Neighborhood Social Environment and Body Mass Index: The Mediating Role of Mental Wellbeing
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Measures
2.2.1. Body Mass Index (BMI)
2.2.2. Physical Activity
2.2.3. Mental Wellbeing
2.2.4. Neighborhood Social Environment
2.2.5. Neighborhood Built Environment
2.2.6. Control Variables
2.3. Data Analysis
Var(Ei) = error variance associated with the indicator variable
3. Results
3.1. Descriptive Statistics
3.2. Confirmatory Factor Analysis
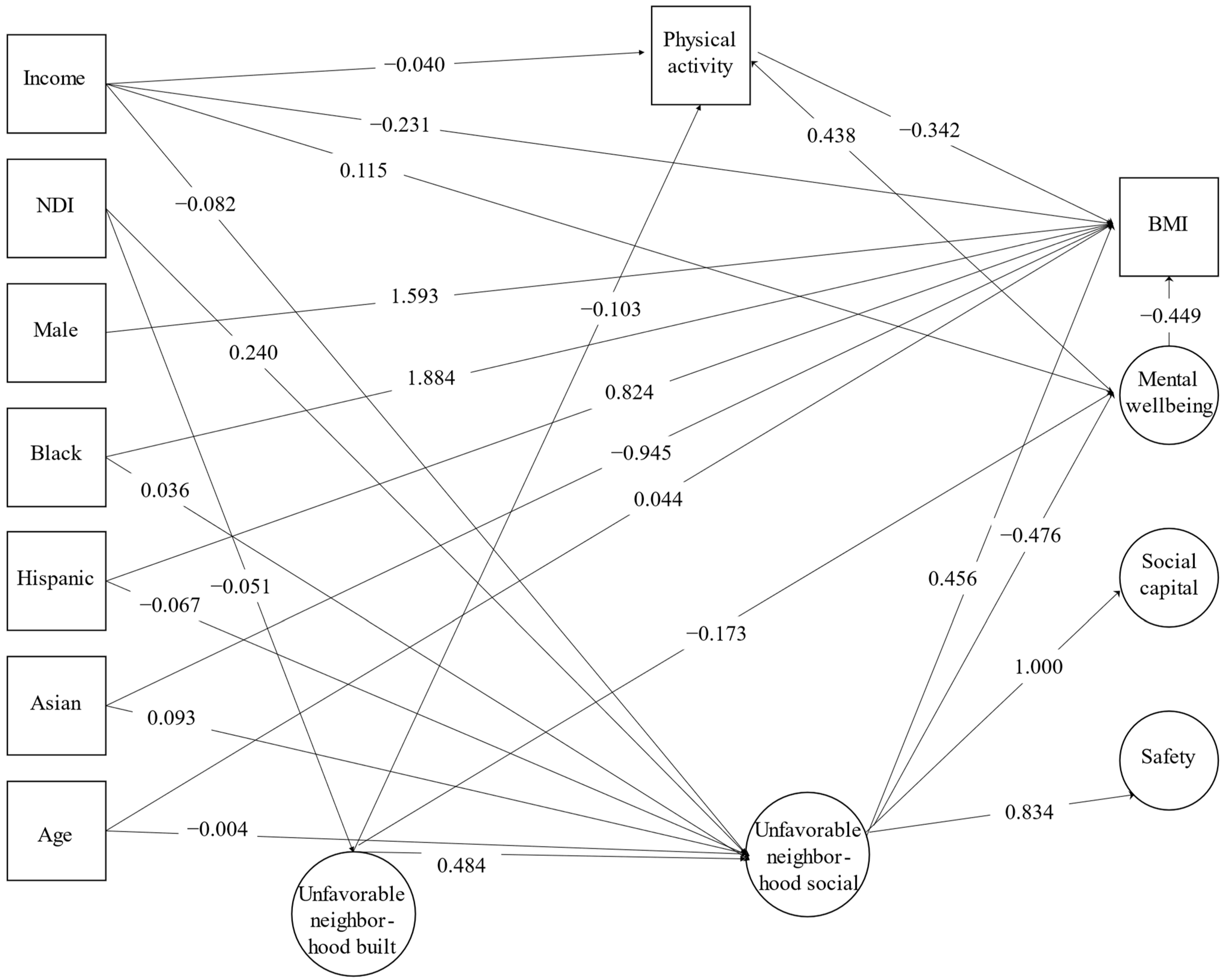
3.3. Structural Model
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diez Roux, A.V.; Mair, C. Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef] [PubMed]
- Leal, C.; Chaix, B. The influence of geographic life environments on cardiometabolic risk factors: A systematic review, a methodological assessment and a research agenda. Obes. Rev. 2011, 12, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.D.; Lakerveld, J.; van Lenthe, F.J.; Kawachi, I.; McKee, M.; Rutter, H.; Glonti, K.; Compernolle, S.; De Bourdeaudhuij, I.; Feuillet, T.; et al. Neighbourhood social capital: Measurement issues and associations with health outcomes. Obes. Rev. 2016, 17, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Cobb, L.K.; Appel, L.J.; Franco, M.; Jones-Smith, J.C.; Nur, A.; Anderson, C.A.M. The relationship of the local food environment with obesity: A systematic review of methods, study quality, and results. Obesity 2015, 23, 1331–1344. [Google Scholar] [CrossRef]
- Kim, J.; Lee, S.; Ramos, W. Investigating the relationship between accessibility of green space and adult obesity rates: A secondary data analysis in the United States. J. Prev. Med. Public. Health 2021, 54, 208–217. [Google Scholar] [CrossRef]
- Ziso, D.; Chun, O.K.; Puglisi, M.J. Increasing access to healthy foods through improving food environment: A review of mixed methods intervention studies with residents of low-income communities. Nutrients 2022, 14, 2278. [Google Scholar] [CrossRef]
- Suglia, S.F.; Shelton, R.C.; Hsiao, A.; Wang, Y.C.; Rundle, A.; Link, B.G. Why the neighborhood social environment is critical in obesity prevention. J. Urban. Health 2016, 93, 206–212. [Google Scholar] [CrossRef]
- Cohen, D.A.; Finch, B.K.; Bower, A.; Sastry, N. Collective efficacy and obesity: The potential influence of social factors on health. Soc. Sci. Med. 2006, 62, 769–778. [Google Scholar] [CrossRef]
- Booth, K.M.; Pinkston, M.M.; Poston, W.S.C. Obesity and the built environment. J. Am. Diet. Assoc. 2005, 105, 110–117. [Google Scholar] [CrossRef]
- Kim, D.; Subramanian, S.V.; Gortmaker, S.L.; Kawachi, I. US state- and county-level social capital in relation to obesity and physical inactivity: A multilevel, multivariable analysis. Soc. Sci. Med. 2006, 63, 1045–1059. [Google Scholar] [CrossRef]
- Bennett, G.G.; McNeill, L.H.; Wolin, K.Y.; Duncan, D.T.; Puleo, E.; Emmons, K.M. Safe to walk? Neighborhood safety and physical activity among public housing residents. PLoS Med. 2007, 4, e306. [Google Scholar] [CrossRef]
- Quinn, T.D.; Wu, F.; Mody, D.; Bushover, B.; Mendez, D.D.; Schiff, M.; Fabio, A. Associations between neighborhood social cohesion and physical activity in the United States, National Health Interview Survey, 2017. Prev. Chronic. Dis. 2019, 16, 190085. [Google Scholar] [CrossRef]
- Kepper, M.M.; Myers, C.A.; Denstel, K.D.; Hunter, R.F.; Guan, W.; Broyles, S.T. The neighborhood social environment and physical activity: A systematic scoping review. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 124. [Google Scholar] [CrossRef] [PubMed]
- McNeill, L.H.; Kreuter, M.W.; Subramanian, S.V. Social Environment and Physical activity: A review of concepts and evidence. Soc. Sci. Med. 2006, 63, 1011–1022. [Google Scholar] [CrossRef] [PubMed]
- Stafford, M.; Cummins, S.; Ellaway, A.; Sacker, A.; Wiggins, R.D.; Macintyre, S. Pathways to obesity: Identifying local, modifiable determinants of physical activity and diet. Soc. Sci. Med. 2007, 65, 1882–1897. [Google Scholar] [CrossRef]
- Fish, J.S.; Ettner, S.; Ang, A.; Brown, A.F. Association of perceived neighborhood safety with [corrected] body mass index. Am. J. Public Health 2010, 100, 2296–2303. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Álvarez, E.; Kawachi, I.; Riera-Romaní, J. Neighbourhood social capital and obesity: A systematic review of the literature. Obes. Rev. 2019, 20, 119–141. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Cardel, M.; Donahoo, W.T. Social and Environmental Factors Influencing Obesity. [Updated 2019 Oct 12]. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Blackman, M.R., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK278977/ (accessed on 8 August 2023).
- Lam, T.M.; Vaartjes, I.; Grobbee, D.E.; Karssenberg, D.; Lakerveld, J. Associations between the built environment and obesity: An umbrella review. Int. J. Health Geogr. 2021, 20, 7. [Google Scholar] [CrossRef]
- Kim, D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiol. Rev. 2008, 30, 101–117. [Google Scholar] [CrossRef]
- Mair, C.; Diez Roux, A.V.; Galea, S. Are neighborhood characteristics associated with depressive symptoms? A critical review. J. Epidemiol. Community Health 2008, 62, 940–946. [Google Scholar] [CrossRef]
- Ottino-González, J.; Jurado, M.A.; García-García, I.; Segura, B.; Marqués-Iturria, I.; Sender-Palacios, M.J.; Tor, E.; Prats-Soteras, X.; Caldú, X.; Junqué, C.; et al. Allostatic load and disordered white matter microstructure in overweight adults. Sci. Rep. 2018, 8, 15898. [Google Scholar] [CrossRef] [PubMed]
- Ahern, J.; Galea, S. Collective efficacy and major depression in urban neighborhoods. Am. J. Epidemiol. 2011, 173, 1453–1462. [Google Scholar] [CrossRef] [PubMed]
- Echeverría, S.; Diez-Roux, A.V.; Shea, S.; Borrell, L.N.; Jackson, S. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The Multi-Ethnic Study of Atherosclerosis. Health Place 2008, 14, 853–865. [Google Scholar] [CrossRef] [PubMed]
- Rios, R.; Aiken, L.S.; Zautra, A.J. Neighborhood contexts and the mediating role of neighborhood social cohesion on health and psychological distress among hispanic and non-hispanic residents. Ann. Behav. Med. 2012, 43, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Luppino, F.S.; van Reedt Dortland, A.K.B.; Wardenaar, K.J.; Wardenaar, K.J.; Bouvy, P.F.; Giltay, E.J.; Zitman, F.G.; Penninx, B.W. Symptom dimensions of depression and anxiety and the metabolic syndrome. Psychosom. Med. 2011, 73, 257–264. [Google Scholar] [CrossRef]
- Mannan, M.; Mamun, A.; Doi, S.; Clavarino, A. Is there a bi-directional relationship between depression and obesity among adult men and women? Systematic review and bias-adjusted meta analysis. Asian J. Psychiatr. 2016, 21, 51–66. [Google Scholar] [CrossRef]
- Avila, C.; Holloway, A.C.; Hahn, M.K.; Morrison, K.M.; Restivo, M.; Anglin, R.; Taylor, V.H. An overview of links between obesity and mental health. Curr. Obes. Rep. 2015, 4, 303–310. [Google Scholar] [CrossRef]
- Romain, K.; Webb, T.; Kumar, M. Depression and obesity: Can the cycle be broken? BJPsych Adv. 2018, 24, 132–140. [Google Scholar] [CrossRef]
- Penninx, B.W.; Milaneschi, Y.; Lamers, F.; Vogelzangs, N. Understanding the somatic consequences of depression: Biological mechanisms and the role of depression symptom profile. BMC Med. 2013, 11, 129. [Google Scholar] [CrossRef]
- Firth, J.; Rosenbaum, S.; Stubbs, B.; Gorczynski, P.; Yung, A.R.; Vancampfort, D. Motivating factors and barriers towards exercise in severe mental illness: A systematic review and meta-analysis. Psychol. Med. 2016, 46, 2869–2881. [Google Scholar] [CrossRef]
- Hiles, S.A.; Lamers, F.; Milaneschi, Y.; Penninx, B.W.J.H. Sit, step, sweat: Longitudinal associations between physical activity patterns, anxiety and depression. Psychol. Med. 2017, 47, 1466–1477. [Google Scholar] [CrossRef] [PubMed]
- DataHaven. DataHaven Community Wellbeing Survey. Available online: https://www.ctdatahaven.org/reports/datahaven-community-wellbeing-survey (accessed on 8 August 2023).
- Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2014.
- Sampson, R.J.; Raudenbush, S.W. Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. Am. J. Sociol. 1999, 105, 603–651. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Slymen, D.J.; Conway, T.L.; Frank, L.D.; Saelens, B.E.; Cain, K.; Chapman, J.E. Income disparities in perceived neighborhood built and social environment attributes. Health Place 2011, 17, 1274–1283. [Google Scholar] [CrossRef]
- Santilli, A.; O’Connor Duffany, K.; Ickovics, J.R. New Haven Health Survey, Findings 2015; Community Alliance for Research and Engagement (CARE), Yale School of Public Health: New Haven, CT, USA, 2016; Available online: http://www.yale.edu/CARE (accessed on 8 August 2023).
- McElroy, E.; McIntyre, J.C.; Bentall, R.P.; Wilson, T.; Holt, K.; Kullu, C.; Nathan, R.; Kerr, A.; Panagaki, K.; McKeown, M.; et al. Mental health, deprivation, and the neighborhood social environment: A network analysis. Clin. Psychol. Sci. 2019, 7, 719–734. [Google Scholar] [CrossRef]
- Stoddard, P.J.; Laraia, B.A.; Warton, E.M.; Moffet, H.H.; Adler, N.E.; Schillinger, D.; Karter, A.J. Neighborhood deprivation and change in bmi among adults with type 2 diabetes. Diabetes Care 2013, 36, 1200–1208. [Google Scholar] [CrossRef]
- Keita, A.D.; Judd, S.E.; Howard, V.J.; Carson, A.P.; Ard, J.D.; Fernandez, J.R. Associations of neighborhood area level deprivation with the metabolic syndrome and inflammation among middle- and older- age adults. BMC Public. Health 2014, 14, 1319. [Google Scholar] [CrossRef]
- Messer, L.C.; Laraia, B.A.; Kaufman, J.S.; Eyster, J.; Holzman, C.; Culhane, J.; Elo, I.; Burke, J.G.; O’Campo, P. The development of a standardized neighborhood deprivation index. J. Urban. Health 2006, 83, 1041–1062. [Google Scholar] [CrossRef]
- United States Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Health Statistics. National Health Interview Survey; National Center for Health Statistics: Hyattsville, MD, USA, 2013.
- United States Census Bureau. “Summary File.” 2007–2011 American Community Survey; U.S. Census Bureau’s American Community Survey Office: Washington, DC, USA, 2013.
- Nunnally, J.C. Psychometric Theory, 2nd ed.; McGraw Hill Book Company: New York, NY, USA, 1987. [Google Scholar]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238–246. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Xia, Y.; Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behav. Res. Methods 2019, 51, 409–428. [Google Scholar] [CrossRef] [PubMed]
- Greenland, S.; Schlesselman, J.J.; Criqui, M.H. The fallacy of employing standardized regression coefficients and correlations as measures of effect. Am. J. Epidemiol. 1986, 123, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Cummings, P. Arguments for and Against Standardized Mean Differences (Effect Sizes). Arch. Pediatr. Adolesc. Med. 2011, 165, 592–596. [Google Scholar] [CrossRef]
- MPLUS. Available online: https://www.statmodel.com/ (accessed on 16 August 2023).
- SAS. Available online: https://www.sas.com (accessed on 16 August 2023).
- American Association for Public Opinion Research. Response Rates—An Overview. Available online: https://www.aapor.org/Education-Resources/For-Researchers/Poll-Survey-FAQ/Response-Rates-An-Overview.aspx (accessed on 13 April 2022).
- Russell-Mayhew, S.; McVey, G.; Bardick, A.; Ireland, A. Mental health, wellness, and childhood overweight/obesity. J. Obes. 2012, 2012, 281801. [Google Scholar] [CrossRef] [PubMed]
- Barrington-Leigh, C.; Wollenberg, J.T. Informing policy priorities using inference from life satisfaction responses in a large community survey. Appl. Res. Qual. Life 2019, 14, 911–924. [Google Scholar] [CrossRef]
- Choi, Y.J.; Matz-Costa, C. Perceived neighborhood safety, social cohesion, and psychological health of older adults. Gerontologist 2018, 58, 196–206. [Google Scholar] [CrossRef]
- Booth, J.; Ayers, S.L.; Marsiglia, F.F. Perceived Neighborhood Safety and Psychological Distress: Exploring Protective Factors. J. Sociol. Soc. Welf. 2012, 39, 8. [Google Scholar] [CrossRef]
- Helliwell, J.F.; Barrington-Leigh, C. How much is social capital worth? In The Social Cure: Identity, Health, and Well-Being; Jetten, J., Haslam, C., Haslam, S.A., Eds.; Taylor and Francis: London, UK, 2011; pp. 55–71. [Google Scholar]
- Takagi, D.; Ikeda, K.; Kawachi, I. Neighborhood social capital and crime victimization: Comparison of spatial regression analysis and hierarchical regression analysis. Soc. Sci. Med. 2012, 75, 1895–1902. [Google Scholar] [CrossRef]
- Robinson, E.; Oldham, M. Weight status misperceptions among UK adults: The use of self-reported vs. measured BMI. BMC Obes. 2016, 3, 21. [Google Scholar] [CrossRef]
- Bray, G.A. Beyond BMI. Nutrients 2023, 15, 2254. [Google Scholar] [CrossRef] [PubMed]
- Curtin, R.; Presser, S.; Singer, E. Changes in telephone survey nonresponse over the past quarter century. Public. Opin. Q. 2005, 69, 87–98. [Google Scholar] [CrossRef]
| Characteristic | Unweighted Mean (SD) or Frequency | Weighted Percent |
|---|---|---|
| Age (years), (range = 18–94) | 57.63 (SD = 17.57) | - |
| Gender | ||
| Female | 9053 | 52.10 |
| Male | 7166 | 47.90 |
| Race | ||
| White | 11,822 | 72.40 |
| Black | 1698 | 8.70 |
| Hispanic | 1463 | 11.30 |
| Asian | 844 | 5.20 |
| American Indian | 392 | 2.40 |
| Income | ||
| Less than $15,000 | 1616 | 10.88 |
| $15,000 to $30,000 | 1999 | 13.64 |
| $30,000 to $50,000 | 2132 | 15.70 |
| $50,000 to $75,000 | 2095 | 16.60 |
| $75,000 to $100,000 | 1667 | 13.86 |
| $100,000 to $200,000 | 2225 | 20.39 |
| $200,000 or more | 1052 | 8.92 |
| Neighborhood Deprivation Index Score, (range = −1.79–4.19) | 0.17 (SD = 1.08) | - |
| Constructs and Indicators | Standardized Factor Loadings | Indicator Reliability | Composite Reliability | Variance Extracted | |
|---|---|---|---|---|---|
| Mental wellbeing | 0.73 | 0.48 | |||
| Overall, how satisfied are you with your life nowadays? | 0.77 | 0.60 | |||
| Overall, how happy did you feel yesterday? | 0.69 | 0.47 | |||
| During the last month, how often have you been bothered by feeling down, depressed, or hopeless? | 0.61 | 0.37 | |||
| Neighborhood social environment (inversely coded: the higher the worse) | 0.86 | 0.75 | |||
| Social capital | 0.84 | 0.71 | |||
| Safety | 0.90 | 0.80 | |||
| Social capital | 0.60 | 0.26 | |||
| Over the past 12 months, have you volunteered for or through an organization or helped out as a volunteer to address needs in your community? | 0.20 | 0.04 | |||
| How would you describe your ability to influence local-government decision making? | 0.32 | 0.10 | |||
| People in this neighborhood can be trusted. | 0.65 | 0.43 | |||
| Children and youth in my town generally have the positive role models they need around here. | 0.75 | 0.56 | |||
| If the fire station closest to your home was going to be closed down by your city or town, how likely is it that neighborhood residents would organize to try to do something to keep the fire station open? | 0.43 | 0.18 | |||
| Safety | 0.51 | 0.26 | |||
| In the past 12 months, have you had anyone deliberately vandalize, try to steal, or steal any property that you own, or anyone attempt to break into your home? | 0.47 | 0.22 | |||
| In the past 12 months, have you had an experience in which someone attacked you, tried to take something from you by force, or physically threatened you? | 0.59 | 0.35 | |||
| I do not feel safe to go on walks in my neighborhood at night. | 0.47 | 0.22 | |||
| Neighborhood built environment (inversely coded: the higher the worse) | 0.56 | 0.28 | |||
| Many stores, banks, markets or places to go are within easy walking distance of my home. | 0.20 | 0.04 | |||
| There are safe sidewalks and crosswalks on most of the streets in my neighborhood. | 0.31 | 0.09 | |||
| There are places to bicycle in or near my neighborhood that are safe from traffic, such as on the street or on special lanes, separate paths or trails. | 0.69 | 0.48 | |||
| My neighborhood has several free or low cost recreation facilities such as parks, playgrounds, public swimming pools, etc. | 0.72 | 0.52 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cunningham, S.D.; Mandelbaum, J.; Shebl, F.M.; Abraham, M.; O’Connor Duffany, K. Neighborhood Social Environment and Body Mass Index: The Mediating Role of Mental Wellbeing. Int. J. Environ. Res. Public Health 2023, 20, 6602. https://doi.org/10.3390/ijerph20166602
Cunningham SD, Mandelbaum J, Shebl FM, Abraham M, O’Connor Duffany K. Neighborhood Social Environment and Body Mass Index: The Mediating Role of Mental Wellbeing. International Journal of Environmental Research and Public Health. 2023; 20(16):6602. https://doi.org/10.3390/ijerph20166602
Chicago/Turabian StyleCunningham, Shayna D., Jennifer Mandelbaum, Fatma M. Shebl, Mark Abraham, and Kathleen O’Connor Duffany. 2023. "Neighborhood Social Environment and Body Mass Index: The Mediating Role of Mental Wellbeing" International Journal of Environmental Research and Public Health 20, no. 16: 6602. https://doi.org/10.3390/ijerph20166602
APA StyleCunningham, S. D., Mandelbaum, J., Shebl, F. M., Abraham, M., & O’Connor Duffany, K. (2023). Neighborhood Social Environment and Body Mass Index: The Mediating Role of Mental Wellbeing. International Journal of Environmental Research and Public Health, 20(16), 6602. https://doi.org/10.3390/ijerph20166602






