Impact of National Tobacco Control Policy on Rates of Hospital Admission for Pneumonia: When Compliance Matters
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Tobacco Control Implementation Scale
2.3. Statistical Data Processing
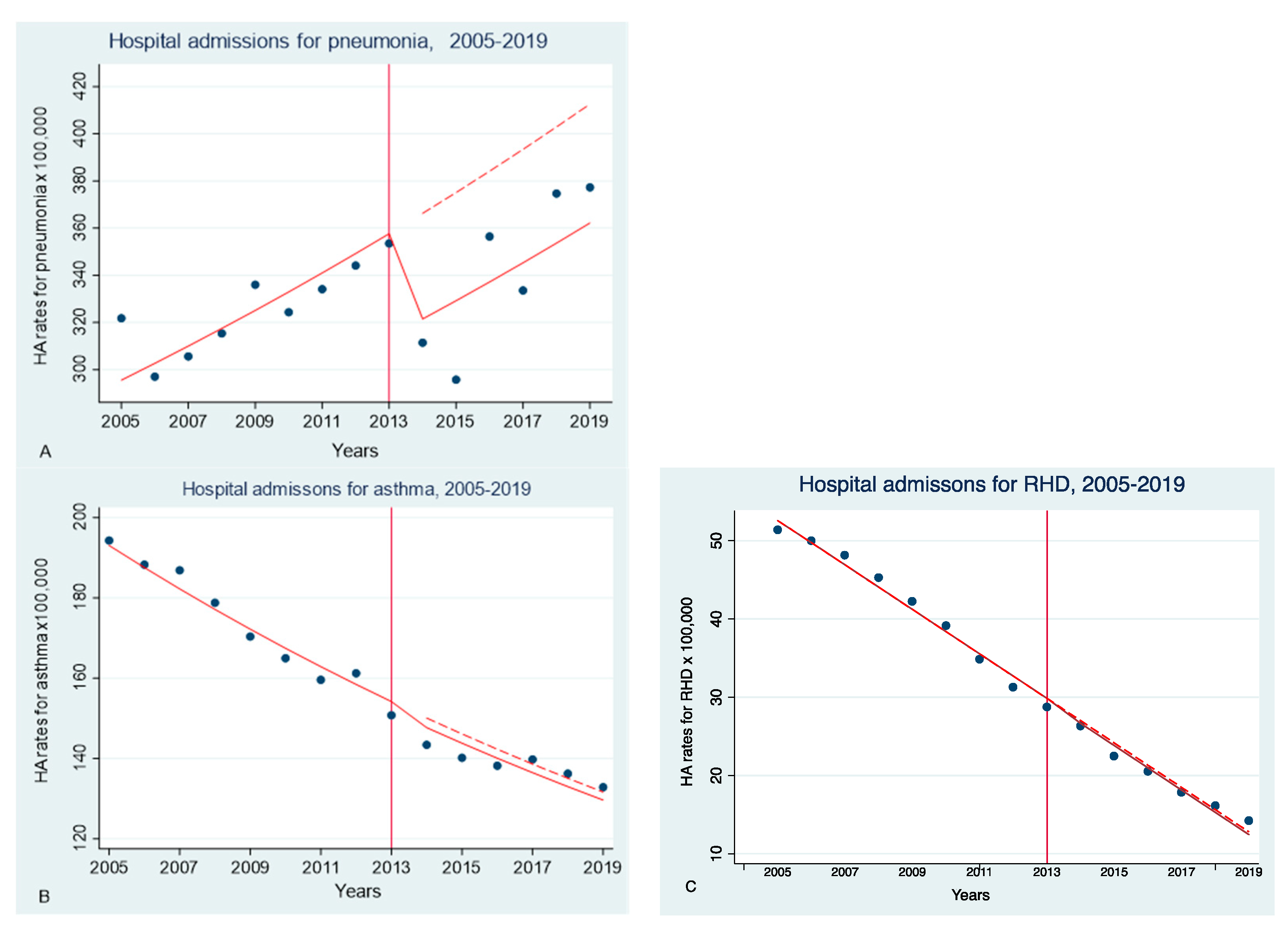
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Tax and Price Measures in Tobacco Control | Protection from Tobacco Smoke | Information and Communication Measures | Rising Awareness about Tobacco Advertising and Promotion | Warning Signs | Offering Help for Smoking Cessation | All Measures | |
|---|---|---|---|---|---|---|---|
| Maximum possible score | 30 | 22 | 15 | 13 | 10 | 10 | 100 |
| All regions | 17.0 | 19.6 | 12.7 | 11.2 | 7.7 | 5.8 | 73.9 |
| The Chuvash Republic | 28.9 | 21.1 | 14.25 | 13.0 | 6.4 | 9.5 | 93.1 |
| Astrakhan Oblast | 25.2 | 20.7 | 12.9 | 11.9 | 7.5 | 7.5 | 85.8 |
| Orenburg Oblast | 16.4 | 18.2 | 14.3 | 11.0 | 8.3 | 4.8 | 73.0 |
| Primorskyi Krai | 19.1 | 19.3 | 11.5 | 11.2 | 7.7 | 3.7 | 72.5 |
| Krasnodar Krai | 15.9 | 17.8 | 13.8 | 11.0 | 8.4 | 5.3 | 72.3 |
| Novosibirsk Oblast | 17.0 | 20.6 | 11.0 | 11.3 | 7.4 | 4.6 | 71.9 |
| Samara Oblast | 15.6 | 18.4 | 12.5 | 10.2 | 7.6 | 7.3 | 71.6 |
| Belgorod Oblast | 14.2 | 21.5 | 12.2 | 9.7 | 8.3 | 5.1 | 70.8 |
| Arkhangelsk Oblast | 17.2 | 18.0 | 13.1 | 10.4 | 7.7 | 3.9 | 70.3 |
| Tyumen Oblast | 9.6 | 20.7 | 13.5 | 11.7 | 7.7 | 6.4 | 69.5 |
References
- Carreras, G.; Lugo, A.; Gallus, S.; Cortini, B.; Fernández, E.; López, M.J.; Soriano, J.B.; López-Nicolás, A.; Semple, S.; Gorini, G.; et al. Burden of disease attributable to second-hand smoke exposure: A systematic review. Prev. Med. 2019, 129, 105833. [Google Scholar] [CrossRef]
- Goodchild, M.; Nargis, N.; D’Espaignet, E.T. Global economic cost of smoking-attributable diseases. Tob. Control. 2018, 27, 58–64. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018. Available online: https://www.who.int/publications/i/item/ncd-country-profiles-2018 (accessed on 15 March 2023).
- Christensen, T.M.; Møller, L.; Jørgensen, T.; Pisinger, C. The impact of the Danish smoking ban on hospital admissions for acute myocardial infarction. Eur. J. Prev. Cardiol. 2014, 21, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Séguret, F.; Ferreira, C.; Cambou, J.-P.; Carriere, I.; Thomas, D. Changes in hospitalization rates for acute coronary syndrome after a two-phase comprehensive smoking ban. Eur. J. Prev. Cardiol. 2013, 21, 1575–1582. [Google Scholar] [CrossRef] [PubMed]
- Cox, B.; Vangronsveld, J.; Nawrot, T.S. Impact of stepwise introduction of smoke-free legislation on population rates of acute myocardial infarction deaths in Flanders, Belgium. Heart 2014, 100, 1430–1435. [Google Scholar] [CrossRef]
- Barone-Adesi, F.; Gasparrini, A.; Vizzini, L.; Merletti, F.; Richiardi, L. Effects of Italian Smoking Regulation on Rates of Hospital Admission for Acute Coronary Events: A Country-Wide Study. PLoS ONE 2011, 6, e17419. [Google Scholar] [CrossRef]
- Kent, B.D.; Sulaiman, I.; Nicholson, T.T.; Lane, S.J.; Moloney, E.D. Acute Pulmonary Admissions Following Implementation of a National Workplace Smoking Ban. Chest 2012, 142, 673–679. [Google Scholar] [CrossRef] [PubMed]
- Humair, J.-P.L.A.; Garin, N.; Gerstel, E.; Carballo, S.; Carballo, D.; Keller, P.-F.; Guessous, I. Acute Respiratory and Cardiovascular Admissions after a Public Smoking Ban in Geneva, Switzerland. PLoS ONE 2014, 9, e90417. [Google Scholar] [CrossRef]
- Galán, I.; Simón, L.; Flores, V.; Ortiz, C.; Fernández-Cuenca, R.; Linares, C.; Boldo, E.; Medrano, M.J.; Pastor-Barriuso, R. Assessing the effects of the Spanish partial smoking ban on cardiovascular and respiratory diseases: Methodological issues. BMJ Open 2015, 5, e008892. [Google Scholar] [CrossRef]
- Kabir, Z.; Caputi, T. OP89 The impact of smoke-free legislation in ireland on lung cancer incidence and mortality. J. Epidemiol. Community Health 2019, 73, A44. [Google Scholar] [CrossRef]
- Gredner, T.; Mons, U.; Niedermaier, T.; Brenner, H.; Soerjomataram, I. Impact of tobacco control policies implementation on future lung cancer incidence in Europe: An international, population-based modeling study. Lancet Reg. Health Eur. 2021, 4, 100074. [Google Scholar] [CrossRef]
- Been, J.V.; Millett, C.; Lee, J.T.; van Schayck, C.P.; Sheikh, A. Smoke-free legislation and childhood hospitalisations for respiratory tract infections. Eur. Respir. J. 2015, 46, 697–706. [Google Scholar] [CrossRef]
- Been, J.V.; Szatkowski, L.; van Staa, T.-P.; Leufkens, H.G.; van Schayck, O.C.; Sheikh, A.; de Vries, F.; Souverein, P. Smoke-free legislation and the incidence of paediatric respiratory infections and wheezing/asthma: Interrupted time series analyses in the four UK nations. Sci. Rep. 2015, 5, 15246. [Google Scholar] [CrossRef] [PubMed]
- Been, J.V.; Mackay, D.F.; Millett, C.; Soyiri, I.; Van Schayck, C.P.; Pell, J.; Sheikh, A. Smoke-free legislation and paediatric hospitalisations for acute respiratory tract infections: National quasi-experimental study with unexpected findings and important methodological implications. Tob. Control. 2017, 27, e160–e166. [Google Scholar] [CrossRef]
- Turner, S.; Mackay, D.; Dick, S.; Semple, S.; Pell, J.P. Associations between a smoke-free homes intervention and childhood admissions to hospital in Scotland: An interrupted time-series analysis of whole-population data. Lancet Public Health 2020, 5, e493–e500. [Google Scholar] [CrossRef] [PubMed]
- Naiman, A.; Glazier, R.H.; Moineddin, R. Association of anti-smoking legislation with rates of hospital admission for cardiovascular and respiratory conditions. Can. Med. Assoc. J. 2010, 182, 761–767. [Google Scholar] [CrossRef]
- Ho, V.; Ross, J.; Steiner, C.A.; Mandawat, A.; Short, M.; Ku-Goto, M.-H.; Krumholz, H.M. A Nationwide Assessment of the Association of Smoking Bans and Cigarette Taxes With Hospitalizations for Acute Myocardial Infarction, Heart Failure, and Pneumonia. Med. Care Res. Rev. 2017, 74, 687–704. [Google Scholar] [CrossRef]
- Gambaryan, M.; Drapkina, O. The effectiveness of implementing tobacco control legislative measures in relation to the smoking prevalence in 10 constituent entities of the Russian Federation from 2013 to 2018. Russ. J. Prev. Med. 2021, 24, 44–51. [Google Scholar] [CrossRef]
- Federal State Statistics Service. The Results of Selective Observation of Behavioural Factors Affecting the Health of the Population in 2013 and 2018. Available online: https://www.gks.ru/free_doc/new_site/ZDOR/Factors2018_2812/index.html (accessed on 15 March 2023). (In Russian)
- Joossens, L. The Tobacco Control Scale: A new scale to measure country activity. Tob. Control. 2006, 15, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Gambaryan, M.; Drapkina, O. The Integrated scale for assessing the implementation of the Federal Tobacco Control Law in the Russian regions. Russ. J. Prev. Med. 2020, 23, 50–59. [Google Scholar] [CrossRef]
- Kontsevaya, A.V.; Agishina, T.A.; Gambaryan, M.G.; Duplyakov, D.V.; Drapkina, O.M. Impact of anti-tobacco policy measures on acute myocardial infarction and unstable angina hospitalization rates in three russian regions. Hum. Ecol. 2020, 27, 37–44. [Google Scholar] [CrossRef]
- Gambaryan, M.G.; Kontsevaya, A.V.; Agishina, T.A.; Drapkina, O.M. Assessing the effectiveness of legislative measures for tobacco control in relation to reducing in-hospital incidence of angina pectoris and myocardial infarction in the Russian Federation and its 10 constituent entities. Cardiovasc. Ther. Prev. 2021, 20, 2911. [Google Scholar] [CrossRef]
- Federal State Statistics Service. Regions of Russia. Socioeconomic Indicators. 2020. Available online: https://gks.ru/bgd/regl/b20_14p/Main.htm.https://gks.ru/bgd/regl/b20_14p/Main.htm (accessed on 15 March 2023). (In Russian)
- Federal State Statistics Service. Results of Selective Monitoring for the Health Status of the Population in 2019. Available online: https://gks.ru/free_doc/new_site/ZDOR/2019/PublishSite/index.html (accessed on 15 March 2023). (In Russian)
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, L.; Bennett, K.; Giampaoli, S.; Capewell, S. Explaining the Decrease in Coronary Heart Disease Mortality in Italy Between 1980 and 2000. Am. J. Public Health 2010, 100, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Baskaran, V.; Murray, R.; Hunter, A.; Lim, W.S.; McKeever, T.M. Effect of tobacco smoking on the risk of developing community acquired pneumonia: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0220204. [Google Scholar] [CrossRef] [PubMed]
| Federal Subjects of Russia | IRR * (95% CI) | p | Relative Change IRR (%) |
|---|---|---|---|
| The Russian Federation | 0.88 (0.79–0.97) | 0.011 | −14.3 |
| The Chuvash Republic | 0.75 (0.62–0.91) | 0.003 | −27.5 |
| Krasnodar Krai | 0.98 (0.8–1.2) | 0.863 | −4.0 |
| Primorskyi Krai | 1.01 (0.99–1.03) | 0.694 | 1.1 |
| Arkhangelsk Oblast | 0.88 (0.77–0.99) | 0.04 | −14.7 |
| Astrakhan Oblast | 0.88 (0.72–1.08) | 0.224 | −17.8 |
| Belgorod Oblast | 0.77 (0.6–0.98) | 0.033 | −27.4 |
| Novosibirsk Oblast | 0.96 (0.79–1.16) | 0.681 | −4.6 |
| Orenburg Oblast | 0.93 (0.76–1.14) | 0.512 | −10.4 |
| Samara Oblast | 0.72 (0.63–0.82) | 0.000 | −32.4 |
| Tyumen Oblast | 0.88 (0.67–1.2) | 0.353 | −13.2 |
| RTCL | rsp * (95% CI) | p |
|---|---|---|
| All MPOWER measures | −0.02 (−0.69; −0.66) | 0.958 |
| Tax/price measures | −0.11 (−0.62;0.86) | 0.764 |
| Smoking bans ** | 0.55 (−1.08; 0.02) | 0.042 |
| Information and communication measures | −0.127 (−0.84; 0.58) | 0.725 |
| Banning tobacco advertising, promotion, sponsorship | −0.004 (−0.745; 0.75) | 0.990 |
| Warning signs | 0.40 (−0.22; 1.03) | 0.208 |
| Smoking cessation support | −0.763 (−1.11; −0.41) | 0.000 |
| Prevalence of smoking | ||
| Smoking prevalence in 2019 | 0.7 (0.32; 1.08) | 0.000 |
| Changes in smoking prevalence 2013–2018 | −0.5 (−1.07; −0.07) | 0.085 |
| Reduction in Hospital Admission Rates (RR%) | Smoking Cessation Support | Prevalence of Smoking in 2019 |
|---|---|---|
| β * 95% CI | β 95% CI | |
| Pneumonia | −4.212 (−7.61; −0.82) ** | 2.40 (0.34; 4.45) |
| p | 0.020 | 0.027 |
| Asthma | −2.43 (−5.39; 0.53) | 1.2 (0.64; 3.04) |
| p | 0.096 | 0.174 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gambaryan, M.; Kontsevaya, A.; Drapkina, O. Impact of National Tobacco Control Policy on Rates of Hospital Admission for Pneumonia: When Compliance Matters. Int. J. Environ. Res. Public Health 2023, 20, 5893. https://doi.org/10.3390/ijerph20105893
Gambaryan M, Kontsevaya A, Drapkina O. Impact of National Tobacco Control Policy on Rates of Hospital Admission for Pneumonia: When Compliance Matters. International Journal of Environmental Research and Public Health. 2023; 20(10):5893. https://doi.org/10.3390/ijerph20105893
Chicago/Turabian StyleGambaryan, Marine, Anna Kontsevaya, and Oxana Drapkina. 2023. "Impact of National Tobacco Control Policy on Rates of Hospital Admission for Pneumonia: When Compliance Matters" International Journal of Environmental Research and Public Health 20, no. 10: 5893. https://doi.org/10.3390/ijerph20105893
APA StyleGambaryan, M., Kontsevaya, A., & Drapkina, O. (2023). Impact of National Tobacco Control Policy on Rates of Hospital Admission for Pneumonia: When Compliance Matters. International Journal of Environmental Research and Public Health, 20(10), 5893. https://doi.org/10.3390/ijerph20105893





