholar] [CrossRef]
- Lee, E.; Roh, J.-S.; Kim, S. User-Centered Interface Design Approach for a Smart Heated Garment. Fibers Polym. 2018, 19, 238–247. [Google Scholar] [CrossRef]
- Caporaso, T.; Grazioso, S.; Di Gironimo, G.; Lanzotti, A. Design of Wearables for Biosignal Acquisition: A User Centered Approach for Concept Generation and Selection. In International Conference on Design, Simulation, Manufacturing: The Innovation Exchange; Rizzi, C., Campana, F., Bici, M., Gherardini, F., Ingrassia, T., Cicconi, P., Eds.; Springer International Publishing: Cham, Switzerland, 2022; pp. 818–826. [Google Scholar]
- Rêgo, A.S.; Filipe, L.; Dias, R.A.; Alves, F.S.; Queiroz, J.; Ainla, A.; Arruda, L.M.; Fangueiro, R.; Bouçanova, M.; Bernardes, R.A.; et al. End-User Assessment of an Innovative Clothing-Based Sensor Developed for Pressure Injury Prevention: A Mixed-Method Study. Int. J. Environ. Res. Public Health 2023, 20, 4039. [Google Scholar] [CrossRef]
- McBee-Black, K. Making Life Easier: A Case Study Exploring the Development of Adaptive Apparel Design Innovations from a User-Centered Approach. Fash. Pract. 2022, 14, 203–224. [Google Scholar] [CrossRef]
- Barboza, R.; Arruda, L.M.; Carvalho, M.A.; Fangueiro, R.; Salgueiro, A.; Parreira, P.; Sousa, L. Required Attributes of a Smart Clothing for Pressure Ulcers Prevention. J. Biomim. Biomater. Biomed. Eng. 2022, 57, 27–36. [Google Scholar] [CrossRef]
- Rêgo, A.D.S.; Furtado, G.E.; Bernardes, R.A.; Santos-Costa, P.; Dias, R.A.; Alves, F.S.; Ainla, A.; Arruda, L.M.; Moreira, I.P.; Bessa, J.; et al. Development of Smart Clothing to Prevent Pressure Injuries in Bedridden Persons and/or with Severely Impaired Mobility: 4NoPressure Research Protocol. Healthcare 2023, 11, 1361. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, V.; Ugur, S. Designing Wearable Technologies through a User Centered Approach. In Proceedings of the 2011 Conference on Designing Pleasurable Products and Interfaces, Milano, Italy, 22–25 June 2011; Association for Computing Machinery: New York, NY, USA, 2011; pp. 1–8. [Google Scholar]
- Aileni, R.M.; Pasca, S.; Valderrama, C.A.; Strungaru, R. Wearable Health Care: Technology Evolution, Algorithms and Needs. In Enhanced Living Environments: From Models to Technologies; Goleva, R.I., Ganchev, I., Dobre, C., Garcia, N., Valderrama, C., Eds.; Institution of Engineering and Technology: London, UK, 2017; pp. 315–343. ISBN 9781785612114. [Google Scholar]
- Francés-Morcillo, L.; Morer-Camo, P.; Rodríguez-Ferradas, M.I.; Cazón-Martín, A. Wearable Design Requirements Identification and Evaluation. Sensors 2020, 20, 2599. [Google Scholar] [CrossRef]
- Scataglini, S.; Danckaers, F.; Huysmans, T.; Sijbers, J.; Andreoni, G. Chapter 53—Design Smart Clothing Using Digital Human Models. In DHM and Posturography; Scataglini, S., Paul, G., Eds.; Academic Press: Cambridge, MA, USA, 2019; pp. 683–698. ISBN 9780128167137. [Google Scholar]
- Tahri Sqalli, M.; Al-Thani, D. Evolution of Wearable Devices in Health Coaching: Challenges and Opportunities. Front. Digit. Health 2020, 2, 545646. [Google Scholar] [CrossRef]
- Hong, Q.N.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; O’Cathain, A.; et al. The Mixed Methods Appraisal Tool (MMAT) Version 2018 for Information Professionals and Researchers. Educ. Inf. 2018, 34, 285–291. [Google Scholar] [CrossRef]
- Kim, E.; Simonse, L.W.L.; Beckman, S.L.; Appleyard, M.M.; Velazquez, H.; Madrigal, A.S.; Agogino, A.M. User-Centered Design Roadmapping: Anchoring Roadmapping in Customer Value Before Technology Selection. IEEE Trans. Eng. Manag. 2022, 69, 109–126. [Google Scholar] [CrossRef]
- Rogers, E.M. Diffusion of Innovations, 5th ed.; Free Press: New York, NY, USA, 2003; ISBN 9780743222099. [Google Scholar]
- Farao, J.; Malila, B.; Conrad, N.; Mutsvangwa, T.; Rangaka, M.X.; Douglas, T.S. A User-Centred Design Framework for mHealth. PLoS ONE 2020, 15, e0237910. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Jin, H. Conceptual Design Framework as a Model for Wheelchair Users’ Sportswear Comfort. Fash. Text. 2019, 6, 23. [Google Scholar] [CrossRef]
- Han, M.; Lee, J.; Kim, J.K.; An, H.K.; Kang, S.W.; Jung, D. Highly sensitive and flexible wearable pressure sensor with dielectric elastomer and carbon nanotube electrodes. Sens. Actuators A Phys. 2020, 305, 111941. [Google Scholar] [CrossRef]
- Jansen-Kosterink, S.; Broekhuis, M.; van Velsen, L. Time to act mature—Gearing eHealth evaluations towards technology readiness levels. Digit. Health 2022, 8, 205520762211133. [Google Scholar] [CrossRef]
- Webster, A.; Gardner, J. Aligning Technology and Institutional Readiness: The Adoption of Innovation. Technol. Anal. Strateg. Manag. 2019, 31, 1229–1241. [Google Scholar] [CrossRef]
- Olechowski, A.L.; Eppinger, S.D.; Joglekar, N.; Tomaschek, K. Technology readiness levels: Shortcomings and improvement opportunities. Syst. Eng. 2020, 23, 395–408. [Google Scholar] [CrossRef]
- Mankins, J.C. Technology Readiness Levels: A White Paper. 1995. Available online: http://www.hq.nasa.gov/office/codeq/trl/trl.pdf (accessed on 1 June 2022).
- Laing, R.M.; Sleivert, G.G. Clothing, textiles, and human performance. Text. Prog. 2002, 32, 1–122. [Google Scholar] [CrossRef]
- Digital Human Modeling. Applications in Health, Safety, Ergonomics, and Risk Management: Ergonomics and Design. In Proceedings of the 8th International Conference, DHM 2017, Held as Part of HCI International 2017, Vancouver, BC, Canada, 9–14 July 2017; Proceedings, Part I. Duffy, V.G., Ed.; Information Systems and Applications, incl. Internet/Web, and HCI; 1st ed. 2017;. Springer International Publishing: Cham, Switzerland, 2017. ISBN 9783319584638. [Google Scholar]
- Nakagawa, H.; Mori, K.; Takahashi, K.; Yamashiro, K.; Ogura, Y.; Goto, A. The Motion Analysis of Transferring from Bed to Wheelchair Conducted in the Nursing Field with Focusing on the Body Pressure Distribution. In Digital Human Modeling. Applications in Health, Safety, Ergonomics, and Risk Management: Ergonomics and Design; Duffy, V.G., Ed.; Springer International Publishing: Cham, Switzerland, 2017; Volume 10286, pp. 141–159. ISBN 9783319584621. [Google Scholar]
- Ulrich, R.S.; Zimring, C.; Zhu, X.; DuBose, J.; Seo, H.-B.; Choi, Y.-S.; Quan, X.; Joseph, A. A Review of the Research Literature on Evidence-Based Healthcare Design. Health Environ. Res. Des. J. 2008, 1, 61–125. [Google Scholar] [CrossRef]
- Baby, R.; Mathur, K.; DenHartog, E. Skin-Textiles Friction: Importance and Prospects in Skin Comfort and in Healthcare in Prevention of Skin Injuries. J. Text. Inst. 2021, 112, 1514–1530. [Google Scholar] [CrossRef]
- Vilhena, L.; Ramalho, A. Friction of Human Skin against Different Fabrics for Medical Use. Lubricants 2016, 4, 6. [Google Scholar] [CrossRef]
- Shishoo, R.L. Importance of Mechanical and Physical Properties of Fabrics in the Clothing Manufacturing Process. Int. J. Cloth. Sci. Technol. 1995, 7, 35–42. [Google Scholar] [CrossRef]
- Koncar, V. Smart Textiles for in Situ Monitoring of Composites; The Textile Institute Book Series; Woodhead Publishing, an imprint of Elsevier: Duxford, UK; Cambridge, MA, USA, 2019; ISBN 9780081023082. [Google Scholar]
- Ismar, E.; Kurşun Bahadir, S.; Kalaoglu, F.; Koncar, V. Futuristic Clothes: Electronic Textiles and Wearable Technologies. Glob. Chall. 2020, 4, 1900092. [Google Scholar] [CrossRef]
- Watel, Q.; Cochrane, C.; Boussu, F. Local Measurement of Dynamic Strain of Impacted Woven Structure. Sens. Actuators A Phys. 2021, 332, 113159. [Google Scholar] [CrossRef]
- Huang, S.; Huang, L. CLO3D-Based 3D Virtual Fitting Technology of Down Jacket and Simulation Research on Dynamic Effect of Cloth. Wirel. Commun. Mob. Comput. 2022, 2022, e5835026. [Google Scholar] [CrossRef]
- Choi, K.-H. 3D Dynamic Fashion Design Development Using Digital Technology and Its Potential in Online Platforms. Fash. Text. 2022, 9, 9. [Google Scholar] [CrossRef]
- Moniruzzaman, M.D.; Rita, A.A.; Oishe, S.H. An Approach to Design Solutions for Garments Using a CAD System. J. Text. Eng. Fash. Technol. 2022, 8, 145–148. [Google Scholar] [CrossRef]
- Pei, J. The Production System of Mass Customization Using 3D Body Scanning Technology. In Digital Manufacturing Technology for Sustainable Anthropometric Apparel; Elsevier: Amsterdam, The Netherlands, 2022; pp. 185–209. ISBN 9780128239698. [Google Scholar]
- Papachristou, E.; Anastassiu, H.T. Application of 3D Virtual Prototyping Technology to the Integration of Wearable Antennas into Fashion Garments. Technologies 2022, 10, 62. [Google Scholar] [CrossRef]
- Vadicherla, T.; Saravanan, D. Textiles and Apparel Development Using Recycled and Reclaimed Fibers. In Roadmap to Sustainable Textiles and Clothing; Muthu, S.S., Ed.; Springer: Singapore, 2014; pp. 139–160. ISBN 9789812870643. [Google Scholar]
- Harmsen, P.; Scheffer, M.; Bos, H. Textiles for Circular Fashion: The Logic behind Recycling Options. Sustainability 2021, 13, 9714. [Google Scholar] [CrossRef]
- Luu, T.T.A.; Baker, J.R. Exploring Consumers’ Purchase Intention of rPET Bottle-Based Apparel in an Emerging Economy. J. Open Innov. Technol. Mark. Complex. 2021, 7, 22. [Google Scholar] [CrossRef]
- Avadanei, M.L.; Olaru, S.; Dulgheriu, I.; Ionesi, S.D.; Loghin, E.C.; Ionescu, I. A New Approach to Dynamic Anthropometry for the Ergonomic Design of a Fashionable Personalised Garment. Sustainability 2022, 14, 7602. [Google Scholar] [CrossRef]
- Sousa, L.B.; Santos-Costa, P.; Marques, I.A.; Cruz, A.; Salgueiro-Oliveira, A.; Parreira, P. Brief Report on Double-Chamber Syringes Patents and Implications for Infusion Therapy Safety and Efficiency. Int. J. Environ. Res. Public Health 2020, 17, 8209. [Google Scholar] [CrossRef] [PubMed]
- Parreira, P.; Sousa, L.B.; Marques, I.A.; Santos-Costa, P.; Braga, L.M.; Cruz, A.; Salgueiro-Oliveira, A. Double-Chamber Syringe versus Classic Syringes for Peripheral Intravenous Drug Administration and Catheter Flushing: A Study Protocol for a Randomised Controlled Trial. Trials 2020, 21, 78. [Google Scholar] [CrossRef]
- Parreira, P.; Sousa, L.B.; Marques, I.A.; Costa, P.; Cortez, S.; Carneiro, F.; Cruz, A.; Salgueiro-Oliveira, A. Development of an Innovative Double-Chamber Syringe for Intravenous Therapeutics and Flushing: Nurses’ Involvement through a Human-Centred Approach. PLoS ONE 2020, 15, e0235087. [Google Scholar] [CrossRef]
- Bernardes, R.; Parreira, P.; Salgueiro-Oliveira, A.; Cruz, A. Funcionalidade e aprendizagem de um dispositivo de reabilitação para doentes pós-enfarte: Perspetiva de enfermeiros de reabilitação. Rev. Enferm. Ref. 2022, 6, e21032. [Google Scholar] [CrossRef]
- Parreira, P.; Sousa, L.B.; Marques, I.A.; Santos-Costa, P.; Cortez, S.; Carneiro, F.; Cruz, A.; Salgueiro-Oliveira, A. Usability Assessment of an Innovative Device in Infusion Therapy: A Mix-Method Approach Study. Int. J. Environ. Res. Public Health 2020, 17, 8335. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, A.B.; Finley, E.P. Qualitative Methods in Implementation Research: An Introduction. Psychiatry Res. 2019, 280, 112516. [Google Scholar] [CrossRef] [PubMed]
- Roulston, K. Reflective Interviewing: A Guide to Theory and Practice; SAGE Publications Ltd.: New York, NY, USA, 2010; pp. 1–216. [Google Scholar]
- De Minayo, M.C.S. Análise qualitativa: Teoria, passos e fidedignidade. Ciência Saúde Coletiva 2012, 17, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, J.L.G.; Erdmann, A.L.; Meirelles, B.H.S.; de Melo Lanzoni, G.M.; da Cunha, V.P.; Ross, R. Integração entre dados quantitativos e qualitativos em uma pesquisa de métodos mistos. Texto Contexto-Enferm. 2017, 26, e1590016. [Google Scholar] [CrossRef]
- Qi, W.; Zhou, L. User-Centered Wearable Product Design for Community Elderly Care. In Proceedings of the 2019 12th International Congress on Image and Signal Processing, BioMedical Engineering and Informatics (CISP-BMEI), Suzhou, China, 19–21 October 2019; pp. 1–5. [Google Scholar]
- Wu, D.; Bian, F.; Wang, Y. A Method for the Evaluation of Functional Clothing for Older Individuals with Restricted Mobility. Fash. Pract. 2021, 13, 113–127. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, D.; Zhao, M.; Li, J. Evaluation on an Ergonomic Design of Functional Clothing for Wheelchair Users. Appl. Ergon. 2014, 45, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Esmail, A.; Poncet, F.; Auger, C.; Rochette, A.; Dahan-Oliel, N.; Labbé, D.; Kehayia, E.; Billebaud, C.; De Guise, É.; Lessard, I.; et al. The Role of Clothing on Participation of Persons with a Physical Disability: A Scoping Review. Appl. Ergon. 2020, 85, 103058. [Google Scholar] [CrossRef] [PubMed]
- Luna-Perejón, F.; Muñoz-Saavedra, L.; Castellano-Domínguez, J.M.; Domínguez-Morales, M. IoT Garment for Remote Elderly Care Network. Biomed. Signal Process. Control. 2021, 69, 102848. [Google Scholar] [CrossRef] [PubMed]
- Barakat-Johnson, M.; Lai, M.; Wand, T.; White, K. A Qualitative Study of the Thoughts and Experiences of Hospital Nurses Providing Pressure Injury Prevention and Management. Collegian 2019, 26, 95–102. [Google Scholar] [CrossRef]
- Sprigle, S.; McNair, D.; Sonenblum, S. Pressure Ulcer Risk Factors in Persons with Mobility-Related Disabilities. Adv. Ski. Wound Care 2020, 33, 146–154. [Google Scholar] [CrossRef] [PubMed]
- Bader, D.L.; Worsley, P.R.; Gefen, A. Bioengineering Considerations in the Prevention of Medical Device-Related Pressure Ulcers. Clin. Biomech. 2019, 67, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Silveira, I. Usabilidade Do Vestuário: Fatores Técnicos/Funcionais. ModaPalavra 2008, 1, 21–39. [Google Scholar] [CrossRef]
- Marteli, L.N.; Paschoarelli, L.C.; Da Silva, F.M.; Trigueiros, P.; Barbieri, F.A. Case Study on the Experience and Perception of Rehabilitators and Caregivers of People with Parkinson’s Disease in the Interaction with Clothing Assistive Devices: Narratives About Everyday Problems, in Portugal. In Advances in Design and Digital Communication II; Martins, N., Brandão, D., Eds.; Springer International Publishing: Cham, Switzerland, 2022; Volume 19, pp. 412–424. ISBN 9783030897345. [Google Scholar]
- Perdomo Delgado, C.N.; Nardoni Marteli, L.; Vizioli Libório, F.H.; Paschoarelli, L.C.; Orsi Mendola, F. Evaluación de La Percepción de Usabilidad, Calidad y Estética de La Cuchara Adaptada. Rev. Chil. Ter. Ocup. 2020, 20, 179. [Google Scholar] [CrossRef]
- Neves, E.P.; Marteli, L.N.; Paschoarelli, L.C. Elderly and Clothing: Considerations about Handling Trimmings. Curr. Trends Fash. Technol. Text. Eng. 2018, 2, 12–14. [Google Scholar] [CrossRef]
- Marteli, L.N.; Paschoarelli, L.C. Older person with Parkinson’s disease and aspects of usability in the interaction with clothing fasteners. Geriatr. Gerontol. Aging 2019, 13, 57–58. [Google Scholar] [CrossRef]
- Youn, S.; Lee, K.-H. Proposing Value-Based Technology Acceptance Model: Testing on Paid Mobile Media Service. Fash. Text. 2019, 6, 13. [Google Scholar] [CrossRef]
- Ju, N.; Lee, K.-H. Consumer Resistance to Innovation: Smart Clothing. Fash. Text. 2020, 7, 21. [Google Scholar] [CrossRef]
- Nardoni Marteli, L.; Alves, A.L.; Trigueiros, P.; Moreira Da Silva, F.; Paschoarelli, L.C. Perception About Usability and Consumption Aspects of Clothing Products by Elderlies with Parkinson’s Disease: A Preliminary Study in Brazil. In Advances in Fashion and Design Research; Broega, A.C., Cunha, J., Carvalho, H., Providência, B., Eds.; Springer International Publishing: Cham, Switzerland, 2023; pp. 258–267. ISBN 9783031167720. [Google Scholar]
- Gao, Y.; Li, H.; Luo, Y. An Empirical Study of Wearable Technology Acceptance in Healthcare. Ind. Manag. Data Syst. 2015, 115, 1704–1723. [Google Scholar] [CrossRef]
- Mahmood, N.; Lee, Y. Factors Influencing Older Adults’ Acceptance of Health Monitoring Smart Clothing. Fam. Consum. Sci. Res. J. 2021, 49, 376–392. [Google Scholar] [CrossRef]
- Keikhosrokiani, P.; Mustaffa, N.; Zakaria, N. Success Factors in Developing IHeart as a Patient-Centric Healthcare System: A Multi-Group Analysis. Telemat. Inform. 2018, 35, 753–775. [Google Scholar] [CrossRef]
- Niknejad, N.; Hussin, A.R.C.; Ghani, I.; Ganjouei, F.A. A Confirmatory Factor Analysis of the Behavioral Intention to Use Smart Wellness Wearables in Malaysia. Univers. Access Inf. Soc. 2020, 19, 633–653. [Google Scholar] [CrossRef]
- Ashby, N.; Jake LaPorte, G.; Richardson, D.; Scioletti, M.; Heymsfield, S.B.; Shepherd, J.A.; McGurk, M.; Bustillos, B.; Gist, N.; Thomas, D.M. Translating Digital Anthropometry Measurements Obtained from Different 3D Body Image Scanners. Eur. J. Clin. Nutr. 2023, 77, 872–880. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Tao, X.; Zeng, X.; Xing, Y.; Xu, Z.; Bruniaux, P. A Machine Learning-Enhanced 3D Reverse Design Approach to Personalized Garments in Pursuit of Sustainability. Sustainability 2023, 15, 6235. [Google Scholar] [CrossRef]


| Variables Evaluated | N | % |
|---|---|---|
| Gender | ||
| Male | 9 | 47.4 |
| Female | 10 | 52.6 |
| Nursing Education | ||
| Degree | 5 | 26.3 |
| Post-graduation/Specialization | 5 | 26.3 |
| Master’s Degree | 7 | 36.8 |
| Doctoral Degree | 2 | 10.5 |
| Clinical practice area | ||
| Medical areas | 15 | 78.9 |
| Surgical areas | 4 | 21.1 |
| M ± SD | CI 95% | |
| Age (in years) | 35.36 ± 9.68 | 30.70–40.03 |
| Professional experience—overall (in years) | 12.31 ± 8.96 | 7.99–16.63 |
| Professional experience in the current ward (in years) | 7.15 ± 8.61 | 3.00–11.31 |
| Quantitative Assessment | Qualitative Assessment | ||
|---|---|---|---|
| Variables Evaluated | MD | CI 95% | Statements |
| Utility | 4.0 | 3.03–4.55 | “The push buttons do not facilitate the exchange that I think it could be, maybe the goal that is to facilitate, no, but it makes sense these push buttons, it confuses at the time of dressing. […]” (Participant 01). “The locking system could be push ped on the simpler push, manipulated and fewer push. The other choice is to create a form of fasteners. The push buttons are too hard; this is not comfortable and will not make it easier to use […]” (Participant 12). “I don’t find the pants cuff adequate; without the cuff, it would make it easier to close, stitch closure through the opening. The push buttons are too many, it’s not practical. These push buttons do not help […]” (Participant 16). |
| It is useful for my work | 4.0 | 3.20–4.75 | |
| It facilitates the performance of my task | 4.0 | 3.15–4.70 | |
| It allows me to be more effective/complete the task effectively | 3.0 | 3.05–4.40 | |
| It allows me to be more efficient/complete the task efficiently | 3.0 | 3.10–4.50 | |
| It meets the expected to respond to my task | 4.0 | 3.25–4.55 | |
| It allows me to complete the task | 3.0 | 3.45–3.75 | |
| It allows me to complete the task easily | 4.0 | 2.85–4.29 | |
| It allows me to complete the task quickly | 3.0 | 2.55–4.05 | |
| It allows me greater control over the task to be performed | 4.0 | 3.55–4.75 | |
| It helps me be more productive in my work | 3.0 | 3.00–3.39 | |
| It allows me to ensure more safety for the patient | 4.0 | 3.20–4.90 | |
| It allows me to respond to my needs | 3.0 | 2.85–4.30 | |
| Quantitative Assessment | Qualitative Assessment | ||
|---|---|---|---|
| Variables Evaluated | MD | CI 95% | Statements |
| Ease of use | 3.0 | 3.02–4.34 | “The push buttons are too many; it’s not practical. These pushes don’t help […]” (Participant 05). “The push buttons have already made it clear that they are too many and hard; it does not facilitate the use […]” (Participant 16). “Push buttons laterally to be able to open and have access to the front and back of the wearer would be interesting, the lateral opening should be whole. But there are too many push buttons […]” (Participant 10). |
| It is easy to use | 3.0 | 2.60–3.95 | |
| It is simple to use | 3.0 | 2.50–3.90 | |
| It is user-friendly | 3.0 | 2.70–4.20 | |
| It requires few manipulations to achieve what is intended | 3.0 | 2.25–3.80 | |
| It allows flexible use according to my needs | 4.0 | 2.80–4.39 | |
| It does not require much physical effort in its use | 4.0 | 2.80–4.39 | |
| It does not require much mental effort in its use | 4.0 | 3.55–4.79 | |
| It allows me to conduct tasks in a logical and consistent sequence | 4.0 | 3.55–4.79 | |
| It is not associated with great possibilities of error in its use | 3.0 | 3.15–4.50 | |
| It allows me to correct any errors quickly and easily | 5.0 | 4.05–5.20 |
| Quantitative Assessment | Qualitative Assessment | ||
|---|---|---|---|
| Variables Evaluated | MD | CI 95% | Statements |
| Ease of learning | 5.0 | 4.35–5.57 | “That opening in the knee doesn’t make sense—for example, a knee wound. Regardless of the situation that occurred at the time, being bad and we must open everything, but the opening goes only to the knee […]” (Participant 02). “The push buttons, where we must put in and take out with force. It needs a manipulation that demands time […]” (Participant 10). “The push buttons, I have already made it clear that they are many and hard, it does not facilitate when dressing, it is confusing […]” (Participant 02). |
| You quickly learn to use it | 5.0 | 4.20–5.40 | |
| You can easily learn to use it | 5.0 | 4.10–5.35 | |
| I quickly remembered how to use it | 6.0 | 4.80–5.85 | |
| I quickly became skilled at using it | 5.0 | 4.10–5.55 | |
| It does not take much prior knowledge to use it | 5.0 | 4.65–5.75 | |
| No written instructions are needed to use it | 5.0 | 4.05–5.40 |
| Quantitative Assessment | Qualitative Assessment | ||
|---|---|---|---|
| Variables Evaluated | MD | CI 95% | Statements |
| I would be satisfied | 4.0 | 3.20–4.55 | “When you lateralize the patient, you have an area that increases the pressure, and that opening is not good, or when it is in dorsal, I run the risk of hurting, I am thinking about the lateral push buttons […]” (Participant 4). The push buttons could have more space and be more malleable because I think it’s important not to be hard, not so hard. The push buttons would interfere with the safety of the user himself […]” (Participant 13). “Then, if you level up specifically the issue of spacing the push buttons. The push buttons could have more spacing and be more pliable because I think it’s important not to be hard, not to be so hard. The push buttons would interfere with the user’s own safety […]” (Participant 19). |
| I would recommend it to colleagues | 4.0 | 3.10–4.45 | |
| It would allow me to perform the tasks I want | 4.0 | 2.95–4.34 | |
| It would be interesting for the performance of my tasks | 4.0 | 3.20–4.65 | |
| I would need to have it in my clinical practice | 3.0 | 2.70–4.35 | |
| It would be pleasant to use | 4.0 | 3.05–4.90 | |
| I would be comfortable with its use | 4.0 | 3.50–4.70 | |
| I would feel confident with its use | 4.0 | 3.40–4.60 | |
| It would give me security in its use | 4.0 | 3.30–4.65 | |
| The dimensions of the device are adequate | 5.0 | 3.90–5.35 | |
| The weight of the device is adequate | 6.0 | 4.80–6.10 | |
| Appearance is adjusted | 5.0 | 4.35–5.75 | |
| I would like to use it often | 4.0 | 3.55–4.80 | |
| It would be easy to adjust it for the performance of my tasks | 4.0 | 3.45–4.85 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salgueiro-Oliveira, A.; Rêgo, A.d.S.; Santos-Costa, P.; Bernardes, R.A.; Filipe, L.; Sousa, L.B.; Barboza, R.; Carvalho, M.; Bouçanova, M.; Lopes, M.C.F.d.G.; et al. Design of Innovative Clothing for Pressure Injury Prevention: End-User Evaluation in a Mixed-Methods Study. Int. J. Environ. Res. Public Health 2023, 20, 6773. https://doi.org/10.3390/ijerph20186773
Salgueiro-Oliveira A, Rêgo AdS, Santos-Costa P, Bernardes RA, Filipe L, Sousa LB, Barboza R, Carvalho M, Bouçanova M, Lopes MCFdG, et al. Design of Innovative Clothing for Pressure Injury Prevention: End-User Evaluation in a Mixed-Methods Study. International Journal of Environmental Research and Public Health. 2023; 20(18):6773. https://doi.org/10.3390/ijerph20186773
Chicago/Turabian StyleSalgueiro-Oliveira, Anabela, Anderson da Silva Rêgo, Paulo Santos-Costa, Rafael A. Bernardes, Luísa Filipe, Liliana B. Sousa, Rochelne Barboza, Miguel Carvalho, Maria Bouçanova, Maria Clara Ferreira da Graça Lopes, and et al. 2023. "Design of Innovative Clothing for Pressure Injury Prevention: End-User Evaluation in a Mixed-Methods Study" International Journal of Environmental Research and Public Health 20, no. 18: 6773. https://doi.org/10.3390/ijerph20186773
APA StyleSalgueiro-Oliveira, A., Rêgo, A. d. S., Santos-Costa, P., Bernardes, R. A., Filipe, L., Sousa, L. B., Barboza, R., Carvalho, M., Bouçanova, M., Lopes, M. C. F. d. G., Apóstolo, J. A., & Parreira, P. (2023). Design of Innovative Clothing for Pressure Injury Prevention: End-User Evaluation in a Mixed-Methods Study. International Journal of Environmental Research and Public Health, 20(18), 6773. https://doi.org/10.3390/ijerph20186773











