The Impact of the Organization of Public Health Systems on the Ability of Countries to Resist the COVID-19 Pandemic: The Experience of Developed Countries of the World and Ukraine
Abstract
:1. Introduction
1.1. Literature Review
1.2. Analysis of the Organization of the Healthcare Sector: The Experience of Developed Countries of the World and Ukraine
- –
- Budget (state) financing, which is known as the Beveridge model (Great Britain, Denmark, Norway, Finland, Sweden, Australia);
- –
- Social compulsory health insurance, which is also called the Bismarck model (Germany, France, Switzerland);
- –
- Private health insurance, which is known in scientific literature as a market or private model (USA) [21].
- –
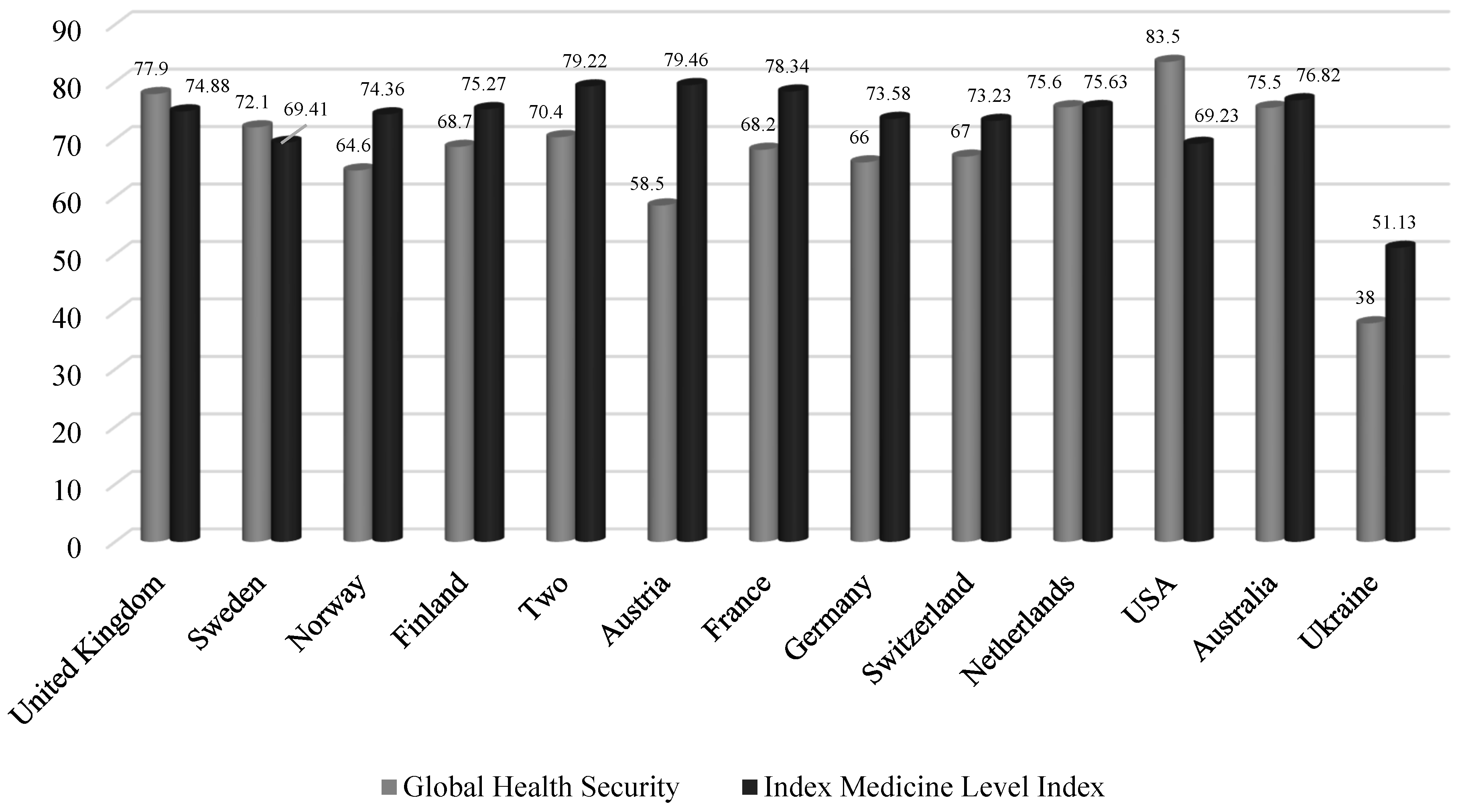
- 67.0–83.5—the most prepared countries;
- –
- 40.3–66.0—more prepared countries;
- –
- 16.2–33.0—the least prepared countries.
2. Materials and Methods
- The number of cases of infection since the beginning of the pandemic;
- The number of deaths caused by coronavirus infection;
- The number of laboratory tests performed to detect the presence of the COVID-19 virus;
- The number of persons who have recovered;
- Number of new cases of diseases per day; the number of deaths per day;
- Percentage of the vaccinated population (1 dose of vaccine) as of 18 October 2021;
- The number of persons who are sick as of 18 October 2021;
- The number of critical cases.
- (1)
- Normalize the variables and find the correlation matrix of the normalized indicators;
- (2)
- Check the presence of multicollinearity in the entire array of data using the Pearson criterion (the actual value is 52.48, which is greater than the corresponding critical value of 50.99; hence, the multicollinearity phenomenon is present in the array);
- (3)
- Determine the multicollinearity of each variable with the array of data using Fisher’s test and Student’s t-test. The actual values obtained exceed the critical value (2.78) for such pairs of indices as the number of cases of infection since the beginning of the pandemic and the number of persons who have recovered, and the number of new cases of the disease per day.
3. Results
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lyeonov, S.; Bilan, S.; Yarovenko, H.; Ostasz, G.; Kolotilina, O. Country’s health profile: Social, economic, behavioral and healthcare determinants. Econ. Sociol. 2021, 14, 322–340. [Google Scholar] [CrossRef]
- Kuzior, A.; Mańka-Szulik, M.; Marszałek-Kotzur, I. The impact of the Covid-19 pandemic on the economic and psychological condition of individuals and societies. In Proceedings of the 37th International Business Information Management Association (IBIMA), Cordoba, Spain, 30–31 May 2021; pp. 8129–8135. [Google Scholar]
- Crowley, R.; Atiq, O.; Hilden, D.; Financial Profit in Medicine. A Position Paper from the American College of Physicians. Ann. Intern. Med. 2021, 10, 1447–1449. [Google Scholar] [CrossRef] [PubMed]
- Kuzior, A.; Kashcha, M.; Kuzmenko, O.; Lyeonov, S.; Brożek, P. Public health system economic efficiency and COVID-19 resilience. Frontier DEA analysis. Int. J. Environ. Res. Public Health 2022, 19, 14727. [Google Scholar] [CrossRef] [PubMed]
- Tommaso, F.D. The New Italian Legislation on Corporate Governance and Business Crisis. The Impact of Covid—19 on SMEs and the Recent Rules to Mitigate the Effects. Financ. Mark. Inst. Risks 2020, 4, 91–108. [Google Scholar] [CrossRef]
- Ahmed, K.M.F. Procuring Covid-19 Vaccine and the Contemporary Geopolitical Paradigm for Bangladesh. Bus. Ethics Leadersh. 2021, 5, 118–126. [Google Scholar] [CrossRef]
- Kashcha, M.; Kwillinski, A.; Petrenko, K. COVID-19 Vaccination Campaign: A Bibliometric Analysis. Health Econ. Manag. Rev. 2022, 2, 8–16. [Google Scholar] [CrossRef]
- Lopez, B.S.; Alcaide, A.V. Blockchain, AI and IoT to Improve Governance, Financial Management and Control of Crisis: Case Study COVID-19. SocioEcon. Chall. 2020, 4, 78–89. [Google Scholar] [CrossRef]
- Kadar, B.; Reicher, R.Z. Innovations in health care management: The effect of the pandemic on the labour market change. Mark. Manag. Innov. 2020, 4, 120–130. [Google Scholar] [CrossRef]
- Kolosok, S.; Jakubowska, A. Covid-19 and public health administration: Trends and prospects. Health Econ. Manag. Rev. 2020, 1, 69–75. [Google Scholar] [CrossRef]
- Shipko, A.; Demikhova, N.; Pajak, K.; Motrechko, V. Health management at the regional level: Multivariable performance assesment. Health Econ. Manag. Rev. 2021, 2, 8–16. [Google Scholar] [CrossRef]
- Lyeonov, S.V.; Kuzmenko, O.; Koibichuk, V.V.; Rubanov, P.M.; Smiianov, V.A. Behavioral, social, economic and legal dimension of the public health system of Ukrain: Descriptive, canonical and factor analysis. Wiadomosci Lekarskie 2021, 74, 3126–3134. [Google Scholar] [CrossRef]
- Fadel, S.; Rouaski, K.; Zakane, A.; Djerboua, A. Estimating Climate Influence of The Potential Covid-19 Pandemic Spreading in Algeria. SocioEcon. Chall. 2021, 6, 24–40. [Google Scholar] [CrossRef]
- Ober, J.; Karwot, J. The Effect of Publicly Available COVID-19 Information on the Functioning of Society, Businesses, Government and Local Institutions: A Case Study from Poland. Int. J. Environ. Res. Public Health 2023, 20, 2719. [Google Scholar] [CrossRef]
- Hinrichs, G.; Bundtzen, H. Impact of COVID-19 on personal insurance sales—Evidence from Germany. Financ. Mark. Inst. Risks 2021, 5, 80–86. [Google Scholar] [CrossRef]
- International Experience of Reforming the Health Care System (Experience of the European Union Countries). Available online: http://euinfocenter.rada.gov.ua/uploads/documents/29185.pdf (accessed on 10 January 2023).
- World Health Organization. Building Health Systems Resilience for Universal Health Coverage and Health Security during the COVID-19 Pandemic and Beyond: A Brief on the WHO Position; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.uhcpartnership.net/wp-content/uploads/2021/10/WHO-UHL-PHC-SP-2021.02-rus.pdf (accessed on 9 January 2023).
- Shrank, W.; DeParle, N.; Gottlieb, S.; Powers, B.; Wilensky, G.; Orszag, P. Health Costs And Financing. Challenges And Strategies for A New Administration. Health Aff. 2021, 40, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Samoilikova, A.; Kunev, R. The impact of health care financing on the economic growth: EU countries analysis. Health Econ. Manag. Rev. 2020, 1, 24–32. [Google Scholar] [CrossRef]
- Postrzednik-Lotko, K. Managing quality of life in the post-pandemic period. Zesz. Nauk. Politech. Śląskiej. Organ. Zarządzanie 2022, 165, 275–284. [Google Scholar] [CrossRef]
- Klymenko, M. Global experience of financing in the field of medical care. Chernihiv Scientific Journal of the Chernihiv State Institute of Economics and Management. Econ. Manag. 2017, 1, 104–112. [Google Scholar]
- Sabetska, T. Problems and prospects of financial support of the sphere of health care of Ukraine. Econ. Soc. 2001, 27. [Google Scholar] [CrossRef]
- Ukraine: Overview of the Health Care Financing Reform 2016–2019. Available online: https://www.euro.who.int/__data/assets/pdf_file/0018/425340/WHO-WB-Joint-Report_UKR_Full-report_Web.pdf (accessed on 21 December 2022).
- Krynychko, L.; Motailo, O. New approaches to financing the health care system. Asp. Public Adm. 2021, 2, 86–100. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://www.who.int/data/gho/data/indicators (accessed on 7 January 2023).
- Budget Space for the Healthcare System in Ukraine. Available online: https://www.euro.who.int/__data/assets/pdf_file/0003/463872/UKR-Budgetary-space-for-health-ukr.pdf (accessed on 27 December 2022).
- The COVID-19 Coronavirus Pandemic. Available online: https://www.worldometers.info/coronavirus/ (accessed on 17 December 2022).
- Welcome to the 2019 Global Health Security Index. 2019. Available online: https://www.ghsindex.org/ (accessed on 5 January 2023).
- Ranking of Countries by Level of Medicine. Available online: https://www.numbeo.com/health-care/rankings_by_country.jsp (accessed on 10 January 2023).
- Letunovska, N.; Kashcha, M.; Dluhopolskyi, O.; Lyeonov, S.; Artyukhova, N.; Gąsior, M.; Sak-Skowron, M. Health risks and country sustainability: The impact of the COVID-19 pandemic with determining cause-and-effect relationships and their transformations. Sustainability 2023, 15, 222. [Google Scholar] [CrossRef]

| Model | State Spending on Healthcare in GDP, % | Advantages | Disadvantages |
|---|---|---|---|
| Beveridge | 6–10 | the types and prices of medical services are virtually unchanged, as they are determined and controlled by the state; medical services and medical assistance are available to the entire population of the state; technologies for financing healthcare institutions and paying labor in the medical field are quite simple | lack of market instruments; stimulation of economic efficiency in the medical field; low motivation to improve the quality of medical services and medical care; the need for significant budgetary resources to finance the development of the medical field |
| Bismarck | 10–13 | high quality of medical services; redistribution of financial resources depending on the needs of the medical field; availability of medical care for all segments of the population; joint payment of medical care | significant costs for maintaining the insurance infrastructure; extensive system of administrative management; financing of healthcare institutions according to complex schemes |
| Market (private) | more than 10 | stimulating the development of innovative technologies in the medical field; stimulating the improvement of the quality of medical services; stimulation of the intensive activity of medical workers; mobility of financial resources | due to the unregulated market of medical services, uneven access to medical care by representatives of different strata of the population; high cost of medical services; significant expenditure of the people on the development of the healthcare sector; the existence of unfair competition between doctors; lack of state control over the definition of the development of priority areas of healthcare development |
| Country | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|---|---|---|---|---|---|---|---|---|---|
| Beveridge model | ||||||||||
| United Kingdom | 9.8 | 9.8 | 9.9 | 10.0 | 10.0 | 9.9 | 9.9 | 9.8 | 9.9 | 10.2 |
| Denmark | 10.3 | 10.2 | 10.2 | 10.2 | 10.2 | 10.2 | 10.1 | 10.0 | 10.1 | 10.0 |
| Norway | 8.9 | 8.8 | 8.8 | 8.9 | 9.3 | 10.1 | 10.6 | 10.3 | 10.0 | 10.5 |
| Finland | 9.1 | 9.2 | 9.6 | 9.8 | 9.8 | 9.6 | 9.4 | 9.1 | 9.0 | 9.2 |
| Sweden | 8.3 | 10.4 | 10.7 | 10.9 | 10.9 | 10.8 | 10.9 | 10.8 | 10.9 | 10.9 |
| Australia | 8.4 | 8.5 | 8.7 | 8.8 | 9.0 | 9.3 | 9.2 | 9.3 | 9.2 | 9.4 |
| Ukraine | 4.1 | 3.7 | 4.1 | 4.2 | 3.6 | 3.6 | 3.2 | 3.4 | 3.3 | 3.2 |
| Bismarck model | ||||||||||
| Austria | 10.2 | 10.0 | 10.2 | 10.3 | 10.4 | 10.4 | 10.4 | 10.4 | 10.3 | 10.4 |
| France | 11.2 | 11.2 | 11.3 | 11.4 | 11.5 | 11.4 | 11.5 | 11.3 | 11.2 | 11.1 |
| Germany | 11.1 | 10.8 | 10.9 | 11.0 | 11.0 | 11.2 | 11.2 | 11.3 | 11.5 | 11.7 |
| Netherlands | 10.2 | 10.2 | 10.5 | 10.6 | 10.6 | 10.3 | 10.3 | 10.1 | 10.0 | 10.2 |
| Switzerland | 9.9 | 10.0 | 10.2 | 10.5 | 10.6 | 11.0 | 11.3 | 11.5 | 11.2 | 11.3 |
| Market (private) model | ||||||||||
| USA | 16.3 | 16.2 | 16.2 | 16.1 | 16.3 | 16.5 | 16.8 | 16.8 | 16.7 | 16.8 |
| Country | Number of Infection Cases since the Outbreak of the Pandemic | The Number of People Who Are Sick as of 18 October 2021 | Number of Critical Cases | Number of Persons Who Have Recovered | Number of Persons Who Have Recovered per Day | Number of Deaths Caused by COVID-19 | Number of Deaths per Day | Number of Tests Carried out to Detect the Presence of COVID-19 |
|---|---|---|---|---|---|---|---|---|
| United Kingdom | 8,272,883 | 1,369,174 | 780 | 6,765,629 | 41,288 | 13,808 | 136 | 316,222,267 |
| Sweden | 1,161,264 | 1962 | 29 | 1,126,758 | 2097 | 14,886 | 0 | 12,879,376 |
| Norway | 195,029 | 105,193 | 16 | 88,952 | 0 | 884 | 13 | 7,987,971 |
| Finland | 148,672 | 101,563 | 36 | 46 | 0 | 1109 | 9 | 7,238,282 |
| Denmark | 36,584 | 7448 | 18 | 355,718 | 537 | 2674 | 0 | 84,475,994 |
| Austria | 766,542 | 19,842 | 213 | 735,565 | 2128 | 11,135 | 15 | 91,294,829 |
| France | 7,069,089 | 91,344 | 12 | 6,860,572 | 6161 | 117,173 | 23 | 146,046,715 |
| Germany | 4,354,487 | 142,822 | 1336 | 4,116,400 | 101 | 95,265 | 82 | 73,348,901 |
| Switzerland | 852,665 | 38,509 | 132 | 802,995 | 606 | 11,161 | 5 | 11,261,111 |
| Netherlands | 2,033,005 | 6034 | 147 | 1,954,438 | 1733 | 18,227 | 12 | 17,632,552 |
| USA | 45,547,920 | 9,700,690 | 16,141 | 35,107,452 | 10,777 | 739,778 | 1819 | 664,075,307 |
| Australia | 133,446 | 26,372 | 296 | 105,596 | 2125 | 1478 | 17 | 40,307,863 |
| Ukraine | 2,578,394 | 21,451 | 177 | 2,304,361 | 6462 | 59,523 | 471 | 13,379,666 |
| COVID—Param. | COVID—Std. Err | SS | F | t | p | |
|---|---|---|---|---|---|---|
| Intercept | 0.40131 | 0.00734 | 0.05017 | 2893.69 | 54.879 | 0.0023 |
| Tot Cases/1 M | 0.01352 | 0.00613 | 0.00042 | 30.44 | 5.623 | 0.0412 |
| Deaths/1 M | −0.15870 | 0.00954 | 0.01024 | 628.44 | −24.074 | 0.0109 |
| Tests/1 M | −0.07372 | 0.00241 | 0.01911 | 1112.33 | −32.987 | 0.0018 |
| New Cases/1 M | −0.11290 | 0.00612 | 0.00571 | 378.81 | −18.657 | 0.0013 |
| New Death/1 M | 0.05830 | 0.01263 | 0.00042 | 26.70 | 5.450 | 0.0351 |
| Active Cases/1 M | −0.19248 | 0.00889 | 0.00831 | 490.12 | −22.093 | 0.0023 |
| Serious, Crit/1 M | 0.19935 | 0.01667 | 0.00231 | 141.42 | 11.657 | 0.0067 |
| Vaccine/1 M | −0.12704 | 0.01454 | 0.00944 | 26.95 | 5.191 | 0.0041 |
| Model 1 | 0.113780 | 0.015606 | 7.245 | 0.0128 | ||
| Model 2 | −0.09672 | 0.01391 | −7.695 | 0.0113 | ||
| Model 3 | 0.10361 | 0.01518 | 7.281 | 0.0156 |
| Med—Param. | Med—Std. Err | SS | F | t | p | |
|---|---|---|---|---|---|---|
| Intercept | −0.7873 | 0.0483 | 0.0074 | 266.1405 | −16.3138 | 0.0001 |
| The share of public spending on healthcare in GDP | 0.4997 | 0.0280 | 0.0088 | 317.7969 | 17.8269 | 0.0001 |
| The global index of health security | 0.5210 | 0.0191 | 0.0207 | 747.7551 | 27.3451 | 0.0000 |
| Ranking of countries by level of medicine | 0.5251 | 0.0301 | 0.0084 | 303.5455 | 17.4226 | 0.0001 |
| Life expectancy at birth, total (years) | 0.5777 | 0.0404 | 0.0056 | 204.0220 | 14.2836 | 0.0001 |
| Death rate, crude (per 1.000 people) | 0.3705 | 0.0280 | 0.0048 | 174.4985 | 13.2098 | 0.0002 |
| Model 1 | −0.2669 | 0.0147 | −18.1791 | 0.0001 | ||
| Model 2 | −0.2693 | 0.0180 | −14.9381 | 0.0001 | ||
| Model 3 | −0.2510 | 0.0169 | −14.8119 | 0.0001 |
| Country | COVID * | Country | COVID * |
|---|---|---|---|
| United Kingdom | 0.915 | Germany | 0.489 |
| Sweden | 0.502 | Switzerland | 0.584 |
| Norway | 0.421 | Netherlands | 0.574 |
| Finland | 0.431 | USA | 0.772 |
| Denmark | 0.565 | Australia | 0.241 |
| Austria | 1.000 | Ukraine | 0.956 |
| France | 0.379 |
| Country | MED * | Country | MED * |
|---|---|---|---|
| United Kingdom | 0.815 | Germany | 0.616 |
| Sweden | 0.767 | Switzerland | 0.893 |
| Norway | 0.811 | Netherlands | 0.845 |
| Finland | 0.669 | USA | 0.932 |
| Denmark | 0.796 | Australia | 1.000 |
| Austria | 0.719 | Ukraine | 0.000 |
| France | 0.885 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuzior, A.; Vasylieva, T.; Liuta, O.; Deineka, O.; Kashcha, M. The Impact of the Organization of Public Health Systems on the Ability of Countries to Resist the COVID-19 Pandemic: The Experience of Developed Countries of the World and Ukraine. Int. J. Environ. Res. Public Health 2023, 20, 6106. https://doi.org/10.3390/ijerph20126106
Kuzior A, Vasylieva T, Liuta O, Deineka O, Kashcha M. The Impact of the Organization of Public Health Systems on the Ability of Countries to Resist the COVID-19 Pandemic: The Experience of Developed Countries of the World and Ukraine. International Journal of Environmental Research and Public Health. 2023; 20(12):6106. https://doi.org/10.3390/ijerph20126106
Chicago/Turabian StyleKuzior, Aleksandra, Tetiana Vasylieva, Olga Liuta, Olha Deineka, and Mariia Kashcha. 2023. "The Impact of the Organization of Public Health Systems on the Ability of Countries to Resist the COVID-19 Pandemic: The Experience of Developed Countries of the World and Ukraine" International Journal of Environmental Research and Public Health 20, no. 12: 6106. https://doi.org/10.3390/ijerph20126106
APA StyleKuzior, A., Vasylieva, T., Liuta, O., Deineka, O., & Kashcha, M. (2023). The Impact of the Organization of Public Health Systems on the Ability of Countries to Resist the COVID-19 Pandemic: The Experience of Developed Countries of the World and Ukraine. International Journal of Environmental Research and Public Health, 20(12), 6106. https://doi.org/10.3390/ijerph20126106










