The Job that Kills the Worker: Analysis of Two Case Reports on Work-Related Stress Deaths in the COVID-19 Era
Abstract
1. Introduction
1.1. The Definition and Reasons for Work-Related Stress
- -
- Working conditions (exposures to physical and mental stressful situations: jobs involving long exposure to heat/cold, noise, toxic and/or hazardous substances, radiation, shifts that exceed the allowed hours, insufficient compensation, etc.);
- -
- Work organization (lack of work schedule planning, relationship with managers or colleagues, attitude between work and studies performed, etc.);
- -
- Communication in the work environment (prospects for career advancement, uncertainty of work shifts, etc.);
- -
- -
- Frequent mood swings;
- -
- Irritability;
- -
- Depression;
- -
- Migraine headaches;
- -
- Insomnia;
- -
- Gastro-intestinal disorders;
- -
- Difficulty with memory or concentration;
- -
1.2. The Hazards of Work Stress in the COVID-19 Era
1.3. The Epidemiology of Work Stress-Related Death in the COVID-19 Era
2. Materials and Methods
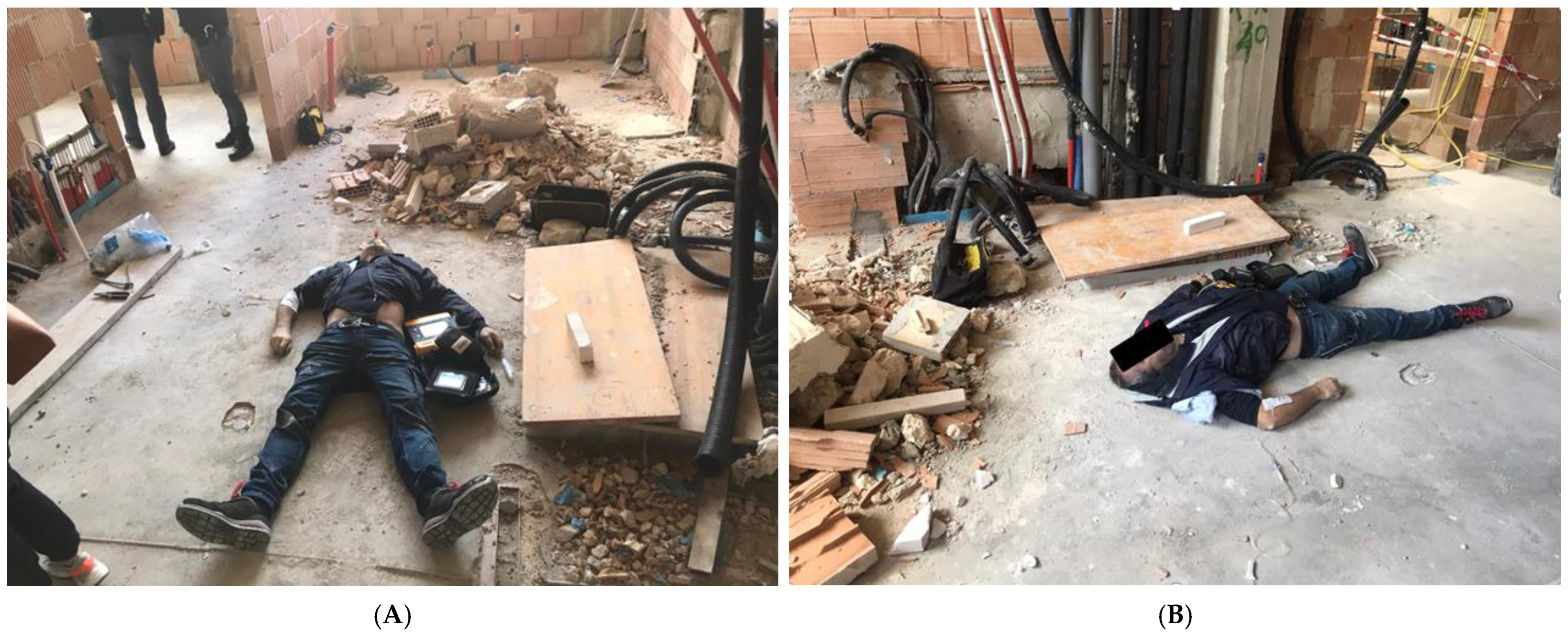
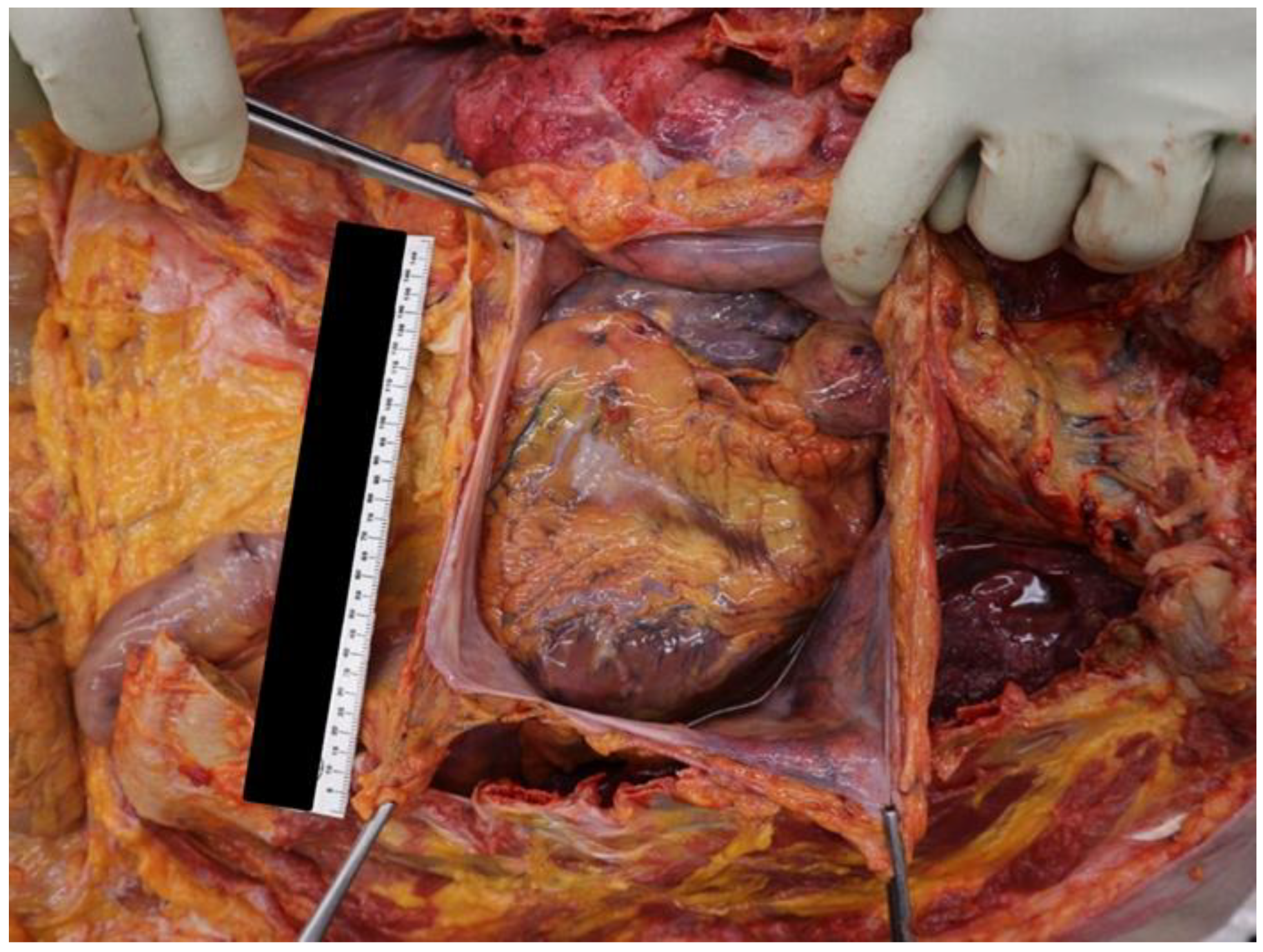
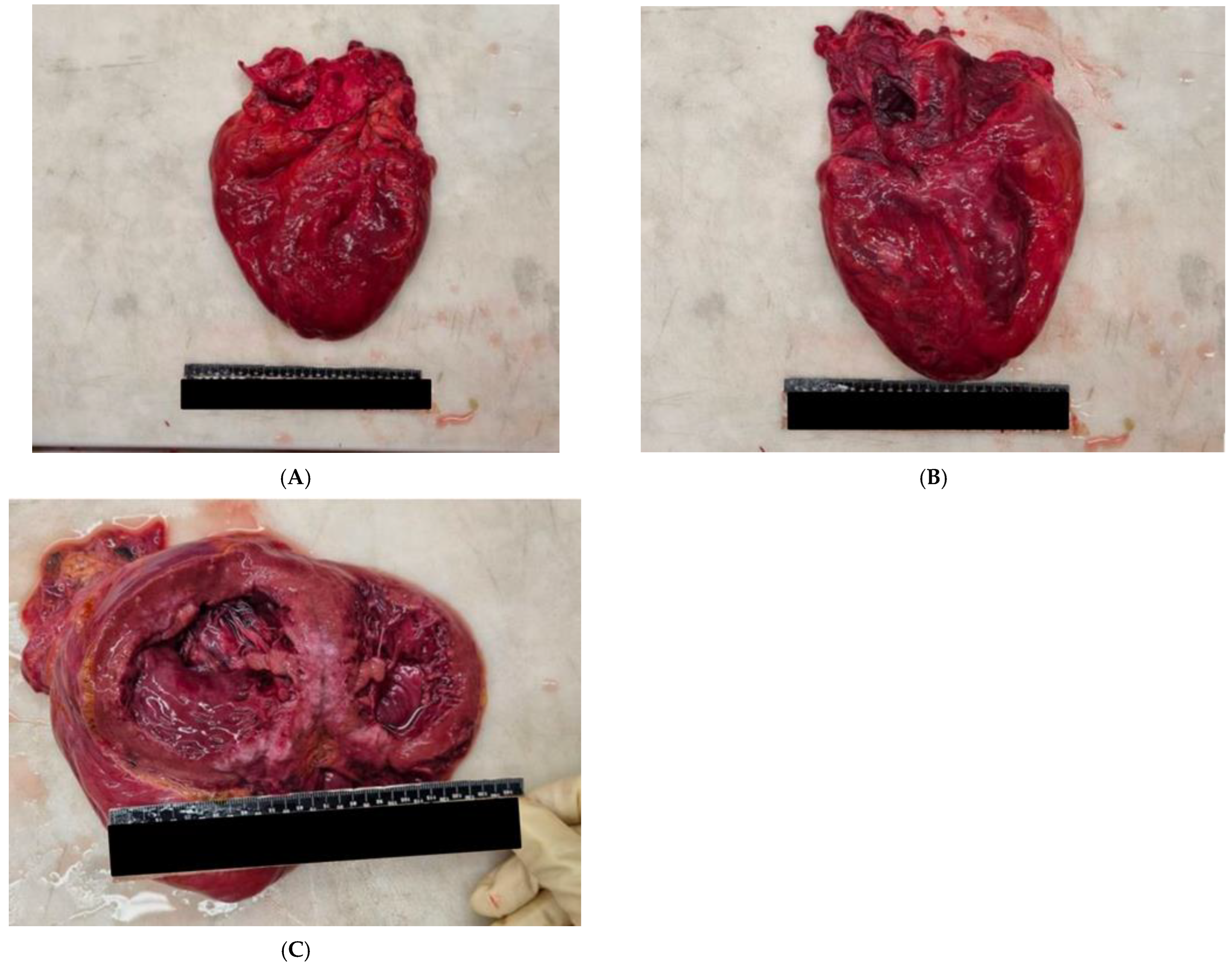
2.1. Case Report 1
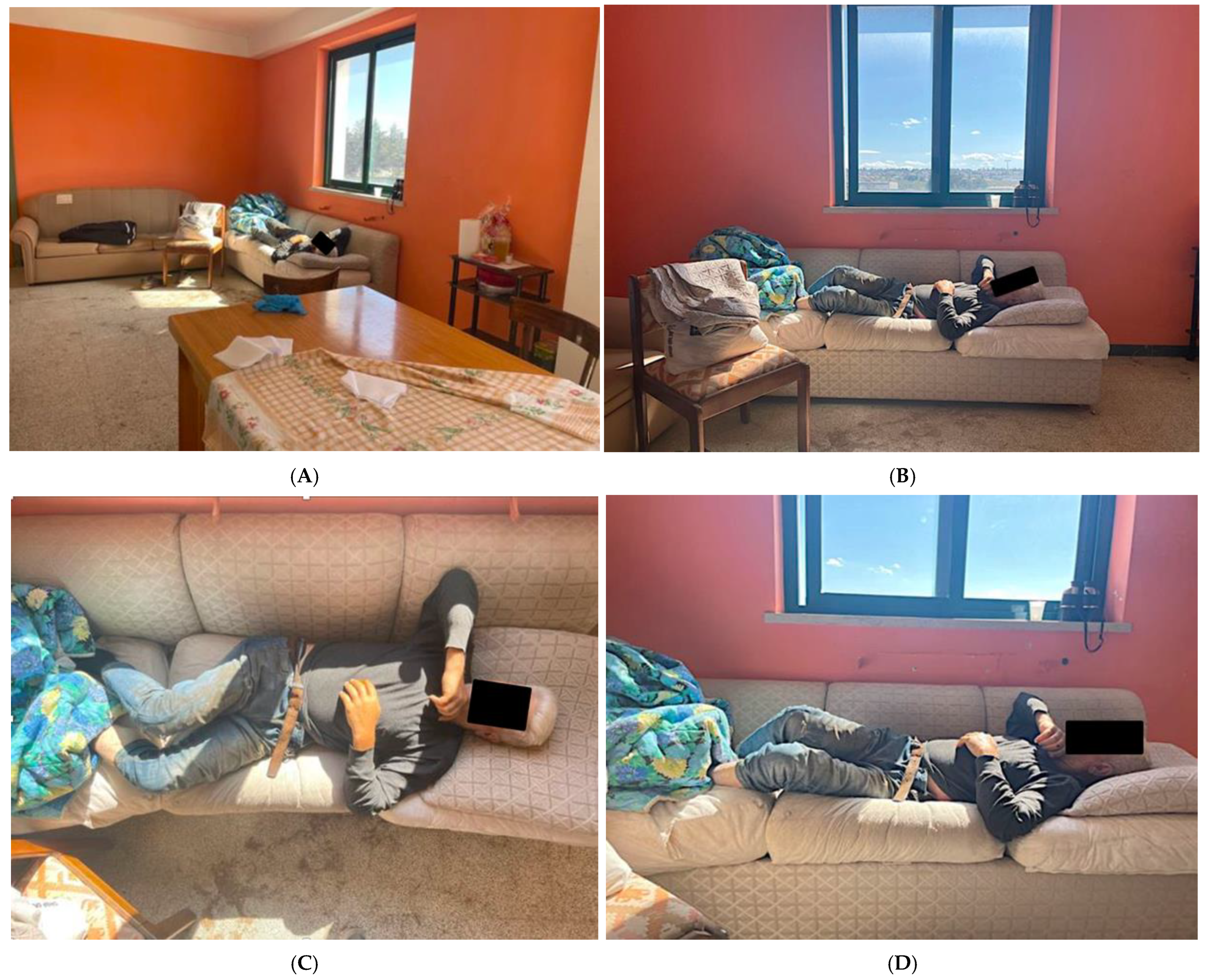
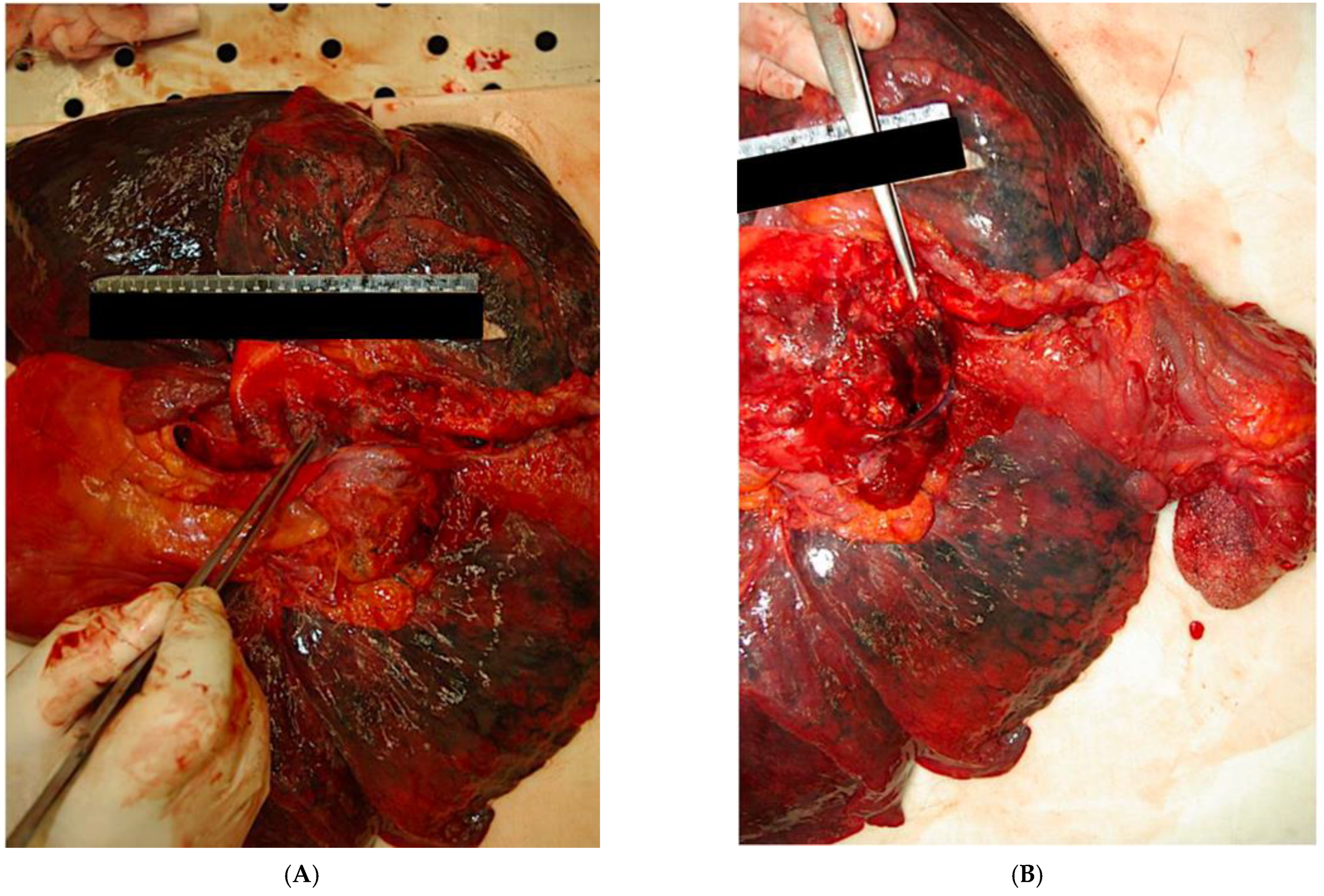
2.2. Case Report 2
3. Discussion
- -
- Deterioration of commitment to work;
- -
- Deterioration of emotions originally associated with work;
- -
- Inadequate fit between person and work.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Restrepo, J.; Lemos, M. Addressing psychosocial work-related stress interventions: A systematic review. Work 2021, 70, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Accordo Europeo sullo Stress sul Lavoro. Accordo Siglato da CES—Sindacato Europeo; UNICE “Confindustria Europea”; UEAPME—Associazione Europea Artigianato e PMI.; CEEP—Associazione Europea Delle Imprese Partecipate dal Pubblico e di Interesse Economico Generale) Bruxelles. 2004. Available online: https://www.icvoltalatina.edu.it/sito/wp-content/uploads/2015/12/Accordo_europeo_sullo_stress_8_10_2004.pdf (accessed on 14 November 2022).
- Direttiva 89/391/CEE del Consiglio, del 12 Giugno 1989, Concernente L’attuazione di Misure Volte a Promuovere il Miglioramento della Sicurezza e della Salute dei Lavoratori Durante il Lavoro. Available online: https://eur-lex.europa.eu/legal-content/IT/TXT/HTML/?uri=CELEX:31989L0391&from=EN (accessed on 14 November 2022).
- Conti, A.; Russotto, S.; Opizzi, A.; Ratti, M.; Nicolini, D.; Vanhaecht, K.; Panella, M. Work-Related Stress among a Cohort of Italian Long-Term Care Workers during the COVID-19 Pandemic: An Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 5874. [Google Scholar] [CrossRef] [PubMed]
- Khan, Y.H.; Mallhi, T.H.; Alotaibi, N.H.; Alzarea, A.I. Work related stress factors among healthcare professionals during COVID-19 pandemic; a call for immediate action. Hosp. Pract. 2020, 48, 244–245. [Google Scholar] [CrossRef] [PubMed]
- Restubog, S.L.D.; Ocampo, A.C.G.; Wang, L. Taking control amidst the chaos: Emotion regulation during the COVID-19 pandemic. J. Vocat. Behav. 2020, 119, 103440. [Google Scholar] [CrossRef] [PubMed]
- Descatha, A.; Sembajwe, G.; Pega, F.; Ujita, Y.; Baer, M.; Boccuni, F.; Di Tecco, C.; Duret, C.; Evanoff, B.A.; Gagliardi, D.; et al. The effect of exposure to long working hours on stroke: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ. Int. 2020, 142, 105746. [Google Scholar] [CrossRef]
- Vinci, F.; Marrone, M.; Tarantino, F.; De Donno, A. Patologia Medico-Legale E Tanatologia. In Quadri Classici e Casistica Illustrata; Aracne Editrice: Roma, Italy, 2012. [Google Scholar]
- Chiodi, V.; Gilli, R.; Puccini, C.; Portigliatti-Barbos, M.; Fallani, M.; De Bernardi, A. Manuale di Medicina Legale; Società Editrice Libraria S.p.A.: Milano, Italy, 1976. [Google Scholar]
- Torre, C.; Varetto, L. L’autopsia Giudiziaria; Piccin Nuova Libreria S.p.A.: Padova, Italy, 1989. [Google Scholar]
- Baudelot, C. La souffrance au travail, réflexion sociologique [Work related stress, sociological analysis]. Soins 2018, 63, 16–19. [Google Scholar] [CrossRef]
- Maslach, C.; Leiter, M. Preventing Burnout and Building Engagement; Jossey-Bass: San Francisco, CA, USA, 2000. [Google Scholar]
- Kivimäki, M.; Jokela, M.; Nyberg, S.T.; Singh-Manoux, A. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet 2015, 386, 1739–1746. [Google Scholar] [CrossRef]
- Ferketich, A.K.; Binkley, P.F. Psychological distress and cardiovascular disease: Results from the 2002 National Health Interview Survey. Eur. Heart J. 2005, 26, 1923–1929. [Google Scholar] [CrossRef]
- De Hert, M.; Detraux, J.; Vancampfort, D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin. Neurosci. 2018, 20, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Sara, J.D.; Prasad, M.; Eleid, M.F.; Zhang, M.; Widmer, R.J.; Lerman, A. Association Between Work-Related Stress and Coronary Heart Disease: A Review of Prospective Studies through the Job Strain, Effort-Reward Balance, and Organizational Justice Models. J. Am. Heart Assoc. 2018, 7, e008073. [Google Scholar] [CrossRef] [PubMed]
- Fallani, P.; Porrone, A. Rapporti tra Cardiopatia Ischemica e Stress Lavorativo: Riflessioni e Valutazione Medico-Legale. Tagete—Archives of Legal Medicine and Dentistry. Available online: https://www.yumpu.com/it/document/view/16041766/27082012-tagete-archives-of-legal-medicine-and-dentistry (accessed on 14 November 2022).
- Fishta, A.; Backé, E.M. Psychosocial stress at work and cardiovascular diseases: An overview of systematic reviews. Int. Arch. Occup. Environ. Health 2015, 88, 997–1014. [Google Scholar] [CrossRef] [PubMed]
- Chandola, T.; Britton, A.; Brunner, E.; Hemingway, H.; Malik, M.; Kumari, M.; Badrick, E.; Kivimaki, M.; Marmot, M. Work stress and coronary heart disease: What are the mechanisms? Eur. Heart J. 2008, 29, 640–648. [Google Scholar] [CrossRef] [PubMed]
- Cannizzaro, E.; Cirrincione, L.; Mazzucco, W.; Scorciapino, A.; Catalano, C.; Ramaci, T.; Ledda, C.; Plescia, F. Night-Time Shift Work and Related Stress Responses: A Study on Security Guards. Int. J. Environ. Res. Public Health 2020, 17, 562. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marrone, M.; Angeletti, C.; Cazzato, G.; Sebastiani, G.; Buongiorno, L.; Caricato, P.; Pititto, F.; Cascardi, E.; Stellacci, A.; De Luca, B.P. The Job that Kills the Worker: Analysis of Two Case Reports on Work-Related Stress Deaths in the COVID-19 Era. Int. J. Environ. Res. Public Health 2023, 20, 884. https://doi.org/10.3390/ijerph20010884
Marrone M, Angeletti C, Cazzato G, Sebastiani G, Buongiorno L, Caricato P, Pititto F, Cascardi E, Stellacci A, De Luca BP. The Job that Kills the Worker: Analysis of Two Case Reports on Work-Related Stress Deaths in the COVID-19 Era. International Journal of Environmental Research and Public Health. 2023; 20(1):884. https://doi.org/10.3390/ijerph20010884
Chicago/Turabian StyleMarrone, Maricla, Carlo Angeletti, Gerardo Cazzato, Gabriele Sebastiani, Luigi Buongiorno, Pierluigi Caricato, Fortunato Pititto, Eliano Cascardi, Alessandra Stellacci, and Benedetta Pia De Luca. 2023. "The Job that Kills the Worker: Analysis of Two Case Reports on Work-Related Stress Deaths in the COVID-19 Era" International Journal of Environmental Research and Public Health 20, no. 1: 884. https://doi.org/10.3390/ijerph20010884
APA StyleMarrone, M., Angeletti, C., Cazzato, G., Sebastiani, G., Buongiorno, L., Caricato, P., Pititto, F., Cascardi, E., Stellacci, A., & De Luca, B. P. (2023). The Job that Kills the Worker: Analysis of Two Case Reports on Work-Related Stress Deaths in the COVID-19 Era. International Journal of Environmental Research and Public Health, 20(1), 884. https://doi.org/10.3390/ijerph20010884









