The Association between Drought Exposure and Respiratory-Related Mortality in the United States from 2000 to 2018
Abstract
1. Introduction
2. Materials and Methods
2.1. Health Data and Study Population
2.2. Environmental Exposure
2.3. Statistical Modeling
3. Results
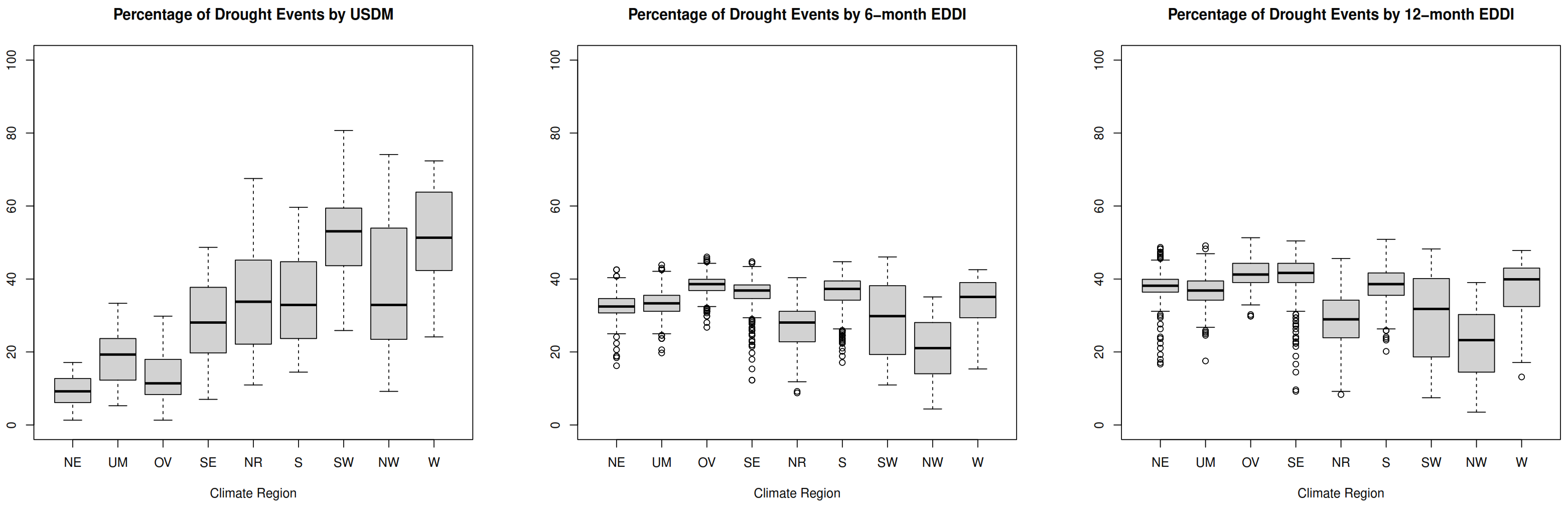
3.1. Data Cleaning and Descriptive Statistics
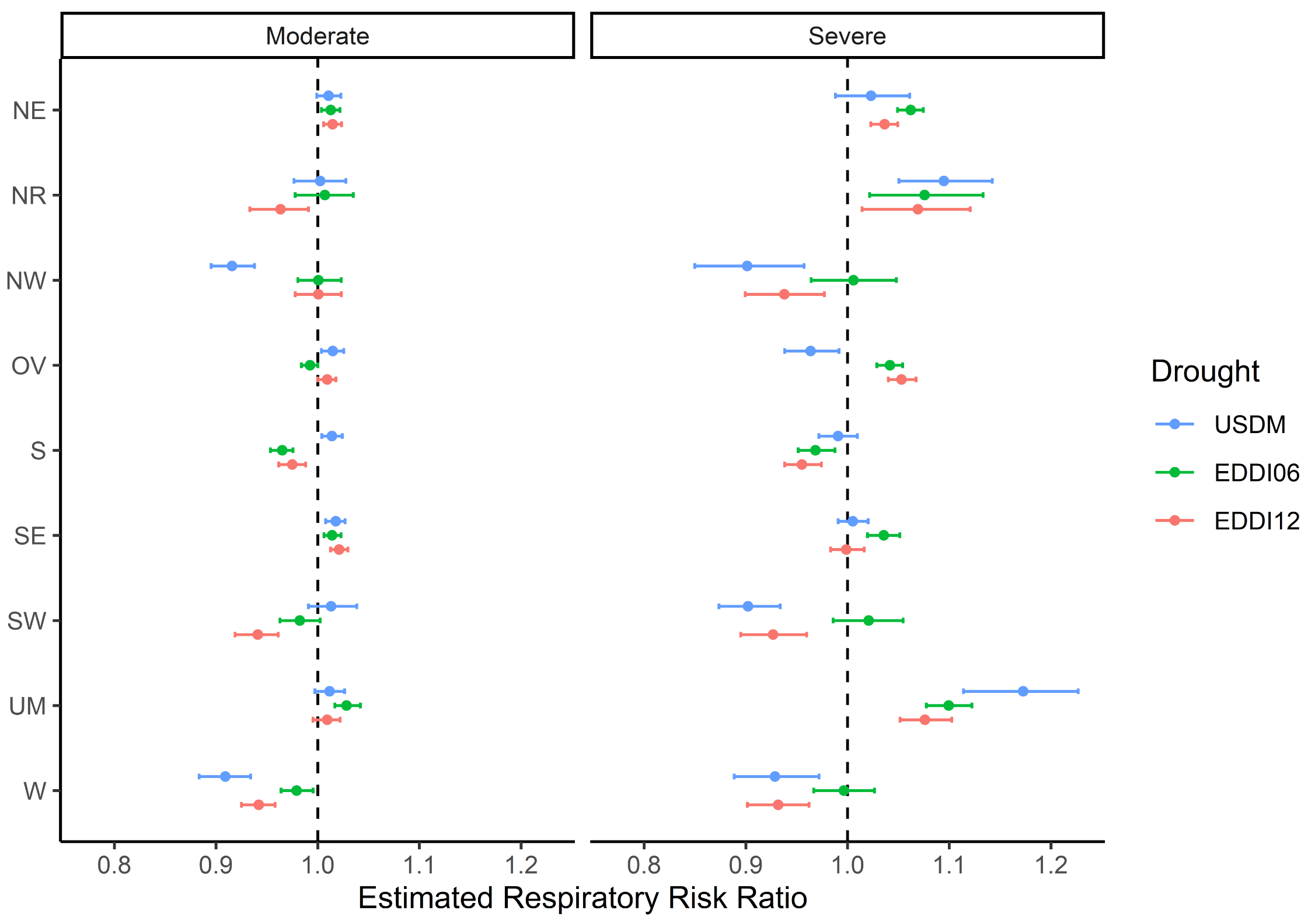
3.2. Association between Drought Exposure and Respiratory Outcomes
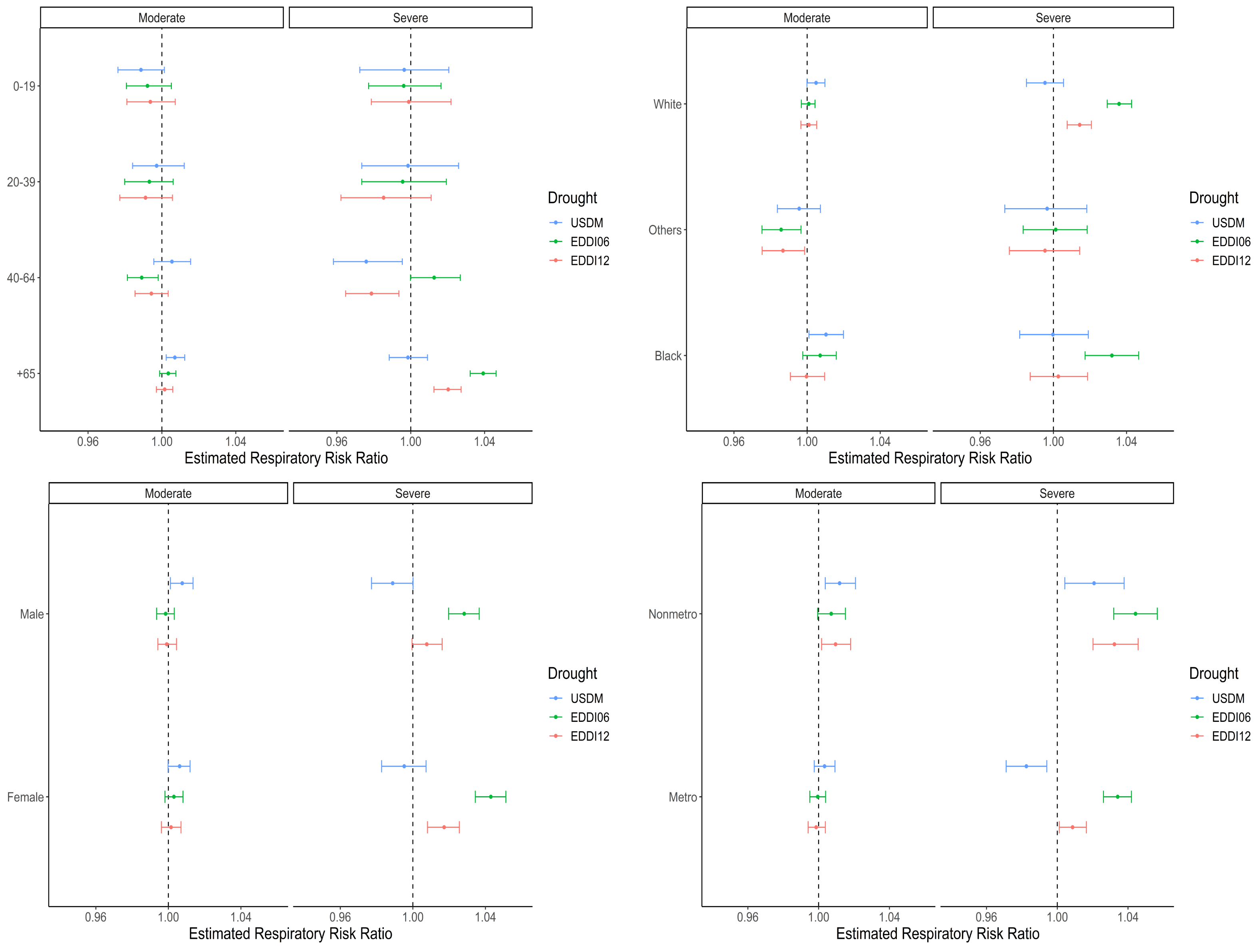
3.3. Stratification Analysis by Age Group, Race, Sex, and Urbanicity
4. Summary and Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| NOAA | National Oceanographic and Atmospheric Administration |
| USDM | United States Drought Monitor |
| EDDI | Evaporative Demand Drought Index |
| Cr | Credible Interval |
| NE | Northeast |
| UM | Upper Midwest |
| OV | Ohio Valley |
| SE | Southeast |
| NR | Northern Rockies and Plains |
| S | South |
| SW | Southwest |
| NW | Northwest |
| W | West |
References
- Li, X.; Cao, X.; Guo, M.; Xie, M.; Liu, X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: Systematic analysis for the Global Burden of Disease Study 2017. BMJ 2020, 368, m234. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.E.; Herring, S.C.; Jantarasami, L.; Adrianopoli, C.; Benedict, K.; Conlon, K.; Escobar, V.; Hess, J.; Luvall, J.; Garcia-Pando, C.P.; et al. Ch. 4: Impacts of extreme events on human health. In The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2016; pp. 99–128. [Google Scholar]
- Campbell, S.; Remenyi, T.A.; White, C.J.; Johnston, F.H. Heatwave and health impact research: A global review. Health Place 2018, 53, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Xu, Z.; Bambrick, H.; Prescott, V.; Wang, N.; Zhang, Y.; Su, H.; Tong, S.; Hu, W. Cardiorespiratory effects of heatwaves: A systematic review and meta-analysis of global epidemiological evidence. Environ. Res. 2019, 177, 108610. [Google Scholar] [CrossRef] [PubMed]
- Ebi, K.L.; Vanos, J.; Baldwin, J.W.; Bell, J.E.; Hondula, D.M.; Errett, N.A.; Hayes, K.; Reid, C.E.; Saha, S.; Spector, J.; et al. Extreme weather and climate change: Population health and health system implications. Annu. Rev. Public Health 2021, 42, 293–315. [Google Scholar] [CrossRef]
- Kang, C.; Park, C.; Lee, W.; Pehlivan, N.; Choi, M.; Jang, J.; Kim, H. Heatwave-related mortality risk and the risk-based definition of heat wave in South Korea: A Nationwide Time-series study for 2011–2017. Int. J. Environ. Res. Public Health 2020, 17, 5720. [Google Scholar] [CrossRef]
- Nhung, N.T.T.; Hoang, L.T.; Hanh, T.T.T.; Toan, L.Q.; Thanh, N.D.; Truong, N.X.; Son, N.A.; Nhat, H.V.; Quyen, N.H.; Nhu, H.V. Effects of heatwaves on hospital admissions for cardiovascular and respiratory disease, in Southern Vietnam, 2010–2018: Time series analysis. Int. J. Environ. Res. Public Health 2020, 20, 3908. [Google Scholar] [CrossRef]
- Puvvula, J.; Jill, P.; Eleanor, R.; Gwon, Y.; Bell, J.E. Joint association between ambient air pollutant mixture and pediatric asthma exacerbations. Environ. Epidemiol. 2022, 6, e225. [Google Scholar] [CrossRef]
- Rau, A.; Abadi, A.; Fiecas, M.B.; Gwon, Y.; Bell, J.E.; Berman, J.D. Nationalwide assessment of ambient monthly fine particulate matter (PM2.5) and the associations with total, cardiovascular and respiratory mortality in the United States. Environ. Res. Health 2023, 1, 025001. [Google Scholar] [CrossRef]
- Varghese, B.; Beaty, M.; Panchuk, S.; Mackie, B.; Chen, C.; Jakab, M.; Yang, T.; Bi, P.; Nairn, J. Heatwave-related mortality in Australia: Who’s impacted the most? Eur. J. Public Health 2020, 30, ckaa165.377. [Google Scholar] [CrossRef]
- Yang, J.; Yin, P.; Sun, J.; Wang, B.; Zhou, M.; Li, M.; Tong, S.; Meng, B.; Guo, Y.; Liu, Q. Heatwave and mortality in 31 major Chinese cities: Definition, vulnerability and implications. Sci. Total Environ. 2019, 649, 695–702. [Google Scholar] [CrossRef]
- Ye, X.; Wolff, R.; Yu, W.; Vaneckova, P.; Pan, X.; Tong, S. Ambient temperature and morbidity: A review of epidemiological eveidence. Environ. Health Perspect. 2012, 120, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Salvador, C.; Nieto, R.; Vicente-Serrano, S.M.; Garcia-Herrera, R.; Gimeno, L.; Vicedo-Cabrera, A.M. Public health implications of Drought in a Climate change context: A Critical Review. Annu. Rev. Public Health 2023, 44, 213–232. [Google Scholar] [CrossRef] [PubMed]
- Abadi, A.M.; Gwon, Y.; Gribble, M.O.; Berman, J.D.; Bilotta, R.; Hobbins, M.; Bell, J.E. Drought and all-cause mortality in Nebraska from 1980 to 2014: Time-series analyses by age, sex, race, urbanicity and drought severity. Sci. Total Environ. 2022, 840, 156660. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.E.; Brown, C.L.; Conlon, K.; Herring, S.; Kunkel, K.E.; Lawrimore, J.; Luber, G.; Schreck, C.; Smith, A.; Uejio, C. Changes in extreme events and the potential impacts on human health. J. Air Wast Manage Assoc. 2018, 68, 265–287. [Google Scholar] [CrossRef]
- Berman, J.D.; Ebisu, K.; Peng, R.D.; Dominici, F.; Bell, M.L. Drought and the risk of hospital admissions and mortality in older adults in western USA from 2000 to 2013: A retrospective study. Lancet Planet Health 2017, 1, e17–e25. [Google Scholar] [CrossRef] [PubMed]
- Munde, S.; Bell, J.E.; Leeper, R.D.; Rennie, J.; Berman, J.D.; Abadi, A.M.; Gwon, Y.; Lookadoo, R. A Comparative Review of Drought Metrics for Public Health Research Applications. In AGU Fall Meeting Abstracts; AGU: New Orleans, LA, USA, 2021; Volume 2021, p. GH25B-0626. [Google Scholar]
- Lynch, K.M.; Lyles, R.H.; Waller, L.A.; Abadi, A.M.; Bell, J.E.; Gibble, M.O. Drought severity and all-cause mortality rates among adults in the United States: 1968–2014. Environ. Health 2020, 19, 52. [Google Scholar] [CrossRef]
- Salvador, C.; Nieto, R.; Linares, C.; Diaz, J.; Gimeno, L. Effects on daily mortality of droughts in Galicia (NW Spain) from 1983 to 2013. Sci. Total Environ. 2019, 662, 121–133. [Google Scholar] [CrossRef]
- Salvador, C.; Nieto, R.; Linares, C.; Diaz, J.; Gimeno, L. Quantification of the effects of droughts on daily mortality in Spain at different timescales at regional and national levels: A meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 6114. [Google Scholar] [CrossRef]
- Salvador, C.; Nieto, R.; Linares, C.; Diaz, J.; Alves, C.; Gimeno, L. Drought effects on specific-cause mortality in Lisbon from 1983 to 2016: Risks assessment by gender and age groups. Sci. Total Environ. 2021, 751, 142332. [Google Scholar] [CrossRef]
- Salvador, C.; Vicedo-Cabrera, A.M.; Libonati, R.; Russo, A.; Garcia, B.N.; Belem, L.B.; Gimeno, L.; Nieto, R. Effects of drought on mortality in macro urban areas of Brazil between 2000 and 2019. GeoHelath 2022, 6, e2021GH000534. [Google Scholar] [CrossRef]
- Romanello, M.; McGushin, A.; Di Napoli, C.; Drummond, P.; Hughes, N.; Jamart, L.; Kennard, H.; Lampard, P.; Rodriguez, B.S.; Arnell, N.; et al. The 2021 report of the Lancet Countdown on health and climate change: Code red for a healthy future. Lancet 2021, 398, 1619–1662. [Google Scholar] [CrossRef] [PubMed]
- Stanke, C.; Kerac, M.; Prudhomme, C.; Medlock, J.; Murray, V. Health effects of drought: A systematic review of the evidence. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef] [PubMed]
- Aderita, S.; Ebi, K. When Land Is Under Pressure Health Is Under Stress. Int. J. Environ. Res. Public Health 2020, 18, 136. [Google Scholar] [CrossRef]
- Ingram, D.D.; Franco, S.J. 2013 NCHS urban–rural classification scheme for counties. Natl. Health Stat. Rep. 2014, 166, 1–73. [Google Scholar]
- Anderson, M.C.; Hain, C.; Otkin, J.; Zhan, X.; Mo, K. An intercomparison of drought indicators based on thermal remote sensing and NLDAS-2 simulations with US drought monitor classifications. J. Hydrometeorol. 2013, 14, 1035–1056. [Google Scholar] [CrossRef]
- Park, S.; Im, J.; Jang, E.; Rhee, J. Drought assessment and monitoring through blending of multi-sensor indices using machine learning approaches. Agric. Meteorol. 2016, 216, 181–187. [Google Scholar] [CrossRef]
- Svoboda, M.D.; LeComte, D.; Hayes, M.; Heim, R.; Gleason, K. The drought monitor. Bull. Am. Meteorol. Soc. 2002, 83, 1181–1190. [Google Scholar] [CrossRef]
- Hobbins, M.T.; Wood, A.; McEvoy, D.J.; Huntington, J.L.; Morton, C.; Anderson, M.; Hain, C. The Evaporative Demand Drought Index. Part I: Linking Drought Evolution to Variations in Evaporative Demand. J. Hydrometeorol. 2016, 17, 1745–1761. [Google Scholar] [CrossRef]
- McEvoy, D.J.; Huntington, J.L.; Hobbins, M.T.; Wood, A.; Morton, C.; Anderson, M.; Hain, C. The Evaporative Demand Drought Index: Part II - CONUS-wide assessment against common drought indicators. J. Hydrometeorol. 2016, 17, 1763–1779. [Google Scholar] [CrossRef]
- Vose, R.S.; Applequist, S.; Squires, M.; Durre, I.; Menne, M.J.; Williams, C.N.; Fennimore, C.; Gleason, K.; Arndt, D. NOAA Monthly U.S. Climate Gridded Dataset (NClimGrid), Version 1 (Monthly Temperature and Precipitation); NOAA National Centers for Environmental Information: Asheville, NC, USA, 2014. [Google Scholar] [CrossRef]
- Field, C.B.; Barros, V.R.; Dokken, D.J.; Mach, K.J.; Mastrandea, M.D. Chapter 11—Human Health: Impacts, adaptation and co-benefits. In Intergovernmental Panel on Climate Change (IPCC); Cambridge University Press: New York, NY, USA, 2014; pp. 709–754. [Google Scholar]
- Hanigan, I.C.; Schirmer, J.; Niyonsenga, T. Drought and distress in southeastern Australia. Environ. Sci. 2018, 109, 13950–13955. [Google Scholar] [CrossRef]
- World Helath Organization (WHO). Gender, Climate Change and Health; World Health Organization: Geneva, Switzerland, 2014; Available online: https://apps.wholint/iris/handle/10665/244781 (accessed on 3 January 2023).
- Berman, J.D.; Ramirez, M.R.; Bell, J.E.; Bilotta, R.; Gerr, F.; Fethke, N.B. The association between drought conditions and increases occupational psychosocial stress among U.S. farmers: An occupational cohort study. Sci. Total Environ. 2021, 798, 149245. [Google Scholar] [CrossRef] [PubMed]
- Friel, S.; Berry, H.; Dinh, H.; OBrien, L.; Walls, H.L. The impact of drought on the association between food security and mental health in a nationally representative Australian sample. BMC Public Health 2014, 14, 1102. [Google Scholar] [CrossRef] [PubMed]
- OBrien, L.V.; Berry, H.L.; Coleman, C.; Hanigan, I.C. Drought as a mental health exposure. Environ. Res. 2014, 131, 181–187. [Google Scholar] [CrossRef]
- Vins, H.; Bell, J.E.; Saha, S.; Hess, J.J. The Mental Health Outcomes of Drought: A Systematic Review and Causal Process Diagram. Int. J. Environ. Res. Public Health 2015, 12, 13251–13275. [Google Scholar] [CrossRef]
- Lookadoo, R.E.; Bell, J.E. Public Health Policy Actions to Address Health Issues Associated with Drought in a Changing Climate. J. Law Med. Ethics 2020, 48, 653–663. [Google Scholar] [CrossRef] [PubMed]
- Zeighami, A.; Kern, J.; Yeates, A.J.; Weber, P.; Bruno, A.A. U.S. West coast droughts and heat waves exacerbate pollution inequality and can evade emission control policies. Nat. Commun. 2023, 14, 1415. [Google Scholar] [CrossRef]
- Libonati, R.; Geirinhas, J.L.; Silva, P.S.; Santos, D.M.; Rodrigues, J.A.; Russo, A.; Peres, L.F.; Narcizo, L.; Gomes, M.E.R.; Rodrigues, A.P.; et al. Drought-heatwave nexus in Brazil and related impacts on health and fires: A comprehensive review. Ann. N. Y. Acad. Sci. 2022, 1517, 44–62. [Google Scholar] [CrossRef]
| Race | Age Group | Male | Female | ||||
|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | ||
| Total | 2,241,979 | 9833.24 | 1685.05 | 2,420,797 | 10,617.53 | 2045.28 | |
| White | 0–19 | 9144 | 40.11 | 13.83 | 6954 | 30.50 | 12.38 |
| 20–39 | 15,984 | 70.11 | 22.18 | 13,103 | 57.47 | 19.32 | |
| 40–64 | 272,667 | 1195.91 | 259.08 | 239,458 | 1050.75 | 249.62 | |
| +65 | 1,711,596 | 7507.00 | 1260.99 | 1,939,091 | 8504.79 | 1639.32 | |
| White Total | 2,009,391 | 8813.12 | 1504.73 | 2,198,606 | 9643.01 | 1860.48 | |
| Black | 0–19 | 744 | 3.26 | 2.25 | 573 | 2.51 | 1.82 |
| 20–39 | 905 | 3.97 | 3.50 | 646 | 2.83 | 1.89 | |
| 40–64 | 7240 | 31.75 | 10.85 | 5560 | 24.39 | 8.95 | |
| +65 | 40,614 | 178.13 | 57.32 | 35,199 | 154.38 | 54.86 | |
| Black Total | 49,503 | 217.12 | 67.97 | 41,978 | 184.11 | 63.38 | |
| Others | 0–19 | 5339 | 23.42 | 5.85 | 3713 | 16.29 | 5.09 |
| 20–39 | 6257 | 27.44 | 6.45 | 5138 | 22.54 | 6.96 | |
| 40–64 | 47,807 | 209.68 | 42.15 | 41,976 | 184.11 | 45.57 | |
| +65 | 123,682 | 502.46 | 89.39 | 129,386 | 567.48 | 108.28 | |
| Others Total | 183,085 | 803.00 | 131.52 | 180,213 | 790.41 | 152.33 | |
| Climate Region | County n | USDM | 6-Month EDDI | 12-Month EDDI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | M | S | No | M | S | No | M | S | ||
| Total | 3107 | 521,813 | 139,047 | 47,536 | 465,495 | 171,999 | 70,902 | 443,610 | 195,772 | 69,014 |
| NE | 245 | 50,638 | 4852 | 370 | 37,668 | 11,228 | 6964 | 34,557 | 13,589 | 7114 |
| (90.7%) | (8.7%) | (0.7%) | (67.4%) | (20.1%) | (12.5%) | (61.9%) | (24.3%) | (13.8%) | ||
| NR | 291 | 43,575 | 16,598 | 6176 | 48,578 | 13,324 | 4546 | 47,271 | 14,407 | 4670 |
| (65.7%) | (25.0%) | (9.3%) | (73.2%) | (19.9%) | (6.9%) | (71.2%) | (21.7%) | (7.0%) | ||
| NW | 119 | 17,136 | 8004 | 1992 | 21,405 | 4566 | 1161 | 21,009 | 4626 | 1497 |
| (63.2%) | (29.5%) | (7.3%) | (78.9%) | (16.8%) | (4.3%) | (77.4%) | (17.0%) | (5.5%) | ||
| OV | 667 | 131,744 | 17,725 | 2607 | 93,700 | 40,194 | 18,182 | 88,925 | 46,136 | 17,015 |
| (86.6%) | (11.7%) | (1.7%) | (61.6%) | (26.4%) | (12.0%) | (58.5%) | (30.3%) | (11.2%) | ||
| S | 657 | 98,560 | 35,761 | 15,475 | 95,239 | 39,179 | 15,378 | 92,430 | 42,532 | 14,834 |
| (65.8%) | (23.9%) | (10.3%) | (63.6%) | (26.2%) | (10.3%) | (61.7%) | (28.4%) | (9.9%) | ||
| SE | 572 | 93,311 | 26,616 | 10,489 | 83,306 | 33,082 | 14,028 | 76,939 | 39,951 | 13,526 |
| (71.5%) | (20.4%) | (8.0%) | (63.9%) | (25.4%) | (10.8%) | (59.0%) | (30.6%) | (10.4%) | ||
| SW | 140 | 15,285 | 10,864 | 5771 | 22,639 | 6417 | 2864 | 22,510 | 6780 | 2630 |
| (47.9%) | (34.0%) | (18.1%) | (70.9%) | (20.1%) | (9.0%) | (70.5%) | (21.2%) | (8.2%) | ||
| UM | 341 | 63,456 | 12,832 | 1460 | 51,630 | 19,735 | 6383 | 49,264 | 22,760 | 5724 |
| (81.6%) | (16.5%) | (1.9%) | (66.4%) | (25.4%) | (8.2%) | (63.4%) | (29.3%) | (7.4%) | ||
| W | 75 | 8108 | 5796 | 3196 | 11,330 | 4374 | 1396 | 10,705 | 4991 | 1404 |
| (47.4%) | (33.9%) | (18.7%) | (66.3%) | (25.6%) | (8.2%) | (62.6%) | (29.2%) | (8.2%) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gwon, Y.; Ji, Y.; Bell, J.E.; Abadi, A.M.; Berman, J.D.; Rau, A.; Leeper, R.D.; Rennie, J. The Association between Drought Exposure and Respiratory-Related Mortality in the United States from 2000 to 2018. Int. J. Environ. Res. Public Health 2023, 20, 6076. https://doi.org/10.3390/ijerph20126076
Gwon Y, Ji Y, Bell JE, Abadi AM, Berman JD, Rau A, Leeper RD, Rennie J. The Association between Drought Exposure and Respiratory-Related Mortality in the United States from 2000 to 2018. International Journal of Environmental Research and Public Health. 2023; 20(12):6076. https://doi.org/10.3390/ijerph20126076
Chicago/Turabian StyleGwon, Yeongjin, Yuanyuan Ji, Jesse E. Bell, Azar M. Abadi, Jesse D. Berman, Austin Rau, Ronald D. Leeper, and Jared Rennie. 2023. "The Association between Drought Exposure and Respiratory-Related Mortality in the United States from 2000 to 2018" International Journal of Environmental Research and Public Health 20, no. 12: 6076. https://doi.org/10.3390/ijerph20126076
APA StyleGwon, Y., Ji, Y., Bell, J. E., Abadi, A. M., Berman, J. D., Rau, A., Leeper, R. D., & Rennie, J. (2023). The Association between Drought Exposure and Respiratory-Related Mortality in the United States from 2000 to 2018. International Journal of Environmental Research and Public Health, 20(12), 6076. https://doi.org/10.3390/ijerph20126076







