Loneliness before and after COVID-19: Sense of Coherence and Hope as Coping Mechanisms
Abstract
1. Introduction
2. Loneliness
2.1. Sense of Coherence (SOC)
2.2. Hope
2.3. The Current Study
3. Method
3.1. Procedure
3.2. Participants
3.3. Measures
3.4. Data Analysis
4. Results
4.1. Preliminary Analyses
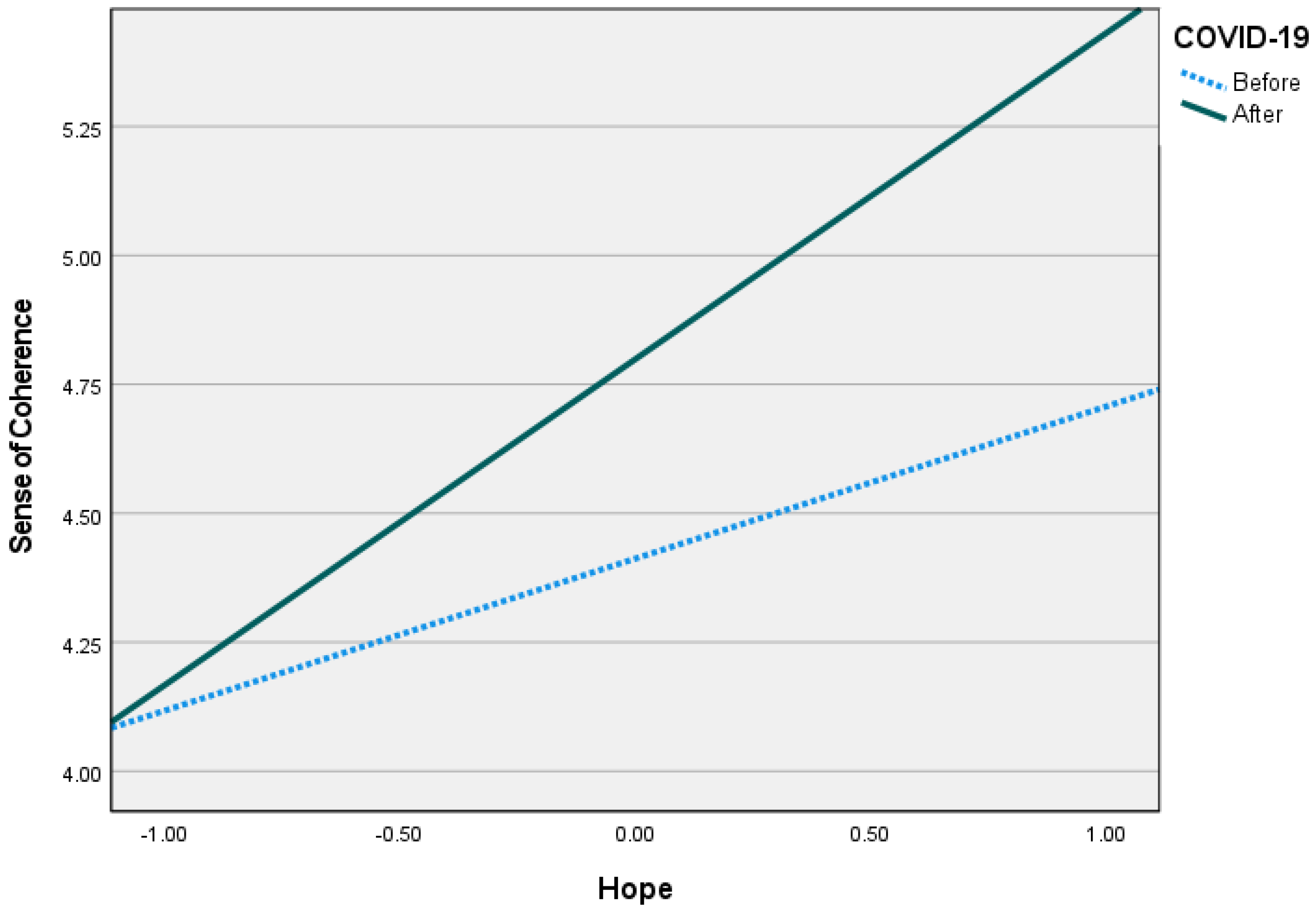
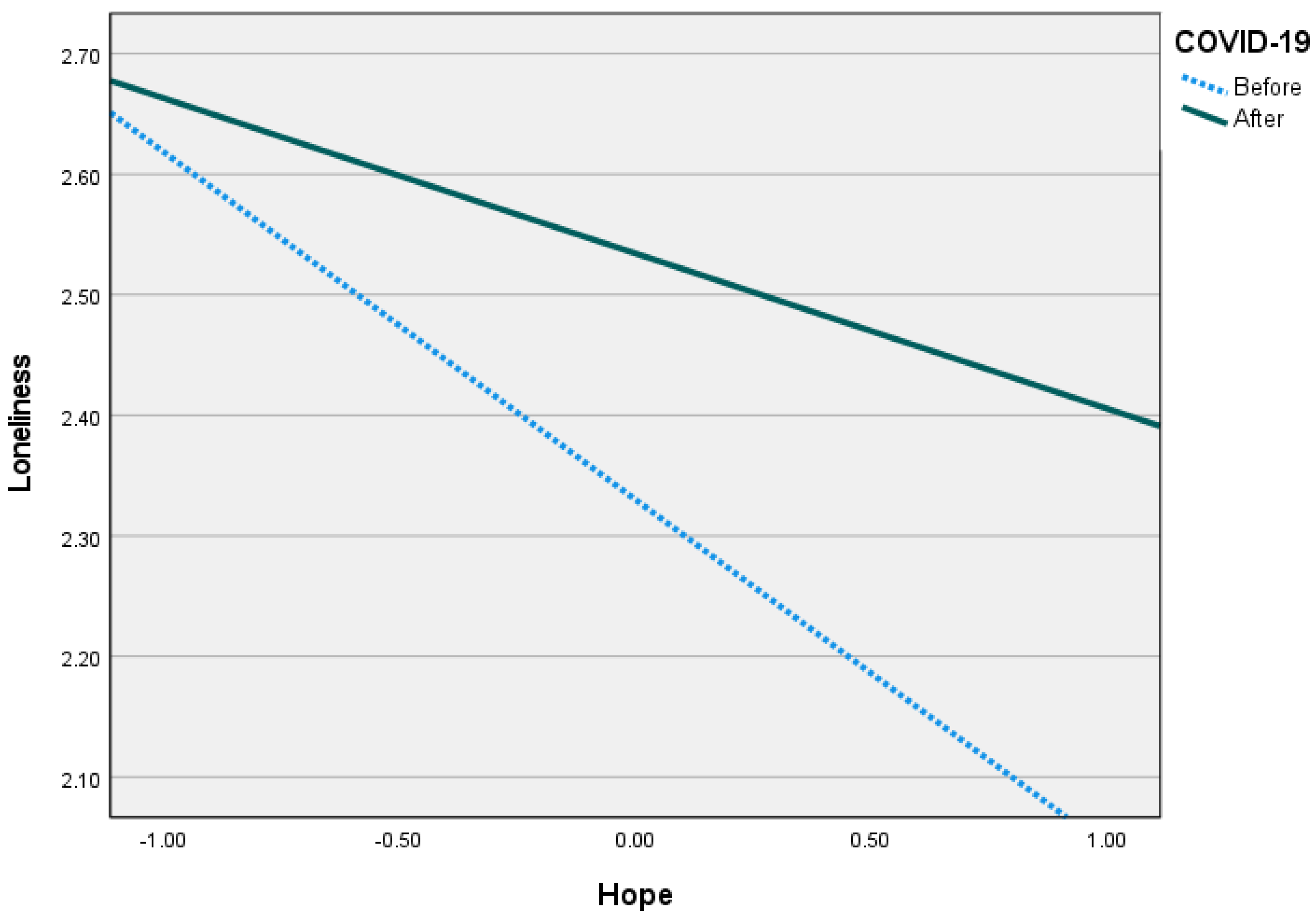
4.2. Moderated Mediation Analyses
5. Discussion
6. Limitations and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rana, I.A.; Bhatti, S.S.; Aslam, A.B.; Jamshed, A.; Ahmad, J.; Shah, A.A. COVID-19 risk perception and coping mechanisms: Does gender make a difference? Int. J. Disaster Risk Reduct. 2021, 55, 102096. [Google Scholar] [CrossRef]
- Kim, S.C.; Sloan, C.; Montejano, A.; Quiban, C. Impacts of coping mechanisms on nursing students’ mental health during COVID-19 lockdown: A cross-sectional survey. Nurs. Rep. 2021, 11, 36–44. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Usher, K.; Durkin, J.; Bhullar, N. The COVID-19 pandemic and mental health impacts. Int. J. Ment. Health Nurs. 2020, 29, 315–318. [Google Scholar] [CrossRef]
- Mancini, A.D. Heterogeneous mental health consequences of COVID-19: Costs and benefits. Psychol. Trauma 2020, 12, S15–S16. [Google Scholar] [CrossRef]
- Banks, J.; Fancourt, D.; Xu, X. Mental health and the COVID-19 pandemic. In World Happiness Report; New York: Sustainable Development Solutions Network; 2021; pp. 107–130. ISBN 978-1-7348080-1-8. [Google Scholar]
- Maresca, G.; Corallo, F.; Catanese, G.; Formica, C.; Lo Buono, V. Coping strategies of healthcare professionals with burnout syndrome: A systematic review. Medicina 2022, 58, 327. [Google Scholar] [CrossRef] [PubMed]
- Freire, C.; Ferradás, M.D.M.; Regueiro, B.; Rodríguez, S.; Valle, A.; Núñez, J.C. Coping strategies and self-efficacy in university students: A person-centered approach. Front. Psychol. 2020, 11, 841. [Google Scholar] [CrossRef] [PubMed]
- Martínez, J.P.; Méndez, I.; Ruiz-Esteban, C.; Fernández-Sogorb, A.; García-Fernández, J.M. Profiles of burnout, coping strategies and depressive symptomatology. Front. Psychol. 2020, 11, 591. [Google Scholar] [CrossRef]
- Peplau, L.A.; Perlman, D. Loneliness: A Sourcebook of Current Theory, Research and Therapy; Wiley: New York, NY, USA, 1982. [Google Scholar]
- Park, M.; Cook, A.R.; Lim, J.T.; Sun, Y.; Dickens, B.L. A systematic review of COVID-19 epidemiology based on current evidence. J. Clin. Med. 2020, 9, 967. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, D.; Rai, M. Social isolation in COVID-19: The impact of loneliness. Int. J. Soc. Psychiatry. 2020, 66, 525–527. [Google Scholar] [CrossRef] [PubMed]
- Buecker, S.; Horstmann, K.T. Loneliness and social isolation during the COVID-19 pandemic. Eur. Psychol. 2022, 26, 251–397. [Google Scholar] [CrossRef]
- Li, L.Z.; Wang, S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020, 291, 113267. [Google Scholar] [CrossRef]
- Luchetti, M.; Lee, J.H.; Aschwanden, D.; Sesker, A.; Strickhouser, J.E.; Terracciano, A.; Sutin, A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020, 75, 897–908. [Google Scholar] [CrossRef] [PubMed]
- Stefana, A.; Youngstrom, E.A.; Hopwood, C.J.; Dakanalis, A. The COVID-19 pandemic brings a second wave of social isolation and disrupted services. Eur. Arch. Psychiatry Clin. Neurosci. 2020, 270, 785–786. [Google Scholar] [CrossRef] [PubMed]
- Bu, F.; Steptoe, A.; Fancourt, D. Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc. Sci. Med. 2020, 265, 113521. [Google Scholar] [CrossRef]
- Pan, Y.; Yang, Z.; Han, X.; Qi, S. Family functioning and mental health among secondary vocational students during the COVID-19 epidemic: A moderated mediation model. Pers Individ Dif. 2021, 171, 110490. [Google Scholar] [CrossRef]
- De Lange, A.M.G.; Kaufmann, T.; Quintana, D.S.; Winterton, A.; Westlye, L.T.; Ebmeier, K.P. Risk factors associated with loneliness, social isolation, and neuroticism in the UK Biobank cohort. PsyArXiv 2020. [Google Scholar]
- Antonovsky, A. Unraveling the Mystery of Health: How People Manage Stress and Stay Well; Jossey-Bass Publishers: San Francisco, CA, USA, 1987; Volume 175. [Google Scholar]
- Mittelmark, M.B.; Bauer, G.F.; Vaandrager, L.; Pelikan, J.M.; Sagy, S.; Eriksson, M.; Lindstrrom, B.; Magistretti, C.M. The Handbook of Salutogenesis, 2nd ed.; Springer Nature: Berlin/Heidelberg, Germany, 2022. [Google Scholar]
- Mana, A.; Bauer, G.F.; Meier Magistretti, C.; Sardu, C.; Juvinyà-Canal, D.; Hardy, L.J.; Catz, O.; Tušl, M.; Sagy, S. Order out of chaos: Sense of coherence and the mediating role of coping resources in explaining mental health during COVID-19 in 7 countries. SSM Mental Health 2021, 1, 100001. [Google Scholar] [CrossRef]
- Langeland, E.; Vinje, F. Applying Salutogenesis in mental healthcare settings. In The Handbook of Salutogenesis, 2nd ed.; Springer Nature: Berlin/Heidelberg, Germany, 2022; pp. 433–439. [Google Scholar]
- Dooris, M.; Doherty, S.; Orme, J. Applying Salutogenesis in higher education. In The Handbook of Salutogenesis, 2nd ed.; Springer Nature: Berlin/Heidelberg, Germany, 2022; pp. 307–319. [Google Scholar]
- Jenny, G.J.; Bauer, G.F.; Vinje, H.F.; Brauchli, R.; Vogt, K.; Torp, S. Applying Salutogenesis in the workplace. In The Handbook of Salutogenesis, 2nd ed.; Springer Nature: Berlin/Heidelberg, Germany, 2022; pp. 321–336. [Google Scholar]
- Gómez-Salgado, J.; Domínguez-Salas, S.; Romero-Martín, M.; Ortega-Moreno, M.; García-Iglesias, J.J.; Ruiz-Frutos, C. Sense of coherence and psychological distress among healthcare workers during the COVID-19 pandemic in Spain. Sustainability 2020, 12, 6855. [Google Scholar] [CrossRef]
- Schmuck, J.; Hiebel, N.; Rabe, M.; Schneider, J.; Erim, Y.; Morawa, E.; Jerg-Bretzke, L.; Beschoner, P.; Albus, C.; Hannemann, J.; et al. Sense of coherence, social support and religiosity as resources for medical personnel during the COVID-19 pandemic: A web-based survey among 4324 health care workers within the German Network University Medicine. PLoS ONE 2021, 16, e0255211. [Google Scholar] [CrossRef]
- Navarro Prados, A.B.; Jiménez García-Tizón, S.; Meléndez, J.C. Sense of coherence and burnout in nursing home workers during the COVID-19 pandemic in Spain. Health Soc. Care Community 2022, 30, 244–252. [Google Scholar] [CrossRef]
- Barni, D.; Danioni, F.; Canzi, E.; Ferrari, L.; Ranieri, S.; Lanz, M.; Iafrate, R.; Regalia, C.; Rosnati, R. Facing the COVID-19 pandemic: The role of sense of coherence. Front. Psychol. 2020, 11, 578440. [Google Scholar] [CrossRef] [PubMed]
- Dadaczynski, K.; Okan, O.; Messer, M.; Rathmann, K. University students’ sense of coherence, future worries and mental health: Findings from the German COVID-HL-survey. Health Promot. Int. 2022, 37, daab070. [Google Scholar] [CrossRef] [PubMed]
- Snyder, C.R. Hope theory: Rainbows in the mind. Psychol. Inq. 2002, 13, 249–275. [Google Scholar] [CrossRef]
- Margalit, M.; Schmidt-Barad, T.; Einav, M. Individual and interpersonal aspects of hope and people with developmental disabilities. In The Positive Psychology of Personal Factors: Implications for Understanding Disability; Lexington Books: New York, NY, USA, 2022; Volume 107. [Google Scholar]
- Gallagher, M.W.; Lopez, S.J. The Oxford Handbook of Hope; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Einav, M.; Margalit, M. The hope theory and specific learning disorders and/or attention deficit disorders (SLD/ADHD): Developmental perspectives. Curr. Opin. Psychol. 2022, 48, 101471. [Google Scholar] [CrossRef] [PubMed]
- Trzebiński, J.; Cabański, M.; Czarnecka, J.Z. Reaction to the COVID-19 pandemic: The influence of meaning in life, life satisfaction, and assumptions on world orderliness and positivity. J. Loss Trauma 2020, 25, 544–557. [Google Scholar] [CrossRef]
- Walsh, F. Loss and resilience in the time of COVID-19: Meaning making, hope, and transcendence. Fam. Process 2020, 59, 898–911. [Google Scholar] [CrossRef]
- Yao, Y.; Lin, M.; Ni, J.; Ni, J. Hope Buffers the Effect of Fear of COVID-19 on Depression among College Students: Insomnia as a Mediator. Int. J. Environ. Res. Public Health 2023, 20, 3245. [Google Scholar] [CrossRef]
- Geiger, K.A.; Kwon, P. Rumination and depressive symptoms: Evidence for the moderating role of hope. Personal. Individ. Differ. 2010, 49, 391–395. [Google Scholar] [CrossRef]
- Karababa, A. The Moderating Role of Hope in the Relationship Between Maladaptive Perfectionism and Anxiety Among Early Adolescents. J. Genet. Psychol. 2020, 181, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Zhao, L.; Han, X.; Wu, S.; Liu, X. Moderating role of hope in the relationship between perceived discrimination and life satisfaction among left-behind children in China. Soc. Behav. Personal. 2020, 48, 1–8. [Google Scholar] [CrossRef]
- Yıldırım, M.; Arslan, G. Exploring the associations between resilience, dispositional hope, preventive behaviors, subjective well-being, and psychological health among adults during early stage of COVID-19. Curr. Psychol. 2022, 41, 5712–5722. [Google Scholar] [CrossRef] [PubMed]
- Laslo-Roth, R.; George-Levi, S.; Margalit, M. Hope during the COVID-19 outbreak: Coping with the psychological impact of quarantine. Couns. Psychol. Q. 2021, 34, 771–785. [Google Scholar] [CrossRef]
- Iecovich, E. Psychometric properties of the Hebrew version of the de Jong Gierveld loneliness scale. Educ. Gerontol. 2013, 39, 12–27. [Google Scholar] [CrossRef]
- De Jong Gierveld, J.; van Tilburg, T. A 6-item scale for overall, emotional and social loneliness confirmatory tests on survey data. Res. Aging 2006, 28, 582–598. Available online: http://roa.sagepub.com/cgi/reprint/28/5/582 (accessed on 27 March 2023). [CrossRef]
- Lackaye, T.; Margalit, M. Comparisons of achievement, effort and self-perceptions among students with learning disabilities and their peers from different achievement groups. J. Learn. Disabil. 2006, 39, 432–446. [Google Scholar] [CrossRef]
- Hayes, J.R. The Complete Problem Solver; Routledge: London, UK, 2013. [Google Scholar]
- Hayes, A.F. Partial, conditional, and moderated mediation: Quantification, inference, and interpretation. Commun. Monogr. 2018, 85, 4–40. [Google Scholar] [CrossRef]
- Hayes, A.F. An index and test of linear moderated mediation. Multivariate Behav. Res. 2015, 50, 1–22. [Google Scholar] [CrossRef]
- Winger, J.G.; Adams, R.N.; Mosher, C.E. Relations of meaning in life and sense of coherence to distress in cancer patients: A meta-analysis. Psycho-Oncology 2016, 25, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Sales, A.; Pinazo-Hernandis, S.; Martinez, D. Effects of a reminiscence program on meaning of life, sense of coherence and coping in older women living in nursing homes during COVID-19. Healthcare 2022, 10, 188. [Google Scholar] [CrossRef]
- Wang, X.; Sun, Y.; Kramer, T. Ritualistic consumption decreases loneliness by increasing meaning. J. Mark Res. 2021, 58, 282–298. [Google Scholar] [CrossRef]
- Tomšik, R. Relationship of loneliness and meaning of life among adolescents. In Proceedings of the Current Trends in Educational Science and Practice VIII: International Proceedings of Scientific Studies, Nitra, Slovakia, June 2015; pp. 66–79. [Google Scholar]
- Burles, M.; Bally, J.M.; Holtslander, L.; Zimmer, M.; Hodgson-Viden, H. Supporting parental caregivers of seriously ill children: Findings from a feasibility and acceptability study of a hope intervention. Child Health Care 2022, 51, 1–19. [Google Scholar] [CrossRef]
- Chan, K.; Wong, F.K.; Lee, P.H. A brief hope intervention to increase hope level and improve well-being in rehabilitating cancer patients: A feasibility test. SAGE Open Nurs. 2019, 5, 2377960819844381. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Einav, M.; Margalit, M. Loneliness before and after COVID-19: Sense of Coherence and Hope as Coping Mechanisms. Int. J. Environ. Res. Public Health 2023, 20, 5840. https://doi.org/10.3390/ijerph20105840
Einav M, Margalit M. Loneliness before and after COVID-19: Sense of Coherence and Hope as Coping Mechanisms. International Journal of Environmental Research and Public Health. 2023; 20(10):5840. https://doi.org/10.3390/ijerph20105840
Chicago/Turabian StyleEinav, Michal, and Malka Margalit. 2023. "Loneliness before and after COVID-19: Sense of Coherence and Hope as Coping Mechanisms" International Journal of Environmental Research and Public Health 20, no. 10: 5840. https://doi.org/10.3390/ijerph20105840
APA StyleEinav, M., & Margalit, M. (2023). Loneliness before and after COVID-19: Sense of Coherence and Hope as Coping Mechanisms. International Journal of Environmental Research and Public Health, 20(10), 5840. https://doi.org/10.3390/ijerph20105840





