Interpersonal and Intimate Violence in Mexican Youth: Drug Use, Depression, Anxiety, and Stress during the COVID-19 Pandemic
Abstract
1. Introduction
1.1. Violence, AOD Use, and Mental Health Conditions before and in the First Year of the Pandemic
1.2. Interpersonal and Intimate Violence
1.3. Relationships and Directionality between Violence, AOD Use, and Mental Health Conditions
1.4. Factors, the Directionality of Associations, and the Social Determinants Yet to Be Explored
2. Methods
2.1. Participants
2.2. Instruments
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Confirmatory Factorial Analyses and Cronbach’s Alpha
3.2. Violence, Harmful AOD Use, Depression, Anxiety, and PTSD in the Total Sample and by Sex and Educational Attainment
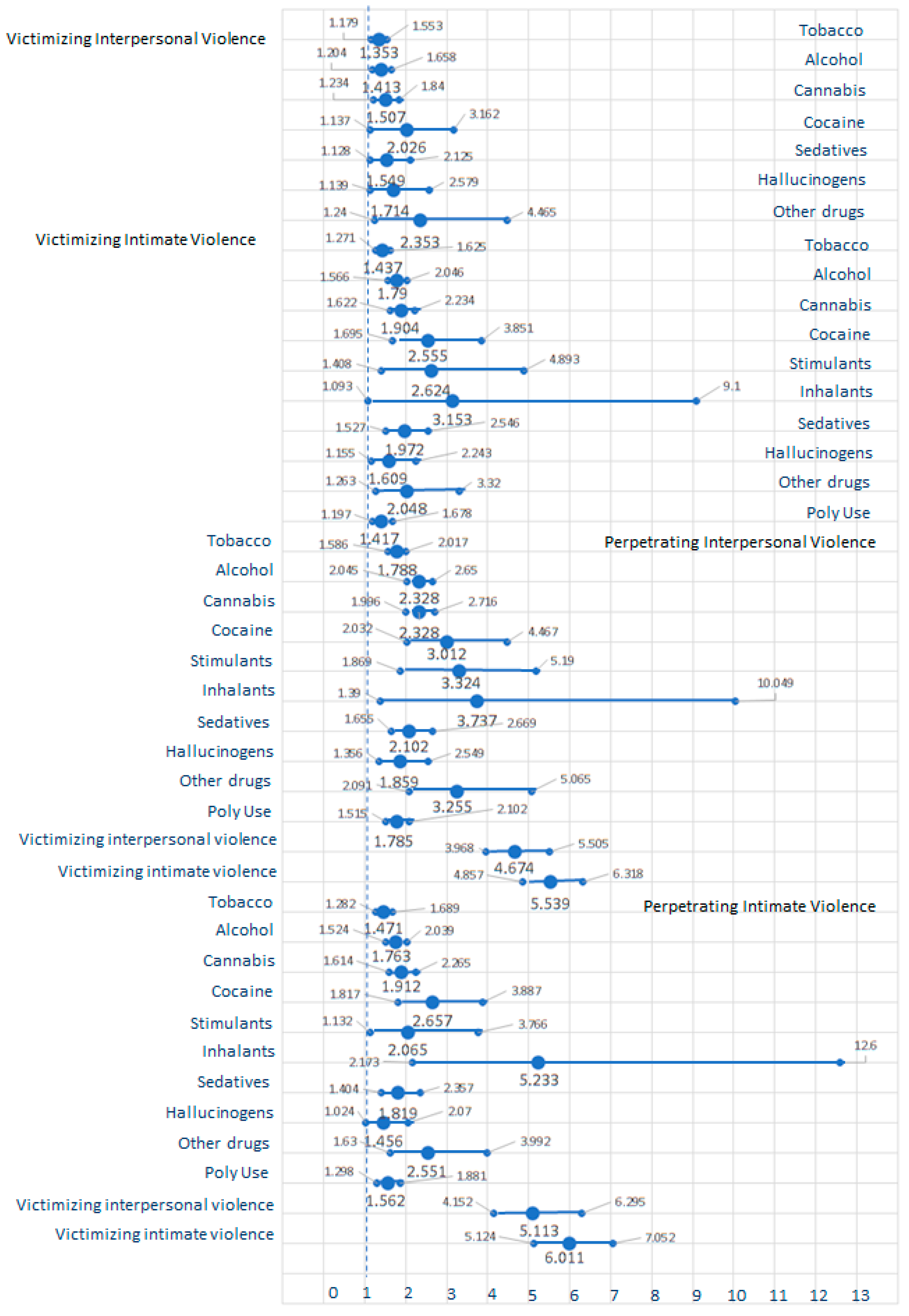
3.3. Relative Risks between Violence, Harmful AOD Use, and Mental Health Symptoms
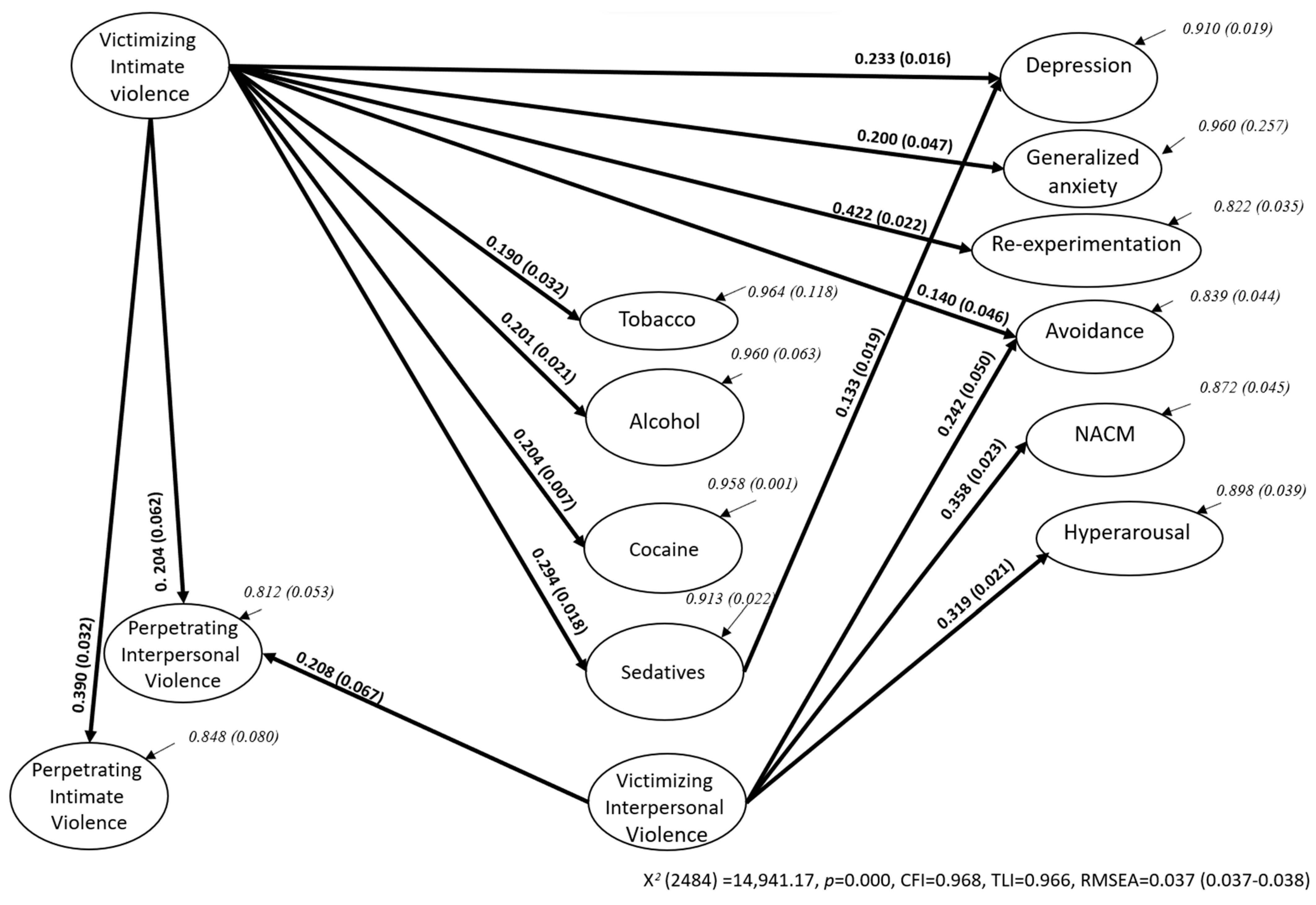
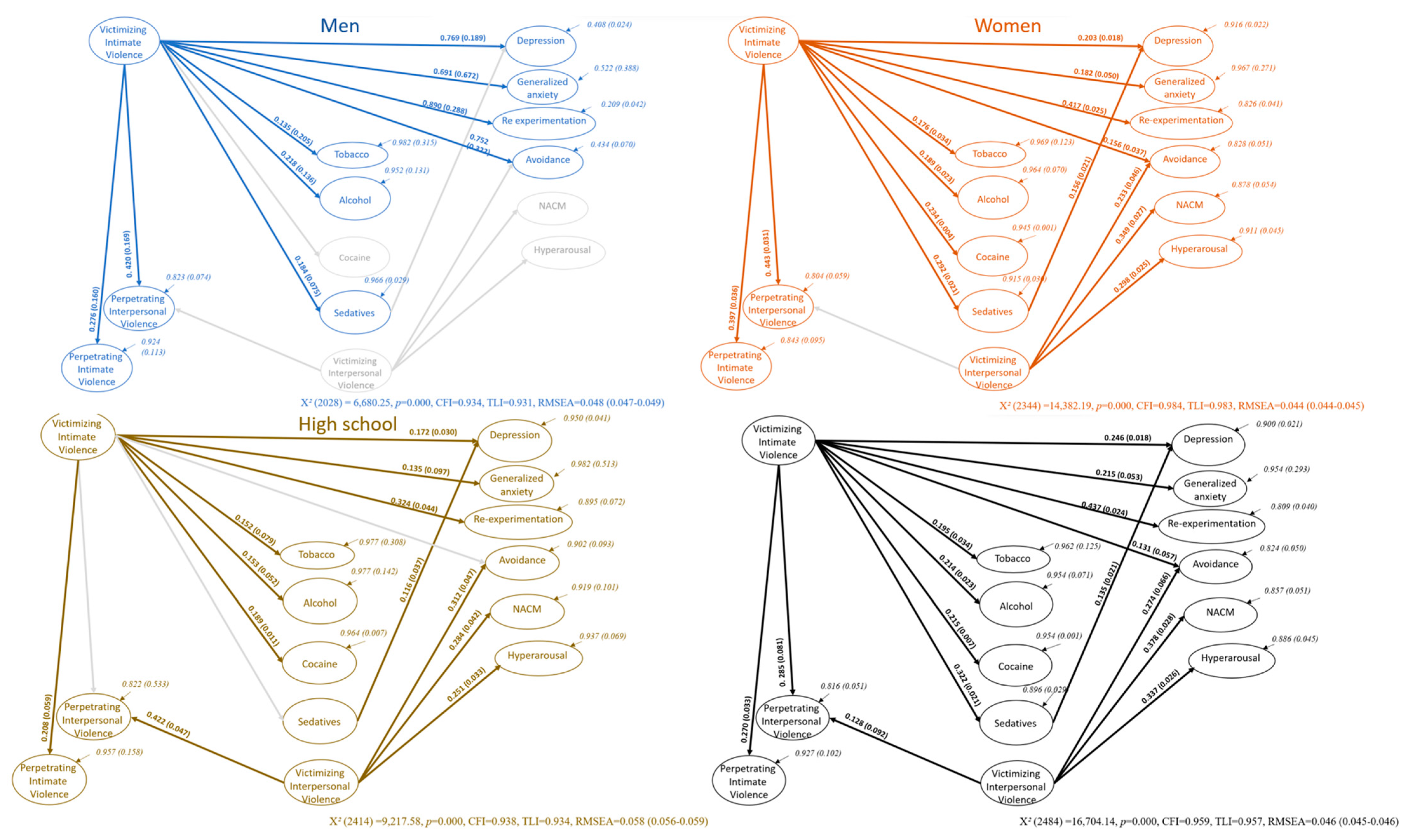
3.4. Structural Equation Modeling
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variables and Measuring Items | Loadings | SE | p< |
|---|---|---|---|
| Victimizing Interpersonal Violence | |||
| Have you been a victim of physical violence (been attacked, hit, slapped, kicked, beaten up)? | 0.884 | ||
| Have you been a victim of emotional violence (insults, humiliation, screaming, being put down, or similar experiences)? | 0.600 | 0.032 | 0.001 |
| Have you been a victim of sexual violence (unwanted touching, sexual act through force, or threat of harm to maintain unwanted sexual activity)? | 0.439 | 0.037 | 0.001 |
| Have you been a victim of sexual harassment (e.g., soliciting intimate/physical contact in exchange for academic or work achievements, felt continuous verbal or online threats)? | 0.320 | 0.036 | 0.001 |
| Victimizing Intimate Violence | |||
| Was this physical abuse inflicted by a family member or your partner? | 0.910 | ||
| Was this emotional abuse inflicted by a family member or your partner? | 0.580 | 0.030 | 0.001 |
| Was this sexual abuse inflicted by a family member or your partner? | 0.494 | 0.047 | 0.001 |
| Was the violence you observed inside your family (e.g., from father to son, from any person to your partner, etc.? | 0.371 | 0.035 | 0.001 |
| Perpetrating interpersonal Violence | |||
| Have you perpetrated any physical violence (hitting, pushing, pinching, etc.)? | 0.739 | ||
| Have you perpetrated any emotional violence (insults, humilliation, screaming, putting down, or similar experiences)? | 0.617 | 0.074 | 0.001 |
| Have you perpetrated any sexual violence (unwanted touching, sexual act through force, or threat of harm to maintain unwanted sexual activity)? | 0.691 | 0.135 | 0.001 |
| Have you perpetrated any sexual harassment (e.g., soliciting intimate/physical contact in exchange for academic or work achievements, sexual insuation to make others feel uncomfortable, repeated insinuations even the resistance of the other person, verbally or online)? | 0.601 | 0.122 | 0.001 |
| Perpetrating Intimate Violence | |||
| Was this physical abuse inflicted on a family member? | 0.907 | ||
| Was this emotional abuse inflicted on a family member? | 0.67 | 0.074 | 0.001 |
| Tobacco products (cigarretes, chewing tobacco, cigars, etc.) | |||
| In the past three months, how often have you used tobacco products (cigarrettes, chewing tobacco, cigars, etc.)? | 0.827 | ||
| During the past three months, how often have you had a strong desire or urge to use tobacco products (cigarrettes, chewing tobacco, cigars, etc.)? | 0.845 | 0.077 | 0.001 |
| During the past three months, how often has your use of tobacco products (cigarrettes, chewing tobacco, cigars, etc.) led to health, social, legal or financial problems? | 0.645 | 0.096 | 0.001 |
| Has a friend or relative or anyone else ever expressed concern about your use of tobacco products (cigarrettes, chewing tobacco, cigars, etc.)? | 0.625 | 0.041 | 0.001 |
| Have you ever tried to cut down on using tobacco Products (cigarrettes, chewing tobacco, cigars, etc.) but failed? | 0.650 | 0.073 | 0.001 |
| Alcoholic beverages (beer, wine, spirits, etc.) | |||
| In the past three months, how often have you used alcoholic beverages (beer, wine, spirits, etc.)? | 0.593 | ||
| During the past three months, how often have you had a strong desire or urge to use alcoholic beverages (beer, wine, spirits, etc.)? | 0.728 | 0.152 | 0.001 |
| During the past three months, how often has your use of alcoholic beverages (beer, wine, spirits, etc.) led to health, social, legal or financial problems? | 0.715 | 0.354 | 0.001 |
| During the past three months, how often have you failed to do what was normally expected of you because of your use of alcoholic beverages (beer, wine, spirits, etc.)? | 0.663 | 0.329 | 0.001 |
| Has a friend or relative or anyone else ever expressed concern about your use of alcoholic beverages (beer, wine, spirits, etc.)? | 0.620 | 0.099 | 0.001 |
| Have you ever tried to cut down on using alcoholic beverages (beer, wine, spirits, etc.) but failed? | 0.437 | 0.106 | 0.001 |
| Cocaine (coke, crack, etc.) | |||
| In the past three months, how often have you used (coke, crack, etc.)? | 0.849 | ||
| During the past three months, how often have you had a strong desire or urge to use cocaine (coke, crack, etc.)? | 0.806 | 0.024 | 0.001 |
| During the past three months, how often has your use of cocaine (coke, crack, etc.) led to health, social, legal or financial problems? | 0.879 | 0.005 | 0.001 |
| During the past three months, how often have you failed to do what was normally expected of you because of your use of cocaine (coke, crack, etc.)? | 0.707 | 0.059 | 0.001 |
| Has a friend or relative or anyone else ever expressed concern about your use of cocaine (coke, crack, etc.)? | 0.681 | 0.014 | 0.001 |
| Have you ever tried to cut down on using cocaine (coke, crack, etc.) but failed? | 0.719 | 0.023 | 0.001 |
| Sedatives or sleeping pills (diazepam, alprazolam, flunitrazepam, midazolam, etc.) | |||
| In the past three months, how often have you used sedatives or sleeping pills (diazepam, alprazolam, flunitrazepam, midazolam, etc.)? | 0.815 | ||
| During the past three months, how often have you had a strong desire or urge to use sedatives or sleeping pills (diazepam, alprazolam, flunitrazepam, midazolam, etc.)? | 0.787 | 0.048 | 0.001 |
| During the past three months, how often has your use of sedatives or sleeping pills (diazepam, alprazolam, flunitrazepam, midazolam, etc.) led to health, social, legal or financial problems? | 0.713 | 0.055 | 0.001 |
| During the past three months, how often have you failed to do what was normally expected of you because of your use of sedatives or sleeping pills (diazepam, alprazolam, flunitrazepam, midazolam, etc.)? | 0.586 | 0.066 | 0.001 |
| Has a friend or relative or anyone else ever expressed concern about your use of sedatives or sleeping pills (diazepam, alprazolam, flunitrazepam, midazolam, etc.)? | 0.653 | 0.027 | 0.001 |
| Have you ever tried to cut down on using Sedatives or sleeping pills (diazepam, alprazolam, flunitrazepam, midazolam, etc.) but failed? | 0.722 | 0.041 | 0.001 |
| Depression (Major Depression Episode, MDE) | |||
| Sadness or depressed mood? | 0.742 | ||
| Discouraged because of how things were going in your life? | 0.687 | 0.029 | 0.001 |
| Loss of interest or pleasure? | 0.673 | 0.032 | 0.001 |
| Feeling worthlessness or not good enough? | 0.650 | 0.038 | 0.001 |
| Recurrent thoughts of death? | 0.611 | 0.051 | 0.001 |
| Indecisiveness or diminished ability to concentrate? | 0.597 | 0.036 | 0.001 |
| Significant weight loss when not dieting or weight gain? | 0.503 | 0.040 | 0.001 |
| Insomnia or hypersomnia | 0.510 | 0.036 | 0.001 |
| Psychomotor agitation or retardation? | 0.584 | 0.048 | 0.001 |
| Fatigue or loss of energy? | 0.621 | 0.036 | 0.001 |
| Symptoms causing impairment in social, occupational, or other important areas of functioning? | 0.718 | 0.040 | 0.001 |
| Generalized Anxiety (GA) | |||
| I have felt nervous or on edge. | 0.703 | ||
| I have felt unable to control my worrying. | 0.808 | 0.041 | 0.001 |
| I have felt so restless it was hard to keep still. | 0.764 | 0.050 | 0.001 |
| I have had trouble relaxing. | 0.808 | 0.038 | 0.001 |
| I have felt afraid something awful could happen. | 0.673 | 0.052 | 0.001 |
| Reexperimentation from the Posttraumatic Check List 5th Edition (PCL-5) | |||
| B1.Repeated, disturbing, and unwanted memories of the stressful experience? | 0.694 | ||
| B2.Repeated, disturbing dreams of the stressful experience? | 0.704 | 0.053 | 0.001 |
| B3.Suddenly feeling or acting as if the stressful experience were actually happening again (as if you were actually back there reliving it)? | 0.769 | 0.052 | 0.001 |
| B4.Feeling very upset when something reminded you of the stressful experience? | 0.763 | 0.032 | 0.001 |
| B5.Having strong physical reactions when something reminded you of the stressful experience (for example, heart pounding, trouble breathing, sweating)? | 0.743 | 0.053 | 0.001 |
| Avoidance from the PCL-5 | |||
| C1.Avoiding memories, thoughts, or feelings related to the stressful experience? | 0.851 | ||
| C2.Avoiding external reminders of the stressful experience (for example, people, places, conversations, activities, objects, or situations)? | 0.833 | 0.032 | 0.001 |
| Negative Alterations in Cognitions and Mood (NACM) from the PCL-5 | |||
| D1.Trouble remembering important parts of the stressful experience? | 0.646 | ||
| D2.Having strong negative beliefs about yourself, other people, or the world (for example, having thoughts such as: I am bad, there is something seriously wrong with me, no one can be trusted, the world is completely dangerous)? | 0.653 | 0.042 | 0.001 |
| D3.Blaming yourself or someone else for the stressful experience or what happened after it? | 0.697 | 0.047 | 0.001 |
| D4.Having strong negative feelings such as fear, horror, anger, guilt, or shame? | 0.760 | 0.048 | 0.001 |
| D5.Loss of interest in activities that you used to enjoy? | 0.580 | 0.037 | 0.001 |
| D6.Feeling distant or cut off from other people? | 0.664 | 0.043 | 0.001 |
| D7.Trouble experiencing positive feelings (for example, being unable to feel happiness or have loving feelings for people close to you? | 0.637 | 0.047 | 0.001 |
| Hyperarousal from the PCL-5 | |||
| E1.Irritable behavior, angry outbursts, or acting aggressively? | 0.589 | ||
| E2.Taking too many risks or doing things that could cause you harm? | 0.600 | 0.050 | 0.001 |
| E3.Being “hyperalert” or watchful or on guard? | 0.592 | 0.050 | 0.001 |
| E4.Feeling jumpy or easily startled? | 0.657 | 0.043 | 0.001 |
| E5.Having difficulty concentrating? | 0.544 | 0.036 | 0.001 |
| E6.Trouble falling or staying asleep? | 0.553 | 0.050 | 0.001 |
References
- World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact. 2020. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 (accessed on 17 May 2023).
- World Health Organization. Intimate Partner Violence. 2023. Available online: https://apps.who.int/violence-info/intimate-partner-violence (accessed on 17 May 2023).
- Pan American Health Organization. Burden of Non-fatal Interpersonal Violence: Trends Over Time. 2020. Available online: https://www.paho.org/en/enlace/burden-other-forms-interpersonal-violence (accessed on 17 May 2023).
- United Nations Office on Drugs and Crime. World Drug Report 2022. 2022. Available online: https://www.unodc.org/res/wdr2022/MS/World_Drug_Report_2022_Exsum_and_Policy_implications_Spanish.pdf (accessed on 17 May 2023).
- Layman, H.M.; Thorisdottir, I.E.; Halldorsdottir; Sigfusdottir, I.D.; Allegrante, J.P.; Kristjansson, A.L. Substance use among youth during the COVID-19 pandemic: A systematic review. Curr. Psychiatry Rep. 2022, 24, 307–324. [Google Scholar] [CrossRef]
- Bourmistrova, N.W.; Solomon, T.; Braude, P.; Strawbridge, R.; Carter, B. Long-term effects of COVID-19 on mental health: A systematic review. J. Affect. Disord. 2022, 299, 118–125. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Statistics and Geography. Violencia Contra las Mujeres en México. 2021. Available online: https://www.inegi.org.mx/tablerosestadisticos/vcmm/ (accessed on 17 May 2023).
- National Committee on Addictions. Mental Health, and Substance Abuse Observer System. 2021. Available online: https://www.gob.mx/cms/uploads/attachment/file/648021/INFORME_PAIS_2021.pdf (accessed on 17 May 2023).
- White, S.J.; Sin, J.; Sweeny, A.; Salisbury, T.; Wahlich, C.; Montesinos, G.C.M.; Gillard, S.; Brett, E.; Alwright, L.; Iqbal, N.; et al. Global prevalence and mental health outcomes of intimate partner violence among women: A systematic review and meta-analysis. Trauma Violence Abus. 2023, 15248380231155529. [Google Scholar] [CrossRef]
- Alexander, E.F.; Johnson, M.D. On categorizing intimate partner violence: A systematic review of exploratory clustering and classification studies. J. Fam. Psychol. 2023, 37, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Kourti, A.; Stavridou, A.; Panagouli, E.; Psaltopoulou, T.; Spiliopoulou, C.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Domestic violence during the COVID-19 pandemic: A systematic review. Trauma Violence Abus. 2023, 24, 719–745. [Google Scholar] [CrossRef] [PubMed]
- Oram, S.; Fisher, H.L.; Minnis, H.; Seedat, S.; Walby, S.; Hegarty, K.; Rouf, K.; Angénieux, C.; Callard, F.; Chandra, P.S.; et al. The Lancet Psychiatry Commission on intimate partner violence and mental health: Advancing mental health services, research, and policy. Lancet Psychiatry 2022, 9, 487–524. [Google Scholar] [CrossRef]
- Johnson, M.P. A Typology of Domestic Violence: Intimate Terrorism, Violent Resistance, and Situational Couple Violence; Northeastern University Press: Lebanon, NH, USA, 2008. [Google Scholar]
- Holtzworth-Munroe, A.; Stuart, G.L. Typologies of male batterers: Three subtypes and the differences among them. Psychol. Bull. 1994, 116, 476–497. [Google Scholar] [CrossRef]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The Life Events Checklist for DSM-5 (LEC.5)-Standard. 2013. [Measurement Instrument]. Available online: https://vdocuments.net/life-events-checklist-for-dsm-5-lec-5.html?page=1 (accessed on 17 May 2023).
- Scott-Storey, K.; O’Donnell, S.; Ford-Gilboe, M.; Varcoe, C.; Wachen, N.; Malcolm, J.; Vincent, C. What about the men? A critical review of men’s experiences of intimate partner violence. Trauma Violence Abus. 2023, 24, 858–872. [Google Scholar] [CrossRef]
- Glowacz, F.; Dziewa, A.; Schmits, E. Intimate partner violence and mental health during lockdown of the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2022, 19, 2535. [Google Scholar] [CrossRef]
- Mellos, E.; Paparrogopoulos, T. Substance use during the COVID-19 pandemic: What is really happening? Psychiatriki 2022, 33, 17–20. [Google Scholar] [CrossRef]
- Craig, S.G.; Ames, M.E.; Bondi, B.C.; Pepler, D.J. Canadian adolescents’ mental health and substance use during the COVID-19 pandemic: Associations with COVID-19 stressors. Can. J. Behav. Sci. 2023, 55, 46–55. [Google Scholar] [CrossRef]
- Brabete, A.C.; Greaves, L.; Wolfson, L.; Stinson, J.; Allen, S.; Poole, N. Substance Use (SU) among Women in the Context of the Corollary Pandemics of COVID-19 and Intimate Partner Violence (IPV); Vancouver, B.C., Ed.; Centre of Excellence for Women’s Health: Vancouver, BC, Canada, 2020; Available online: https://covid19mentalhealthresearch.ca/wp-content/uploads/2021/01/GREAVES_CMH-KS-final-report-2020-11-23.pdf (accessed on 17 January 2023).
- Machisa, M.; Shamu, S. Mental ill health and factors associated with men’s use of intimate partner violence in Zimbabwe. BMC Public Health 2018, 18, 376. [Google Scholar] [CrossRef]
- Morales-Chainé, S.; López, M.A.; Bosch, M.A.; Beristain, A.A.; Robles, G.R.; Garibay, R.C.R.; Astudillo, G.C.I.; Lira, C.I.A.; Rangel, G.M.G. Mental health symptoms, binge drinking, and the experience of abuse during the COVID-19 lockdown in Mexico. Front. Public Health 2021, 9, 656036. [Google Scholar] [CrossRef]
- Caldentey, C.; Tirado-Muñoz, J.; Ferrer, T.; Fonseca-Casals, F.; Rossi, P.; Mestre-Pintó, J.I.; Torrens-Melich, M. Intimate partner violence among female drug users admitted to the general hospital: Screening and prevalence. Adicciones 2017, 29, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Low, S.; Tiberio, S.S.; Shortt, J.W.; Capaldi, D.M.; Eddy, J.M. Associations of couples’ intimate partner violence in young adulthood and substance use: A dyadic approach. Psyhcol. Violence 2017, 7, 120–127. [Google Scholar] [CrossRef]
- Dos-Santos, I.B.; Costa-Leite, F.M.; Costa-Amorim, M.H.; Ambrosio-Maciel, P.M.; Gigante, D.P. Violence against women in life: Study among primary care users. Cienc. Saude Colect. 2020, 25, 1935–1946. [Google Scholar] [CrossRef]
- Barchi, F.; Winter, S.; Dougherty, D.; Ramaphane, P. Intimate partner violence against women in Northwestern Botswana: The maun women’s Study. Violence Against Women 2018, 24, 1909–1927. [Google Scholar] [CrossRef]
- Zhong, S.; Yu, R.; Fazel, S. Drug use disorders and violence: Associations with individual drug categories. Epidemiol. Rev. 2020, 42, 103–116. [Google Scholar] [CrossRef]
- Bosch, J.; Weaver, T.L.; Arnold, L.D.; Clark, E.M. The impact of intimate partner violence on women’s physical health: Findings from the Missouri behavioral risk factor surveillance system. J. Interpers. Violence 2017, 32, 3402–3419. [Google Scholar] [CrossRef] [PubMed]
- Biswas, C.S. Spousal violence against working women in India. J. Fam. Violence 2017, 32, 55–67. Available online: https://link.springer.com/article/10.1007/s10896-016-9889-9 (accessed on 17 May 2023). [CrossRef]
- Hernández, W. Violence with femicide risk: Its effects on women and their children. J. Interpers. Violence 2018, 36, 886260518815133. [Google Scholar] [CrossRef]
- Gubi, D.; Nansubuga, E.; Wandera, S.O. Correlates of intimate partner violence among married women in Uganda: A cross-sectional survey. BMD Public Health 2020, 20, 1–11. [Google Scholar] [CrossRef]
- Elhai, J.D.; Palmieri, P.A. The factor structure of posttraumatic stress disorder: A literature update, critique of methodology, and agenda for future research. J. Anxiety Disord. 2011, 25, 849–854. [Google Scholar] [CrossRef]
- Morales-Chainé, S.; Robles, G.R.; López, M.A.; Bosch, M.A.; Beristain, A.A.G.; Treviño, S.C.C.L.; Palafox, P.G.; Lira, C.I.A.; Barragan, T.L.; Rangel, G.M.G. Screening tool for mental health problems during COVID-19 pandemic: Psychometrics and associations with sex, grieving, contagion, and seeking psychological care. Front. Psychol. 2022, 13, 882573. [Google Scholar] [CrossRef] [PubMed]
- Browne, M.W.; Cudeck, R. Alternative ways of assessing model fit. In Testing Structural Equation Models; Bollen, K.A., Long, J.S., Eds.; Sage Publications: New York, NY, USA, 1993; pp. 136–162. [Google Scholar]
- Li, C. Statistical estimation of structural equation models with a mixture of continuous and categorical observed variables. Behav. Res. Methods 2021, 53, 2191–2213. [Google Scholar] [CrossRef] [PubMed]
- West, S.G.; Taylor, A.B.; Wu, W. Model fit and model selection in structural equation modeling. In Handbook of Structural Equation Modeling; Hoyle, R.H., Ed.; Guilford Press: New York, NY, USA, 2012; pp. 380–392. [Google Scholar]
- Eysenbach, G. Improving the quality of web surveys: The checklist for reporting results of internet W-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef] [PubMed]
- General Protection of Personal Information in Possession of Obligated Parties Act, of January 26, 2017 (DOF 26-01-2017). Available online: http://www.diputados.gob.mx/LeyesBiblio/pdf/LGPDPPSO.pdf (accessed on 13 March 2020).
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5)—LEC-5 and Extended Criterion A [Measurement instrument]. 2013. Available online: https://www.ptsd.va.gov/professional/assessment/documents/PCL5_criterionA_form.PDF (accessed on 17 January 2023).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- World Health Organization. The Alcohol, Smoking and Substance Involvement Screening Test: Manual for Use in Primary Care. 2010. Available online: https://www.who.int/publications/i/item/978924159938-2 (accessed on 12 April 2022).
- Morales-Chainé, S.; Robles-García, R.; Barragán-Torres, L.; Treviño, S.C.C.L. Remote screening for alcohol, smoking, and substance involvement by sex, age, lockdown condition, and psychological care-seeking in the primary care setting during the COVID-19 pandemic in México. Int. J. Ment. Health Addict. 2022. [Google Scholar] [CrossRef]
- Morales-Chainé, S.; Robles, G.R.; Bosch, M.A.; Treviño, S.C.C.L. Depressive, anxious, and Post-Traumatic Stress symptoms related to violence during the COVID-19 pandemic, by sex, COVID-19 status, and interventions-seeking conditions among the general population. Int. J. Environ. Res. Public Health 2022, 19, 12559. [Google Scholar] [CrossRef]
- Goldberg, D.P.; Reed, G.M.; Robles, R.; Minhas, F.; Razzaque, B.; Fortés, S.; Mari, J.J.; Lam, T.P.; García, J.A.; Gask, L.; et al. Screening for anxiety, depression, and anxious depression in primary care: A field study for ICD-11 PHC. J. Affect. Disord. 2017, 213, 199–206. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD CheckList for DSM-5 (PCL-5)-Standard. 2013. Available online: https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.PDF (accessed on 17 January 2023).
- Blevins, C.A.; Weathers, F.W.; Davis, M.T.; Witte, T.K.; Domino, J.L. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J. Trauma. Stress 2015, 28, 489–498. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. 2018. Available online: https://www.R-project.org (accessed on 17 January 2023).
- IBM Corp. Released 2017. IBM SPSS Statistics for Windows; Version 25.0; IBM Corp: Armonk, NY, USA, 2017. [Google Scholar]
- Tiburcio, S.M.; Rosete-Mohedano, G.; Natera, R.G.; Martínez, V.N.A.; Carreño, G.S.; Pérez, C.D. Validez y confiabilidad de la prueba de detección de consumo de alcohol, tabaco y sustancias (ASSIST) en estudiantes universitarios. Adicciones 2016, 28, 19–27. Available online: https://www.adicciones.es/index.php/adicciones/article/view/786/750 (accessed on 17 January 2023).
- Keeley, J.W.; Reed, G.M.; Roberts, M.C.; Evans, S.C.; Robles, R.; Matsumoto, C.; Brewin, C.R.; Cloitre, M.; Perkonigg, A.; Rousseau, C.; et al. Disorders specifically associated with stress: A case-controlled field study for ICD-11 mental and behavioural disorders. Int. J. Clin. Health Psychol. 2016, 16, 109–127. [Google Scholar] [CrossRef] [PubMed]
- Boreham, M.; Marlow, S.; Gilchrist, G. ‘That warm feeling that [alcohol] gave me was what I interpreted love would feel like’ Lived experience of excessive alcohol use and care proceeding by mothers in the family justice system in the UK. Addict. Behav. 2019, 92, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Barbero, B.; López-Pereira, P.; Barrio, G.; Vives-Cases, C. Intimate partner violence against young women: Prevalence and associated factors in Europe. J. Epidemiol. Community Health 2018, 72, 611–616. [Google Scholar] [CrossRef]
- Ismayilova, L. Spousal violence in 5 transitional countries: A population-based multilevel analysis of individual and contextual factors. Am. J. Public Health 2015, 105, e12–e22. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.J.; Mazerolle, P.; Broidy, L.; Baird, K. Exploring the prevalence and correlates associated with intimate partner violence during pregnancy in Bangladesh. J. Interpers. Violence 2021, 36, 663–690. [Google Scholar] [CrossRef]

| TOTAL | |||||||
| n | % | ||||||
| 7420 | 100 | ||||||
| Men | Women | High school | University | ||||
| n | % | n | % | n | % | n | % |
| 2314 | 31.20 | 5106 | 68.8 | 1689 | 22.80 | 5731 | 77.20 |
| Scales-Factors | X2 | df | p ≤ | RMSEA | Confidence Interval | SRMR | CFI | TLI | Cronbach’s Alpha |
|---|---|---|---|---|---|---|---|---|---|
| LEC-5 | |||||||||
| Victimizing Interpersonal Violence | 343.566 | 13 | 0.001 | 0.059 | 0.053–0.064 | 0.949 | 0.917 | 0.76 | |
| Victimizing Intimate Violence | 6.087 | 2 | 0.048 | 0.017 | 0.001–0.032 | 0.999 | 0.997 | 0.76 | |
| Perpetrating Interpersonal Violence | 94.634 | 2 | 0.001 | 0.079 | 0.066–0.093 | 0.952 | 0.855 | 0.68 | |
| Perpetrating Intimate Violence | 0.000 | 0 | 0.000 | 0.000 | 0.000–0.000 | 1.000 | 1.000 | 0.68 | |
| ASSIST | |||||||||
| Once in Lifetime | 272.565 | 35 | 0.001 | 0.030 | 0.027–0.034 | 0.981 | 0.975 | 0.60 | |
| Tobacco | 86.199 | 4 | 0.001 | 0.053 | 0.043–0.063 | 0.013 | 0.994 | 0.986 | 0.83 |
| Alcohol | 163.646 | 8 | 0.001 | 0.051 | 0.045–0.058 | 0.018 | 0.986 | 0.973 | 0.77 |
| Cannabis | 155.431 | 7 | 0.001 | 0.053 | 0.046–0.061 | 0.013 | 0.992 | 0.982 | 0.85 |
| Cocaine | 190.925 | 6 | 0.001 | 0.064 | 0.057–0.072 | 0.014 | 0.992 | 0.981 | 0.87 |
| Stimulants | 161.657 | 6 | 0.001 | 0.059 | 0.051–0.067 | 0.008 | 0.995 | 0.988 | 0.92 |
| Inhalants | 65.051 | 3 | 0.001 | 0.053 | 0.042–0.064 | 0.010 | 0.997 | 0.985 | 0.85 |
| Sedatives | 94.670 | 7 | 0.001 | 0.041 | 0.034–0.049 | 0.010 | 0.995 | 0.990 | 0.86 |
| Hallucinogens | 323.535 | 8 | 0.001 | 0.073 | 0.066–0.080 | 0.026 | 0.960 | 0.925 | 0.71 |
| Opioids | 158.546 | 3 | 0.001 | 0.084 | 0.073–0.095 | 0.009 | 0.998 | 0.990 | 0.96 |
| Other | 220.741 | 7 | 0.001 | 0.064 | 0.057–0.072 | 0.017 | 0.989 | 0.976 | 0.86 |
| MDE | |||||||||
| Depression | 1210.246 | 42 | 0.001 | 0.072 | 0.069–0.076 | 0.034 | 0.954 | 0.939 | 0.89 |
| GA | |||||||||
| Anxiety | 74.940 | 5 | 0.001 | 0.043 | 0.035–0.052 | 0.005 | 0.998 | 0.995 | 0.93 |
| PCL-5 | |||||||||
| Re-experimentation | 15.073 | 4 | 0.005 | 0.024 | 0.012–0.038 | 0.008 | 0.999 | 0.997 | 0.86 |
| NACM | 229.317 | 10 | 0.001 | 0.068 | 0.061–0.076 | 0.020 | 0.983 | 0.964 | 0.86 |
| Hyperarousal | 200.198 | 8 | 0.001 | 0.071 | 0.063–0.080 | 0.030 | 0.972 | 0.947 | 0.78 |
| PTSD | 4535.593 | 162 | 0.001 | 0.076 | 0.074–0.078 | 0.044 | 0.916 | 0.901 | 0.93 |
| TOTAL | |||||||||||||||
| n | % | ||||||||||||||
| 7420 | 100 | ||||||||||||||
| Victimizing Interpersonal Violence | Victimizing Intimate Violence | ||||||||||||||
| n | % | n | % | ||||||||||||
| 1853 | 25.00 | 1874 | 25.26 | ||||||||||||
| Men | Women | High school | University | Men | Women * | High school | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 579 | 25.02 | 1274 | 24.95 | 407 | 24.10 | 1446 | 25.23 | 515 | 22.26 | 1359 | 26.62 | 427 | 25.28 | 1447 | 25.25 |
| Perpetrating Interpersonal Violence | Perpetrating Intimate Violence | ||||||||||||||
| n | % | n | % | ||||||||||||
| 1742 | 23.48 | 1141 | 15.38 | ||||||||||||
| Men | Women | High school | University | Men | Women * | High school | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 532 | 22.99 | 1210 | 23.70 | 384 | 22.73 | 1358 | 23.70 | 315 | 13.61 | 826 | 16.18 | 253 | 14.98 | 888 | 15.49 |
| Harmful tobacco use | Harmful alcohol use | ||||||||||||||
| n | % | n | % | ||||||||||||
| 1919 | 25.90 | 1497 | 20.20 | ||||||||||||
| Men * | Women | High school * | University | Men * | Women | High school * | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 683 | 29.50 | 1236 | 24.20 | 498 | 29.50 | 1421 | 24.80 | 547 | 23.60 | 950 | 18.60 | 371 | 22.00 | 1126 | 19.60 |
| Harmful cannabis use | Harmful cocaine use | ||||||||||||||
| n | % | n | % | ||||||||||||
| 927 | 12.50 | 137 | 1.80 | ||||||||||||
| Men * | Women | High school * | University | Men * | Women | High school * | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 365 | 15.80 | 562 | 11.00 | 239 | 14.20 | 688 | 12.00 | 62 | 2.70 | 75 | 1.50 | 48 | 2.80 | 89 | 1.60 |
| Harmful stimulant use | Harmful inhalant use | ||||||||||||||
| n | Total % | n | % | ||||||||||||
| 57 | 0.80 | 22 | 0.30 | ||||||||||||
| Men * | Women | High school * | University | Men | Women | High school | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 26 | 1.10 | 31 | 0.60 | 22 | 1.30 | 35 | 0.60 | 10 | 0.40 | 12 | 0.20 | 8 | 0.50 | 14 | 0.20 |
| Harmful sedative use | Harmful hallucinogen use | ||||||||||||||
| n | % | n | % | ||||||||||||
| 357 | 4.80 | 203 | 2.70 | ||||||||||||
| Men | Women * | High school | University | Men * | Women | High school | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 81 | 3.50 | 276 | 5.40 | 84 | 5.00 | 273 | 4.80 | 85 | 3.70 | 118 | 2.30 | 56 | 3.30 | 147 | 2.60 |
| Harmful opioid use | Harmful use of other drugs | ||||||||||||||
| n | % | n | % | ||||||||||||
| 8 | 0.10 | 100 | 1.30 | ||||||||||||
| Men | Women | High school | University | Men | Women | High school | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 3 | 0.10 | 5 | 0.10 | 2 | 0.10 | 6 | 0.10 | 32 | 1.40 | 68 | 1.30 | 25 | 1.50 | 75 | 1.30 |
| Polydrug Use | |||||||||||||||
| n | % | ||||||||||||||
| 1405 | 18.93 | ||||||||||||||
| Men * | Women | High school | University | ||||||||||||
| n | % | n | % | n | % | n | % | ||||||||
| 525 | 22.69 | 880 | 17.23 | 352 | 20.84 | 1053 | 18.37 | ||||||||
| Depression | Generalized Anxiety | ||||||||||||||
| n | % | n | % | ||||||||||||
| 3299 | 44.46 | 3553 | 47.90 | ||||||||||||
| Men | Women * | High school * | University | Men | Women * | High school | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 868 | 37.51 | 2431 | 47.61 | 794 | 47.01 | 2505 | 43.71 | 979 | 42.30 | 2574 | 50.40 | 834 | 49.40 | 2719 | 47.40 |
| PTSD symptoms | Comorbidity | ||||||||||||||
| n | % | n | % | ||||||||||||
| 2187 | 29.47 | 2713 | 36.56 | ||||||||||||
| Men | Women * | High school * | University | Men | Women | High school * | University | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % |
| 565 | 24.42 | 1622 | 31.77 | 566 | 33.51 | 1621 | 28.28 | 708 | 30.60 | 2005 | 39.27 | 685 | 40.56 | 2028 | 35.39 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chainé, S.M.; Bacigalupe, G.; García, R.R.; Montoya, A.L.; Romero, V.F.; Gispert, M.A.I. Interpersonal and Intimate Violence in Mexican Youth: Drug Use, Depression, Anxiety, and Stress during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 6484. https://doi.org/10.3390/ijerph20156484
Chainé SM, Bacigalupe G, García RR, Montoya AL, Romero VF, Gispert MAI. Interpersonal and Intimate Violence in Mexican Youth: Drug Use, Depression, Anxiety, and Stress during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(15):6484. https://doi.org/10.3390/ijerph20156484
Chicago/Turabian StyleChainé, Silvia Morales, Gonzalo Bacigalupe, Rebeca Robles García, Alejandra López Montoya, Violeta Félix Romero, and Mireya Atzala Imaz Gispert. 2023. "Interpersonal and Intimate Violence in Mexican Youth: Drug Use, Depression, Anxiety, and Stress during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 15: 6484. https://doi.org/10.3390/ijerph20156484
APA StyleChainé, S. M., Bacigalupe, G., García, R. R., Montoya, A. L., Romero, V. F., & Gispert, M. A. I. (2023). Interpersonal and Intimate Violence in Mexican Youth: Drug Use, Depression, Anxiety, and Stress during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 20(15), 6484. https://doi.org/10.3390/ijerph20156484







