Characteristics and Effectiveness of Co-Designed Mental Health Interventions in Primary Care for People Experiencing Homelessness: A Systematic Review
Abstract
1. Introduction
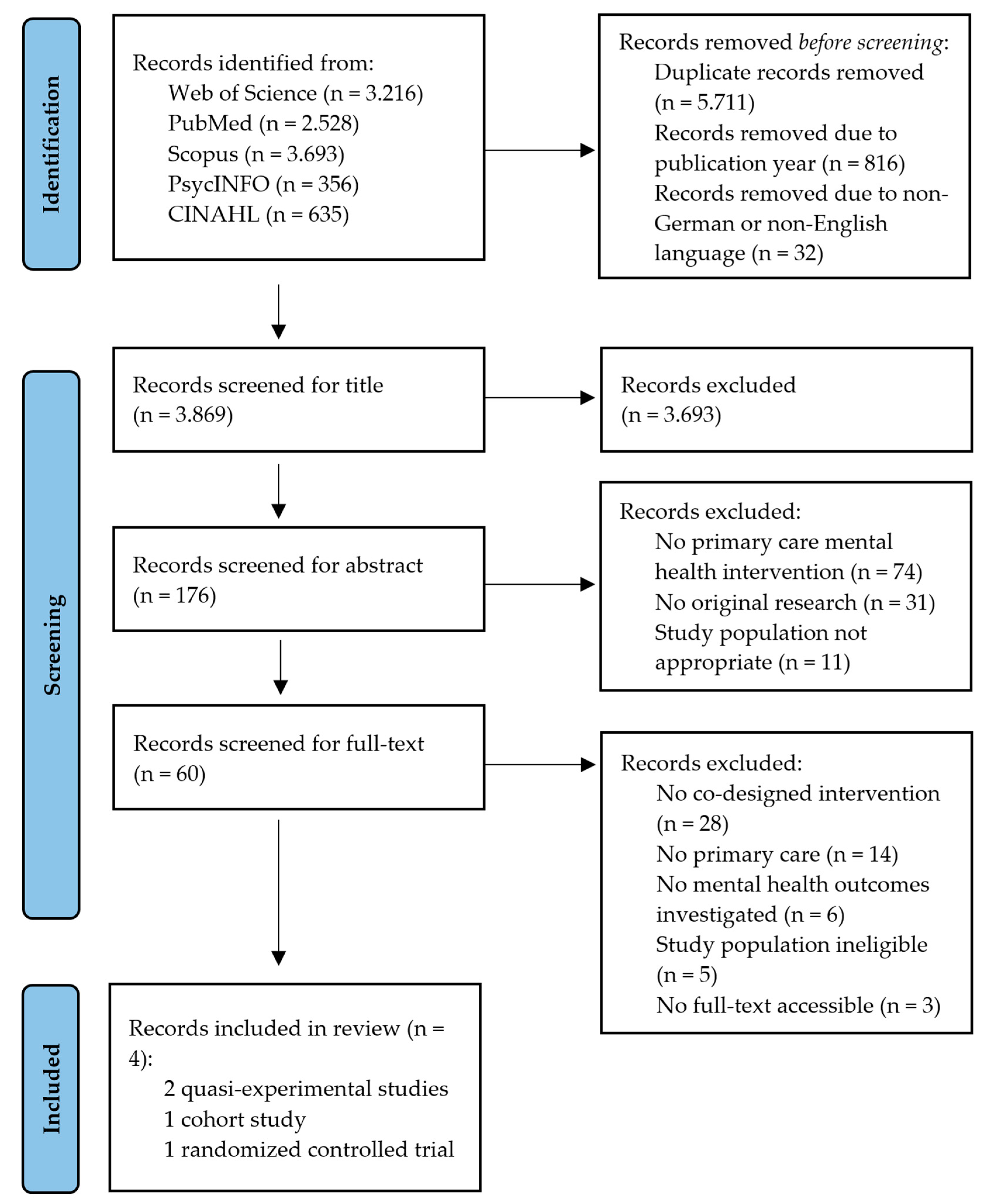
2. Materials and Methods
2.1. Search Strategy
2.2. Criteria for Study Selection
2.3. Types of Outcomes
2.4. Data Extraction
2.5. Data Evaluation
3. Results
3.1. Characteristics of Participants and Settings
3.2. Characteristics of Interventions
3.3. Impact and Effectiveness of Interventions
3.3.1. Mental Health
3.3.2. Quality of Life
3.3.3. Service Use
3.3.4. Summary of Other Outcomes
4. Discussion
4.1. Limitations
4.2. Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Omerov, P.; Craftman, Å.G.; Mattsson, E.; Klarare, A. Homeless persons’ experiences of health- and social care: A systematic integrative review. Health Soc. Care Community 2020, 28, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Stafford, A.; Wood, L. Tackling Health Disparities for People Who Are Homeless? Start with Social Determinants. Int. J. Environ. Res. Public Health 2017, 14, 1535. [Google Scholar] [CrossRef] [PubMed]
- Aldridge, R.W.; Menezes, D.; Lewer, D.; Cornes, M.; Evans, H.; Blackburn, R.M.; Byng, R.; Clark, M.; Denaxas, S.; Fuller, J.; et al. Causes of death among homeless people: A population-based cross-sectional study of linked hospitalisation and mortality data in England. Wellcome Open Res. 2019, 4, 49. [Google Scholar] [CrossRef] [PubMed]
- Johnson, G.; Chamberlain, C. Homelessness and Substance Abuse: Which Comes First? Aust. Soc. Work. 2008, 61, 342–356. [Google Scholar] [CrossRef]
- Cheung, A.M.; Hwang, S.W. Risk of death among homeless women: A cohort study and review of the literature. CMAJ 2004, 170, 1243–1247. [Google Scholar] [CrossRef]
- Fazel, S.; Geddes, J.R.; Kushel, M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 2014, 384, 1529–1540. [Google Scholar] [CrossRef]
- Ayano, G.; Assefa, D.; Haile, K.; Chaka, A.; Solomon, H.; Hagos, P.; Yohannis, Z.; Haile, K.; Bekana, L.; Agidew, M.; et al. Mental, neurologic, and substance use (MNS) disorders among street homeless people in Ethiopia. Ann. Gen. Psychiatry 2017, 16, 40. [Google Scholar] [CrossRef]
- Gutwinski, S.; Schreiter, S.; Deutscher, K.; Fazel, S. The prevalence of mental disorders among homeless people in high-income countries: An updated systematic review and meta-regression analysis. PLoS Med. 2021, 18, e1003750. [Google Scholar] [CrossRef]
- Hossain, M.M.; Sultana, A.; Tasnim, S.; Fan, Q.; Ma, P.; McKyer, E.L.J.; Purohit, N. Prevalence of mental disorders among people who are homeless: An umbrella review. Int. J. Soc. Psychiatry 2020, 66, 528–541. [Google Scholar] [CrossRef]
- Salize, H.J.; Werner, A.; Jacke, C.O. Service provision for mentally disordered homeless people. Curr. Opin. Psychiatry 2013, 26, 355–361. [Google Scholar] [CrossRef]
- Bristow, K.; Edwards, S.; Funnel, E.; Fisher, L.; Gask, L.; Dowrick, C.; Chew Graham, C. Help Seeking and Access to Primary Care for People from “Hard-to-Reach” Groups with Common Mental Health Problems. Int. J. Fam. Med. 2011, 2011, 490634. [Google Scholar] [CrossRef] [PubMed]
- Milloy, M.-J.; Kerr, T.; Bangsberg, D.R.; Buxton, J.; Parashar, S.; Guillemi, S.; Montaner, J.; Wood, E. Homelessness as a structural barrier to effective antiretroviral therapy among HIV-seropositive illicit drug users in a Canadian setting. AIDS Patient Care STDS 2012, 26, 60–67. [Google Scholar] [CrossRef]
- Lasser, K.E.; Himmelstein, D.U.; Woolhandler, S. Access to care, health status, and health disparities in the United States and Canada: Results of a cross-national population-based survey. Am. J. Public Health 2006, 96, 1300–1307. [Google Scholar] [CrossRef] [PubMed]
- Lewis, J.H.; Andersen, R.M.; Gelberg, L. Health care for homeless women. J. Gen. Intern. Med. 2003, 18, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Farnarier, C.; Fano, M.; Magnani, C.; Jaffré, Y. Projet TREPSAM: Trajectoire de soins des personnes sans abri à Marseille. Rapport de recherche. Available online: https://halshs.archives-ouvertes.fr/halshs-03454716/document (accessed on 16 September 2022).
- North, C.S.; Smith, E.M. A systematic study of mental health services utilization by homeless men and women. Soc. Psychiatry Psychiatr. Epidemiol. 1993, 28, 77–83. [Google Scholar] [CrossRef]
- Folsom, D.P.; Hawthorne, W.; Lindamer, L.; Gilmer, T.; Bailey, A.; Golshan, S.; Garcia, P.; Unützer, J.; Hough, R.; Jeste, D.V. Prevalence and risk factors for homelessness and utilization of mental health services among 10,340 patients with serious mental illness in a large public mental health system. Am. J. Psychiatry 2005, 162, 370–376. [Google Scholar] [CrossRef]
- Rothbard, A.B.; Min, S.-Y.; Kuno, E.; Wong, Y.-L.I. Long-term effectiveness of the ACCESS program in linking community mental health services to homeless persons with serious mental illness. J. Behav. Health Serv. Res. 2004, 31, 441–449. [Google Scholar] [CrossRef]
- McGill, B.; Corbett, L.; Grunseit, A.C.; Irving, M.; O’Hara, B.J. Co-Produce, Co-Design, Co-Create, or Co-Construct-Who Does It and How Is It Done in Chronic Disease Prevention? A Scoping Review. Healthcare 2022, 10, 647. [Google Scholar] [CrossRef]
- Slattery, P.; Saeri, A.K.; Bragge, P. Research co-design in health: A rapid overview of reviews. Health Res. Policy Syst. 2020, 18, 17. [Google Scholar] [CrossRef]
- Tee, S.; Üzar Özçetin, Y.S. Promoting positive perceptions and person centred care toward people with mental health problems using co-design with nursing students. Nurse Educ. Today 2016, 44, 116–120. [Google Scholar] [CrossRef]
- Tindall, R.M.; Ferris, M.; Townsend, M.; Boschert, G.; Moylan, S. A first-hand experience of co-design in mental health service design: Opportunities, challenges, and lessons. Int. J. Ment. Health Nurs. 2021, 30, 1693–1702. [Google Scholar] [CrossRef]
- O’Reilly, F.; Doyle, J.; Keenan, E. Innovative co-design of integrated services designed to improve access to health care. Int J Integr Care 2017, 17, 480. [Google Scholar] [CrossRef]
- O’Brien, J.; Fossey, E.; Palmer, V.J. A scoping review of the use of co-design methods with culturally and linguistically diverse communities to improve or adapt mental health services. Health Soc. Care Community 2021, 29, 1–17. [Google Scholar] [CrossRef]
- Donetto, S.; Pierri, P.; Tsianakas, V.; Robert, G. Experience-based Co-design and Healthcare Improvement: Realizing Participatory Design in the Public Sector. Des. J. 2015, 18, 227–248. [Google Scholar] [CrossRef]
- Mullins, R.M.; Kelly, B.E.; Chiappalone, P.S.; Lewis, V.J. ‘No-one has listened to anything I’ve got to say before’: Co-design with people who are sleeping rough. Health Expect. 2021, 24, 930–939. [Google Scholar] [CrossRef]
- Campagnaro, C.; Di Prima, N.; Ceraolo, S. Co-Design and the Collective Creativity Processes in Care Systems and Places. Soc. Incl. 2021, 9, 130–142. [Google Scholar] [CrossRef]
- Joyce, D.P.; Limbos, M. Identification of cognitive impairment and mental illness in elderly homeless men: Before and after access to primary health care. Can. Fam. Physician 2009, 55, 1110–1111.e6. [Google Scholar]
- Stergiopoulos, V.; Schuler, A.; Nisenbaum, R.; Deruiter, W.; Guimond, T.; Wasylenki, D.; Hoch, J.S.; Hwang, S.W.; Rouleau, K.; Dewa, C. The effectiveness of an integrated collaborative care model vs. a shifted outpatient collaborative care model on community functioning, residential stability, and health service use among homeless adults with mental illness: A quasi-experimental study. BMC Health Serv. Res. 2015, 15, 348. [Google Scholar] [CrossRef]
- Rog, D.J.; Marshall, T.; Dougherty, R.H.; George, P.; Daniels, A.S.; Ghose, S.S.; Delphin-Rittmon, M.E. Permanent supportive housing: Assessing the evidence. Psychiatr. Serv. 2014, 65, 287–294. [Google Scholar] [CrossRef]
- Aubry, T.; Goering, P.; Veldhuizen, S.; Adair, C.E.; Bourque, J.; Distasio, J.; Latimer, E.; Stergiopoulos, V.; Somers, J.; Streiner, D.L.; et al. A Multiple-City RCT of Housing First With Assertive Community Treatment for Homeless Canadians with Serious Mental Illness. Psychiatr. Serv. 2016, 67, 275–281. [Google Scholar] [CrossRef]
- Jego, M.; Abcaya, J.; Ștefan, D.-E.; Calvet-Montredon, C.; Gentile, S. Improving Health Care Management in Primary Care for Homeless People: A Literature Review. Int. J. Environ. Res. Public Health 2018, 15, 309. [Google Scholar] [CrossRef]
- Dickins, K.; Buchholz, S.W.; Ingram, D.; Hamilton, R.J.; Braun, L.T.; Karnik, N.S.; Earle, M. “Now that you’ve got that coverage”: Promoting use of a regular source of primary care among homeless persons. J. Am. Assoc. Nurse Pract. 2019, 33, 158–166. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009, 3, e123–e130. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- FEANTSA. ETHOS: European Typology of Homelessness and Housing Exclusion. Available online: https://www.feantsa.org/download/ethos2484215748748239888.pdf (accessed on 11 August 2022).
- Cochrane Effective Practice and Organisation of Care. Data Collection Form. EPOC Resources for Review Authors. Available online: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/good_practice_data_extraction_form.doc (accessed on 1 July 2022).
- Cochrane Methods. Tool to Assess Risk of Bias in Cohort Studies. Available online: http://methods.cochrane.org/sites/methods.cochrane.org.bias/files/uploads/Tool%20to%20Assess%20Risk%20of%20Bias%20in%20Cohort%20Studies.pdf (accessed on 1 July 2022).
- Cochrane Training. Chapter 8: Assessing risk of bias in a randomized trial. Available online: https://training.cochrane.org/handbook/current/chapter-08 (accessed on 1 July 2022).
- Corrigan, P.W.; Kraus, D.J.; Pickett, S.A.; Schmidt, A.; Stellon, E.; Hantke, E.; Lara, J.L. Using Peer Navigators to Address the Integrated Health Care Needs of Homeless African Americans With Serious Mental Illness. Psychiatr. Serv. 2017, 68, 264–270. [Google Scholar] [CrossRef]
- Gilmer, T.P.; Stefancic, A.; Ettner, S.L.; Manning, W.G.; Tsemberis, S. Effect of full-service partnerships on homelessness, use and costs of mental health services, and quality of life among adults with serious mental illness. Arch. Gen. Psychiatry 2010, 67, 645–652. [Google Scholar] [CrossRef]
- Stergiopoulos, V.; Gozdzik, A.; Nisenbaum, R.; Durbin, J.; Hwang, S.W.; O’Campo, P.; Tepper, J.; Wasylenki, D. Bridging Hospital and Community Care for Homeless Adults with Mental Health Needs: Outcomes of a Brief Interdisciplinary Intervention. Can. J. Psychiatry 2018, 63, 774–784. [Google Scholar] [CrossRef]
- Larkin, M.; Boden, Z.V.R.; Newton, E. On the Brink of Genuinely Collaborative Care: Experience-Based Co-Design in Mental Health. Qual. Health Res. 2015, 25, 1463–1476. [Google Scholar] [CrossRef]
- Yoo, D.; Huldtgren, A.; Woelfer, J.P.; Hendry, D.G.; Friedman, B. A value sensitive action-reflection model. In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, CHI’13: CHI Conference on Human Factors in Computing Systems, Paris, France, 27 April–2 May 2013; Mackay, W.E., Brewster, S., Bødker, S., Eds.; ACM: New York, NY, USA, 2013; pp. 419–428, ISBN 9781450318990. [Google Scholar]
- Cumming, J.; Clarke, F.J.; Holland, M.J.G.; Parry, B.J.; Quinton, M.L.; Cooley, S.J. A Feasibility Study of the My Strengths Training for Life™ (MST4Life™) Program for Young People Experiencing Homelessness. Int. J. Environ. Res. Public Health 2022, 19, 3320. [Google Scholar] [CrossRef]
- Palma, P.D.; Nordenram, G. The perceptions of homeless people in Stockholm concerning oral health and consequences of dental treatment: A qualitative study. Spec. Care Dentist. 2005, 25, 289–295. [Google Scholar] [CrossRef]
- Rae, B.E.; Rees, S. The perceptions of homeless people regarding their healthcare needs and experiences of receiving health care. J. Adv. Nurs. 2015, 71, 2096–2107. [Google Scholar] [CrossRef]
- Lippert, A.M.; Lee, B.A. Stress, Coping, and Mental Health Differences among Homeless People. Sociol. Inq. 2015, 85, 343–374. [Google Scholar] [CrossRef]
- Gelberg, L.; Andersen, R.M.; Leake, B.D. The Behavioral Model for Vulnerable Populations: Application to medical care use and outcomes for homeless people. Health Serv. Res. 2000, 34, 1273–1302. [Google Scholar] [PubMed]
- Benston, E.A. Housing Programs for Homeless Individuals with Mental Illness: Effects on Housing and Mental Health Outcomes. Psychiatr. Serv. 2015, 66, 806–816. [Google Scholar] [CrossRef] [PubMed]
- Feldman, B.J.; Craen, A.M.; Enyart, J.; Batchelor, T.; Friel, T.J.; Dusza, S.W.; Greenberg, M.R. Prevalence of Homelessness by Gender in an Emergency Department Population in Pennsylvania. J. Am. Osteopath. Assoc. 2018, 118, 85–91. [Google Scholar] [CrossRef]
- Pleace, N. Exclusion by Definition: The Under-representation of Women in European Homelessness Statistics. In Women’s Homelessness in Europe; Mayock, P., Bretherton, J., Eds.; Palgrave Macmillan UK: London, UK, 2016; pp. 105–126. ISBN 978-1-137-54515-2. [Google Scholar]
- Smith, C.; Castañeda, E. Sick Enough? Mental Illness and Service Eligibility for Homeless Individuals at the Border. Soc. Sci. 2020, 9, 145. [Google Scholar] [CrossRef]
| Authors | Sample Size | Study Design | Duration of Participation | Participants | ETHOS Category | Sex Distribution | Types of Intervention | Types of Outcome Measures | Results |
|---|---|---|---|---|---|---|---|---|---|
| Corrigan et al. [40] | 67 | RCT | 12 months | African Americans with serious mental illness who were homeless | 1.1 | Male: 41 (61%); Female: 26 (39%) | A one-year trial of PNP compared with TAU | Physical illness; psychiatric disorder; recovery; quality of life | Significant improvement in self-reported physical and mental health, recovery, and quality of life for those in the PNP program compared with treatment as usual, while both groups improved their domicile and insurance coverage. |
| Gilmer et al. [41] | 363 | Quasi-experimental | 24 months | Adult PEH with severe mental illness who were FSP clients and clients receiving public mental health services | 1.1; 2.1 | Male: 228 (63%); Female: 135 (37%) | Housing First programs that do “whatever it takes” to improve residential stability and mental health outcomes | Recovery outcomes; mental health service use; mental health services and housing costs from the perspective of the public mental health system; quality of life | Participation in an FSP was associated with substantial increases in outpatient services and days spent in housing. Reductions in costs of inpatient/emergency and justice system services offset 82% of the cost of the FSP. |
| Stergiopoulos et al. [29] | 142 | Quasi-experimental | 12 months | Men experiencing homelessness and mental illness | 1.1; 2.1; 8.1 | Male: 142 (100%) | Shelter-based collaborative mental healthcare models IMCC and SOCC | Community functioning; residential stability; health service use | Participants experienced significant improvements in community functioning, housing, hospitalizations, emergency department visits, and community-based physician visits in both shelter-based collaborative mental healthcare programs over time. Due to the lack of observable differences, the less resource-intensive SOCC appears more favorable than the IMCC. |
| Stergiopoulos et al. [42] | 223 | Cohort study | 6 months | Adult PEH with mental health needs | 1.1; 2.1; 8.1 | Male: 173 (78%); Female: 50 (22%) | CATCH program, a 4- to 6-month interdisciplinary intervention offering case management, peer support, access to primary psychiatric care, and supplementary community services | Change in participant health status; mental health symptoms; disease-specific quality of life; substance use; acute service use; housing; working-alliance construct | CATCH participants showed significant mental and physical health gain and reductions in mental health symptoms, substance use, and hospital admissions. An association was found between the strength of the participant-case manager working alliance and reduced healthcare use and mental health symptoms. |
| Authors | Quality Appraisal Tool | Domain | Risk of Bias |
|---|---|---|---|
| Corrigan et al. [40] | Risk of Bias assessment [37] | Random sequence generation | Unclear |
| Allocation concealment | Unclear | ||
| Blinding of participants and personnel | High risk | ||
| Blinding of outcome assessment | Unclear | ||
| Incomplete outcome data | Low risk | ||
| Selective outcome reporting | Low risk | ||
| Gilmer et al. [41] | Risk of Bias assessment [37] | Random sequence generation | High risk |
| Allocation concealment | High risk | ||
| Blinding of participants and personnel | High risk | ||
| Blinding of outcome assessment | Unclear | ||
| Incomplete outcome data | Low risk | ||
| Selective outcome reporting | Low risk | ||
| Stergiopoulos et al. [29] | Risk of Bias assessment [37] | Random sequence generation | High risk |
| Allocation concealment | High risk | ||
| Blinding of participants and personnel | High risk | ||
| Blinding of outcome assessment | Unclear | ||
| Incomplete outcome data | Low risk | ||
| Selective outcome reporting | Low risk | ||
| Stergiopoulos et al. [42] | Tool to Assess Risk of Bias in Cohort Studies [38] | Selection of exposed and non-exposed cohorts was drawn from the same population | Low risk |
| Confidence in the assessment of exposure | Low risk | ||
| Confidence that the outcome of interest was not present at start of study | Low risk | ||
| Matching of exposed and unexposed for all variables that are associated with the outcome of interest or adjustment of statistical analysis for these prognostic variables | Low risk | ||
| Confidence in the assessment of the presence or absence of prognostic factors | Low risk | ||
| Confidence in the assessment of outcome | High risk | ||
| Adequacy of follow-up of cohorts | High risk | ||
| Similarity of co-interventions between groups | High risk |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schiffler, T.; Kapan, A.; Gansterer, A.; Pass, T.; Lehner, L.; Gil-Salmeron, A.; McDermott, D.T.; Grabovac, I. Characteristics and Effectiveness of Co-Designed Mental Health Interventions in Primary Care for People Experiencing Homelessness: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 892. https://doi.org/10.3390/ijerph20010892
Schiffler T, Kapan A, Gansterer A, Pass T, Lehner L, Gil-Salmeron A, McDermott DT, Grabovac I. Characteristics and Effectiveness of Co-Designed Mental Health Interventions in Primary Care for People Experiencing Homelessness: A Systematic Review. International Journal of Environmental Research and Public Health. 2023; 20(1):892. https://doi.org/10.3390/ijerph20010892
Chicago/Turabian StyleSchiffler, Tobias, Ali Kapan, Alina Gansterer, Thomas Pass, Lisa Lehner, Alejandro Gil-Salmeron, Daragh T. McDermott, and Igor Grabovac. 2023. "Characteristics and Effectiveness of Co-Designed Mental Health Interventions in Primary Care for People Experiencing Homelessness: A Systematic Review" International Journal of Environmental Research and Public Health 20, no. 1: 892. https://doi.org/10.3390/ijerph20010892
APA StyleSchiffler, T., Kapan, A., Gansterer, A., Pass, T., Lehner, L., Gil-Salmeron, A., McDermott, D. T., & Grabovac, I. (2023). Characteristics and Effectiveness of Co-Designed Mental Health Interventions in Primary Care for People Experiencing Homelessness: A Systematic Review. International Journal of Environmental Research and Public Health, 20(1), 892. https://doi.org/10.3390/ijerph20010892









