Mental Health Issues as a Consequence of the Pandemic: Group Psycho-Educational Intervention to Support Patients Recovered from COVID-19 Infection
Abstract
1. Introduction
1.1. COVID-19 and Mental Health
1.2. Group Psycho-Educational Intervention for Patients Recovered from COVID-19 Infection: Where We Started and the Structure of the Intervention
2. The Current Study: Aims
3. Materials and Methods
3.1. Participants and Data Collection Procedure
3.2. Data Analysis
3.2.1. Corpus Preparation and Text’s Encoding Strings
3.2.2. Thematic Analysis of Elementary Contexts
3.2.3. Correspondence Analysis
4. Results
4.1. Descriptive Statistics
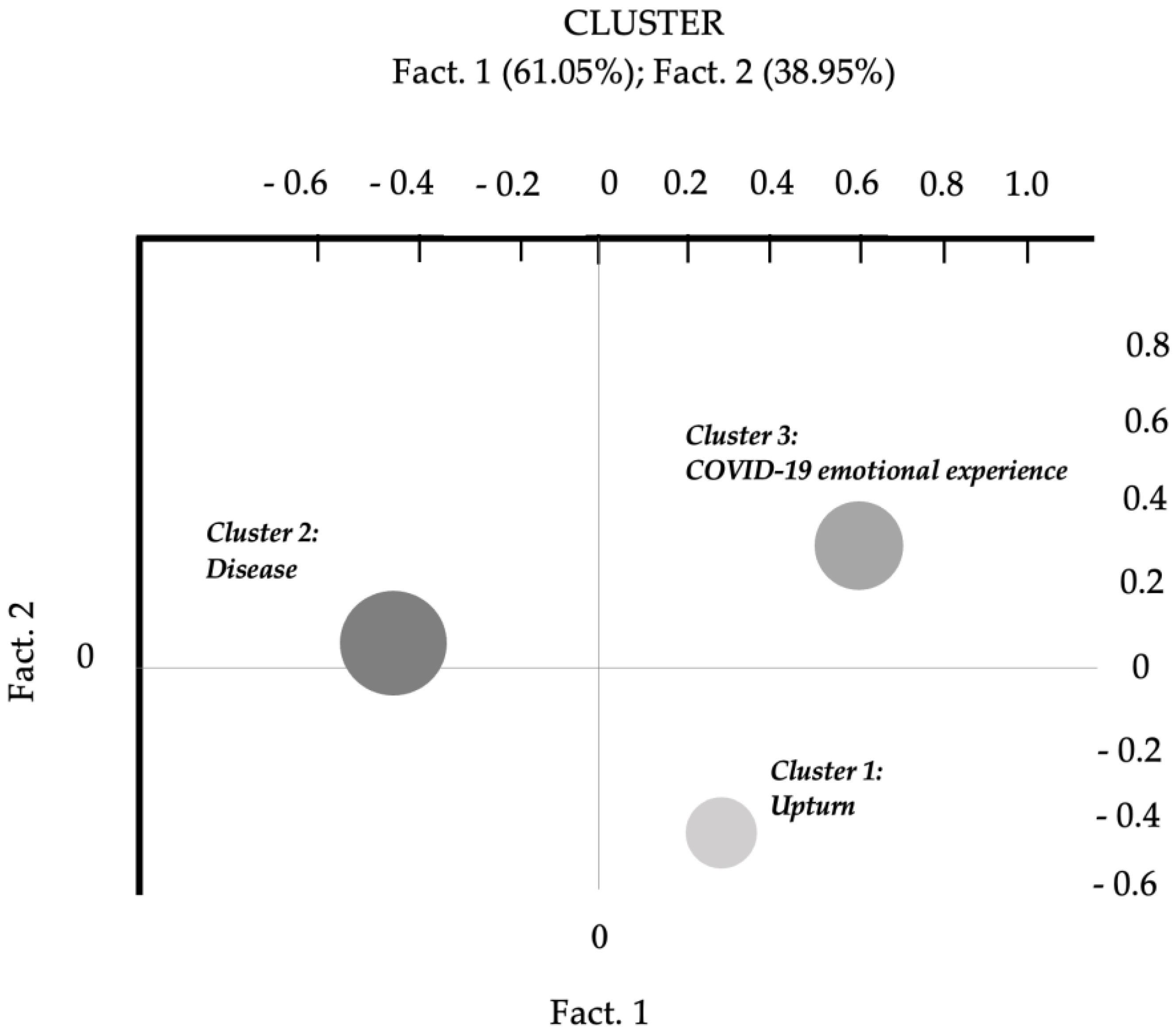
4.2. Thematic Analysis of Elementary Contexts
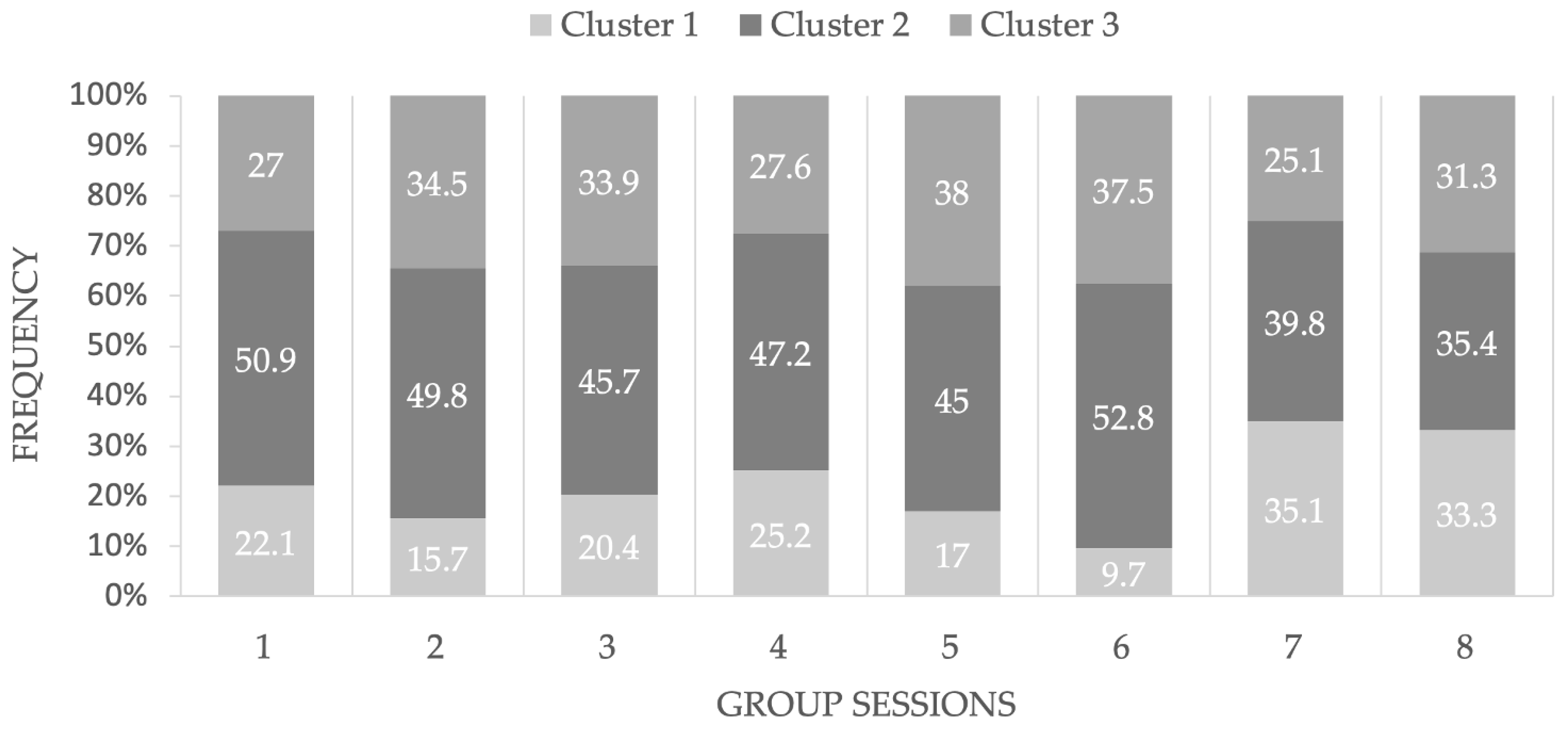
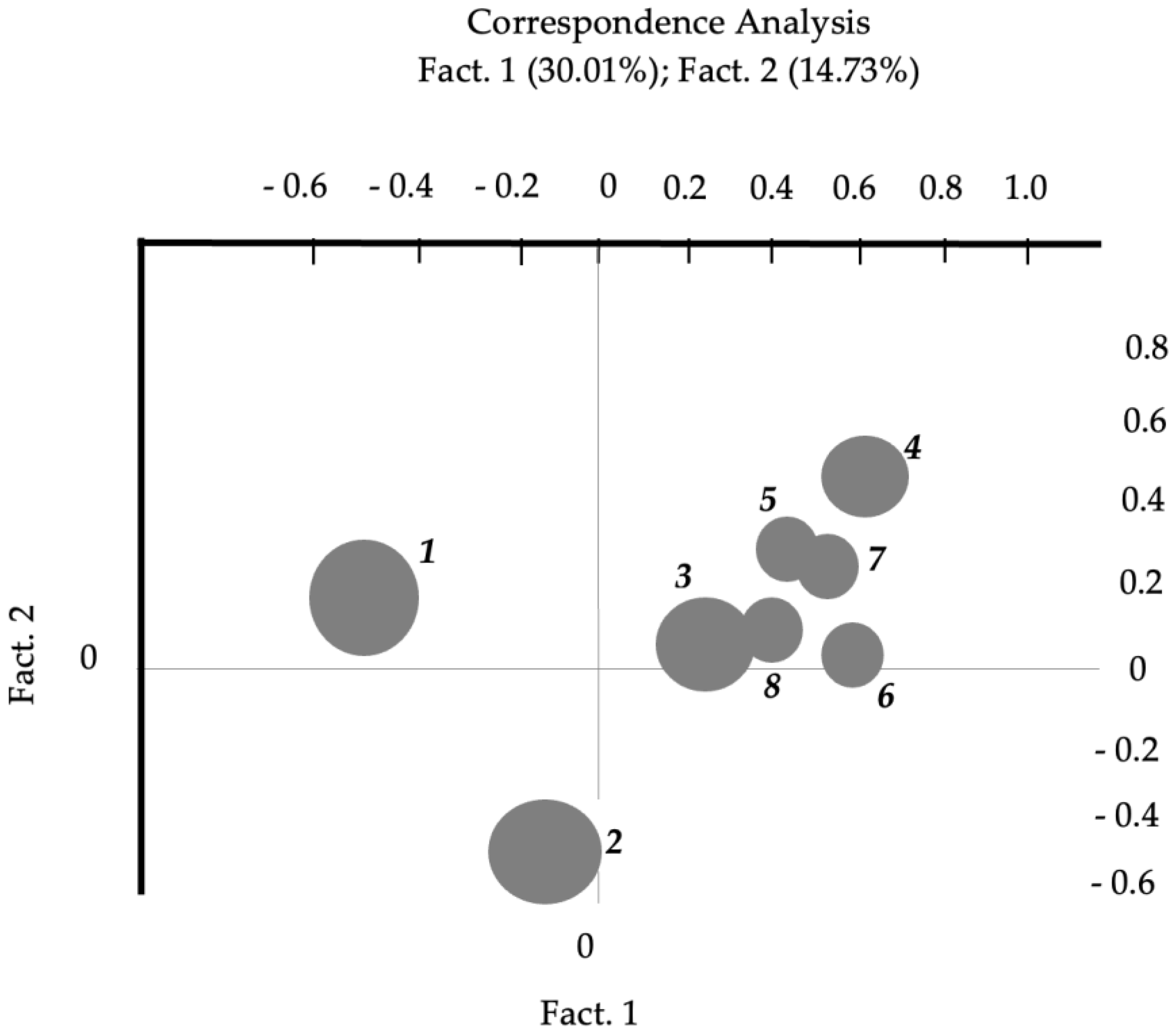
4.3. Correspondence Analysis
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Bonati, M.; Campi, R.; Segre, G. Psychological impact of the quarantine during the COVID-19 pandemic on the general European adult population: A systematic review of the evidence. Epidemiol. Psychiatr. Sci. 2022, 31, e27. [Google Scholar] [CrossRef] [PubMed]
- Panzeri, M.; Santarpia, G.; Fusar Poli, C.; Molgora, S.; Saita, E.; Facchin, F. The Short-Term Psychological Impact of COVID-19: A Systematic Review of the Literature. Ric. Psicol. 2022, 4, 5176327. [Google Scholar] [CrossRef]
- Inchausti, F.; MacBeth, A.; Hasson-Ohayon, I.; Dimaggio, G. Psychological Intervention and COVID-19: What We Know So Far and What We Can Do. J. Contemp. Psychother. 2020, 50, 243–250. [Google Scholar] [CrossRef]
- Odone, A.; Delmonte, D.; Scognamiglio, T.; Signorelli, C. COVID-19 deaths in Lombardy, Italy: Data in context. Lancet Public Health 2020, 5, e310. [Google Scholar] [CrossRef] [PubMed]
- Delmastro, M.; Zamariola, G. Depressive symptoms in response to COVID-19 and lockdown: A cross-sectional study on the Italian population. Sci. Rep. 2020, 10, 22457. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Saita, E.; Facchin, F.; Pagnini, F.; Molgora, S. In the Eye of the Covid-19 Storm: A Web-Based Survey of Psychological Distress among People Living in Lombardy. Front. Psychol. 2021, 12, 566753. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Ohayon, M.M.; Griffiths, M.D.; Lin, C.Y.; Pakpour, A.H. Fear of COVID-19 and its association with mental health-related factors: Systematic review and meta-analysis. BJPsych Open 2022, 8, e73. [Google Scholar] [CrossRef]
- Vagnini, D.; Hou, W.K.; Hougen, C.; Cano, A.; Bonanomi, A.; Facchin, F.; Molgora, S.; Pagnini, F.; Saita, E. The impact of COVID-19 perceived threat and restrictive measures on mental health in Italy, Spain, New York, and Hong Kong: An international multisite study. Front. Psychol. 2022, 13, 1002936. [Google Scholar] [CrossRef]
- Arora, T.; Grey, I.; Östlundh, L.; Alamoodi, A.; Omar, O.M.; Hubert Lam, K.B.; Grandner, M. A systematic review and meta-analysis to assess the relationship between sleep duration/quality, mental toughness and resilience amongst healthy individuals. Sleep Med. Rev. 2022, 62, 101593. [Google Scholar] [CrossRef]
- Cénat, J.M.; Farahi, S.M.M.M.; Dalexis, R.D.; Darius, W.P.; Bekarkhanechi, F.M.; Poisson, H.; Broussard, C.; Ukwu, G.; Auguste, E.; Nguyen, D.D.; et al. The global evolution of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2022, 315, 70–95. [Google Scholar] [CrossRef] [PubMed]
- Dragioti, E.; Li, H.; Tsitsas, G.; Lee, K.H.; Choi, J.; Kim, J.; Choi, Y.J.; Tsamakis, K.; Estradé, A.; Agorastos, A.; et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 2022, 94, 1935–1949. [Google Scholar] [CrossRef] [PubMed]
- Yunitri, N.; Chu, H.; Kang, X.L.; Jen, H.J.; Pien, L.C.; Tsai, H.T.; Kamil, A.R.; Chou, K.R. Global prevalence and associated risk factors of posttraumatic stress disorder during COVID-19 pandemic: A meta-analysis. Int. J. Nurs. Stud. 2022, 126, 104136. [Google Scholar] [CrossRef]
- World Health Organization. A Clinical Case Definition of Post COVID-19 Condition by a Delphi Consensus, 6 October 2021. Available online: https://apps.who.int/iris/handle/10665/345824 (accessed on 10 January 2023).
- De Tanti, A.; Conforti, J.; Bruni, S.; De Gaetano, K.; Cappalli, A.; Basagni, B.; Bertoni, D.; Saviola, D. Cognitive and psychological outcomes and follow-up in severely affected COVID-19 survivors admitted to a rehabilitation hospital. Neurol. Sci. 2023, 44, 1481–1489. [Google Scholar] [CrossRef] [PubMed]
- Bellan, M.; Soddu, D.; Balbo, P.E.; Baricich, A.; Zeppegno, P.; Avanzi, G.C.; Baldon, G.; Bartolomei, G.; Battaglia, M.; Battistini, S.; et al. Respiratory and Psychophysical Sequelae among Patients with COVID-19 Four Months after Hospital Discharge. JAMA Netw. Open 2021, 4, e2036142. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Huang, L.; Wang, Y.; Li, X.; Ren, L.; Gu, X.; Kang, L.; Guo, L.; Liu, M.; Zhou, X.; et al. 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet 2021, 397, 220–232. [Google Scholar] [CrossRef]
- Onder, G.; Floridia, M.; Giuliano, M.; Lo Noce, C.; Tiple, D.; Bertinato, L.; Mariniello, R.; Laganà, M.G.; Della Vecchia, A.; Gianferro, R.; et al. Indicazioni ad Interim sui Principi di Gestione del Long-COVID; Versione del 1° luglio 2021; Rapporto ISS COVID-19 n. 15/2021; Istituto Superiore di Sanità: Roma, Italy, 2021. [Google Scholar]
- Sykes, D.L.; Holdsworth, L.; Jawad, N.; Gunasekera, P.; Morice, A.H.; Crooks, M.G. Post-COVID-19 Symptom Burden: What is Long-COVID and How Should We Manage It? Lung 2021, 199, 113–119. [Google Scholar] [CrossRef]
- Khraisat, B.; Toubasi, A.; AlZoubi, L.; Al-Sayegh, T.; Mansour, A. Meta-analysis of prevalence: The psychological sequelae among COVID-19 survivors. Int. J. Psychiatry Clin. Pract. 2022, 26, 234–243. [Google Scholar] [CrossRef]
- Aiyegbusi, O.L.; Hughes, S.E.; Turner, G.; Rivera, S.C.; McMullan, C.; Chandan, J.S.; Haroon, S.; Price, G.; Davies, E.H.; Nirantharakumar, K.; et al. Symptoms, complications and management of long COVID: A review. J. R. Soc. Med. 2021, 114, 428–442. [Google Scholar] [CrossRef]
- Lopez-Leon, S.; Wegman-Ostrosky, T.; Perelman, C.; Sepulveda, R.; Rebolledo, P.A.; Cuapio, A.; Villapol, S. More than 50 Long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16144. [Google Scholar] [CrossRef] [PubMed]
- Carfì, A.; Bernabei, R.; Landi, F.; Gemelli Against COVID-19 Post-Acute Care Study Group. Persistent symptoms in patients after acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post-Coronavirus Disease 2019 (COVID-19) Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022, 226, 1593–1607. [Google Scholar] [CrossRef] [PubMed]
- Corno, G.; Villani, D.; de Montigny, F.; Pierce, T.; Bouchard, S.; Molgora, S. The role of perceived social support on pregnant women’s mental health during the COVID-19 pandemic. J. Reprod. Infant Psychol. 2022, 1–15. [Google Scholar] [CrossRef]
- Femia, G.; Federico, I.; Ciullo, V.; Provenzano, S.; De Luca, A.; Picano, F.; Giacobbi, M.; D’Argenzio, M.; Valeri, I.; Albani, C.; et al. Gli effetti psicologici della pandemia: Strategie di coping e tratti di personalità. Cogn. Clin. 2020, 17, 119–135. [Google Scholar] [CrossRef]
- Orrù, G.; Ciacchini, R.; Gemignani, A.; Conversano, C. Psychological intervention measures during the COVID-19 pandemic. Clin. Neuropsychiatry 2020, 17, 76–79. [Google Scholar] [CrossRef]
- Fan, Y.; Shi, Y.; Zhang, J.; Sun, D.; Wang, X.; Fu, G.; Mo, D.; Wen, J.; Xiao, X.; Kong, L. The effects of narrative exposure therapy on COVID-19 patients with post-traumatic stress symptoms: A randomized controlled trial. J. Affect. Disord. 2021, 293, 141–147. [Google Scholar] [CrossRef]
- Bäuerle, A.; Jahre, L.; Teufel, M.; Jansen, C.; Musche, V.; Schweda, A.; Fink, M.; Dinse, H.; Weismüller, B.; Dörrie, N.; et al. Evaluation of the E-Mental Health Mindfulness-Based and Skills-Based “CoPE It” Intervention to Reduce Psychological Distress in Times of COVID-19: Results of a Bicentre Longitudinal Study. Front. Psychiatry 2021, 12, 768132. [Google Scholar] [CrossRef]
- Bureau, R.; Bemmouna, D.; Faria, C.G.F.; Goethals, A.C.; Douhet, F.; Mengin, A.C.; Fritsch, A.; Zinetti Bertschy, A.; Frey, I.; Weiner, L. My Health Too: Investigating the Feasibility and the Acceptability of an Internet-Based Cognitive-Behavioral Therapy Program Developed for Healthcare Workers. Front. Psychol. 2021, 12, 760678. [Google Scholar] [CrossRef]
- Bossi, F.; Zaninotto, F.; D’Arcangelo, S.; Lattanzi, N.; Malizia, A.P.; Ricciardi, E. Mindfulness-based online intervention increases well-being and decreases stress after COVID-19 lockdown. Sci. Rep. 2022, 12, 6483. [Google Scholar] [CrossRef]
- Rossi Ferrario, S.; Panzeri, A.; Cerutti, P.; Sacco, D. The Psychological Experience and Intervention in Post-Acute COVID-19 Inpatients. Neuropsychiatr. Dis. Treat. 2021, 17, 413–422. [Google Scholar] [CrossRef]
- Diotaiuti, P.; Valente, G.; Mancone, S.; Corrado, S.; Bellizzi, F.; Falese, L.; Langiano, E.; Vilarino, G.T.; Andrade, A. Effects of Cognitive Appraisals on Perceived Self-Efficacy and Distress during the COVID-19 Lockdown: An Empirical Analysis Based on Structural Equation Modeling. Int. J. Environ. Res. Public Health 2023, 20, 5294. [Google Scholar] [CrossRef]
- Weiner, L.; Berna, F.; Nourry, N.; Severac, F.; Vidailhet, P.; Mengin, A.C. Efficacy of an online cognitive behavioral therapy program developed for healthcare workers during the COVID-19 pandemic: The REduction of STress (REST) study protocol for a randomized controlled trial. Trials 2020, 21, 870. [Google Scholar] [CrossRef]
- Bryant, R.A.; Dawson, K.S.; Keyan, D.; Azevedo, S.; Yadav, S.; Tran, J.; Rawson, N.; Harvey, S. Effectiveness of a Videoconferencing-Delivered Psychological Intervention for Mental Health Problems during COVID-19: A Proof-of-Concept Randomized Clinical Trial. Psychother. Psychosom. 2022, 91, 63–72. [Google Scholar] [CrossRef]
- Esterwood, E.; Saeed, S.A. Past Epidemics, Natural Disasters, COVID19, and Mental Health: Learning from History as we Deal with the Present and Prepare for the Future. Psychiatr. Q. 2020, 91, 1121–1133. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, C.E.; Sansom-Daly, U.M.; McGill, B.C.; McCarthy, M.; Girgis, A.; Grootenhuis, M.; Barton, B.; Patterson, P.; Osborn, M.; Lowe, C.; et al. Online parent-targeted cognitive-behavioural therapy intervention to improve quality of life in families of young cancers survivors: Study protocol for a randomized controlled trial. Trials 2015, 16, 153. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Li, X.; Jiang, J.; Xu, X.; Wu, J.; Xu, Y.; Lin, X.; Hall, J.; Xu, H.; Xu, J.; et al. The Effect of Cognitive Behavioral Therapy on Depression, Anxiety, and Stress in Patient with COVID-19: A Randomized Controlled Trial. Front. Psychiatry 2020, 11, 580827. [Google Scholar] [CrossRef] [PubMed]
- Si, M.; Xiao, W.; Pan, C.; Wang, H.; Huang, Y.; Lian, J.; Mak, W.W.S.; Leng, Z.; Su, X.; Tang, Q.; et al. Mindfulness-based online intervention on mental health and quality of life among COVID-19 patients in China: An intervention design. Infect. Dis. Poverty 2021, 10, 69. [Google Scholar] [CrossRef]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, G.M.; Sassaroli, S. Il Colloquio in Psicoterapia Cognitiva. Tecnica e Pratica Clinica; Raffaello Cortina Editore: Milano, Italy, 2013. [Google Scholar]
- Leahy, R.L.; Tirch, D.; Napolitano, L.A. Emotion Regulation in Psychotherapy: A Practitioner’s Guide; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Segal, Z.V.; Williams, J.M.G.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse; Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Goodman, R.; Calderon, A. The Use of Mindfulness in Trauma Counseling. J. Ment. Health Couns. 2012, 34, 254–268. [Google Scholar] [CrossRef]
- Segal, Z.V.; Teasdale, J.D.; Williams, J.M.G. Mindfulness-Based Cognitive Therapy: Theoretical Rationale and Empirical Status. In Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition; Hayes, S.C., Follette, V.M., Linehan, M.M., Eds.; Guilford Press: New York, NY, USA, 2004; pp. 45–65. [Google Scholar]
- Murray, H.; Grey, N.; Wild, J.; Warnock-Parkes, E.; Kerr, A.; Clark, D.M.; Ehlers, A. Cognitive therapy for post-traumatic stress disorder following critical illness and intensive care unit admission. Cogn. Behav. Therap. 2020, 13, e13. [Google Scholar] [CrossRef]
- Murray, H.; Ehlers, A. Cognitive therapy for moral injury in post-traumatic stress disorder. Cogn. Behav. Therap. 2021, 14, e8. [Google Scholar] [CrossRef] [PubMed]
- Carli, R.; Paniccia, R.M. L’analisi Emozionale del Testo. Uno Strumento Psicologico per Leggere Testi e Discorsi [The Emotional Text Analysis: A Psychological Tool for Reading Text and Discourses]; Franco Angeli: Milano, Italy, 2002. [Google Scholar]
- Lancia, F. Strumenti per L’Analisi dei Testi. Introduzione All’uso di T-LAB [Instruments for Text Analysis. An Introduction to the Use of T-LAB]; Franco Angeli: Milano, Italy, 2004. [Google Scholar]
- Jamili, S.; Ebrahimipour, H.; Adel, A.; Badiee Aval, S.; Hoseini, S.J.; Vejdani, M.; Ebnehoseini, Z. Experience of patients hospitalized with COVID-19: A Qualitative study of a pandemic disease in Iran. Health Expect 2020, 25, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Cheng, J.; Zou, J.; Duan, L.; Campbell, J.E. Health-related quality of life of hospitalized COVID-19 survivors: An initial exploration in Nanning city, China. Soc. Sci Med. 2021, 274, 113748. [Google Scholar] [CrossRef] [PubMed]
- Nandasena, H.M.R.K.G.; Pathirathna, M.L.; Atapattu, A.M.M.P.; Prasanga, P.T.S. Quality of life of COVID-19 patients after discharge: Systematic review. PLoS ONE 2022, 17, e0263941. [Google Scholar] [CrossRef]
- Qu, G.; Zhen, Q.; Wang, W.; Fan, S.; Wu, Q.; Zhang, C.; Li, B.; Liu, G.; Yu, Y.; Li, Y.; et al. Health-related quality of life of COVID-19 patients after discharge: A multicenter follow-up study. J. Clin. Nurs. 2021, 30, 1742–1750. [Google Scholar] [CrossRef]
- Del Rio, G.; Luppi, M. Gruppi e Relazione D’aiuto. Saperi, Competenze, Emozioni; Franco Angeli: Milano, Italy, 2010. [Google Scholar]
- Fonagy, P.; Campbell, C.; Bateman, A. Mentalizing, attachment, and epistemic trust in group therapy. Int. J. Group Psychother. 2017, 67, 176–201. [Google Scholar] [CrossRef]
| Nr | Themes | Targets | Working Instruments |
|---|---|---|---|
| 1 | The pandemic and the disease: subjective experience. | History of illness experience and shared representation. Assessment of baseline psychological well-being using psychometric scales. | Narration of the illness experience in the group: patients tell their own illness story in a safe context. The homework includes a graphic exercise in which patients are asked to indicate physical symptoms on a drawing of the human body. They have a card with a printed stylized human figure, on which participants must mark the part of their body perceived as the most affected by post-COVID-19 symptoms. |
| 2 | Post-COVID-19 and related symptoms. | Indicate physical symptoms, recognize psychological impact of the disease in the present; favor a realistic interpretation of the emotional states connected to the symptoms, and recognize the cognitive biases in the elaboration of one’s own experience of illness. | Sharing within the group the homework assigned at the end of session one. Explanation of the Cognitive Model Antecedent Beliefs and Consequences (ABC) [43]: patients are invited to share and discuss the emotional impact of physical symptoms using the ABC scheme. Then, participants receive the ABC scheme and the homework entails using the scheme to analyze the situations experienced during the following week. |
| 3 | Dominant emotions and social perception. | Recognize the prevailing emotions in the experience of illness; stigma, isolation, emotional regulation, use of social support. | Sharing within the group the homework assigned at the end of session two: patients share emotions acknowledged through the ABC scheme. The ABC scheme is modified by adding a social resource mapping. The homework entails using the modified ABC scheme to analyze concrete situations during the following week, also evaluating the presence of social support as a resource. |
| 4 | “Nourishing behaviors”. | Identify and practice wellness behaviors in everyday life. | Introduction to grounding practices [46]: simple practices are proposed in session four and subsequently included at the beginning of each module. Sharing within the group the homework assigned at the end of session three. Presentation of “Wellness Strategies”, a Mindfulness Based Cognitive Therapy (MBCT) protocol [45,47]. Homework requires that participants identify and introduce well-being behaviors (i.e., “nourishing behaviors”) and grounding practices in their daily lives. |
| 5 | Cognitive restructuring. | Recognize and analyze negative automatic thoughts; identify alternative thoughts. | Grounding practices. Sharing within the group the homework assigned at the end of session four. One of the psychologists conducts a psycho-educational session on dysfunctional automatic thoughts. The homework entails using a form to examine automatic thoughts [44]: patients receive a list of possible automatic thoughts, and they must use it to analyze concrete situations, and to recognize their automatic thoughts. |
| 6 | Coping strategies. | Use functional coping strategies to promote adaptation. | Grounding practices. Sharing within the group the homework assigned at the end of session five. Psycho-education on adaptive coping strategies. Homework: patients receive information material on coping strategies [44], and a list of possible coping strategies. They must reflect upon which strategies they use the most, and they write them in a diary. |
| 7 | Planning and future orientation. | Validate resources; identify concrete goals to pursue in the near future; complete an individual and collective synthesis of group work proposing a representative image, or a metaphor. | Grounding practices. Sharing within the group the homework assigned at the end of session six. Using a form to identify realistic goals [48] through which patients are required to imagine and set realistic goals to be achieved in the near future. Choice of a metaphorical image [49] for the group: patients select an image (among the proposed ones) that allows them to re-read their path through illness using a metaphor. Choice of a shared name of the group. The module ends with the delivery of a certificate of participation. |
| 8 | Follow-up. | Verification of objectives, resumption of adaptive strategies, and assessment of current (end of group intervention) psychological well-being with psychometric scales. | Patients talk about the difficulties that emerged since the seventh session, and the strategies used to deal with them. |
| M ± SD (Min; Max) | |
|---|---|
| Age | 62.68 ± 8.19 (54; 80) |
| Days of hospitalization | 25.28 ± 22.89 (6; 84) |
| n | |
| Gender Female Male | 10 8 |
| Work Status Full-time job Retired | 11 7 |
| Prescribed therapy for COVID-19 infection Pharmacological treatment CPAP Hospitalization in intensive care unit | 10 5 3 |
| Mourning of a beloved one due to COVID-19 Yes No | 3 15 |
| Cluster | Explained Variance | Theme | Lexical Units | χ2 * | Quotes |
|---|---|---|---|---|---|
| Cluster 2: Disease | 48.40% | Concrete elements and contextual factors related to COVID-19 disease | Doctor | 53.554 | “At that moment… the pain I felt at the hospital was just indescribable.” “Due to COVID-19 I was hospitalized urgently and I was like that for a week, dressed the same way… I had nothing, I missed everything. Imagine… I spent the day lying down in bed, I felt pain everywhere and I was alone.” |
| COVID-19 | 44.815 | ||||
| Hospital | 28.634 | ||||
| To hospitalize | 16.051 | ||||
| To miss | 10.972 | ||||
| Pain | 10.721 | ||||
| Cluster 3: COVID-19 Emotional Experience | 26.45% | Emotional factors related to COVID-19 and inability to move forward | Anxiety | 200.804 | “It was a nightmare that led to seeing and thinking only of the worst, of the most terrible things... anxiety took over me.” “I tried in every way not to have fear, but I was discouraged just thinking about what was happening.” |
| To think | 169.876 | ||||
| Fear | 27.002 | ||||
| Nightmare | 12.813 | ||||
| Anger | 11.812 | ||||
| Cluster 1: Upturn | 25.15% | Prospective of positive change | Power | 297.442 | “My past has deeply affected me, but I try to harness my strength and think that we must always move on, whatever happens in life.” “I felt the power to take back what is beautiful in life, after so much effort. So, this period that I’m leaving behind has been like climbing a mountain [...] After a long time I want take up again everything I never even imagined before.” |
| Strength | 30.576 | ||||
| Life | 26.934 | ||||
| To move on | 12.505 | ||||
| To take up again | 11.985 | ||||
| Motivation | 11.664 |
| Factor 1: Cognitive Restructuring | Factor 2: Emotional Elaboration | ||||||
|---|---|---|---|---|---|---|---|
| Negative Pole (Bottom of the Graph) | Test Value * | Positive Pole (Top of the Graph) | Test Value * | Negative Pole (Left of the Graph) | Test Value * | Positive Pole (Right of the Graph) | Test Value * |
| To hospitalize | −8.5523 | To think | 5.4622 | Pain | −6.4075 | Pleasure | 3.1728 |
| Ambulance | −7.6656 | Work | 5.1991 | Cold | −6.0669 | Alone | 2.6933 |
| Doctor | −7.5842 | Help | 4.3638 | Cramp | −4.896 | Need | 2.1196 |
| Intensive care unit | −7.4841 | Strategy | 3.5306 | Body | −4.2272 | Sadness | 2.1158 |
| To die | −5.0759 | To cope | 3.3999 | Tachycardia | −3.7914 | To relax | 2.0202 |
| Heavy | −2.1507 | Relation | 2.0437 | Medicine | −2.2747 | To feel | 2.0094 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vagnini, D.; Lamperti, N.; Molgora, S.; Barile, F.; Facchin, F.; Mazza, U.; Saita, E. Mental Health Issues as a Consequence of the Pandemic: Group Psycho-Educational Intervention to Support Patients Recovered from COVID-19 Infection. Int. J. Environ. Res. Public Health 2023, 20, 6105. https://doi.org/10.3390/ijerph20126105
Vagnini D, Lamperti N, Molgora S, Barile F, Facchin F, Mazza U, Saita E. Mental Health Issues as a Consequence of the Pandemic: Group Psycho-Educational Intervention to Support Patients Recovered from COVID-19 Infection. International Journal of Environmental Research and Public Health. 2023; 20(12):6105. https://doi.org/10.3390/ijerph20126105
Chicago/Turabian StyleVagnini, Denise, Nicolò Lamperti, Sara Molgora, Francesca Barile, Federica Facchin, Umberto Mazza, and Emanuela Saita. 2023. "Mental Health Issues as a Consequence of the Pandemic: Group Psycho-Educational Intervention to Support Patients Recovered from COVID-19 Infection" International Journal of Environmental Research and Public Health 20, no. 12: 6105. https://doi.org/10.3390/ijerph20126105
APA StyleVagnini, D., Lamperti, N., Molgora, S., Barile, F., Facchin, F., Mazza, U., & Saita, E. (2023). Mental Health Issues as a Consequence of the Pandemic: Group Psycho-Educational Intervention to Support Patients Recovered from COVID-19 Infection. International Journal of Environmental Research and Public Health, 20(12), 6105. https://doi.org/10.3390/ijerph20126105










