A Review of the Relationship between Socioeconomic Status Change and Health
Abstract
1. Introduction
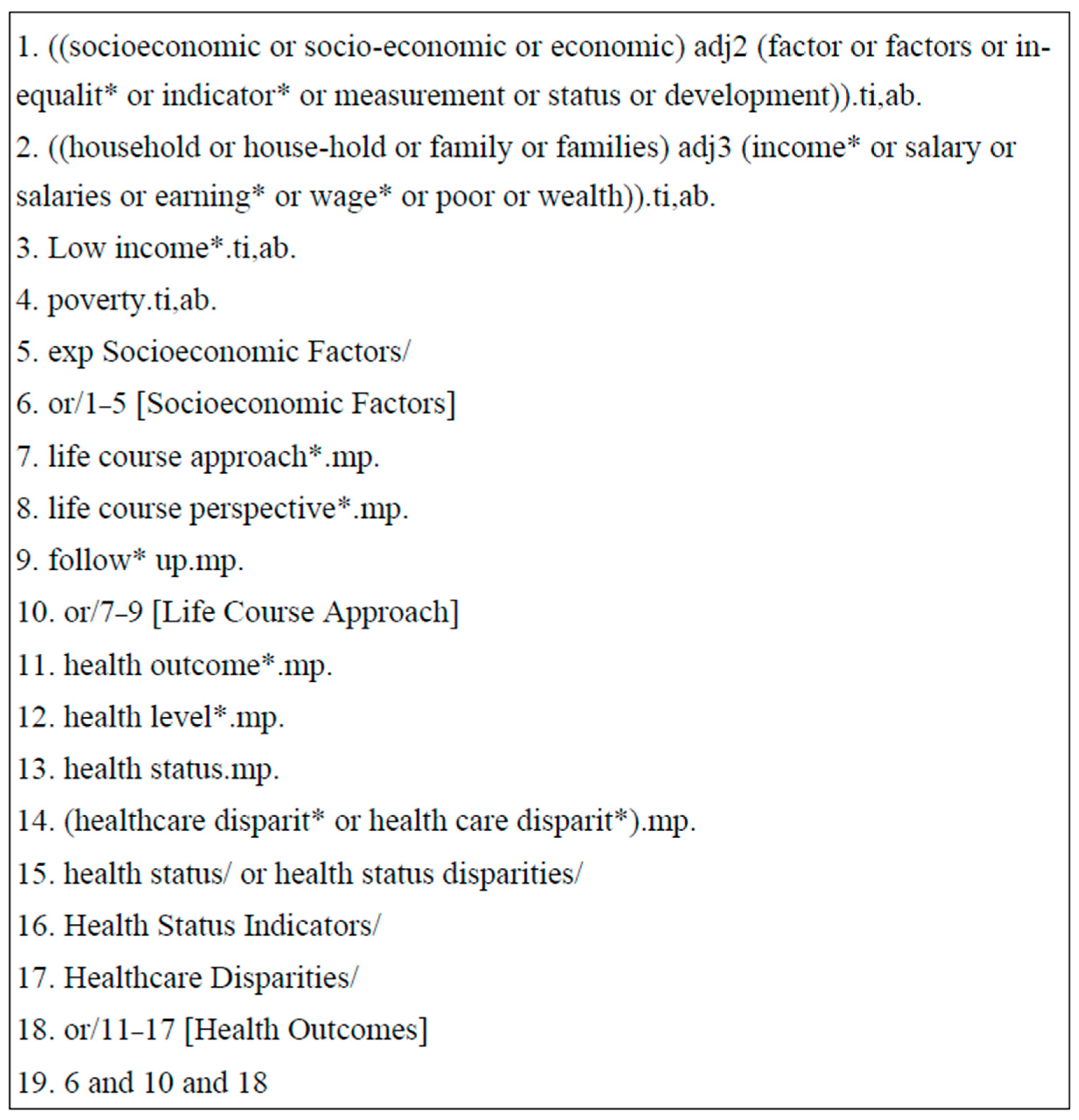
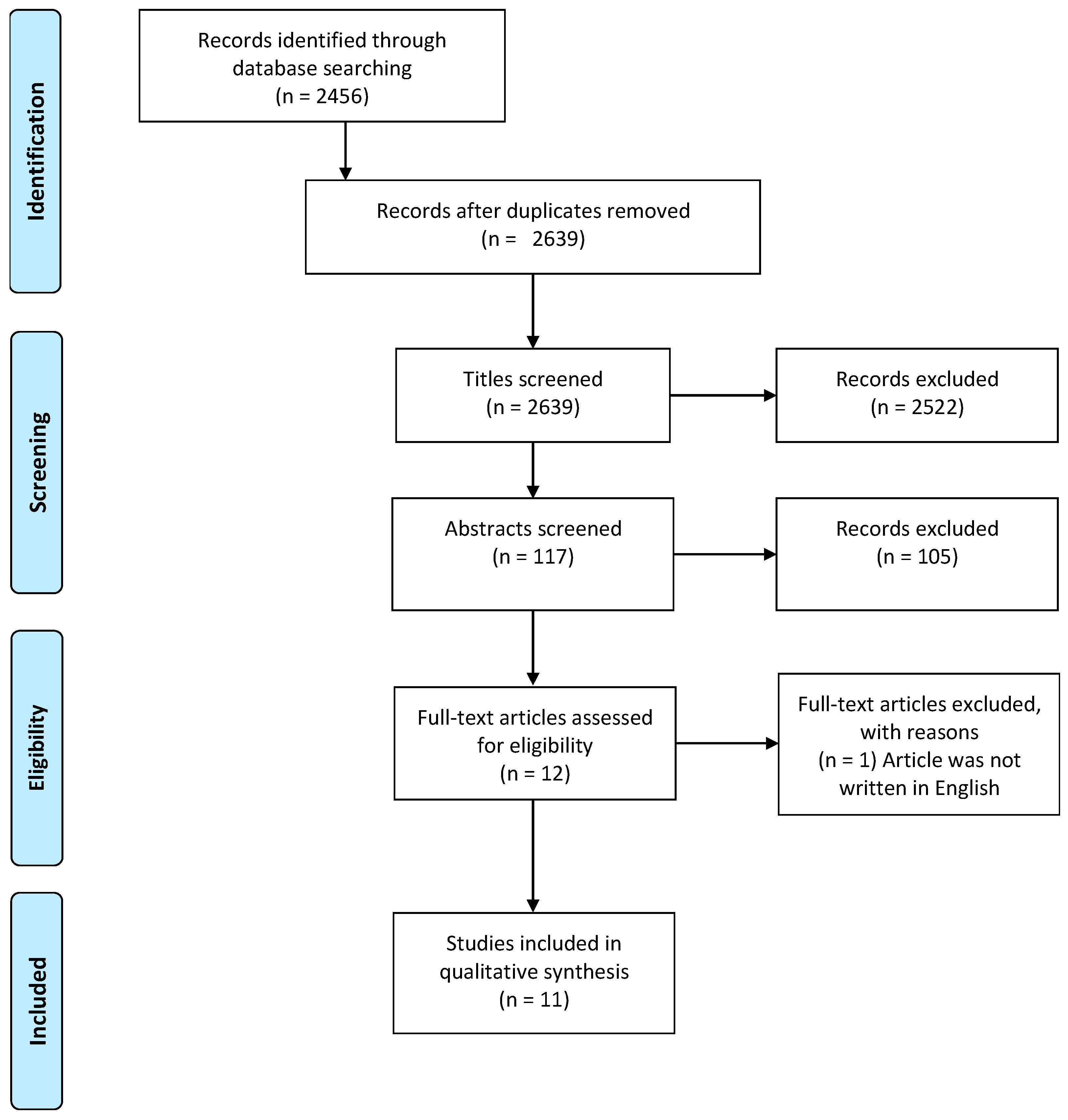
2. Methods
3. Results
- (i)
- SES change and general physical health
- (ii)
- SES change and mental health
- (iii)
- SES changes and cardiovascular health
- (iv)
- SES change and oral health
4. Discussion
5. Limitations
6. Conclusions and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Public Health Services. Available online: http://www.euro.who.int/en/health-topics/Health-systems/public-health-services (accessed on 20 January 2020).
- Clark, A.M.; DesMeules, M.; Luo, W.; Duncan, A.S.; Wielgosz, A. Socioeconomic status and cardiovascular disease: Risks and implications for care. Nat. Rev. Cardiol. 2009, 6, 712–722. [Google Scholar] [CrossRef] [PubMed]
- Arpey, N.C.; Gaglioti, A.H.; Rosenbaum, M.E. How Socioeconomic Status Affects Patient Perceptions of Health Care: A Qualitative Study. J. Prim. Care Community Health 2017, 8, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Fritzell, J.; Nermo, M.; Lundberg, O. The impact of income: Assessing the relationship between income and health in Sweden. Scand. J. Public Health 2004, 32, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Winkleby, M.A.; Jatulis, D.E.; Frank, E.; Fortmann, S.P. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. Am. J. Public Health 1992, 82, 816–820. [Google Scholar] [CrossRef] [PubMed]
- Goodman, E.; Slap, G.B.; Huang, B. The public health impact of socioeconomic status on adolescent depression and obesity. Am. J. Public Health 2003, 93, 1844–1850. [Google Scholar] [CrossRef] [PubMed]
- Hallqvist, J.; Lynch, J.; Bartley, M.; Lang, T.; Blane, D. Can we disentangle life course processes of accumulation, critical period and social mobility? An analysis of disadvantaged socio-economic positions and myocardial infarction in the Stockholm Heart Epidemiology Program. Soc. Sci. Med. 2004, 58, 1555–1562. [Google Scholar] [CrossRef]
- Osypuk, T.L.; Slaughter-Acey, J.C.; Kehm, R.D.; Misra, D.P. Life-course Social Mobility and Reduced Risk of Adverse Birth Outcomes. Am. J. Prev. Med. 2016, 51, 975–982. [Google Scholar] [CrossRef]
- Alvarado, B.E.; Zunzunegui, M.V.; Béland, F.; Bamvita, J.M. Life course social and health conditions linked to frailty in Latin American older men and women. J. Gerontol. A Biol. Sci. Med. Sci. 2008, 63, 1399–1406. [Google Scholar] [CrossRef]
- Cundiff, J.M.; Boylan, J.M.; Pardini, D.A.; Matthews, K.A. Moving up matters: Socioeconomic mobility prospectively predicts better physical health. Health Psychol. 2017, 36, 609–617. [Google Scholar] [CrossRef]
- Baldassari, A.R.; Cleveland, R.J.; Callahan, L.F. Independent associations of childhood and current socioeconomic status with risk of self-reported doctor-diagnosed arthritis in a family-medicine cohort of North-Carolinians. BMC Musculoskelet. Disord. 2013, 14, 327. [Google Scholar] [CrossRef]
- Robertson, T.; Popham, F.; Benzeval, M. Socioeconomic position across the lifecourse & allostatic load: Data from the West of Scotland Twenty-07 cohort study. BMC Public Health 2014, 14, 184. [Google Scholar]
- Padyab, M.; Norberg, M. Socioeconomic inequalities and body mass index in Vasterbotten County, Sweden: A longitudinal study of life course influences over two decades. Int. J. Equity Health 2014, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Barros, F.C.; Matijasevich, A.; Santos, I.S.; Horta, B.L.; da Silva, B.G.C.; Munhoz, T.N.; Fazel, S.; Stein, A.; Pearson, R.M.; Anselmi, L.; et al. Social inequalities in mental disorders and substance misuse in young adults: A birth cohort study in Southern Brazil. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 717–726. [Google Scholar] [CrossRef]
- Kaplan, G.A.; Shema, S.J.; Leite, C.M. Socioeconomic determinants of psychological well-being: The role of income, income change, and income sources during the course of 29 years. Ann. Epidemiol. 2008, 18, 531–537. [Google Scholar] [CrossRef]
- Ahrens, K.R.; Garrison, M.M.; Courtney, M.E. Health outcomes in young adults from foster care and economically diverse backgrounds. Pediatrics 2014, 134, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Kamphuis, C.B.; Turrell, G.; Giskes, K.; Mackenbach, J.P.; Van Lenthe, F.J. Socioeconomic inequalities in cardiovascular mortality and the role of childhood socioeconomic conditions and adulthood risk factors: A prospective cohort study with 17-years of follow up. BMC Public Health 2012, 12, 1045. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N.; Chen, J.T.; Coull, B.A.; Selby, J.V. Lifetime socioeconomic position and twins’ health: An analysis of 308 pairs of United States women twins. PLoS Med. 2005, 2, e162. [Google Scholar] [CrossRef]
- Thomson, W.M.; Poulton, R.; Milne, B.J.; Caspi, A.; Broughton, J.R.; Ayers, K.M.S. Socioeconomic inequalities in oral health in childhood and adulthood in a birth cohort. Community Dent. Oral Epidemiol. 2004, 32, 345–353. [Google Scholar] [CrossRef]
- Pickett, K.E.; Wilkinson, R.G. Inequality: An underacknowledged source of mental illness and distress. Br. J. Psychiatry 2010, 197, 426–428. [Google Scholar] [CrossRef]
- De Hert, M.; Detraux, J.; Vancampfort, D. The intriguing relationship between coronary health disease and mental disorders. Dialogues Clin. Neurosci. 2018, 20, 31–40. [Google Scholar] [CrossRef]
- Newton, S.; Braithwaite, D.; Akinyemiju, F.T. Socio-economic status over the life course and obesity: Systematic revire and meta-analysis. PLoS ONE 2017, 12, e0177151. [Google Scholar] [CrossRef] [PubMed]
- Ball, K.; Crawford, D. Socioeconomic status and weight change in adults: A review. Soc. Sci. Med. 2005, 60, 1987–2010. [Google Scholar] [PubMed]
- Mochari-Greenberger, H.; Mills, T.; Simpson, S.L.; Mosca, L. Knowledge, preventive action, and barriers to cardiovascular disease prevention by race and ethnicity in women: An American Heart Association national survey. J. Womens Health 2010, 19, 1243–1249. [Google Scholar] [CrossRef]
- Dorfer, C.; Benz, C.; Aida, J.; Campard, G. The relationship of oral health with general health and NCDs: A brief review. Int. Dent. J. 2017, 67 (Suppl. 2), 14–18. [Google Scholar] [PubMed]
| Author, Year | Study Design * | Country | n | Time Period | Exposure & Outcome Measures | Main Findings |
|---|---|---|---|---|---|---|
| Ahrens et al., 2014 [16] | P | USA | 2513 youths & adolescents | 17/18 to 25/26 years | Education, economic insecurity, physical health | Consistent pattern of increased health risk, BMI, and hypertension in relation to change from economically secure to insecure. |
| Alvarado et al., 2008 [9] | C | Seven Latin American and Caribbean (LAC) cities | 10,661 men and women over the age of 60 years | Retrospective data for participants over the age of 60 years | Gender, family economics, times of hunger, education, occupation, income, marital status & self-rated health | Those who had experienced impoverished childhoods were more likely to be frail. Those of low education, manual occupation, and perceived economic hardship later in life were related to greater likelihood of frailty after 60 years of age. |
| Baldassari et al., 2013 [11] | C | USA | 1276 | Retrospective data for participants between 22 and 94 years (mean = 57 years) | Age, ethnicity, gender, BMI, self and parental homeownership and occupation, education & Arthritis | The relationship between SES and arthritis was greatest in groups that fell from middle to low SES, followed by always low, and lastly low to middle SES. The risk of developing arthritis was 2 times greater for individuals who fell from high to low SES but not statistically significant due to small sample size. |
| Barros et al., 2018 [14] | R | Brazil | 3701 | 30-year follow-up | Family income, delivery payment mode, mother’s schooling, height, skin color & Mental health | Low SES was linked with mental disorders, suicide attempts, and alcohol misuse. Never poor had the lowest prevalence. Individuals whose families started their life as poor but then improved their SES by age 30 had lower prevalence than those who started off in a better SES and became poor. |
| Cundiff et al., 2017 [10] | P | USA | 1165 males | Students attending first grade were assessed every 6 months for the first 4 years and then annually for 9 years | Hollingshead Index (marital status, retired/employed status, educational, and occupational prestige) & Physical health | Upward mobility of SES has a protective effect on physical health, independent of baseline childhood SES, current adult SES, race, physical childhood health, and child and adolescent BMI. Increase in SES has an additive protective effect over time. |
| Kamphuis et al., 2012 [17] | R | Netherlands | 27,027 | 17-year follow-up | Education, occupation of father, type of health insurance, car ownership, housing tenure, and financial problems with paying bills & Physical health | When adjusted, adulthood SES had significantly greater contribution to cardiovascular disease (CVD) mortality independent of childhood SES. Most of the association with childhood SES was its contribution to adulthood risk factors. Those with greater adulthood material had a lower risk of CVD mortality. |
| Kaplan et al., 2008 [15] | R | USA | 1127 | Four data collection periods between 1965 and 1999 | Mean income, Income slope, and income sources & Mental health | Average income, income increases, and receipt of profit income were positively associated with higher purpose in life, self-acceptance, personal growth, and environmental mastery (mental health). Profit income positively associated with psychological well-being |
| Krieger et al., 2005 [18] | R | USA | 352 twin pairs | 0–14 years | Adult household class, father’s education level, adult education level & Physical health | Poorer health was more likely to be reported in the working-class twin. Cardiovascular health differed among discordant twins based on their adulthood socioeconomic position. Those who experienced cumulative deprivation had the worst health. |
| Padyab & Norberg, 2014 [13] | R | Sweden | 3440 | 60+ years | Education, and Occupational class & Physical health (BMI) | The social mobility model was rejected when looking at SES and BMI. Findings supported the accumulation and critical period models of SES and BMI for women |
| Robertson et al., 2014 [12] | R | Scotland | 2580 | 20-year period | Head of household occupational social class at age 15 & adulthood, highest education attained & Physical health | Those who had higher socioeconomic position (SEP) during all 3 examined life-stages had the lowest mean allostatic load. Highest allostatic load was seen in individuals who had a higher childhood SEP followed by lower SEP in the 2 remaining life-stages. The greater SEP accumulation over time the lower the allostatic load. |
| Thomson et al., 2004 [19] | P | New Zealand | 1037 | Assessments conducted at ages 0, 3, 5, and 26 years | Parental occupational class, adult occupational class & Physical health | The severity of dental caries (mean Decayed and Filled primary dental Surfaces (DFS)) was lowest in the low to high SES trajectory group and highest in the low-to-low group. Mean dental caries were lowest to highest as follows: high to high, low to high, high to low, low to low. Upward mobility hypothesis is supported as those who rose from low to high SES had the best oral health outcomes second to those that were high to high. Downward mobility was also supported as high to low had the worse oral health second to low to low SES. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barakat, C.; Konstantinidis, T. A Review of the Relationship between Socioeconomic Status Change and Health. Int. J. Environ. Res. Public Health 2023, 20, 6249. https://doi.org/10.3390/ijerph20136249
Barakat C, Konstantinidis T. A Review of the Relationship between Socioeconomic Status Change and Health. International Journal of Environmental Research and Public Health. 2023; 20(13):6249. https://doi.org/10.3390/ijerph20136249
Chicago/Turabian StyleBarakat, Caroline, and Theodore Konstantinidis. 2023. "A Review of the Relationship between Socioeconomic Status Change and Health" International Journal of Environmental Research and Public Health 20, no. 13: 6249. https://doi.org/10.3390/ijerph20136249
APA StyleBarakat, C., & Konstantinidis, T. (2023). A Review of the Relationship between Socioeconomic Status Change and Health. International Journal of Environmental Research and Public Health, 20(13), 6249. https://doi.org/10.3390/ijerph20136249







