Specialized Care Resources for Diagnosis and Management of Patients Who Have Suffered Falls: Results of a National Survey in Geriatric Units
Abstract
1. Introduction
2. Materials and Methods
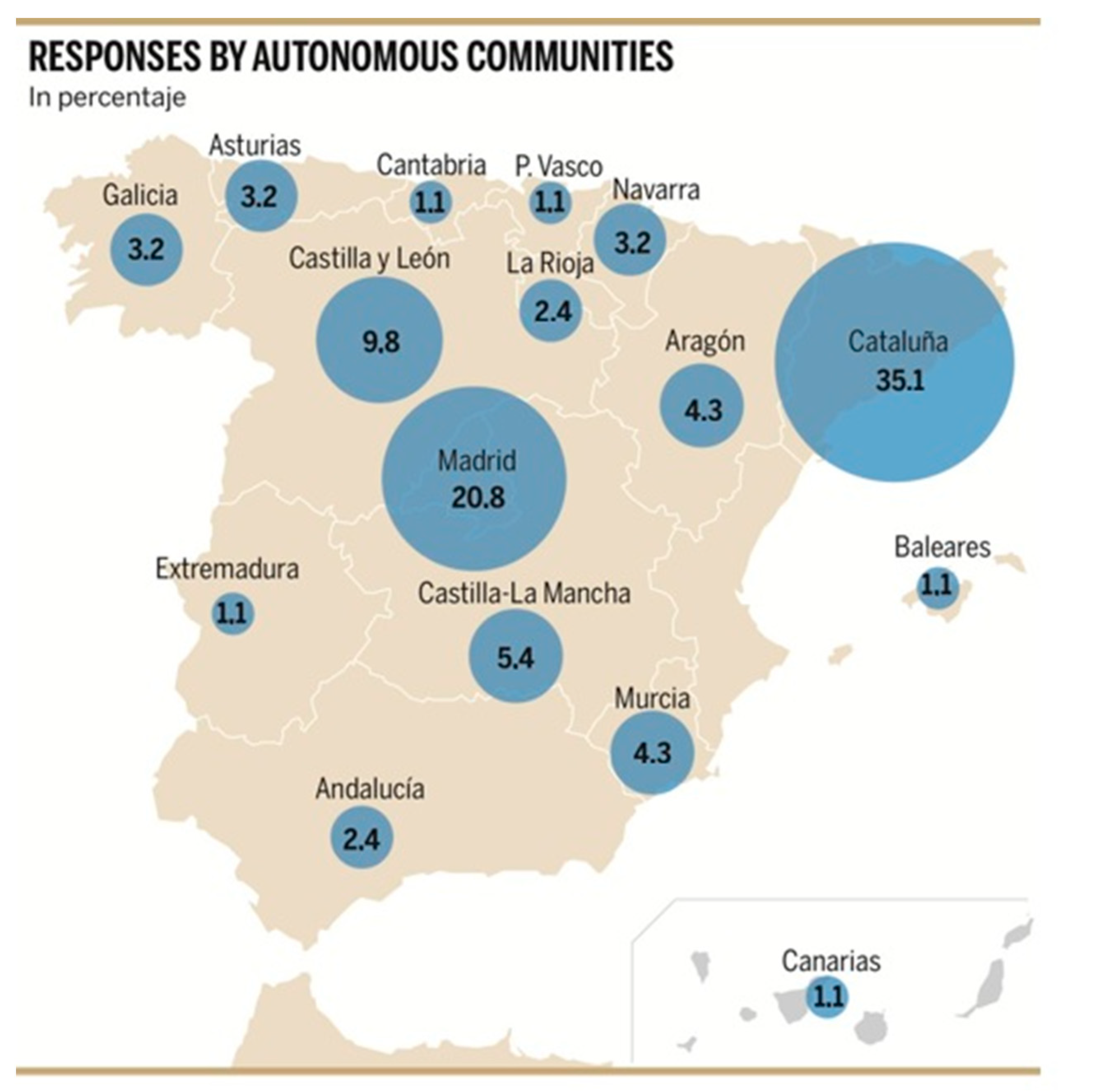
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Survey
- Regarding the assessment and diagnosis of falls. Please indicate only one of the following options, as the most valid in the practice of your unit or service:
- 2.
- Regarding the tools for assessing the falls in your Service. Please tick all the valid options:
- 3.
- How many patients per month are evaluated in this consultation?:
- 4.
- Do you carry out any scientific activity in relation to falls in your unit/service? If so, could you indicate the line of investigation?
- 5.
- Would someone in your service be interested in collaborating in multicenter studies on falls?
- 6.
- Regarding intervention programs with physical exercise at the hospital level. Which of the following options is more valid in the practice of your unit or service:
- 7.
- Regarding intervention programs with physical exercise at the community level. Which of the following options is closest to your usual practice (several can be indicated):
References
- Tinetti, M.E.; Speechley, M.; Ginter, S.F. Risk Factors for Falls Among Elderly Persons Living in the Community. N. Engl. J. Med. 1988, 319, 1701–1707. [Google Scholar] [CrossRef]
- Pérez-Ros, P.; Martínez-Arnau, F.M.; Tarazona-Santabalbina, F.J. Risk Factors and Number of Falls as Determinants of Quality of Life of Community-Dwelling Older Adults. J. Geriatr. Phys. Ther. 2019, 42, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Cardiovascular Health Study Collaborative Research Group. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J. Am. Geriatr. Soc. 2001, 49, 664–672.
- Panel on Prevention of Falls in Older Persons; American Geriatrics Society; British Geriatrics Society. Summary of the Updated American Geriatrics Society/British Geriatrics Society Clinical Practice Guideline for Prevention of Falls in Older Persons. J. Am. Geriatr. Soc. 2011, 59, 148–157. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Van der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World Guidelines for Falls Prevention and Management for Older Adults: A Global Initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef]
- DiBardino, D.; Cohen, E.R.; Didwania, A. meta-Analysis: Multidisciplinary Fall Prevention Strategies in the Acute Care Inpatient Population. J. Hosp. Med. 2012, 7, 497–503. [Google Scholar] [CrossRef]
- Gillespie, L.D.; Robertson, M.C.; Gillespie, W.J.; Sherrington, C.; Gates, S.; Clemson, L.M.; Lamb, S.E. Interventions for Preventing Falls in Older People Living in the Community. Cochrane Database Syst. Rev. 2012, CD007146. [Google Scholar] [CrossRef]
- Preventing Falls and Harm From Falls in Older People. Best Practice Guidelines for Australian Community Care. Available online: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/preventing-falls-and-harm-falls-older-people-guidebook-australian-community-care (accessed on 26 April 2021).
- Alcalde Tirado, P. Miedo a Caerse [Fear of falling]. Rev. Esp. Geriatr. Gerontol. 2010, 45, 38–44. [Google Scholar] [CrossRef]
- Dent, E.; Lien, C.; Lim, W.S.; Wong, W.C.; Wong, C.H.; Ng, T.P.; Woo, J.; Dong, B.; De la Vega, S.; Hua Poi, P.J.; et al. The Asia-Pacific Clinical Practice Guidelines for the Management of Frailty. J. Am. Med. Dir. Assoc. 2017, 18, 564–575. [Google Scholar] [CrossRef]
- Falls: Assessment and Prevention of Falls in Older People. Available online: www.nice.org.uk/guidance/CG161 (accessed on 7 September 2018).
- Gomez, F.; Curcio, C.L.; Brennan-Olsen, S.L.; Boersma, D.; Phu, S.; Vogrin, S.; Suriyaarachchi, P.; Duque, G. Effects of the Falls and Fractures Clinic as an Integrated Multidisciplinary Model of Care in Australia: A Pre-Post Study. BMJ Open 2019, 9, e027013. [Google Scholar] [CrossRef]
- Cameron, I.D.; Dyer, S.M.; Panagoda, C.E.; Murray, G.R.; Hill, K.D.; Cumming, R.G.; Kerse, N. Interventions for Preventing Falls in Older People in Care Facilities and Hospitals. Cochrane Database Syst. Rev. 2018, CD005465. [Google Scholar] [CrossRef] [PubMed]
- Perell, K.L.; Manzano, M.L.; Weaver, R.; Fiuzat, M.; Voss-McCarthy, M.; Opava-Rutter, D.; Castle, S.C. Outcomes of a Consult Fall Prevention Screening Clinic. Am. J. Phys. Med. Rehabil. 2006, 85, 882–888. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Miller, M.; Whitehead, C.; Crotty, M. Falls Clinics: An Opportunity To Address Frailty and Improve Health Outcomes (Preliminary Evidence). Aging Clin. Exp. Res. 2010, 22, 170–174. [Google Scholar] [CrossRef]
- 2018 NICE Impact Report on Falls and Fragility Fractures. Available online: https://www.bgs.org.uk/resources/2018-nice-impact-report-on-falls-and-fragility-fractures. (accessed on 29 August 2018).
- Baker, R. Gait Analysis Methods in Rehabilitation. J. Neuroeng. Rehabil. 2006, 3, 4. [Google Scholar] [CrossRef]
- Graham, J.E.; Ostir, G.V.; Kuo, Y.F.; Fisher, S.R.; Ottenbacher, K.J. Relationship between Test Methodology and Mean Velocity in Timed Walk Tests: A Review. Arch. Phys. Med. Rehabil. 2008, 89, 865–872. [Google Scholar] [CrossRef]
- Graham, J.E.; Ostir, G.V.; Fisher, S.R.; Ottenbacher, K.J. Assessing Walking Speed in Clinical Research: A Systematic Review. J. Eval. Clin. Pract. 2008, 14, 552–562. [Google Scholar] [CrossRef]
- Falls. Available online: http://www.who.int/mediacentre/factsheets/fs344/es/.2018 (accessed on 26 April 2021).
- Casas Herrero, Á.; Cadore, E.L.; Martínez Velilla, N.; Izquierdo Redin, M. Physical Exercise in the Frail Elderly: An Update. Rev. Esp. Geriatr. Gerontol. 2015, 50, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Lopez, P.; Pinto, R.S.; Radaelli, R.; Rech, A.; Grazioli, R.; Izquierdo, M.; Cadore, E.L. Benefits of Resistance Training in Physically Frail Elderly: A Systematic Review. Aging Clin. Exp. Res. 2018, 30, 889–899. [Google Scholar] [CrossRef]
- Lopez, P.; Izquierdo, M.; Radaelli, R.; Sbruzzi, G.; Grazioli, R.; Pinto, R.S.; Cadore, E.L. Effectiveness of Multimodal Training on Functional Capacity in Frail Older People: A Meta-Analysis of Randomized Controlled Trials. J. Aging Phys. Act. 2018, 26, 407–418. [Google Scholar] [CrossRef]
- Viladrosa, M.; Casanova, C.; Ghiorghies, A.C.; Jürschik, P. Effectiveness of Physical Exercise on Fitness in Frail Older Adults: A Systematic Review of Randomised Trials. Rev. Esp. Geriatr. Gerontol. 2017, 52, 332–341. [Google Scholar] [CrossRef]
- García-Molina, R.; Ruíz-Grao, M.C.; Noguerón-García, A.; Martínez-Reig, M.; Esbrí-Víctor, M.; Izquierdo, M.; Abizanda, P. Benefits of a Multicomponent Falls Unit-Based Exercise Program in Older Adults With Falls in Real Life. Exp. Gerontol. 2018, 110, 79–85. [Google Scholar] [CrossRef]
- Ramirez-Campillo, R.; Diaz, D.; Martinez-Salazar, C.; Valdés-Badilla, P.; Delgado-Floody, P.; Méndez-Rebolledo, G.; Cañas-Jamet, R.; Cristi-Montero, C.; García-Hermoso, A.; Celis-Morales, C.; et al. Effects of Different Doses of High-Speed Resistance Training on Physical Performance and Quality of Life in Older Women: A Ran-Domized Controlled Trial. Clin. Interv. Aging. 2016, 11, 1797–1804. [Google Scholar] [CrossRef]
- Toraman, N.F.; Ayceman, N. Effects of Six Weeks of Detraining on Retention of Functional Fitness of Old People After Nine Weeks of Multicomponent Training. Br. J. Sports Med. 2005, 39, 565–568. [Google Scholar] [CrossRef]
- Falls in Older People: Assessing Risk and Prevention. Available online: https://www.nice.org.uk/guidance/cg161 (accessed on 12 June 2013).
- Vogler, C.M.; Menant, J.C.; Sherrington, C.; Ogle, S.J.; Lord, S.R. Evidence of Detraining After 12-Week Home-Based Exercise Programs Designed To Reduce Fall-Risk Factors in Older People Recently Discharged From Hospital. Arch. Phys. Med. Rehabil. 2012, 93, 1685–1691. [Google Scholar] [CrossRef]
- Eggenberger, P.; Theill, N.; Holenstein, S.; Schumacher, V.; De Bruin, E.D. Multicomponent Physical Exercise With Simultaneous Cognitive Training To Enhance Dual-Task Walking of Older Adults: A Secondary Analysis of a 6-Month Randomized Controlled Trial With 1-Year Follow-Up. Clin. Interv. Aging 2015, 10, 1711–1732. [Google Scholar] [CrossRef] [PubMed]
- Tarazona-Santabalbina, F.J.; Gómez-Cabrera, M.C.; Pérez-Ros, P.; Martínez-Arnau, F.M.; Cabo, H.; Tsaparas, K.; Salvador-Pascual, A.; Rodriguez-Mañas, L.; Viña, J.A. Multicomponent Exercise Intervention That Reverses Frailty and Improves Cognition, Emotion, and Social Networking in the Community-Dwelling Frail Elderly: A Randomized Clinical Trial. J. Am. Med. Dir. Assoc. 2016, 17, 426–433. [Google Scholar] [CrossRef] [PubMed]
- Casas-Herrero, Á.; Sáez de Asteasu, M.L.; Antón-Rodrigo, I.; Sánchez-Sánchez, J.L.; Montero-Odasso, M.; Marín-Epelde, I.; Ramón-Espinoza, F.; Zambom-Ferraresi, F.; Petidier-Torregrosa, R.; Elexpuru-Estomba, J.; et al. Effects of Vivifrail Multicomponent Intervention on Functional Capacity: A Multicentre, Randomized Controlled Trial. J. Cachexia Sarcopenia Muscle 2022, 13, 884–893. [Google Scholar] [CrossRef]
- Estrategia De Promoción de la Salud y Prevención en el SNS. Actualización Del Documento de Consenso Sobre Prevención de la Fragilidad en la Persona Mayor (2022). Available online: https://www.sanidad.gob.es/ciudadanos/pdf/Estrategia_de_Salud_Publica_2022.pdf (accessed on 5 May 2022).
- Casas Anguita, J.; Repullo Labrador, J.R.; Donaldo Campos, J. La encuesta como técnica de investigación. Elaboración de cuestionarios y tratamiento estadístico de los datos. Aten. Primaria 2003, 31, 527–538. [Google Scholar] [CrossRef] [PubMed]
| Resources | Frequency | Percentage |
|---|---|---|
| A consultation dedicated to the evaluation of falls | 5 | 5.5 |
| A general outpatient clinic (not dedicated to falls) with a specific fall assessment protocol | 14 | 15.4 |
| A general geriatric outpatient clinic with comprehensive geriatric assessment of geriatric syndromes | 45 | 49.5 |
| A multidisciplinary fall assessment unit located in a geriatric day hospital | 11 | 12.1 |
| A multidisciplinary fall assessment unit not located in a geriatric day hospital | 13 | 14.3 |
| No answer | 3 | 3.3 |
| Total | 83 | 100 |
| Fall Assessment Tools | Frequency | Percentage |
|---|---|---|
| Posturograph, device for gait evaluation, functional tests and dynamometer | 5 | 5.5 |
| Posturograph without device for gait evaluation or functional tests | 5 | 5.5 |
| Functional test and gait evaluation device | 2 | 2.2 |
| Evaluation with functional tests only | 68 | 74.7 |
| Grip strength assessment with dynamometer only | 1 | 1.2 |
| No answer | 5 | 5.5 |
| Total | 91 | 100 |
| Number of Patients/Month | Frequency | Percentage |
|---|---|---|
| 1–5 | 23 | 25.3 |
| 6–10 | 19 | 20.9 |
| 11–20 | 29 | 31.0 |
| >20 | 17 | 18.7 |
| No answer | 3 | 3.3 |
| Total | 91 | 100 |
| Intervention | Frequency | Percentage |
|---|---|---|
| Multidisciplinary fall assessment unit with physical exercise program | 10 | 11 |
| Exercise or rehabilitation program in geriatric day hospital but not designed for falls | 16 | 17.6 |
| Fall-specific exercise program performed in the hospital but not part of the falls unit | 27 | 29.7 |
| No rehabilitation/exercise program for gait or falls | 36 | 39.6 |
| Prescription of exercise at home with already known protocols or guidelines (such as those of Vivifrail) | 1 | 1.1 |
| No answer | 1 | 1.1 |
| Total | 91 | 100 |
| Number of People Participating in the Exercise Programs Each Month | Frequency | Percentage | Percentage without an Answer |
|---|---|---|---|
| 5–10 | 5 | 5.5 | 71.4 |
| 11–15 | 1 | 1.1 | 14.3 |
| >16 | 1 | 1.1 | 14.3 |
| No answer | 84 | 92.3 | |
| Total | 91 | 100 | 100 |
| Providers’ Knowledge about Exercise Programs | Frequency | Percentage |
|---|---|---|
| I do not know what resources are available at the community level in my area | 18 | 19.8 |
| There is a specific fall or gait intervention program that I can refer my patients to | 11 | 12.1 |
| There are resources in my area but I do not know how I can refer patients from the hospital | 1 | 1.1 |
| There are resources that provide specific exercise programs that are not specific to falls or walking | 16 | 17.6 |
| We do not have an established protocol and general recommendations are given | 28 | 30.8 |
| We prescribe exercise at home with already known protocols or guidelines (such as those of Vivifrail) | 15 | 16.5 |
| No answer | 2 | 2.2 |
| Total | 91 | 100 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartolomé Martín, I.; Esteve Arríen, A.; Neira Álvarez, M.; Cristofori, G.; Cedeno-Veloz, B.A.; Esbrí Víctor, M.; Pérez Pena, B.; González Ramírez, A.; Caballero-Mora, M.Á.; on behalf of the Falls Study Group of Sociedad Española de Medicina Geriátrica (SEMEG). Specialized Care Resources for Diagnosis and Management of Patients Who Have Suffered Falls: Results of a National Survey in Geriatric Units. Int. J. Environ. Res. Public Health 2023, 20, 5975. https://doi.org/10.3390/ijerph20115975
Bartolomé Martín I, Esteve Arríen A, Neira Álvarez M, Cristofori G, Cedeno-Veloz BA, Esbrí Víctor M, Pérez Pena B, González Ramírez A, Caballero-Mora MÁ, on behalf of the Falls Study Group of Sociedad Española de Medicina Geriátrica (SEMEG). Specialized Care Resources for Diagnosis and Management of Patients Who Have Suffered Falls: Results of a National Survey in Geriatric Units. International Journal of Environmental Research and Public Health. 2023; 20(11):5975. https://doi.org/10.3390/ijerph20115975
Chicago/Turabian StyleBartolomé Martín, Irene, Ainhoa Esteve Arríen, Marta Neira Álvarez, Giovanna Cristofori, Bernardo Abel Cedeno-Veloz, Mariano Esbrí Víctor, Bárbara Pérez Pena, Alfonso González Ramírez, María Ángeles Caballero-Mora, and on behalf of the Falls Study Group of Sociedad Española de Medicina Geriátrica (SEMEG). 2023. "Specialized Care Resources for Diagnosis and Management of Patients Who Have Suffered Falls: Results of a National Survey in Geriatric Units" International Journal of Environmental Research and Public Health 20, no. 11: 5975. https://doi.org/10.3390/ijerph20115975
APA StyleBartolomé Martín, I., Esteve Arríen, A., Neira Álvarez, M., Cristofori, G., Cedeno-Veloz, B. A., Esbrí Víctor, M., Pérez Pena, B., González Ramírez, A., Caballero-Mora, M. Á., & on behalf of the Falls Study Group of Sociedad Española de Medicina Geriátrica (SEMEG). (2023). Specialized Care Resources for Diagnosis and Management of Patients Who Have Suffered Falls: Results of a National Survey in Geriatric Units. International Journal of Environmental Research and Public Health, 20(11), 5975. https://doi.org/10.3390/ijerph20115975







