Pre- and Post-Pandemic Religiosity and Mental Health Outcomes: A Prospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Sample
2.3. Measures
2.4. Religious Importance (RI)
2.5. Religious Attendance (RA)
2.6. Mental Health Outcomes
2.7. Statistical Analysis
2.7.1. Changes in Religious Importance (RI) and Religious Attendance (RA)
2.7.2. Associations between T1 RI, RA, and Mental Health Outcomes at T2
2.7.3. Associations between T2 RI, RA, and Mental Health Outcomes at T2
2.7.4. Supplemental Analyses: Association between Changes in RI and RA from T1 to T2 and Mental Health Outcomes during the Pandemic (T2)
3. Results
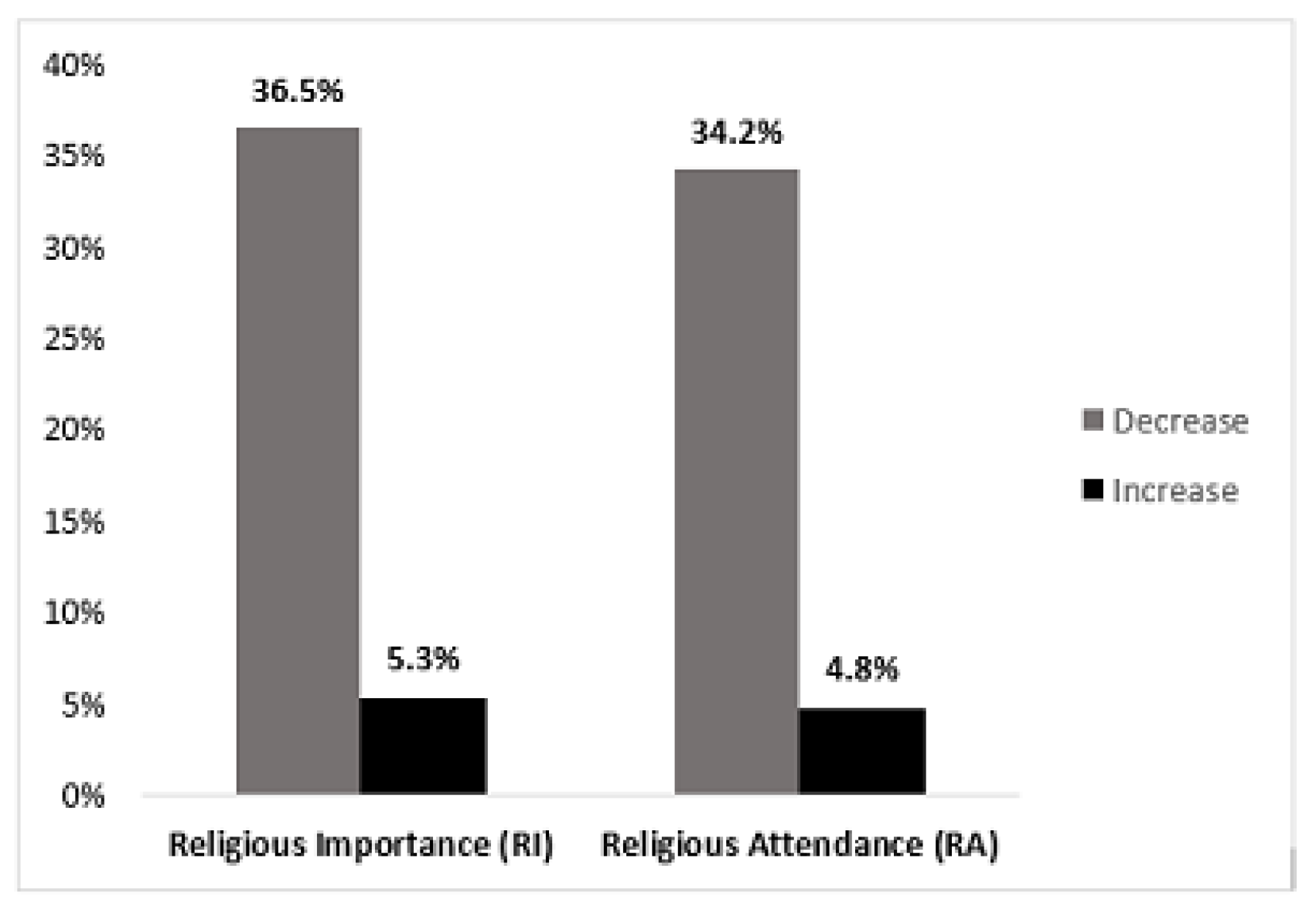
3.1. Change in RI and RA from T1 to T2
3.1.1. Change in Religious Importance (RI)
3.1.2. Change in Religious Attendance (RA)
3.2. Effects of T1 RI and RA on Mental Health Outcomes during Pandemic (T2)
3.2.1. Effects of T1 RI on T2 Mental Health Outcomes
3.2.2. Effects of T1 RA on T2 Mental Health Outcomes
3.3. Effects of T2 RI and RA on Mental Health Outcomes during Pandemic (T2)
3.3.1. Effects of T2 RI on T2 Mental Health Outcomes
3.3.2. Effects of T2 RA on T2 Mental Health Outcomes
3.4. Supplemental Analyses: Factors Associated with Changes in RI and RA from T1–T2
3.4.1. COVID-19 Experiences and Decrease in RI and RA from T1–T2
3.4.2. COVID-19 Experiences and Increase in RI and RA from T1–T2
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Counted, V.; Pargament, K.I.; Bechara, A.O.; Joynt, S.; Cowden, R.G. Hope and well-being in vulnerable contexts during the COVID-19 pandemic: Does religious coping matter? J. Posit. Psychol. 2020, 17, 70–81. [Google Scholar] [CrossRef]
- Goodwin, E.; Kraft, K. Mental health and spiritual well-being in humanitarian crises: The role of faith communities providing spiritual and psychosocial support during the COVID-19 pandemic. J. Int. Humanit. Action 2022, 7, 21. [Google Scholar] [CrossRef]
- Hart, C.W.; Koenig, H.G. Special Section: Religion and Health Response to the COVID-19 Pandemic. J. Relig. Health 2020, 59, 2191–2192. [Google Scholar] [CrossRef]
- Modell, S.M.; Kardia, S.L.R. Religion as a Health Promoter During the 2019/2020 COVID Outbreak: View from Detroit. J. Relig. Health 2020, 59, 2243–2255. [Google Scholar] [CrossRef]
- Pew Research Center. Most Americans Say Coronavirus Outbreak Has Impacted Their Lives. Available online: https://www.pewresearch.org/social-trends/2020/03/30/most-americans-say-coronavirus-outbreak-has-impacted-their-lives/ (accessed on 22 January 2023).
- Chirico, F.; Nucera, G. An Italian Experience of Spirituality from the Coronavirus Pandemic. J. Relig. Health 2020, 59, 2193–2195. [Google Scholar] [CrossRef] [PubMed]
- DeRossett, T.; LaVoie, D.J.; Brooks, D. Religious Coping Amidst a Pandemic: Impact on COVID-19-Related Anxiety. J. Relig. Health 2021, 60, 3161–3176. [Google Scholar] [CrossRef] [PubMed]
- Dobrakowski, P.P.; Skalski, S.; Surzykiewicz, J.; Muszyńska, J.; Konaszewski, K. Religious Coping and Life Satisfaction during the COVID-19 Pandemic among Polish Catholics. The Mediating Effect of Coronavirus Anxiety. J. Clin. Med. 2021, 10, 4865. [Google Scholar] [CrossRef]
- Edara, I.R.; del Castillo, F.; Ching, G.S.; del Castillo, C.D. Religiosity, Emotions, Resilience, and Wellness during the COVID-19 Pandemic: A Study of Taiwanese University Students. Int. J. Environ. Res. Public Health 2021, 18, 6381. [Google Scholar] [CrossRef]
- Frent, S.; Frent, M.; Popovici, A. Religiosity and mental health consequences of COVID-19 pandemic. Eur. Respir. J. 2022, 60 (Suppl. S66), 4280. [Google Scholar] [CrossRef]
- Lucchetti, G.; Góes, L.G.; Amaral, S.G.; Ganadjian, G.T.; Andrade, I.; Almeida, P.O.D.A.; Carmo, V.M.D.; Manso, M.E.G. Spirituality, religiosity and the mental health consequences of social isolation during Covid-19 pandemic. Int. J. Soc. Psychiatry 2020, 67, 672–679. [Google Scholar] [CrossRef]
- Serfaty, D.R.; Lugasi, T.; Strous, R.D. Anxiety Reactions and Coping Modalities with the COVID-19 Pandemic: A Cross-Sectional Study Comparing a Population of Religious Patients with Mental Illness and their Health Caregivers. J. Relig. Health 2021, 60, 1494–1506. [Google Scholar] [CrossRef] [PubMed]
- VanderWeele, T.J. Love of Neighbor During a Pandemic: Navigating the Competing Goods of Religious Gatherings and Physical Health. J. Relig. Health 2020, 59, 2196–2202. [Google Scholar] [CrossRef] [PubMed]
- Długosz, P.; Liszka, D.; Yuzva, L. The Link between Subjective Religiosity, Social Support, and Mental Health among Young Students in Eastern Europe during the COVID-19 Pandemic: A Cross-Sectional Study of Poland and Ukraine. Int. J. Environ. Res. Public Health 2022, 19, 6446. [Google Scholar] [CrossRef] [PubMed]
- Galiatsatos, P.; Monson, K.; Oluyinka, M.; Negro, D.; Hughes, N.; Maydan, D.; Golden, S.H.; Teague, P.; Hale, W.D. Community Calls: Lessons and Insights Gained from a Medical–Religious Community Engagement During the COVID-19 Pandemic. J. Relig. Health 2020, 59, 2256–2262. [Google Scholar] [CrossRef]
- Hong, B.A.; Handal, P.J. Science, Religion, Government, and SARS-CoV-2: A Time for Synergy. J. Relig. Health 2020, 59, 2263–2268. [Google Scholar] [CrossRef] [PubMed]
- Schmuck, J.; Hiebel, N.; Rabe, M.; Schneider, J.; Erim, Y.; Morawa, E.; Jerg-Bretzke, L.; Beschoner, P.; Albus, C.; Hannemann, J.; et al. Sense of coherence, social support and religiosity as resources for medical personnel during the COVID-19 pandemic: A web-based survey among 4324 health care workers within the German Network University Medicine. PLoS ONE 2021, 16, e0255211. [Google Scholar] [CrossRef]
- Chow, S.K.; Francis, B.; Ng, Y.H.; Naim, N.; Beh, H.C.; Ariffin, M.A.A.; Yusuf, M.H.M.; Lee, J.W.; Sulaiman, A.H. Religious Coping, Depression and Anxiety among Healthcare Workers during the COVID-19 Pandemic: A Malaysian Perspective. Healthcare 2021, 9, 79. [Google Scholar] [CrossRef]
- Mahmood, Q.K.; Jafree, S.R.; Sohail, M.M.; Akram, M.B. A Cross-Sectional Survey of Pakistani Muslims Coping with Health Anxiety through Religiosity during the COVID-19 Pandemic. J. Relig. Health 2021, 60, 1462–1474. [Google Scholar] [CrossRef]
- Pirutinsky, S.; Cherniak, A.D.; Rosmarin, D.H. COVID-19, Mental Health, and Religious Coping Among American Orthodox Jews. J. Relig. Health 2020, 59, 2288–2301. [Google Scholar] [CrossRef]
- Rigoli, F. The Link Between COVID-19, Anxiety, and Religious Beliefs in the United States and the United Kingdom. J. Relig. Health 2021, 60, 2196–2208. [Google Scholar] [CrossRef]
- Weissman, M.M. Children of Depressed Parents. Arch. Gen. Psychiatry 1987, 44, 847–853. [Google Scholar] [CrossRef]
- Weissman, M.M. Offspring of Depressed Parents. Arch. Gen. Psychiatry 1997, 54, 932–940. [Google Scholar] [CrossRef] [PubMed]
- Weissman, M.M.; Wickramaratne, P.; Gameroff, M.J.; Warner, V.; Pilowsky, D.; Kohad, R.G.; Verdeli, H.; Skipper, J.; Talati, A. Offspring of Depressed Parents: 30 Years Later. Am. J. Psychiatry 2016, 173, 1024–1032. [Google Scholar] [CrossRef] [PubMed]
- Weissman, M.M.; Wickramaratne, P.; Nomura, Y.; Warner, V.; Pilowsky, D.; Verdeli, H. Offspring of Depressed Parents: 20 Years Later. Am. J. Psychiatry 2006, 163, 1001–1008. [Google Scholar] [CrossRef]
- Svob, C.; Reich, L.; Wickramaratne, P.; Warner, V.; Weissman, M.M. 6.149 Religion and Spirituality Predict Lower Rates of Suicide Attempts and Ideation in Children and Adolescents at Risk for Major Depressive Disorder. J. Am. Acad. Child Adolesc. Psychiatry 2016, 10, S251. [Google Scholar] [CrossRef]
- Svob, C.; Weissman, M.M. The role of religiosity in families at high-risk for depression. Ethics Med. Public Health 2019, 9, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Svob, C.; Wickramaratne, P.J.; Reich, L.; Zhao, R.; Talati, A.; Gameroff, M.J.; Saeed, R.; Weissman, M.M. Association of Parent and Offspring Religiosity with Offspring Suicide Ideation and Attempts. JAMA Psychiatry 2018, 75, 1062–1070. [Google Scholar] [CrossRef]
- Qualtrics. Qualtrics Software; Qualtrics: River Park Drive Provo, UT, USA, 2020; Available online: https://www.qualtrics.com (accessed on 1 January 2023).
- Murphy, E.; Svob, C.; Van Dijk, M.; Gameroff, M.J.; Skipper, J.; Abraham, E.; Yangchen, T.; Posner, J.; Shankman, S.A.; Wickramaratne, P.J.; et al. The effects of the pandemic on mental health in persons with and without a psychiatric history. Psychol. Med. 2021, 53, 2476–2484. [Google Scholar] [CrossRef] [PubMed]
- Endicott, J. A Diagnostic Interview. Arch. Gen. Psychiatry 1978, 35, 837–844. [Google Scholar] [CrossRef]
- Leckman, J.F. Best Estimate of Lifetime Psychiatric Diagnosis. Arch. Gen. Psychiatry 1982, 39, 879–883. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; O’Hara, M.W.; Chmielewski, M.; McDade-Montez, E.A.; Koffel, E.; Naragon, K.; Stuart, S. Further validation of the IDAS: Evidence of convergent, discriminant, criterion, and incremental validity. Psychol. Assess. 2008, 20, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Watson, D.; O’Hara, M.W.; Naragon-Gainey, K.; Koffel, E.; Chmielewski, M.; Kotov, R.; Stasik, S.M.; Ruggero, C.J. Development and Validation of New Anxiety and Bipolar Symptom Scales for an Expanded Version of the IDAS (the IDAS-II). Assessment 2012, 19, 399–420. [Google Scholar] [CrossRef] [PubMed]
- Rzepa, S.; Weissman, M. Social Adjustment Scale Self-Report (SAS-SR). In Encyclopedia of Quality of Life and Well-Being Research; Michalos, A.C., Ed.; Springer: Berlin/Heidelberg, Germany, 2014; pp. 6017–6021. [Google Scholar] [CrossRef]
- Maxwell, A.E. Comparing the Classification of Subjects by Two Independent Judges. Br. J. Psychiatry 1970, 116, 651–655. [Google Scholar] [CrossRef] [PubMed]
- McNemar, Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 1947, 12, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Stuart, A. A Test for Homogeneity of the Marginal Distributions in a Two-Way Classification. Biometrika 1955, 42, 412–416. [Google Scholar] [CrossRef]
- Agresti, A. An Introduction to Categorical Data Analysis, 2nd ed.; Wiley & Sons, Inc.: Gainsville, FL, USA, 2002; p. 372. [Google Scholar]
- Agresti, A.; Natarajan, R. Modeling Clustered Ordered Categorical Data: A Survey. Int. Stat. Rev. 2001, 69, 345–371. [Google Scholar] [CrossRef]
- Kang, J.H.; Mason, R.N.; Tarshis, T.P. 51.14 Relationship between Religion/Spirituality and Mental Health in Youth during COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, S255. [Google Scholar] [CrossRef]
- Kowalczyk, O.; Roszkowski, K.; Montane, X.; Pawliszak, W.; Tylkowski, B.; Bajek, A. Religion and Faith Perception in a Pandemic of COVID-19. J. Relig. Health 2020, 59, 2671–2677. [Google Scholar] [CrossRef]
- Francis, B.; Ken, C.S.; Han, N.Y.; Ariffin, M.A.A.; Yusuf, M.H.; Wen, L.J.; Petrus, C.F.; Chin, B.H.; Gill, J.S.; Sulaiman, A.H.; et al. Religious Coping During the COVID-19 Pandemic: Gender, Occupational and Socio-economic Perspectives Among Malaysian Frontline Healthcare Workers. Alpha Psychiatry 2021, 22, 194–199. [Google Scholar] [CrossRef]
- Hvidtjørn, D.; Hjelmborg, J.; Skytthe, A.; Christensen, K.; Hvidt, N.C. Religiousness and Religious Coping in a Secular Society: The Gender Perspective. J. Relig. Health 2014, 53, 1329–1341. [Google Scholar] [CrossRef] [PubMed]
- Mirola, W.A. A Refuge for Some: Gender Differences in the Relationship between Religious Involvement and Depression. Sociol. Relig. 1999, 60, 419–437. [Google Scholar] [CrossRef]
- Norton, M.C.; Skoog, I.; Franklin, L.M.; Corcoran, C.; Tschanz, J.T.; Zandi, P.P.; Breitner, J.C.S.; Welsh-Bohmer, K.A.; Steffens, D.C. Gender Differences in the Association Between Religious Involvement and Depression: The Cache County (Utah) Study. J. Gerontol. Ser. B 2006, 61, P129–P136. [Google Scholar] [CrossRef] [PubMed]

| MENTAL HEALTH OUTCOMES 1 | Religious Importance (RI) | Religious Attendance (RA) | ||
|---|---|---|---|---|
| B (s.e. B) | p-Value | B (s.e.B) | p-Value | |
| PHQ-9 | ||||
| Depression | −0.08 (0.28) | 0.777 | 0.19 (0.32) | 0.541 |
| Suicidality | 0.01 (0.02) | 0.721 | −0.01 (0.02) | 0.602 |
| IDAS-II | ||||
| Depression | −0.22 (0.65) | 0.734 | 0.15 (0.67) | 0.823 |
| Suicidality | −0.20 (0.10) | 0.050 1 | −0.01 (0.11) | 0.929 |
| Anxiety | −0.14 (0.18) | 0.462 | 0.04 (0.19) | 0.821 |
| Traumatic Symptoms | 0.18 (0.18) | 0.314 | 0.44 (0.18) | 0.084 1 |
| Well-Being | −0.004 (0.41) | 0.992 | −0.31 (0.41) | 0.458 |
| SASSR | ||||
| Overall Social Adjustment | −0.10 (0.03) | 0.027 | −0.03 (0.03) | 0.376 |
| MENTAL HEALTH OUTCOMES 1 | Religious Importance (RI) | Religious Attendance (RA) | ||
|---|---|---|---|---|
| B (s.e. B) | p-Value | B (s.e.B) | p-Value | |
| PHQ-9 | ||||
| Depression | 0.15 (0.45) | 0.738 | −0.76 (0.43) | 0.079 1 |
| Suicidality | −0.06 (0.03) | 0.027 | −0.02 (0.03) | 0.569 |
| IDAS-II | ||||
| Depression | −0.35 (1.05) | 0.740 | −1.67 (0.99) | 0.095 1 |
| Suicidality | −0.002 (0.16) | 0.989 | −0.01 (0.16) | 0.950 |
| Anxiety | −0.39 (0.29) | 0.191 | −0.33 (0.28) | 0.248 |
| Traumatic Symptoms | 0.17 (0.28) | 0.560 | −0.11 (0.27) | 0.683 |
| Well-Being | 0.68 (0.65) | 0.301 | 0.33 (0.62) | 0.595 |
| SASSR | ||||
| Overall Social Adjustment | −0.03 (0.04) | 0.518 | −0.05 (0.04) | 0.208 |
| MENTAL HEALTH OUTCOMES 1 | B (s.e. B) | p-Value |
|---|---|---|
| PHQ-9 | ||
| Depression | −0.76 (0.50) | 0.133 |
| Suicidality | −0.03 (0.03) | 0.348 |
| IDAS-II | ||
| Depression | −2.35 (1.16) | 0.043 |
| Suicidality | −0.13 (0.18) | 0.473 |
| Anxiety | −0.72 (0.33) | 0.029 |
| Traumatic Symptoms | −0.52 (0.31) | 0.097 1 |
| Well-Being | 1.1 (0.73) | 0.131 |
| SASSR | ||
| Overall Social Adjustment | −0.07 (0.05) | 0.144 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Svob, C.; Murphy, E.; Wickramaratne, P.J.; Gameroff, M.J.; Talati, A.; van Dijk, M.T.; Yangchen, T.; Weissman, M.M. Pre- and Post-Pandemic Religiosity and Mental Health Outcomes: A Prospective Study. Int. J. Environ. Res. Public Health 2023, 20, 6002. https://doi.org/10.3390/ijerph20116002
Svob C, Murphy E, Wickramaratne PJ, Gameroff MJ, Talati A, van Dijk MT, Yangchen T, Weissman MM. Pre- and Post-Pandemic Religiosity and Mental Health Outcomes: A Prospective Study. International Journal of Environmental Research and Public Health. 2023; 20(11):6002. https://doi.org/10.3390/ijerph20116002
Chicago/Turabian StyleSvob, Connie, Eleanor Murphy, Priya J. Wickramaratne, Marc J. Gameroff, Ardesheer Talati, Milenna T. van Dijk, Tenzin Yangchen, and Myrna M. Weissman. 2023. "Pre- and Post-Pandemic Religiosity and Mental Health Outcomes: A Prospective Study" International Journal of Environmental Research and Public Health 20, no. 11: 6002. https://doi.org/10.3390/ijerph20116002
APA StyleSvob, C., Murphy, E., Wickramaratne, P. J., Gameroff, M. J., Talati, A., van Dijk, M. T., Yangchen, T., & Weissman, M. M. (2023). Pre- and Post-Pandemic Religiosity and Mental Health Outcomes: A Prospective Study. International Journal of Environmental Research and Public Health, 20(11), 6002. https://doi.org/10.3390/ijerph20116002





