The Function of Bed Management in Pandemic Times—A Case Study of Reaction Time and Bed Reconversion
Abstract
1. Introduction
An Italian Case Study
2. Materials and Methods
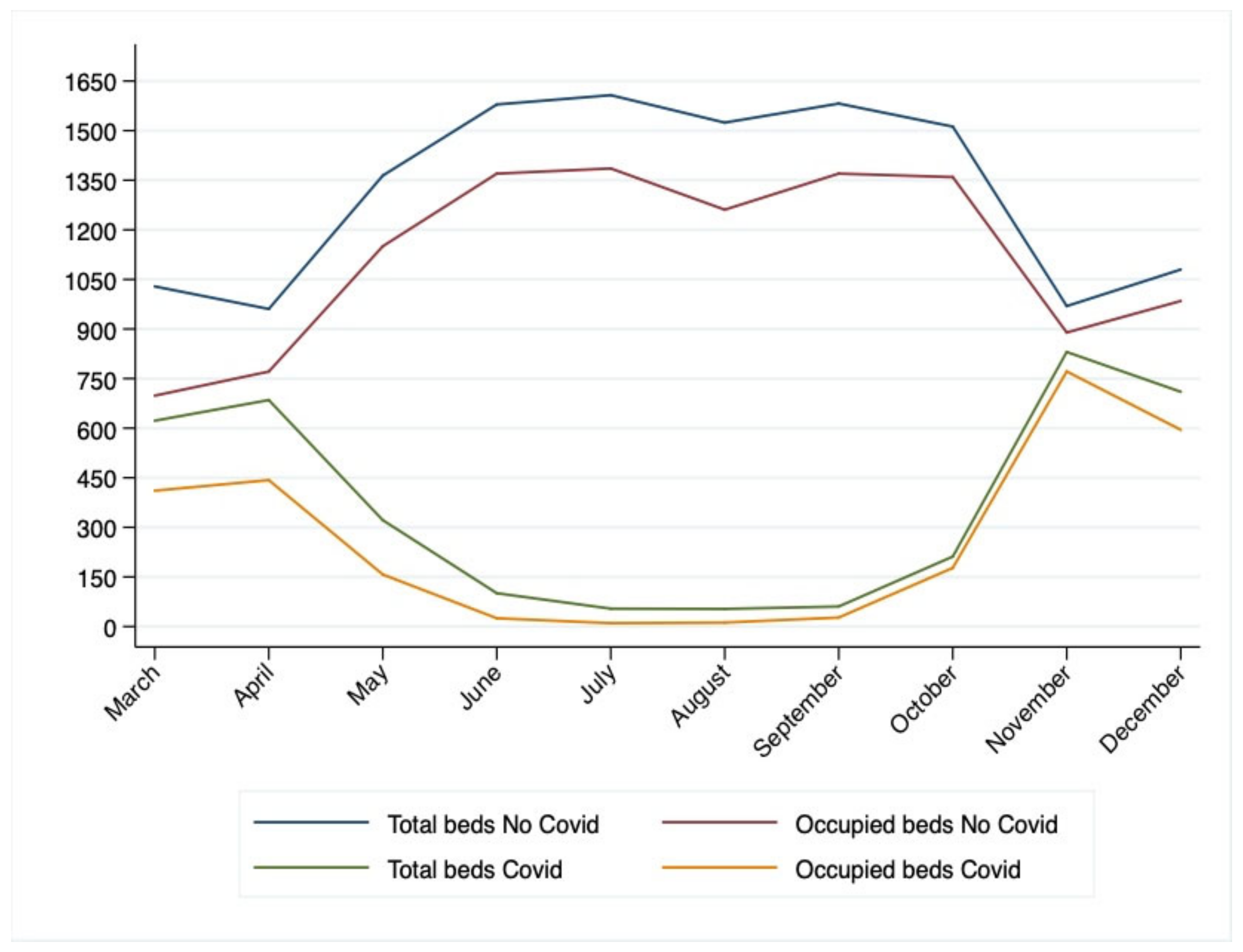
3. Results
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Howell, E.; Bessman, E.; Kravet, S.; Kolodner, K.; Marshall, R.; Wright, S. Active bed management by hospitalists and emergency department throughput. Ann. Intern. Med. 2008, 149, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Boaden, R.; Proudlove, N.; Wilson, M. An exploratory study of bed management. J. Manag. Med. 1999, 13, 234–250. [Google Scholar] [CrossRef] [PubMed]
- Proudlove, N.; Boaden, R.; Jorgensen, J. Developing bed managers: The why and the how. J. Nurs. Manag. 2007, 15, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Balaji, R.; Brownlee, M. Bed Management Optimization. Infosys. 2009. Available online: https://www.infosys.com/industries/healthcare/documents/hospital-bed-management.pdf (accessed on 5 March 2023).
- He, L.; Madathil, S.C.; Oberoi, A.; Servis, G.; Khasawneh, M.T. A systematic review of research design and modeling techniques in inpatient bed management. Comput. Ind. Eng. 2019, 127, 451–466. [Google Scholar] [CrossRef]
- Schroeder, R.G.; Goldstein, S.M.; Rungtusanatham, M.J. Operations Management; McGraw-Hill: New York, NY, USA, 1993; Volume 1081. [Google Scholar]
- OECD. Health at a Glance; Organisation for Economic Co-Operation and Development: Paris, France, 2019. [Google Scholar]
- OECD. Health at a Glance 2020; Organisation for Economic Co-Operation and Development: Paris, France, 2020. [Google Scholar]
- Goic, M.; Bozanic-Leal, M.S.; Badal, M.; Basso, L.J. COVID-19: Short-term forecast of ICU beds in times of crisis. PLoS ONE 2021, 16, e0245272. [Google Scholar] [CrossRef] [PubMed]
- Bosa, I.; Castelli, A.; Castelli, M.; Ciani, O.; Compagni, A.; Galizzi, M.M.; Garofano, M.; Ghislandi, S.; Giannoni, M.; Marini, G.; et al. Response to COVID-19: Was Italy (un) prepared? Health Econ. Policy Law 2021, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Pecoraro, F.; Clemente, F.; Luzi, D. The Efficiency in the Ordinary Hospital Bed Management in Italy: An In-Depth Analysis of Intensive Care Unit in the Areas Affected by COVID-19 Before the Outbreak. PLos ONE 2020, 15, e0239249. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Úbeda, E.F.; Sánchez-Martín, P.; Torrego-Ellacuría, M.; Del Rey-Mejías, Á.; Morales-Contreras, M.F.; Puerta, J.-L. Flexibility and Bed Margins of the Community of Madrid’s Hospitals During the First Wave of the SARS-CoV-2 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 3510. [Google Scholar] [CrossRef] [PubMed]
- Calabuig, J.M.; Jiménez-Fernández, E.; Sánchez-Pérez, E.A.; Manzanares, S. Modeling Hospital Resource Management During the COVID-19 Pandemic: An Experimental Validation. Econometrics 2021, 9, 38. [Google Scholar] [CrossRef]
- Agnoletti, V.; Russo, E.; Circelli, A.; Benni, M.; Bolondi, G.; Martino, C.; Santonastaso, D.P.; Brogi, E.; Pratico, B.; Coccolini, F.; et al. From intensive care to step-down units: Managing patients throughput in response to COVID-19. Int. J. Qual. Health Care 2021, 33, mzaa091. [Google Scholar] [CrossRef] [PubMed]
- Trentini, F.; Marziano, V.; Guzzetta, G.; Tirani, M.; Cereda, D.; Poletti, P.; Piccarreta, R.; Barone, A.; Preziosi, G.; Arduini, F.; et al. Pressure on the Health-Care System and Intensive Care Utilization During the COVID-19 Outbreak in the Lombardy Region of Italy: A Retrospective Observational Study in 43,538 Hospitalized Patients. Am. J. Epidemiol. 2022, 191, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Tarrac, S.E. Application of the updated CDC isolation guidelines for health care facilities. AORN J. 2008, 87, 534–546. [Google Scholar] [CrossRef] [PubMed]
- Stake, R.E. The Art of Case Study Research; SAGE Publishing: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Nicholls, S.G.; Quach, P.; von Elm, E.; Guttmann, A.; Moher, D.; Petersen, I.; Sørensen, H.T.; Smeeth, L.; Langan, S.M.; Benchimol, E.I. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement: Methods for arriving at consensus and developing reporting guidelines. PLoS ONE 2015, 10, e0125620. [Google Scholar] [CrossRef] [PubMed]
- OECD. Health at a Glance 2021; Organisation for Economic Co-operation and Development: Paris, France, 2021. [Google Scholar] [CrossRef]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef] [PubMed]
- WHO. Hospital Readiness Checklist for COVID-19; Interim Version 24 February 2020; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Wei, E.K.; Long, T.; Katz, M.H. Nine lessons learned from the COVID-19 pandemic for improving hospital care and health care delivery. JAMA Intern. Med. 2021, 181, 1161–1163. [Google Scholar] [CrossRef] [PubMed]
- Griffin, K.M.; Karas, M.G.; Ivascu, N.S.; Lief, L. Hospital preparedness for COVID-19: A practical guide from a critical care perspective. Am. J. Respir. Crit. Care Med. 2020, 201, 1337–1344. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, J.; Soutar, G.; Mazzarol, T. Factors Enhancing the Effect of Word of Mouth on Consumer Outcomes. Eur. J. Mark. 2006, 42, 344–364. [Google Scholar] [CrossRef]
| Year | Acute Beds | Occupancy Days | ED Accesses | Surgeries | Outpatient Services |
|---|---|---|---|---|---|
| 2020 | 2735 | 668,094 | 416,566 | 58,786 | 22,734,702 |
| Setting | Admitted | Deceased | In-Hospital Mortality |
|---|---|---|---|
| Intermediate care | 1124 | 46 | 4% |
| Inpatient | 5470 | 549 | 10% |
| ICU-sub ICU | 504 | 147 | 29% |
| Total | 7098 | 742 | 10% |
| Month | Hospital COVID Readmissions from Intermediate Care |
|---|---|
| March | 0 |
| April | 15 |
| May | 26 |
| June | 17 |
| July | 1 |
| August | 0 |
| September | 1 |
| October | 6 |
| November | 5 |
| December | 17 |
| Timing | Month | Setting | COVID Total Beds | BOR COVID | No-COVID Total Beds | BOR No-COVID |
|---|---|---|---|---|---|---|
| Wave 1 | 3-May | Intermediate care | 35 | 35% | 0 | 0% |
| Wave 1 | 3-May | Inpatients | 449 | 71% | 954 | 68% |
| Wave 1 | 3-May | ICU-sub ICU | 146 | 57% | 75 | 63% |
| Wave 1 | 4-April | Intermediate care | 90 | 83% | 0 | 0% |
| Wave 1 | 4-April | Inpatients | 454 | 66% | 895 | 81% |
| Wave 1 | 4-April | ICU-sub ICU | 141 | 48% | 65 | 67% |
| Wave 1 | 5-May | Intermediate care | 123 | 69% | 14 | 64% |
| Wave 1 | 5-May | Inpatients | 241 | 50% | 1136 | 88% |
| Wave 1 | 5-May | ICU-sub ICU | 63 | 39% | 109 | 70% |
| Interval | 5-May | Intermediate care | 94 | 51% | 33 | 56% |
| Interval | 5-May | Inpatients | 86 | 33% | 1321 | 84% |
| Interval | 5-May | ICU-sub ICU | 44 | 27% | 118 | 75% |
| Interval | 6-June | Intermediate care | 41 | 39% | 53 | 57% |
| Interval | 6-June | Inpatients | 41 | 23% | 1383 | 89% |
| Interval | 6-June | ICU-sub ICU | 23 | 6% | 143 | 75% |
| Interval | 7-July | Intermediate care | 0 | 0% | 52 | 51% |
| Interval | 7-July | Inpatients | 32 | 31% | 1408 | 89% |
| Interval | 7-July | ICU-sub ICU | 22 | 0% | 147 | 71% |
| Interval | 8-August | Intermediate care | 0 | 0% | 38 | 58% |
| Interval | 8-August | Inpatients | 31 | 37% | 1340 | 85% |
| Interval | 8-August | ICU-sub ICU | 22 | 2% | 145 | 67% |
| Interval | 9-September | Intermediate care | 0 | 0% | 39 | 81% |
| Interval | 9-September | Inpatients | 34 | 59% | 1378 | 87% |
| Interval | 9-September | ICU-sub ICU | 22 | 16% | 144 | 72% |
| Wave 2 | 9-September | Intermediate care | 0 | 0% | 57 | 65% |
| Wave 2 | 9-September | Inpatients | 41 | 63% | 1401 | 90% |
| Wave 2 | 9-September | ICU-sub ICU | 24 | 19% | 144 | 76% |
| Wave 2 | 10-October | Intermediate care | 40 | 90% | 72 | 80% |
| Wave 2 | 10-October | Inpatients | 167 | 90% | 1305 | 92% |
| Wave 2 | 10-October | ICU-sub ICU | 37 | 55% | 136 | 78% |
| Wave 2 | 11-November | Intermediate care | 100 | 98% | 45 | 99% |
| Wave 2 | 11-November | Inpatients | 626 | 93% | 828 | 93% |
| Wave 2 | 11-November | ICU-sub ICU | 104 | 86% | 96 | 78% |
| Wave 2 | 12-December | Intermediate care | 118 | 94% | 45 | 82% |
| Wave 2 | 12-December | Inpatients | 493 | 83% | 938 | 93% |
| Wave 2 | 12-December | ICU-sub ICU | 100 | 78% | 96 | 80% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barchielli, C.; Vainieri, M.; Seghieri, C.; Salutini, E.; Zoppi, P. The Function of Bed Management in Pandemic Times—A Case Study of Reaction Time and Bed Reconversion. Int. J. Environ. Res. Public Health 2023, 20, 6179. https://doi.org/10.3390/ijerph20126179
Barchielli C, Vainieri M, Seghieri C, Salutini E, Zoppi P. The Function of Bed Management in Pandemic Times—A Case Study of Reaction Time and Bed Reconversion. International Journal of Environmental Research and Public Health. 2023; 20(12):6179. https://doi.org/10.3390/ijerph20126179
Chicago/Turabian StyleBarchielli, Chiara, Milena Vainieri, Chiara Seghieri, Eleonora Salutini, and Paolo Zoppi. 2023. "The Function of Bed Management in Pandemic Times—A Case Study of Reaction Time and Bed Reconversion" International Journal of Environmental Research and Public Health 20, no. 12: 6179. https://doi.org/10.3390/ijerph20126179
APA StyleBarchielli, C., Vainieri, M., Seghieri, C., Salutini, E., & Zoppi, P. (2023). The Function of Bed Management in Pandemic Times—A Case Study of Reaction Time and Bed Reconversion. International Journal of Environmental Research and Public Health, 20(12), 6179. https://doi.org/10.3390/ijerph20126179





