Peristomal Skin Complications in Ileostomy and Colostomy Patients: What We Need to Know from a Public Health Perspective
Abstract
1. Introduction
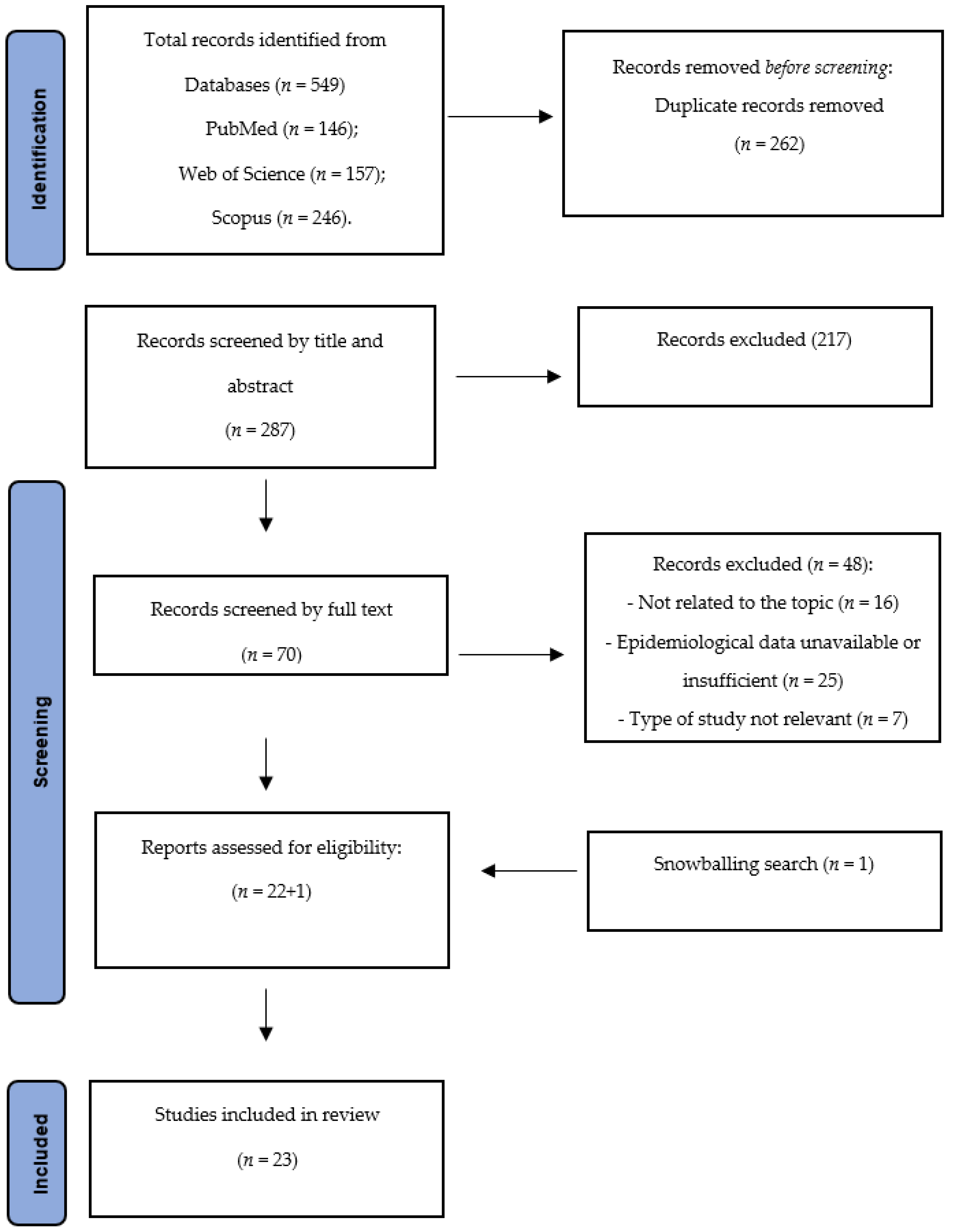
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion/Exclusion Criteria
2.3. Selection Process and Data Extraction
3. Results
3.1. Clinical-Epidemiological Burden of PSCs
3.2. Time of onset of PSCs
3.3. Classification and Assessment Tools
3.4. Risk Factors Related to PSCs
3.5. Hospital Admissions and Readmissions Related to PSCs
| First Author, Year, [Ref.] | Study Type | N. of Included Studies | Type of Ostomy Surgery | Underlying Diseases Leading to Ostomy Surgery | Main Findings |
|---|---|---|---|---|---|
| Malik T.A.M, 2018, [38] | Systematic review | 18 trials | Ileostomy and Colostomy | Colorectal cancer, diverticular disease, fecal incontinence, constipation, irritable bowel syndrome, typhoid, tuberculosis, trauma, colovesical fistula and familial adenomatous polyposis syndrome | PSCs had the highest incidence across all ostomy types at 14.0% (2.4–46.2%), followed by parastomal hernia, which occurred in 5.5% of patients (0–88.2%). PSCs were most common in patients with a loop ileostomy (median 14.0%) and loop colostomy (median 32.3%). |
| First Author, Year, Country, [Ref.] | Study Type | Sample Size and Population Characteristics | Type of Surgery (Ileo- or Colostomy) | Underlying Diseases | Epidemiological Data on PSCs | Type of PSCs and Related Data | Classification Tools | Risk Factors Related to PSCs | Time-to-Onset of PSCs | Hospitaladmissions/Readmissions/Other Healthcare Services Costs |
|---|---|---|---|---|---|---|---|---|---|---|
| Salvadalena G.D, 2013, US, [29] | Prospective study | Tot: 47 patients; M: 24 patients (51%); F: 23 patients (50%); Age: 47.6 ± 15.2 years (range 20–81 years) | Colostomy: 8 patients (17%); Ileostomy: 37 patients (79%); Urostomy: 2 patients (4%) | Ulcerative colitis; Crohn disease; Colorectal cancer; Perforated colon; Bladder cancer; Fistula; Others (Clostridium difficile colitis, indeterminate colitis, failed ileoanal pouch, familial adenomatous polyposis) | PSCs combined cumulative incidence: 63% | Moisture-associated skin damage: 14 patients; Skin infections (e.g., fungus or folliculitis): 11 patients; Erosion (excoriated; moist and bleeding): 8 patients; Erythema: 7 patients. | N.A. | N.A. | Most frequently 21–40 days after surgery ostomy | N.A. |
| Lindholm E, 2013, Sweden, [30] | Prospective study | Tot: 144 patients; Mean age: 67 years (range 53.5–78 years) | End colostomy: 84 patients (58%); Loop colostomy: 10 patients (7%); End ileostomy: 26 patients (18%); Loop ileostomy: 24 patients (17%). | Diverticulitis: 41 patients (28%); Gynecological cancer: 28 patients (19%); Rectal cancer: 19 patients (14%); Colon cancer: 18 patients (13%); IBD: 15 patients (10%); Other types of cancers, fistulas, or sphincter rupture after delivery: 23 patients (16%). | PSCs Prevalence: at 3–6 months: 45%; at 12 months: 21%; at 24 months: 18%. | N.A. | Severe peristomal skin problems (classified as E++): 4–19% | N.A. | On ward: 9 patients (6.5%); After 2 weeks: 22 patients (19.3%); After 3 months: 14 patients (13.6%); After 6 months: 12 patients (16.9); After 1 year: 3 patients (5.3%); After 2 year: 1 patient (3.8%). | N.A. |
| Baykara Z.G, 2014, Turkey, [22] | Retrospective study | Tot: 748 patients; M: 408 patients (54.5%); F: 340 patients (45.5%); Mean age: 56.60 ± 16.73 years. | Ileostomy: 363 patients (48.5%); Colostomy: 354 patients (47.3%) | Cancer: 545 patients (72.9%); IBD: 58 patients (7.8%); Bowel obstruction: 35 patients (4.7%); Injuries: 34 patients (4.5%); Intestinal perforation: 14 patients (1.9%); Fistula: 13 patients (1.7%) Familial adenomatous polyposis: 11 patients (1.5%); Anorectal malformation: 6 patients (0.8%); Mesenteric ischemia: 6 patients (0.8%); Sigmoid volvulus: 6 patients (0.8%); Intra-abdominal abscess: 4 patients (0.5%); Other: 16 patients (2.1%) | PSCs rate by type of surgery Emergency: 43 patients (19.5%); Planned: 93 patients (17.6%) | Peristomal skin problems: 136 (48.7%) Maceration: 2 (0.7%) Allergy: 1 (0.4%) | N.A. | Unplanned/ Emergency ostomy procedure; Multiple ostomies; Type of ostomy. | N.A. | N.A. |
| Sarkut P, 2015, Turkey, [23] | Retrospective study | Tot: 141 patients; M: 95 patients (67%); F: 46 patients (33%); Mean age: 47 years (range: 17–67 years) | End ileostomy 43%; Loop ileostomy 46%; Double-barrel ileostomy 11%. | Benign causes: 48%; Malign causes: 52% | N.A. | Maceration in the peristomal skin: 10 patients | N.A. | N.A. | N.A. | N.A. |
| Carlsson E, 2016, Sweden, [31] | Prospective Study | Tot: 207 patients; F: 53% Mean age: 70 years (range 19–94 years); Elective surgery: 74% | Colostomy: 146 patients (71%); End ileostomy: 54 patients (26%); Loop ileostomy: 7 patients (3%) | Colorectal cancer: 62%; IBD: 19% | PSCs prevalence: 23 patients (11%); PSCs with colostomy: 9 patients (6%); PSCs with an end or loop ileostomy: 14 patients (23%) | N.A. | Erythematous-erosive skin lesions (E+): 16 patients; Erythematous-erosive skin lesions (E++): 5 patients; Ulcerations (pyoderma gangrenosum): 2 patients | N.A. | N.A. | N.A. |
| Cressey B.D, 2017, USA, [24] | Retrospective study | Tot: 18 patients; M: 11 patients; F: 7 patients; Mean age: 60.4 years (range: 35–87 years) | Colostomy: 9 patients; Ileostomy: 3 patients; Ileal conduit diversions: 6 patients | Cancer (colorectal: 7 patients; genitourinary: 6 patients; ovarian: 2 patients) | N.A. | Peristomal contact dermatitis: 12 patients; Erythematous extending out from the stoma: 18 patients; Erosion: 1 patient; Ulceration: 1 patient. | N.A. | N.A. | N.A. | N.A. |
| Taneja C, 2017, US, [13] | Retrospective study | Tot: 128 patients; M: 67 patients (52.3%); F: 61 patients (47.7%); Mean Age: 60.6 ± 15.6 years | Colostomy: 51 patients (40%); Ileostomy: 64 patients (50%) | N.A. | PSCs incidence: 36.7% within 90 days following surgery [35.3% (n = 18) with colostomies; 43.8% (n = 28) with ileostomies]. | N.A. | N.A. | N.A. | Average time from surgery to first notation of PSCs: 23.7 ± 20.5 days; Colostomy: 23.2 ± 20.8 days; Ileostomy: 24.2 ± 21.1 days. | The mean length of stay for the index admission: 21.5 days for patients with PSCs vs. 13.9 days for all other patients. Readmissions: 22 patients (46.8%) with PSCs vs. 27 patients (33.3%) without PSCs; Readmissions for PSCs with colostomy: 8 patients (44.4%); Readmissions for PSCs with ileostomy: 14 patients (50.0%); Mean number of outpatient care visits: 11.4 (6.2%); Outpatient care visits for PSCs with colostomy: 13.4 (6.3%); Outpatient care visits for PSCs with ileostomy: 10.4 (5.7%); Mean number of home care visits: Home care visits for PSCs with colostomy: 9.2 (4.4%); -Home care visits for PSCs with ileostomy: 8.7 (5.0%). |
| Harputlu D.U, 2018, Turkey, [32] | Prospective study | Tot: 35 patients; F: 22 patients (62.9%); Mean age: 57.45 ± 14.70 years; Intervention group (home care visits): 18 patients; Control group (outpatient/ clinic care): 17 patients | Ileostomy: 21 patients (60.0%); Permanent ostomy: 18 patients (51.4%); Unspecified ostomy: 8 patients (22.9%) | No chronic disease: 20 patients (57.1%); Rectal cancer: 14 patients (40%); Unspecified cause: 1 patient (2.9%) | N.A. | PSCs in Intervention group (Home nursing care): Irritant dermatitis: 12 patients (66.7%); 16.7% with a colostomy and 50% with an ileostomy. Mechanical trauma: 3 patients (16.7%); Allergic dermatitis: 2 patients (11.1%); Both allergic and irritant dermatitis: 1 patient (5.6%) PSCs in Control group (Outpatient/clinic care): Irritant dermatitis: 14 patients (82.4%); 23.5% with a colostomy and 58.8% with an ileostomy. Mechanical trauma: 2 patients (11.8%); Allergic dermatitis: 1 patient (5.9%) | Application of the OST to describe the severity, extent, and likely cause of a peristomal skin disorder | Diabetes mellitus; Immobility: Chemotherapy or/and radiotherapy | Irritant dermatitis in intervention group: appearance in the early postoperative period (0 to 29 days) in 2 patients with colostomy and 3 with ileostomy; Irritant dermatitis in control group: appearance in the early postoperative period (0 to 29 days) in 3 patients with ileostomy | N.A. |
| Nichols TR, 2018 US, [34] | Cross-sectional study | M: 1230 patients; Mean age: 53.5 years (range 65.1 ±12.6 years); F: 1070 patients; Mean age: 46.5 years (range 61.8 ±13.4 years) | Ileostomy: 1031 patients (44.3%); Colostomy: 920 patients (39.5%); Urostomy: 308 patients (13.2%); Multiple types: 33 patients (1.4%) | N.A. | N.A. | Peristomal skin irritation | Self-report assessment: Level 1: peristomal skin integrity, no presence of irritated skin (n = 551 patients); Level 2: low to moderate level of reddening and irritation, occasional but slight blistering (n = 1029 patients); Level 3: severe irritation and reddening with severe blistering, denuded skin and ulceration (n = 427 patients). | N.A. | N.A. | N.A. |
| Nichols & Inglese, 2018 US, [18] | Cross-sectional study | M: 1230 patients (53.48%); Mean age: 65.12 ± 12.62 years; F: 1030 patients (46.52%); Mean age: 61.77 ± 13.43 years | Colostomy: 920 patients (39.50%); Ileostomy: 1031 patients (44.27%); Urostomy: 308 patients (13.22%); Multiple stomas: 33 patients (1.42%); Unknown: 37 patients (1.59%) | N.A. | N.A. | Skin irritation | Self-report assessment: Intact (normal) skin: 551 patients; Mild to moderate skin irritation: 1029 patients; Severely irritated skin: 427 patients | N.A. | N.A. | N.A. |
| Menin G, 2019, Italy, [5] | Cross-sectional study | Tot: 110 patients; M: 57 patients (51.8%); F: 53 patients (48.2%); Mean age: 69 years (range 19–90 years) | Ileostomy 47.3%; Colostomy 38.2%; Other types of procedures 14.5%. | Cancer: 58 patients (52.7%); Chronic intestinal inflammatory: 10 patients (9.1%); Diverticulitis: 9 patients (8.2%); Others: 33 patients 30% | N.A. | Erythema: 19 patients (17.3%); Papules: 2 patients (1.8%); Pustules: 2 patients (1.8%); Vesicles: 2 patients (1.8%); Bubbles (>0.5 mm): 1 patients (0.9%); Overgrowth of tissue: 14 patients (12.7%); Erosion: 36 patients (32.7%); Healing ulcer: 5 patients (4.6%); Mixed ulcer: 21 patients (19.1%); Worsening ulcer: 8 patients (7.3%) | The Peristomal Lesion Scale (PLS) vs. SACS Instruments: PSCs according to PLS: Elementary (Erythema, Papules, Pustules, Vesicles, Bubbles (>0.5 mm): 26 patients; Overgrowth of tissue: 14 patients; Ulcerative (Erosion, Healing ulcer, Mixed ulcer, Worsening ulcer): 70 patients. -PSCs according to SACS classification *: L1: 22 patients (20%); L2: 39 patients (35.5%); L3: 22 patients (20%); L4: 11 patients (10%); LX: 15 patients (14.5%) | - | - | - |
| Taneja C, 2019, US, [3] | Retrospective study | Tot: 168 patients; M: 78 patients (46.4%); F: 90 patients (53.6%); Mean age: 63.9 years | Colostomy: 108 patients (64.3%); Ileostomy: 40 patients (23.8%) | N.A. | PSCs incidence: 36.3% | N.A. | N.A. | N.A. | PSCs within 90 days of ostomy surgery: 36.3% (ileostomy, 47.5%; colostomy, 36.1%); Mean time from surgery to first notation of a PSC: 26.4 days; Ileostomy group: 24.1 days; Colostomy groups: 27.2 days | Patients with PSCs were more likely to be readmitted to hospital by day 120 (55.7% vs. 35.5% for those without PSCs); Mean length of stay for PSCs patients readmitted to hospital: 11.0 days vs. 6.8 days for those without PSCs; Mean number of outpatient care visits: Colostomy: 7.4 (6.3%); Ileostomy: 5.7 (2.0%), Mean total PSCs healthcare cost over 120 days per patients: USD 58,329 vs. USD 50,298 for those without PSCs |
| Nagano M, 2019, Japan, [25] | Retrospective study | Tot: 89 patients; M: 58 patients (65.2%); F: 31 patients (34.8%); Mean age: 65 years | Ileostomy: 52 patients (58.4%); Colostomy: 37 patients (41.6%) | Colorectal cancer | N.A. | MASD | N.A. | Ileostomies; Temporary stomas; Chemotherapy | 8 week after ostomy surgery: 51.9% of MASD | N.A. |
| Voegeli D., 2020, UK, [37] | Multinational survey | Tot: 4235 patients; M: 55% F: 45% | Colostomy: 43%; Ileostomy: 38%; More than one: 2% | N.A. | PSCs self-reported incidence: 73.4% | Itching: 67%; Bleeding: 45%; Discoloration: 38%; Burning: 32%; Moisture from damage: 28%; Pain: 21%; Wounds:11%; Tissue overgrowth: 7% | N.A. | Higher risk of PSCs after ileostomy surgery: 1.9 higher than in those with colostomy; 1.5 times higher risk of PSCs in the first 2 years after ostomy surgery; Greater risk in women: 1.35 more than in men. | N.A. | N.A. |
| Carbonell B.B, 2020, Switzerland, [26] | Retrospective study | Tot: 111 patients; M: 64 patients (58%); F: 47 patients (42%); Mean age: 67.61 ± 15 | Colostomy: 40 patients (36%); Ileostomy: 71 patients (64%) | Malignant disease: 72 patients (65%); Benign disease: 39 patients (35%) | PSCs rate: 73% | Mild complications: Hyperemic lesion: 6 patients (5%); Erosive lesion: 25 patients (23%); Suture Fissure: 9 patients (8%); Relevant complications: Ulcerative lesion: 6 patients (5%); Muco-cutaneous separation: 57 patients (51%); Abscess: 3 patients (3%); Retraction: 5 patients (5%); Necrosis: 2 patients (2%) | SACS classification | Predictors for persistence of peristomal complications at 30 postoperative days: ASA score III/IV; urgent surgery | Early peristomal complications are common, usually mild. They are most likely to persist beyond 30 days in patients operated as emergencies and with an ASA score of III-IV | N.A. |
| Salvadalena G, 2020, US, [12] | Retrospective study | Tot: 73 patients; M: 44 patients; F: 29 patients; Mean age: 56.2 ± 14.2 years | Colostomy: 35 patients (48.0%); Ileostomy: 33 patients (45.2%) | Bowel cancer: 36 patients (49.3%); Bladder cancer: 4 patients (5.5%); Crohn’s disease: 4 patients (5.5%); Ulcerative colitis: 8 patients (11.0%); Diverticulitis: 11 patients (15.1%); Familial polyposis: 1 patients (1.4%); Intestinal obstruction and/or perforation: 5 patients (6.8%); Other: 10 patients (13.7%) | N.A. | Irritant dermatitis: 37 patients (50.7%); Maceration: 15 patients (20.5%); Mechanical trauma: 12 patients (16.4%); Folliculitis: 3 patients (4.1%); Pyoderma gangrenosum, fungal rash, skin infection: 1 patient (1.4%) | Severities were grouped into mild, moderate, and severe, using a range score (0–15). | Stoma duration and/or peristomal creases; Increased risk of PSCs for every 1-week increase in ostomy duration. | 64 days after undergoing ostomy surgery | N.A. |
| Ayik C, 2020, Turkey, [27] | Retrospective study | Tot: 572 patients; M: 302 patients; F: 270 patients; Mean age: 59.15 ± 13.86 years | End colostomy: 253 patients (44.2%); Loop colostomy: 40 patients (7%); End ileostomy: 151 patients (26.4%); Loop ileostomy: 128 patients (22.4%) | N.A. | N.A. | Early PSCs: PICD: 181 patients (31.6%); - Late PSCs: PICD: 149 patients (26%) | N.A. | BMI > 24.9 kg/m2; Temporary ostomy; Ileostomy | Early period (<30 days after surgery): 56.5% of complications; -Late period (>30 days after surgery): 36.2% of complications | N.A. |
| Singh N, 2021, India, [33] | Prospective study | Tot: 36 patients; M: 28 patients; F: 8 patients; Age < 30: 19 patients; Age > 30: 17 patients | End Ileostomy: 13 patients; Loop Ileostomy: 23 patients | N.A. | N.A. | Peristomal irritation: 33 patients (91.7 %); Skin escoriation: 24 patients (66.7 %) | N.A. | N.A. | Early period (<30 days after surgery) | N.A. |
| Maeda S, 2021, Japan, [28] | Retrospective study | Tot: 185 patients; M: 131 patients (70.8%); F: 54 patients (29.2%); Mean age: 62 years (range: 27–83 years) | Loop Ileostomy: 185 patients (100%) | Rectal malignancies Adenocarcinoma: 174 patients (94.1%) | Skin disorders: 62 patients (33.5%) | N.A. | N.A. | Higher BMI (≥25.0 kg/m2); Lower ostomy height (<20 mm) | N.A. | Readmissions: 3 patients |
| He D, 2021, China, [21] | Retrospective study | Tot: 491 patients; M: 217 patients (65.96%); F: 112 patients (34.04%); Age ≤ 60: 171 patients (51.98%); Age > 60: 158 patients (48.02%) | Ileostomy | Colorectal cancer | N.A. | Peristomal dermatitis: 85 patients (17.31%) | N.A. | Diabetes; Female gender | Within one month after ileostomy. | N.A. |
| Fellows J, 2021, Multinational, [36] | Multinational survey | Tot: 5187 patients; M: 56%; F: 44%; More than 18 years of age. | Colostomy: 51%; Ileostomy: 33% | N.A. | PSCs rate: 88% | PSC with >1 or 1 symptoms/signs (e.g., pain, itching, burning): 78% | Self-report assessment: Peristomal skin with mild discoloration: 32%; Peristomal skin with medium discoloration: 16%; Peristomal skin with severe discoloration: 4% | N.A. | N.A. | N.A. |
| Pittmann J, 2022, US, [35] | Web-based survey | Tot: 202 patients; M: 144 patients; F: 46 patients; Mean age: 54.91 ± 14.52 years | Ileostomy: 89 patients (45.41%); Colostomy: 50 patients (25.51%); Multiple stomies: 13 patients (6.63%) | Cancer: 81 patients (46.55%); Ulcerative colitis: 39 patients (22.41%); Crohn disease: 23 patients (13.22%); Diverticulitis: 7 patients (4.02%); Trauma: 2 patients (1.15%); Other: 22 patients (12.64%) | N.A. | Peristomal skin irritation: 78% (n =135/173) | N.A. | N.A. | N.A. | N.A. |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Meisner, S.; Lehur, P.-A.; Moran, B.; Martins, L.; Jemec, G.B.E. Peristomal skin complications are common, expensive, and difficult to manage: A population based cost modeling study. PLoS ONE 2012, 7, e37813. [Google Scholar] [CrossRef] [PubMed]
- Persson, E.; Berndtsson, I.; Carlsson, E.; Hallén, A.-M.; Lindholm, E. Stoma-related complications and stoma size—A 2-year follow up. Color. Dis. 2010, 12, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Taneja, C.; Netsch, D.; Rolstad, B.S.; Inglese, G.; Eaves, D.; Oster, G. Risk and Economic Burden of Peristomal Skin Complications Following Ostomy Surgery. J. Wound Ostomy Cont. Nurs. 2019, 46, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Romão, M.; Figueira, D.; Galante, H.; Guerreiro, J.; Romano, S. Who are the ostomy patients and caregivers attending Portuguese community pharmacies? A cross-sectional study. BMC Health Serv. Res. 2020, 20, 914. [Google Scholar] [CrossRef] [PubMed]
- Menin, G.; Roveron, G.; Barbierato, M.; Peghetti, A.; Zanotti, R. Design and validation of a “Peristomal Lesion Scale” for peristomal skin assessment. Int. Wound J. 2019, 16, 433–441. [Google Scholar] [CrossRef]
- Ambe, P.C.; Kurz, N.R.; Nitschke, C.; Odeh, S.F.; Möslein, G.; Zirngibl, H. Intestinal ostomy: Classification, indications, ostomy care and complication management. Dtsch. Ärzteblatt Int. 2018, 115, 182–187. [Google Scholar] [CrossRef]
- Gálvez, A.M.; Sánchez, F.J.; Moreno, C.A.; Fernández, A.P.; García, R.B.; López, M.C.; Ramírez, M.B.; López, M.C.; Burrero, L.V.; Berja, P.J.; et al. Value-based healthcare in ostomies. Int. J. Environ. Res. Public Health 2020, 17, 5879. [Google Scholar] [CrossRef]
- Claessens, I.; Probert, R.; Tielemans, C.; Steen, A.; Nilsson, C.; Andersen, B.D.; Størling, Z.M. The ostomy life study: The everyday challenges faced by people living with a stoma in a snapshot. Gastrointest. Nurs. 2015, 13, 18–25. [Google Scholar] [CrossRef]
- Krishnamurty, D.; Blatnik, J.; Mutch, M. Stoma complications. Clin. Colon Rectal Surg. 2017, 30, 193–200. [Google Scholar] [CrossRef]
- Maglio, A.; Malvone, A.P.; Scaduto, V.; Brambilla, D.; Denti, F.C. The frequency of early stomal, peristomal and skin complications. Br. J. Nurs. 2021, 30, 1272–1276. [Google Scholar] [CrossRef]
- Husain, S.; Cataldo, T. Late stomal complications. Clin. Colon Rectal Surg. 2008, 21, 031–040. [Google Scholar] [CrossRef] [PubMed]
- Salvadalena, G.; Colwell, J.C.; Skountrianos, G.; Pittman, J. Lessons learned about peristomal skin complications: Secondary analysis of the ADVOCATE trial. J. Wound Ostomy Cont. Nurs. 2020, 47, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Taneja, C.; Netsch, D.; Rolstad, B.S.; Inglese, G.; Lamerato, L.; Oster, G. Clinical and economic burden of peristomal skin complications in patients with recent ostomies. J. Wound Ostomy Cont. Nurs. 2017, 44, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Steinhagen, E.; Colwell, J.; Cannon, L.M. Intestinal stomas—Postoperative stoma care and peristomal skin complications. Clin. Colon Rectal Surg. 2017, 30, 184–192. [Google Scholar] [CrossRef]
- Nybaek, H.; Jemec, G.; Jemec, G. Skin problems in stoma patients. J. Eur. Acad. Dermatol. Venereol. 2010, 24, 249–257. [Google Scholar] [CrossRef]
- Ustundag, H.; Gul, A.; Togluk, E. Assessment of peristomal skin complications in Turkish individuals with in intestinal stoma: A retrospective study. Int. J. Caring Sci. 2022, 15, 627–632. Available online: http://www.internationaljournalofcaringsciences.org/docs/64.pp_627_632-ustundag.pdf. (accessed on 3 October 2022).
- Nybaek, H.; Knudsen, D.B.; Laursen, T.N.; Karlsmark, T.; Jemec, G.B. Quality of life assessment among patients with peristomal skin disease. Eur. J. Gastroenterol. Hepatol. 2010, 22, 139–143. [Google Scholar] [CrossRef]
- Nichols, T.R.; Inglese, G.W. The burden of peristomal skin complications on an ostomy population as assessed by health utility and the physical component summary of the SF-36v2 ®. Value Health 2018, 21, 89–94. [Google Scholar] [CrossRef]
- Colwell, J.C.; Pittman, J.; Raizman, R.; Salvadalena, G. A randomized controlled trial determining variances in ostomy skin conditions and the economic impact (ADVOCATE trial). J. Wound Ostomy Cont. Nurs. 2018, 45, 37–42. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- He, D.; Liang, W.; Yao, Q.; Zhao, J.; Liu, R.; Chen, G.; Wang, H.; Ye, X.; Huang, R. The effect of stoma education class on peristomal dermatitis in colorectal cancer patients with defunctioning ileostomy—A retrospective study of 491 patients. Transl. Cancer Res. 2021, 10, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Baykara, Z.G.; Demir, S.G.; Karadag, A.; Harputlu, D.; Kahraman, A.; Karadag, S.; Hin, A.O.; Togluk, E.; Altinsoy, M.; Erdem, S.; et al. A multicenter, retrospective study to evaluate the effect of preoperative stoma site marking on stomal and peristomal complications. Ostomy Wound Manag. 2014, 60, 16–26. [Google Scholar]
- Sarkut, P.; Dundar, H.Z.; Tirnova, I.; Ozturk, E.; Yilmazlar, T. Is stoma care effective in terms of morbidity in complicated ileostomies? Int. J. Gen. Med. 2015, 8, 243–246. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cressey, B.D.; Belum, V.R.; Scheinman, P.; Silvestri, D.; McEntee, N.; Livingston, V.; Lacouture, M.E.; Zippin, J.H. Stoma care products represent a common and previously underreported source of peristomal contact dermatitis. Contact Dermat. 2017, 76, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Nagano, M.; Ogata, Y.; Ikeda, M.; Tsukada, K.; Tokunaga, K.; Iida, S. Peristomal moisture-associated skin damage and independence in pouching system changes in persons with new fecal ostomies. J. Wound Ostomy Cont. Nurs. 2019, 46, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Carbonell, B.B.; Treter, C.; Staccini, G.; MajnoHurst, P.; Christoforidis, D. Early peristomal complications: Detailed analysis, classification and predictive risk factors. Ann Ital Chir. 2020, 91, 69–73. [Google Scholar] [PubMed]
- Ayik, C.; Özden, D.; Cenan, D. Ostomy complications, risk factors, and applied nursing care: A retrospective, descriptive study. Wound Manag. Prev. 2020, 66, 20–30. [Google Scholar] [CrossRef]
- Maeda, S.; Ouchi, A.; Komori, K.; Kinoshita, T.; Oshiro, T.; Ito, S.; Abe, T.; Shimizu, Y. Risk factors for peristomal skin disorders associated with temporary ileostomy construction. Surg. Today 2021, 51, 1152–1157. [Google Scholar] [CrossRef]
- Salvadalena, G.D. The incidence of stoma and peristomal complications during the first 3 months after ostomy creation. J. Wound Ostomy Cont. Nurs. 2013, 40, 400–406. [Google Scholar] [CrossRef]
- Lindholm, E.; Persson, E.; Carlsson, E.; Hallén, A.-M.; Fingren, J.; Berndtsson, I. Ostomy-related complications after emergent abdominal surgery: A 2-year follow-up study. J. Wound Ostomy Cont. Nurs. 2013, 40, 603–610. [Google Scholar] [CrossRef]
- Carlsson, E.; Fingren, J.; Hallén, A.-M.; Petersén, C.; Lindholm, E. The prevalence of ostomy-related complications 1 year after ostomy surgery: A prospective, descriptive, clinical study. Ostomy Wound Manag. 2016, 62, 34–48. [Google Scholar]
- Harputlu, D.; Özsoy, S.A. A prospective, experimental study to assess the effectiveness of home care nursing on the healing of peristomal skin complications and quality of life. Ostomy Wound Manag. 2018, 64, 18–30. [Google Scholar] [CrossRef]
- Singh, N.; Bhatia, P.K.; Goyal, K.S.; Pundeer, S.; Kallem, S.R.; Gandhi, H.; Devi, D. Prospective study of clinical profile and early complications of ileostomy. J. Evol. Med. Dent. Sci. 2021, 10, 694–700. [Google Scholar] [CrossRef]
- Nichols, T. Health utility, social interactivity, and peristomal skin status: A cross-sectional study. J. Wound Ostomy Cont. Nurs. 2018, 45, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Pittman, J.; Colwell, J.; Mulekar, M.S. Ostomy complications and quality of life of ostomy support belt/garment wearers: A web-based survey. J. Wound Ostomy Cont. Nurs. 2022, 49, 60–68. [Google Scholar] [CrossRef]
- Fellows, J.; Voegeli, D.; Håkan-Bloch, J.; Herschend, N.O.; Størling, Z. Multinational survey on living with an ostomy: Prevalence and impact of peristomal skin complications. Br. J. Nurs. 2021, 30, S22–S30. [Google Scholar] [CrossRef]
- Voegeli, D.; Karlsmark, T.; Eddes, E.H.; Hansen, H.D.; Zeeberg, R.; Håkan-Bloch, J.; Hedegaard, C.J. Factors influencing the incidence of peristomal skin complications: Evidence from a multinational survey on living with a stoma. Gastrointest. Nurs. 2020, 18, S31–S38. [Google Scholar] [CrossRef]
- Malik, T.; Lee, M.J.; Harikrishnan, A.B. The incidence of stoma related morbidity—A systematic review of randomised controlled trials. Ann. R Coll. Surg. Engl. 2018, 100, 501–508. [Google Scholar] [CrossRef]
- Bloemen, A.; Aarts, F.; Bouvy, N.; Nijhuis, P. Evaluation of a new elastic ostomy appliance to decrease skin complications: Results of a pilot study. Wound Manag. Prev. 2020, 66, 30–36. [Google Scholar] [CrossRef]
- Martins, L.; Tavernelli, K.; Sansom, W.; Dahl, K.; Claessens, I.; Porrett, T.; Andersen, B.D. Strategies to reduce treatment costs of peristomal skin complications. Br. J. Nurs. 2012, 21, 1312–1315. [Google Scholar] [CrossRef]
- Burch, J. Care of patients with peristomal skin complications. Nurs. Stand. 2014, 28, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Szewczyk, M.T.; Majewska, G.; Cabral, M.V.; Hölzel-Piontek, K. The effects of using a moldable skin barrier on peristomal skin condition in persons with an ostomy: Results of a prospective, observational, multinational study. Ostomy Wound Manag. 2014, 60, 16–26. [Google Scholar]
- Colwell, J.C.; McNichol, L.; Boarini, J. North America wound, ostomy, and continence and enterostomal therapy nurses current ostomy care practice related to peristomal skin issues. J. Wound Ostomy Cont. Nurs. 2017, 44, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Salomé, G.M.; de Almeida, S.A.; Mendes, B.; de Carvalho, M.R.F.; Junior, M.R.M. Assessment of subjective well-being and quality of life in patients with intestinal stoma. J. Coloproctol. 2015, 35, 168–174. [Google Scholar] [CrossRef][Green Version]
- Ratliff, C.R.; Goldberg, M.; Jaszarowski, K.; McNichol, L.; Pittman, J.; Gray, M. Peristomal Skin Health: A WOCN Society Consensus Conference. J. Wound Ostomy Cont. Nurs. 2021, 48, 219–231. [Google Scholar] [CrossRef] [PubMed]
- Foà, C.; Bisi, E.; Calcagni, A.; Goldoni, A.; Moscatelli, M.P.; Pellicani, V.; Uccelli, S.; Sarli, L.; Artioli, G. Infectious risk in ostomy patient: The role of nursing competence. Acta Bio Medica Atenei Parm. 2019, 90, 53. [Google Scholar]
- Morss-Walton, P.C.; Yi, J.Z.; Gunning, M.; McGee, J.S. Ostomy 101 for dermatologists: Managing peristomal skin diseases. Dermatol. Ther. 2021, 34, e15069. [Google Scholar] [CrossRef]
- Murken, D.R.; Bleier, J.I.S. Ostomy-related complications. Clin. Colon Rectal Surg. 2019, 32, 176–182. [Google Scholar] [CrossRef]
- Jonkers, H.A.F.; Draaisma, W.A.; Roskott, A.M.; van Overbeeke, A.J.; Broeders, I.A.M.J.; Consten, E.C.J. Early complications after stoma formation: A prospective cohort study in 100 patients with 1-year follow-up. Int. J. Color. Dis. 2012, 27, 1095–1099. [Google Scholar] [CrossRef]
- LeBlanc, K.; Whiteley, I.; McNichol, L.; Salvadalena, G.; Gray, M. Peristomal medical adhesive-related skin injury: Results of an international consensus meeting. J. Wound Ostomy Cont. Nurs. 2019, 46, 125–136. [Google Scholar] [CrossRef]
- White, P.; Evans, M. Clinical governance for ostomates at risk of peristomal skin complications. Br. J. Nurs. 2019, 28, S24–S32. [Google Scholar] [CrossRef] [PubMed]
- European Commission. Expert panel on Effective Ways of Investing in Health (EXPH). Defining Value in “Value-Based Healthcare”. 2019. Available online: https://health.ec.europa.eu/system/files/2019-11/024_defining-value-vbhc_en_0.pdf (accessed on 24 October 2022).
- Brown, P.; Zhou, Y.; RELISH Consortium. Large expert-curated database for benchmarking document similarity detection in biomedical literature search. Database 2019, 2019, baz085. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
D’Ambrosio, F.; Pappalardo, C.; Scardigno, A.; Maida, A.; Ricciardi, R.; Calabrò, G.E. Peristomal Skin Complications in Ileostomy and Colostomy Patients: What We Need to Know from a Public Health Perspective. Int. J. Environ. Res. Public Health 2023, 20, 79. https://doi.org/10.3390/ijerph20010079
D’Ambrosio F, Pappalardo C, Scardigno A, Maida A, Ricciardi R, Calabrò GE. Peristomal Skin Complications in Ileostomy and Colostomy Patients: What We Need to Know from a Public Health Perspective. International Journal of Environmental Research and Public Health. 2023; 20(1):79. https://doi.org/10.3390/ijerph20010079
Chicago/Turabian StyleD’Ambrosio, Floriana, Ciro Pappalardo, Anna Scardigno, Ada Maida, Roberto Ricciardi, and Giovanna Elisa Calabrò. 2023. "Peristomal Skin Complications in Ileostomy and Colostomy Patients: What We Need to Know from a Public Health Perspective" International Journal of Environmental Research and Public Health 20, no. 1: 79. https://doi.org/10.3390/ijerph20010079
APA StyleD’Ambrosio, F., Pappalardo, C., Scardigno, A., Maida, A., Ricciardi, R., & Calabrò, G. E. (2023). Peristomal Skin Complications in Ileostomy and Colostomy Patients: What We Need to Know from a Public Health Perspective. International Journal of Environmental Research and Public Health, 20(1), 79. https://doi.org/10.3390/ijerph20010079





