Association between Initial Opioid Prescription and Patient Pain with Continued Opioid Use among Opioid-Naïve Patients Undergoing Elective Surgery in a Large American Health System
Abstract
1. Introduction
2. Materials and Methods
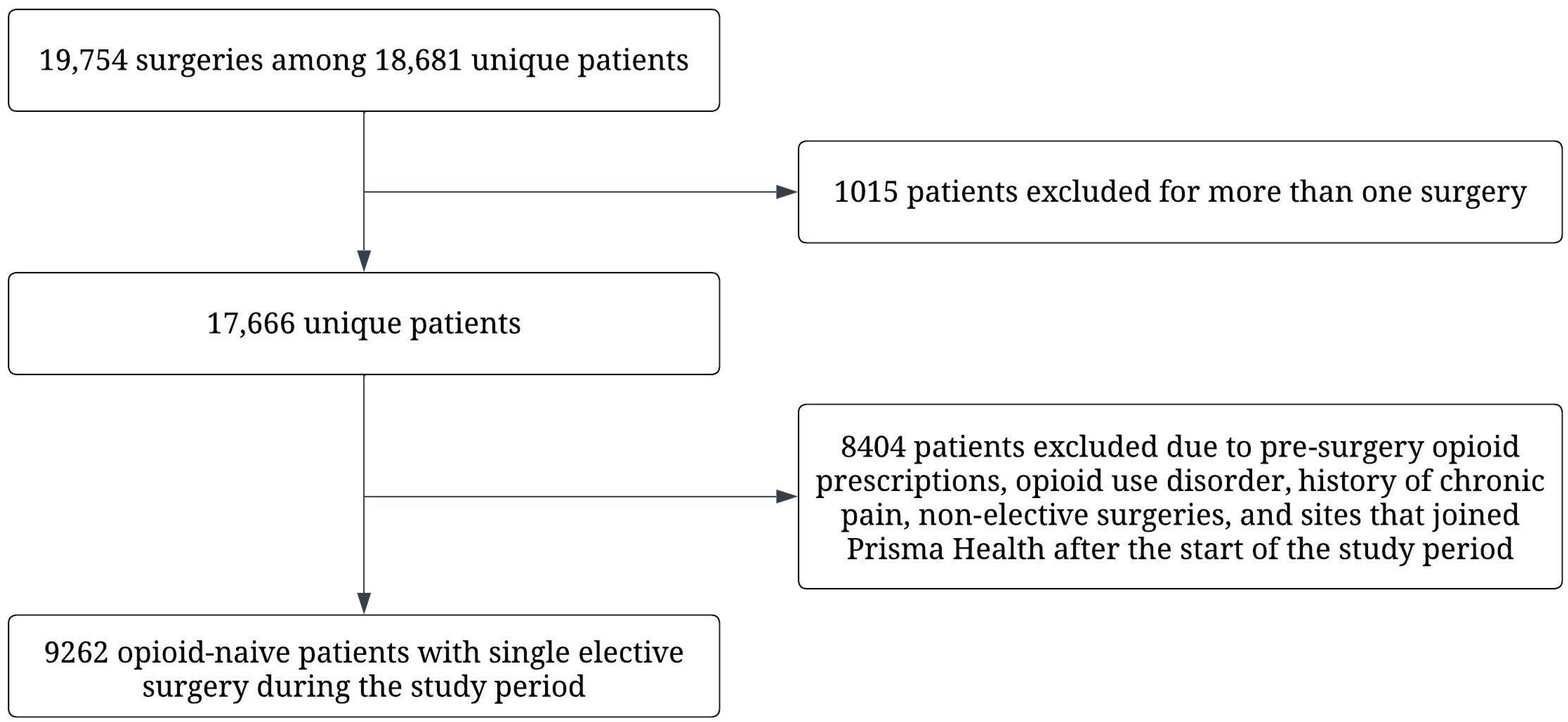
2.1. Data Source and Patient Cohort
2.2. Characteristics of the First Opioid Prescription and Need for Pain Management
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Manchikanti, L.; Singh, A. Therapeutic opioids: A ten-year perspective on the complexities and complications of the escalating use, abuse, and nonmedical use of opioids. Pain Physician 2008, 11, S63–S88. [Google Scholar] [CrossRef] [PubMed]
- Urman, R.D.; Seger, D.L.; Fiskio, J.M.; Neville, B.A.; Harry, E.M.; Weiner, S.G.; Lovelace, B.; Fain, R.; Cirillo, J.; Schnipper, J.L. The Burden of Opioid-Related Adverse Drug Events on Hospitalized Previously Opioid-Free Surgical Patients. J. Patient Saf. 2021, 17, e76–e83. [Google Scholar] [CrossRef] [PubMed]
- Larach, D.B.; Waljee, J.F.; Hu, H.M.; Lee, J.S.; Nalliah, R.; Englesbe, M.J.; Brummett, C.M. Patterns of Initial Opioid Prescribing to Opioid-Naive Patients. Ann. Surg. 2020, 271, 290–295. [Google Scholar] [CrossRef] [PubMed]
- Rennert, L.; Howard, K.A.; Walker, K.B.; Furmanek, D.L.; Blackhurst, D.W.; Cancellaro, V.A.; Litwin, A.H. Evaluation of policies limiting opioid exposure on opioid prescribing and patient pain in opioid-naive patients undergoing elective surgery in a large American health system. J. Patient Saf. 2023, 19, 71–78. [Google Scholar] [CrossRef]
- Serrell, E.C.; Greenberg, C.C.; Borza, T. Surgeons and perioperative opioid prescribing: An underappreciated contributor to the opioid epidemic. Cancer 2021, 127, 184–187. [Google Scholar] [CrossRef]
- Brummett, C.M.; Waljee, J.F.; Goesling, J.; Moser, S.; Lin, P.; Englesbe, M.J.; Bohnert, A.S.; Kheterpal, S.; Nallamothu, B.K. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017, 152, e170504. [Google Scholar] [CrossRef]
- Shah, A.; Hayes, C.J.; Martin, B.C. Factors Influencing Long-Term Opioid Use Among Opioid Naive Patients: An Examination of Initial Prescription Characteristics and Pain Etiologies. J. Pain 2017, 18, 1374–1383. [Google Scholar] [CrossRef]
- Kolodny, A.; Frieden, T.R. Ten Steps the Federal Government Should Take Now to Reverse the Opioid Addiction Epidemic. JAMA 2017, 318, 1537. [Google Scholar] [CrossRef]
- Babu, K.M.; Brent, J.; Juurlink, D.N. Prevention of Opioid Overdose. N. Engl. J. Med. 2019, 380, 2246–2255. [Google Scholar] [CrossRef]
- Dunn, K.M. Opioid Prescriptions for Chronic Pain and Overdose: A Cohort Study. Ann. Intern. Med. 2010, 152, 85. [Google Scholar] [CrossRef]
- Adewumi, A.D.; Hollingworth, S.A.; Maravilla, J.C.; Connor, J.P.; Alati, R. Prescribed Dose of Opioids and Overdose: A Systematic Review and Meta-Analysis of Unintentional Prescription Opioid Overdose. CNS Drugs 2018, 32, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Cheatle, M.D.; Compton, P.A.; Dhingra, L.; Wasser, T.E.; O’Brien, C.P. Development of the Revised Opioid Risk Tool to Predict Opioid Use Disorder in Patients with Chronic Nonmalignant Pain. J. Pain 2019, 20, 842–851. [Google Scholar] [CrossRef]
- Webster, L.R. Risk Factors for Opioid-Use Disorder and Overdose . Anesth. Analg. 2017, 125, 1741–1748. [Google Scholar] [CrossRef] [PubMed]
- Cauley, C.E.; Anderson, G.; Haynes, A.B.; Menendez, M.; Bateman, B.T.; Ladha, K. Predictors of In-hospital Post-operative Opioid Overdose After Major Elective Operations: A Nationally Representative Cohort Study. Ann. Surg. 2017, 265, 702–708. [Google Scholar] [CrossRef]
- Lawal, O.D.; Gold, J.; Murthy, A.; Ruchi, R.; Bavry, E.; Hume, A.L.; Lewkowitz, A.K.; Brothers, T.; Wen, X. Rate and Risk Factors Associated With Prolonged Opioid Use After Surgery: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e207367. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, K.M.; Hellman, D. Opioid Prescribing and the Ethical Duty to Do No Harm. Am. J. Law Med. 2020, 46, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Dowell, D.; Ragan, K.R.; Jones, C.M.; Baldwin, G.T.; Chou, R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain—United States, 2022. MMWR Recomm. Rep. 2022, 71, 1–95. [Google Scholar] [CrossRef]
- Brat, G.A.; Agniel, D.; Beam, A.; Yorkgitis, B.; Bicket, M.; Homer, M.; Fox, K.P.; Knecht, D.B.; McMahill-Walraven, C.N.; Palmer, N.; et al. Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: Retrospective cohort study. BMJ 2018, 360, j5790. [Google Scholar] [CrossRef]
- Shah, A.; Hayes, C.J.; Martin, B.C. Characteristics of Initial Prescription Episodes and Likelihood of Long-Term Opioid Use—United States, 2006–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 265–269. [Google Scholar] [CrossRef]
- Guy, G.P., Jr.; Zhang, K.; Bohm, M.K.; Losby, J.; Lewis, B.; Young, R.; Murphy, L.B.; Dowell, D. Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 697–704. [Google Scholar] [CrossRef]
- Dowell, D.; Haegerich, T.M.; Chou, R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA 2016, 315, 1624–1645. [Google Scholar] [CrossRef] [PubMed]
- Sekhri, S.; Arora, S.; Cottrell, H.; Baerg, T.; Duncan, A.; Hu, H.M.; Englesbe, M.J.; Brummett, C.; Waljee, J. Probability of Opioid Prescription Refilling After Surgery: Does Initial Prescription Dose Matter? Ann. Surg. 2018, 268, 271–276. [Google Scholar] [CrossRef]
- Massie, L.; Gunaseelan, V.; Waljee, J.; Brummett, C.; Schwalb, J.M. Relationship between initial opioid prescription size and likelihood of refill after spine surgery. Spine J. 2021, 21, 772–778. [Google Scholar] [CrossRef] [PubMed]
- Scully, R.E.; Schoenfeld, A.J.; Jiang, W.; Lipsitz, S.; Chaudhary, M.A.; Learn, P.A.; Koehlmoos, T.; Haider, A.H.; Nguyen, L.L. Defining Optimal Length of Opioid Pain Medication Prescription After Common Surgical Procedures. JAMA Surg. 2018, 153, 37. [Google Scholar] [CrossRef] [PubMed]
- Alam, A. Long-term Analgesic Use After Low-Risk Surgery: A Retrospective Cohort Study. Arch. Intern. Med. 2012, 172, 425. [Google Scholar] [CrossRef] [PubMed]
- Lanzillotta-Rangeley, J.; Clark, A.; Christianson, A.; Kalarchian, M.A. Association of Prescription Opioid Exposure and Patient Factors With Prolonged Post-operative Opioid Use in Opioid-Naïve Patients. AANA J. 2020, 88, 18–26. [Google Scholar]
- Carroll, J.J.; Marshall, B.D.L.; Rich, J.D.; Green, T.C. Exposure to fentanyl-contaminated heroin and overdose risk among illicit opioid users in Rhode Island: A mixed methods study. Int. J. Drug Policy 2017, 46, 136–145. [Google Scholar] [CrossRef]
- Hoppe, J.A.; Kim, H.; Heard, K. Association of Emergency Department Opioid Initiation With Recurrent Opioid Use. Ann. Emerg. Med. 2015, 65, 493–499. [Google Scholar] [CrossRef]
- Agniel, D.; Brat, G.A.; Marwaha, J.S.; Fox, K.; Knecht, D.; Paz, H.L.; Bicket, M.C.; Yorkgitis, B.; Palmer, N.; Kohane, I. Association of Postsurgical Opioid Refills for Patients With Risk of Opioid Misuse and Chronic Opioid Use Among Family Members. JAMA Netw. Open 2022, 5, e2221316. [Google Scholar] [CrossRef]
- Jones, M.R.; Viswanath, O.; Peck, J.; Kaye, A.D.; Gill, J.S.; Simopoulos, T.T. A Brief History of the Opioid Epidemic and Strategies for Pain Medicine. Pain Ther. 2018, 7, 13–21. [Google Scholar] [CrossRef]
- Bicket, M.C.; Long, J.J.; Pronovost, P.J.; Alexander, G.C.; Wu, C.L. Prescription Opioid Analgesics Commonly Unused After Surgery: A Systematic Review. JAMA Surg. 2017, 152, 1066. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Overall 9262 | 0 MME 2043 (22.1%) | 0 < MME ≤ 90 1409 (15.2%) | MME >90 5810 (62.7%) | p-Value | |
|---|---|---|---|---|---|---|
| Age, Mean (SD) | 51.62 (16.34) | 54.41 (16.48) | 53.05 (16.84) | 50.30 (16.02) | <0.001 | |
| Sex, n (%) | Male | 3194 (34.5) | 694 (34.0) | 544 (38.6) | 1956 (33.7) | 0.002 |
| Female | 6068 (65.5) | 1349 (66.0) | 865 (61.4) | 3854 (66.3) | ||
| Race/Ethnicity, n (%) | Hispanic | 470 (5.1) | 96 (4.7) | 62 (4.5) | 312 (5.4) | 0.041 |
| Non-Hispanic White | 7239 (78.8) | 1641 (81.1) | 1105 (79.7) | 4493 (77.8) | ||
| Non-Hispanic Black | 1315 (14.3) | 257 (12.7) | 190 (13.7) | 868 (15.0) | ||
| Other | 159 (1.7) | 30 (1.5) | 30 (2.2) | 99 (1.7) | ||
| Elective Surgeries (CPT Type), n (%) | Bariatric Surgery | 31 (0.3) | 22 (1.1) | 0 (0.0) | 9 (0.2) | <0.001 |
| Carpal Tunnel Release | 797 (8.6) | 383 (18.7) | 185 (13.1) | 229 (3.9) | ||
| Colectomy | 568 (6.1) | 39 (1.9) | 54 (3.8) | 475 (8.2) | ||
| Hemorrhoidectomy | 380 (4.1) | 51 (2.5) | 13 (0.9) | 316 (5.4) | ||
| Hysterectomy | 1416 (15.3) | 363 (17.8) | 108 (7.7) | 945 (16.3) | ||
| Laparoscopic Appendectomy | 561 (6.1) | 79 (3.9) | 73 (5.2) | 409 (7.0) | ||
| Laparoscopic Cholecystectomy | 2359 (25.5) | 452 (22.1) | 348 (24.7) | 1559 (26.8) | ||
| Parathyroidectomy | 330 (3.6) | 36 (1.8) | 39 (2.8) | 255 (4.4) | ||
| Reflux Surgery | 51 (0.6) | 7 (0.3) | 14 (1.0) | 30 (0.5) | ||
| Thyroidectomy | 795 (8.6) | 203 (9.9) | 138 (9.8) | 454 (7.8) | ||
| Transurethral Prostate Surgery | 319 (3.4) | 143 (7.0) | 53 (3.8) | 123 (2.1) | ||
| Ventral Hernia Repair | 1655 (17.9) | 265 (13.0) | 384 (27.3) | 1006 (17.3) | ||
| Tobacco Smoking, n (%) | Current Smoker | 1295 (14.0) | 240 (11.7) | 184 (13.1) | 871 (15.0) | <0.001 |
| Former Smoker | 2417 (26.1) | 562 (27.5) | 390 (27.7) | 1465 (25.2) | ||
| Never Smoked | 5526 (59.7) | 1237 (60.5) | 833 (59.1) | 3456 (59.5) | ||
| Unknown | 24 (0.3) | 4 (0.2) | 2 (0.1) | 18 (0.3) | ||
| Tobacco Vaping, n (%) | Current User | 212 (2.3) | 32 (1.6) | 40 (2.8) | 140 (2.4) | <0.001 |
| Former User | 218 (2.4) | 46 (2.3) | 41 (2.9) | 131 (2.3) | ||
| Never Used | 7661 (82.8) | 1661 (81.3) | 1279 (90.8) | 4721 (81.3) | ||
| Unknown | 1167 (12.6) | 304 (14.9) | 49 (3.5) | 814 (14.0) | ||
| Mental Disorder, n (%) | Yes | 3260 (35.2) | 655 (32.1) | 513 (36.4) | 2092 (36.0) | 0.003 |
| No | 6002 (64.8) | 1388 (67.9) | 896 (63.6) | 3718 (64.0) | ||
| Pre-operative Pain, n (%) | None/Mild | 6547 (70.7) | 1411 (69.1) | 1188 (84.3) | 3948 (68.0) | <0.001 |
| Moderate/Severe | 2044 (23.8) | 400 (22.1) | 187 (13.6) | 1457 (27.0) | ||
| Post-operative Pain, n (%) | None/Mild | 6231 (67.3) | 1353 (66.2) | 1164 (82.6) | 3714 (63.9) | <0.001 |
| Moderate/Severe | 2333(27.2) | 457 (25.2) | 211 (15.3) | 1665 (31.0) | ||
| Discharge Pain, n (%) | None/Mild | 6346 (68.5) | 1501 (73.5) | 1060 (75.2) | 3785 (65.1) | <0.001 |
| Moderate/Severe | 2916 (31.5) | 542 (26.5) | 349 (24.8) | 2025 (34.9) | ||
| MME in First Prescription, Mean (SD) | 149.86 (155.60) | 0.00 (0.00) | 61.67 (14.84) | 223.95 (152.56) | <0.001 | |
| Any Refill, n (%) | Yes | 1209 (13.1) | -- | 149 (10.6) | 1059 (18.2) | <0.001 |
| No | 8053 (86.9) | -- | 1260 (89.4) | 4751 (81.8) | ||
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
| Predictors | Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value |
| MME > 90 (reference: MME ≤ 90) | 1.79 (1.52–2.14) | <0.001 | 1.57 (1.30–1.90) | <0.001 |
| Moderate/Severe Pre-operative Pain (reference: None/Mild) | 1.88 (1.64–2.16) | <0.001 | 1.34 (1.10–1.62) | 0.003 |
| Moderate/Severe Post-operative Pain (reference: None/Mild) | 1.90 (1.66–2.16) | <0.001 | 1.18 (0.97–1.43) | 0.101 |
| Moderate/Severe Discharge Pain (reference: None/Mild) | 1.76 (1.55–2.00) | <0.001 | 1.35 (1.16–1.57) | <0.001 |
| Any Pain (reference: No) | 1.90 (1.67–2.96) | <0.001 | 1.66 (1.45–191) | <0.001 |
| Predictors | Odds Ratio (95% CI) | p-Value | |
|---|---|---|---|
| Age | 1.00 (1.00–1.01) | 0.951 | |
| Race/Ethnicity (reference: Non-Hispanic White) | Hispanic | 1.00 (0.43–2.37) | 0.916 |
| Non-Hispanic Black | 1.30 (1.07–1.54) | 0.006 | |
| Non-Hispanic Other | 1.43 (0.86–2.28) | 0.151 | |
| Sex (reference: Male) | Female | 1.15 (0.97–1.35) | 0.102 |
| Tobacco Smoking (reference: Never Smoked) | Current Smoker | 1.80 (1.51–2.15) | <0.001 |
| Former Smoker | 1.19 (1.01–1.40) | 0.034 | |
| Unknown | 1.53 (0.34–5.03) | 0.521 | |
| Tobacco Vaping (reference: Never Used) | Current User | 1.00 (0.67–1.54) | 0.988 |
| Former User | 1.32 (0.72–2.35) | 0.342 | |
| Unknown | 1.05 (0.67–1.69) | 0.828 | |
| Psychological Disorder (reference: No) | Yes | 1.40 (1.22–1.61) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Babatunde, A.; Rennert, L.; Walker, K.B.; Furmanek, D.L.; Blackhurst, D.W.; Cancellaro, V.A.; Litwin, A.H.; Howard, K.A. Association between Initial Opioid Prescription and Patient Pain with Continued Opioid Use among Opioid-Naïve Patients Undergoing Elective Surgery in a Large American Health System. Int. J. Environ. Res. Public Health 2023, 20, 5766. https://doi.org/10.3390/ijerph20105766
Babatunde A, Rennert L, Walker KB, Furmanek DL, Blackhurst DW, Cancellaro VA, Litwin AH, Howard KA. Association between Initial Opioid Prescription and Patient Pain with Continued Opioid Use among Opioid-Naïve Patients Undergoing Elective Surgery in a Large American Health System. International Journal of Environmental Research and Public Health. 2023; 20(10):5766. https://doi.org/10.3390/ijerph20105766
Chicago/Turabian StyleBabatunde, Abass, Lior Rennert, Kevin B. Walker, Douglas L. Furmanek, Dawn W. Blackhurst, Vito A. Cancellaro, Alain H. Litwin, and Kerry A. Howard. 2023. "Association between Initial Opioid Prescription and Patient Pain with Continued Opioid Use among Opioid-Naïve Patients Undergoing Elective Surgery in a Large American Health System" International Journal of Environmental Research and Public Health 20, no. 10: 5766. https://doi.org/10.3390/ijerph20105766
APA StyleBabatunde, A., Rennert, L., Walker, K. B., Furmanek, D. L., Blackhurst, D. W., Cancellaro, V. A., Litwin, A. H., & Howard, K. A. (2023). Association between Initial Opioid Prescription and Patient Pain with Continued Opioid Use among Opioid-Naïve Patients Undergoing Elective Surgery in a Large American Health System. International Journal of Environmental Research and Public Health, 20(10), 5766. https://doi.org/10.3390/ijerph20105766






