Unraveling Depressive Symptomatology and Risk Factors in a Changing World
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.1.1. Outcome Definitions and Measurements
2.1.2. Covariates of Interest
2.1.3. Statistical Analysis
2.1.4. Research Questions
- −
- What is the prevalence of depressive symptoms in the Portuguese adult population after the lockdown resulting from the COVID-19 pandemic?
- −
- What are the sociodemographic factors, lifestyles, and health characteristics associated with depressive symptoms in the Portuguese adult population after the lockdown resulting from the COVID-19 pandemic?
- −
- How are these associated with different levels of depressive symptoms?
3. Results
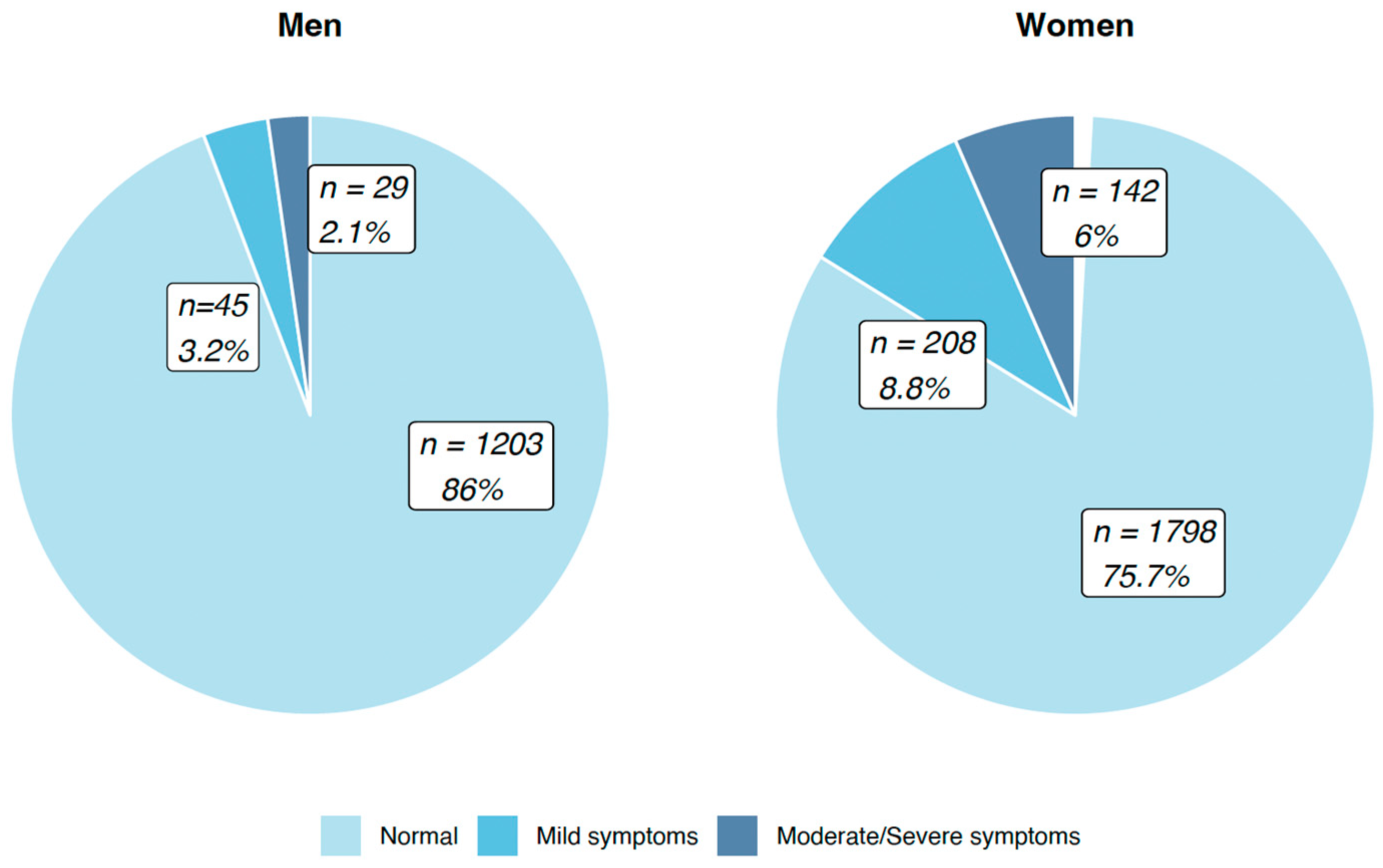
3.1. Symptoms of Depression According to Sociodemographic Factors, Lifestyle, and Health Characteristics
3.2. Factors Associated with Different Levels of Depression
4. Discussion
- (1)
- There was a high prevalence of depressive symptoms (12%) in the late phase of the pandemic.
- (2)
- There are population groups that are particularly vulnerable to depressive symptoms: the elderly (who remain more vulnerable to COVID-19 even after vaccination) and people living in isolation.
- (3)
- There is potentially an important role of physical exercise as a protective agent.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Ayuso-Mateos, J.L.; Vázquez-Barquero, J.L.; Dowrick, C.; Lehtinen, V.; Dalgard, O.S.; Casey, P.; Wilkinson, C.; Lasa, L.; Page, H.; Dunn, G.; et al. Depressive disorders in Europe: Prevalence figures from the ODIN study. J. Affect. Disord. 2001, 67, 241–248. [Google Scholar] [CrossRef]
- Koyanagi, A.; Stickley, A.; Haro, J.M.; Haringsma, R.; Kittel, F. Prevalence and correlates of major depressive disorder in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. J. Affect. Disord. 2017, 210, 20–27. [Google Scholar]
- Stickley, A.; Koyanagi, A.; Haro, J.M.; Haringsma, R.; Kittel, F. Prevalence of depression and anxiety in Europe: A meta-analysis of E-mental health survey studies. J. Affect. Disord. 2018, 235, 1–9. [Google Scholar]
- Nuevo, R.; Chatterji, S.; Verdes, E.; Naidoo, N.; Arango, C.; Ayuso-Mateos, J.L.; Haro, J.M. Availability of mental health care and stigma associated with mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. J. Affect. Disord. 2016, 190, 48–56. [Google Scholar]
- Pinfold, V.; Toulmin, H.; Thornicroft, G. Stigma in the workplace: A review of the evidence on the impact of mental health-related stigma on employment. J. Ment. Health Train. Educ. Pract. 2018, 13, 3–20. [Google Scholar]
- Merikangas, K.R.; He, J.P.; Brody, D.; Fisher, P.W.; Bourdon, K.; Koretz, D.S. Prevalence and treatment of mental disorders among US children in the 2001–2004 NHANES. Pediatrics 2010, 125, 75–81. [Google Scholar] [CrossRef]
- Zhao, Z.; Ding, N.; Song, S.; Liu, Y.; Wen, D. Association between depression and overweight in Chinese adolescents: A cross-sectional study. BMJ Open 2019, 9, e024177. [Google Scholar] [CrossRef]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Lu, J.; Xu, X.; Huang, Y.; Li, T.; Ma, C.; Xu, G.; Yin, H.; Xu, X.; Ma, Y.; Wang, L.; et al. Prevalence of depressive disorders and treatment in China: A cross-sectional epidemiological study. Lancet Psychiatry 2021, 8, 981–990. [Google Scholar] [CrossRef]
- Chen, N.-W.; Mutambudzi, M.; Markides, K.S. Trajectories of concurrent depressive symptoms and cognitive function on health outcomes and mortality among older Mexican Americans. Arch. Gerontol. Geriatr. 2022, 100, 104663. [Google Scholar] [CrossRef]
- Ni, X.; Su, H.; Lv, Y.; Li, R.; Chen, C.; Zhang, D.; Chen, Q.; Zhang, S.; Yang, Z.; Sun, L.; et al. The major risk factor for depression in the Chinese middle-aged and elderly population: A cross-sectional study. Front. Psychiatry 2022, 13, 986389. [Google Scholar] [CrossRef]
- John, A.; Pirkis, J.; Gunnell, D.; Appleby, L.; Morrissey, J. Trends in suicide during the COVID-19 pandemic. BMJ 2020, 12, 371. [Google Scholar] [CrossRef]
- Gémes, K.; Bergström, J.; Papola, D.; Barbui, C.; Lam, A.I.F.; Hall, B.J.; Seedat, S.; Morina, N.; Quero, S.; Campos, D.; et al. Symptoms of anxiety and depression during the COVID-19 pandemic in six European countries and Australia - Differences by prior mental disorders and migration status. J. Affect Disord. 2022, 311, 214–223. [Google Scholar] [CrossRef]
- Rodrigues, A.M.; Gouveia, N.; da Costa, L.P.; Eusébio, M.; Ramiro, S.; Machado, P.; Mourão, A.F.; Silva, I.; Laires, P.; Sepriano, A.; et al. EpiReumaPt- the study of rheumatic and musculoskeletal diseases in Portugal: A detailed view of the methodology. Acta Reumatol. Port. 2015, 40, 110–124. [Google Scholar]
- Pais-Ribeiro, J.; Silva, I.; Ferreira, T.; Martins, A.; Meneses, R.; Baltar, M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol. Health Med. 2007, 12, 225–235. [Google Scholar] [CrossRef]
- Gloster, A.T.; Lamnisos, D.; Lubenko, J.; Presti, G.; Squatrito, V.; Constantinou, M.; Nicolaou, C.; Papacostas, S.; Aydın, G.; Chong, Y.Y.; et al. Impact of COVID-19 pandemic on mental health: An international study. PLoS ONE 2020, 15, e0244809. [Google Scholar] [CrossRef]
- Ahmed, N.; Barnett, P.; Greenburgh, A.; Pemovska, T.; Stefanidou, T.; Lyons, N.; Ikhtabi, S.; Talwar, S.; Francis, E.R.; Harris, S.M.; et al. Mental health in Europe during the COVID-19 pandemic: A systematic review. Lancet Psychiatry 2023, 10, 537–556. [Google Scholar] [CrossRef] [PubMed]
- Canavarro, M.C.; Torres, L. Prevalence of depression and its associated factors in a representative sample of the Portuguese population. J. Affect. Disord. 2015, 185, 131–140. [Google Scholar]
- Silva, N.; Lopes, C.; Paúl, C. Depression and associated factors in older adults living in Portugal: Results from the HBSC study. J. Affect. Disord. 2018, 235, 8–15. [Google Scholar]
- Sousa, R.D.; Rodrigues, A.M.; Gregório, M.J.; Branco, J.C.; Gouveia, M.J.; Canhão, H.; Dias, S.S. Anxiety and Depression in the Portuguese Older Adults: Prevalence and Associated Factors. Front. Med. 2017, 4, 196. [Google Scholar] [CrossRef]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef] [PubMed]
- Renaud-Charest, O.; Lui, L.M.W.; Eskander, S.; Ceban, F.; Ho, R.; Di Vincenzo, J.D.; Rosenblat, J.D.; Lee, Y.; Subramaniapillai, M.; McIntyre, R.S. Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. J. Psychiatr. Res. 2021, 144, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Daly, M.; Robinson, E. Depression and anxiety during COVID-19. Lancet 2022, 399, 518. [Google Scholar] [CrossRef]
- Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry 2017, 4, 146–158. [Google Scholar] [CrossRef]
- Albert, P.R. Why is depression more prevalent in women? J. Psychiatry Neurosci. 2015, 40, 219–221. [Google Scholar] [CrossRef]
- Bromberger, J.T.; Schott, L.L.; Kravitz, H.M.; Sowers, M.; Avis, N.E.; Gold, E.B.; Randolph, J.F.; Matthews, K.A. Longitudinal change in reproductive hormones and depressive symptoms across the menopausal transition: Results from the Study of Women’s Health Across the Nation (SWAN). Arch. Gen. Psychiatry 2010, 67, 598–607. [Google Scholar] [CrossRef] [PubMed]
- Piccinelli, M.; Wilkinson, G. Gender differences in depression: Critical review. Br. J. Psychiatry 2000, 177, 486–492. [Google Scholar] [CrossRef]
- Costantini, E.; Trama, F.; Villari, D.; Maruccia, S.; Li Marzi, V.; Natale, F.; Balzarro, M.; Mancini, V.; Balsamo, R.; Marson, F.; et al. The Impact of Lockdown on Couples’ Sex Lives. J. Clin. Med. 2021, 10, 1414. [Google Scholar] [CrossRef]
- Yildiz, E.; Koc Apaydin, Z.; Alay, B.; Dincer, Z.; Cigri, E. COVID-19 History Increases the Anxiety of Mothers with Children in Intensive Care during the Pandemic in Turkey. Children 2022, 9, 1448. [Google Scholar] [CrossRef]



| All (n = 3425) | Missing (n %) | Normal (n = 3001) (HADS-D 0–7) | Missing (n%) | Mild (n = 253) (HADS-D 8–10) | Missing (n%) | Moderate/Severe (n = 171) (HADS-D 11–21) | Missing (n%) | |
|---|---|---|---|---|---|---|---|---|
| Sociodemographic | ||||||||
| Marital status | 3 (0.09) | 1 (0.03) | 2 (0.79) | - | ||||
| Married | 2241 (65.49%) | 1969 (87.86%) | 160 (7.14%) | 112 (5.00%) | ||||
| Other | 1181 (34.51%) | 1031 (87.30%) | 91 (7.71%) | 59 (5.00%) | ||||
| Education level | 7 (0.20) | 5 (0.00) | 1 (0.40) | 1 (0.58) | ||||
| 0–4 years | 1168 (34.17%) | 926 (79.28%) | 141 (12.07%) | 101 (8.65%) | ||||
| 5–9 years | 698 (20.42%) | 614 (87.97%) | 47 (6.73%) | 37 (5.30%) | ||||
| 10–12 years | 746 (21.83%) | 682 (91.42%) | 38 (5.09%) | 26 (3.49%) | ||||
| >12 years | 806 (23.58%) | 774 (96.03%) | 26 (3.23%) | 6 (0.74%) | ||||
| Employment status | 37 (1.08) | 27 (0.90) | 4 (0.02) | 6 (3.51) | ||||
| Employed full/part-time | 1744 (51.48%) | 1650 (94.61%) | 67 (3.84%) | 27 (1.55%) | ||||
| Retired | 1158 (34.18%) | 966 (83.42%) | 111 (9.59%) | 81 (6.99%) | ||||
| Other | 486 (14.34%) | 358 (73.66%) | 71 (14.61%) | 57 (11.73%) | ||||
| Income perception | 57 (1.66) | 44 (1.47) | 5 (1.98) | 8 (4.68) | ||||
| Living comfortably with the present income | 1130 (33.55%) | 1076 (95.22%) | 37 (3.27%) | 17 (1.50%) | ||||
| Living with the present income | 1597 (47.42%) | 1421 (88.98%) | 113 (7.08%) | 63 (3.94%) | ||||
| Finding it difficult to live with the present income | 463 (13.75%) | 354 (76.46%) | 59 (12.74%) | 50 (10.80%) | ||||
| Finding it very difficult to live with the present income | 178 (5.29%) | 106 (59.55%) | 39 (21.91%) | 33 (18.54%) | ||||
| Household size | 46 (1.34) | 34 (1.13) | 5 (1.98) | 7 (4.09) | ||||
| One person | 585 (17.31%) | 469 (80.17%) | 66 (11.28%) | 50 (8.55%) | ||||
| Two people | 1205 (35.66%) | 1046 (86.80%) | 93 (7.72%) | 66 (5.48%) | ||||
| Three or more people | 1589 (47.03%) | 1452 (91.38%) | 89 (5.60%) | 48 (3.02%) | ||||
| BMI (kg/m2) | 141 (4.12) | 106 (3.53) | 23 (9.09) | 12 (7.02) | ||||
| Underweight/normal | 1237 (37.67%) | 1116 (90.22%) | 69 (5.58%) | 52 (4.20%) | ||||
| Overweight | 1332 (40.56%) | 1180 (88.59%) | 89 (6.68%) | 63 (4.73%) | ||||
| Obese | 715 (21.77%) | 599 (83.78%) | 72 (10.07%) | 44 (6.15%) | ||||
| Alcohol intake | 35 (1.02) | 25 (0.83) | 3 (1.19) | 7 (4.37) | ||||
| Daily | 833 (24.57%) | 779 (93.52%) | 34 (4.08%) | 20 (2.40%) | ||||
| Occasional | 1182 (34.87%) | 1091 (92.30%) | 58 (4.91%) | 33 (2.79%) | ||||
| Never | 1375 (40.56%) | 1106 (80.44%) | 158 (11.49%) | 111 (8.07%) | ||||
| Smoking habits | 32 (0.93) | 23 (0.77) | 3 (1.19) | 6 (3.51) | ||||
| Past smoker | 758 (22.34%) | 698 (92.08%) | 36 (4.75%) | 24 (3.17%) | ||||
| Current/occasional smoker | 516 (15.21%) | 464 (89.13%) | 31 (6.01%) | 21 (4.07%) | ||||
| Never | 2119 (62.45%) | 1816 (85.70%) | 183 (8.64%) | 120 (5.66%) | ||||
| Regular physical Exercise | 38 (1.11) | 29 (0.97) | 4 (1.58) | 5 (2.92) | ||||
| Never | 1744 (51.49%) | 1451 (83.20%) | 177 (10.15%) | 116 (6.65%) | ||||
| Yes | 830 (24.51%) | 773 (93.13%) | 32 (3.86%) | 25 (3.01%) | ||||
| Occasionally | 813 (24.00%) | 748 (92.00%) | 40 (4.92%) | 25 (3.08%) | ||||
| Health | ||||||||
| Multimorbidity (self-reported) | - | - | - | |||||
| No | 1719 (50.19%) | 1615 (93.95%) | 62 (3.61%) | 42 (2.44%) | ||||
| Yes | 1706 (49.81%) | 1386 (81.24%) | 191 (11.20%) | 129 (7.56%) | ||||
| COVID-19 | ||||||||
| COVID-19 infection | 15 (0.44) | 15 (0.50) | - | - | ||||
| No | 3145 (92.23%) | 2749 (87.41%) | 238 (7.57%) | 158 (5.02%) | ||||
| Yes | 265 (7.77%) | 237 (89.43%) | 15 (5.66%) | 11 (4.91%) |
| Normal vs. Mild | |||
|---|---|---|---|
| Relative Risk Ratio | [95% CI] | ||
| Gender | |||
| Male | Ref | - | |
| Female | 1.85 | [1.26–2.71] | |
| Age group | |||
| 25–34 | Ref | - | |
| 35–44 | 3.02 | [1.13–8.06] | |
| 45–54 | 1.49 | [0.55–4.03] | |
| 55–64 | 1.76 | [0.64–4.81] | |
| 65–74 | 1.16 | [0.39–3.47] | |
| ≥75 years | 1.62 | [0.53–4.91] | |
| NUTSII | |||
| LVT | Ref | - | |
| Norte | 1.68 | [1.06–2.67] | |
| Centro | 1.84 | [1.14–2.97] | |
| Alentejo | 1.30 | [0.64–2.65] | |
| Algarve | 2.38 | [1.06–5.33] | |
| Azores | 1.78 | [1.00–3.15] | |
| Madeira | 1.45 | [0.77–2.73] | |
| Education level | |||
| 0–4 years | Ref | - | |
| 5–9 years | 0.77 | [0.51–1.17] | |
| 10–12 years | 0.96 | [0.60–1.53] | |
| >12 years | 0.72 | [0.41–1.24] | |
| Employment status | |||
| Employed full/part-time | Ref | - | |
| Retired | 1.87 | [1.10–3.16] | |
| Other | 2.33 | [1.52–3.58] | |
| Income perception | |||
| Living comfortably with the present income | Ref | - | |
| Living with the present income | 1.58 | [1.03–2.43] | |
| Finding it difficult to live with the present income | 2.48 | [1.51–4.08] | |
| Finding it very difficult to live with the present income | 4.64 | [2.58–8.37] | |
| BMI (kg/m2) | |||
| Underweight/normal | Ref | - | |
| Overweight | 1.03 | [0.73–1.47] | |
| Obese | 1.16 | [0.80–1.70] | |
| Alcohol intake | |||
| Never | Ref | - | |
| Daily | 0.55 | [0.35–0.85] | |
| Occasional | 0.66 | [0.47–0.95] | |
| Regular Exercise | |||
| Never | Ref | - | |
| Yes | 0.41 | [0.27–0.62] | |
| Occasionally | 0.67 | [0.45–0.98] | |
| Multimorbidity (self-reported) | |||
| No | Ref | - | |
| Yes | 2.27 | [1.54–3.35] | |
| Normal vs. Moderate/Severe | |||
| Relative Risk ratio | [95% CI] | ||
| Gender | |||
| Male | Ref | - | |
| Female | 2.16 | [1.33–3.50] | |
| Age group | |||
| 25–34 years | Ref | - | |
| 35–44 years | 0.86 | [0.27–2.79] | |
| 45–54 years | 0.75 | [0.25–2.21] | |
| 55–64 years | 1.63 | [0.56–4.70] | |
| 65–74 years | 0.58 | [0.18–1.89] | |
| ≥75 years | 0.66 | [0.20–2.20] | |
| NUTSII | |||
| LVT | Ref | - | |
| Norte | 1.13 | [0.69–1.85] | |
| Centro | 0.82 | [0.47–1.43] | |
| Alentejo | 0.66 | [0.29–1.52] | |
| Algarve | 0.18 | [0.02–1.43] | |
| Azores | 0.84 | [0.42–1.67] | |
| Madeira | 0.79 | [0.38–1.67] | |
| Education level | |||
| 0–4 years | Ref | - | |
| 5–9 years | 0.79 | [0.50–1.26] | |
| 10–12 years | 0.81 | [0.46–1.44] | |
| >12 years | 0.19 | [0.07–0.51] | |
| Employment status | |||
| Employed full/part-time | Ref | - | |
| Retired | 3.54 | [1.90–6.58] | |
| Other | 3.84 | [2.25–6.55] | |
| Income perception | |||
| Living comfortably with the present income | Ref | - | |
| Living with the present income | 1.38 | [0.77–2.47] | |
| Finding it difficult to live with the present income | 3.12 | [1.68–5.79] | |
| Finding it very difficult to live with the present income | 6.84 | [3.41–13.72] | |
| BMI (kg/m2) | |||
| Underweight/normal | Ref | - | |
| Overweight | 0.84 | [0.55–1.27] | |
| Obese | 0.78 | [0.49–1.24] | |
| Alcohol intake | |||
| Never | Ref | - | |
| Daily | 0.43 | [0.25–0.75] | |
| Occasional | 0.56 | [0.38–0.87] | |
| Regular Exercise | |||
| Never | Ref | - | |
| Yes | 0.44 | [0.27–0.71] | |
| Occasionally | 0.56 | [0.34–0.93] | |
| Multimorbidity (self-reported) | |||
| No | Ref | - | |
| Yes | 1.51 | [0.95–2.39] | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sousa, R.D.; Henriques, A.R.; Caldas de Almeida, J.; Canhão, H.; Rodrigues, A.M. Unraveling Depressive Symptomatology and Risk Factors in a Changing World. Int. J. Environ. Res. Public Health 2023, 20, 6575. https://doi.org/10.3390/ijerph20166575
Sousa RD, Henriques AR, Caldas de Almeida J, Canhão H, Rodrigues AM. Unraveling Depressive Symptomatology and Risk Factors in a Changing World. International Journal of Environmental Research and Public Health. 2023; 20(16):6575. https://doi.org/10.3390/ijerph20166575
Chicago/Turabian StyleSousa, Rute Dinis, Ana Rita Henriques, José Caldas de Almeida, Helena Canhão, and Ana Maria Rodrigues. 2023. "Unraveling Depressive Symptomatology and Risk Factors in a Changing World" International Journal of Environmental Research and Public Health 20, no. 16: 6575. https://doi.org/10.3390/ijerph20166575
APA StyleSousa, R. D., Henriques, A. R., Caldas de Almeida, J., Canhão, H., & Rodrigues, A. M. (2023). Unraveling Depressive Symptomatology and Risk Factors in a Changing World. International Journal of Environmental Research and Public Health, 20(16), 6575. https://doi.org/10.3390/ijerph20166575








