Qualitative Evaluation of YouTube Videos on Dental Fear, Anxiety and Phobia
Abstract
1. Introduction
2. Materials and Methods
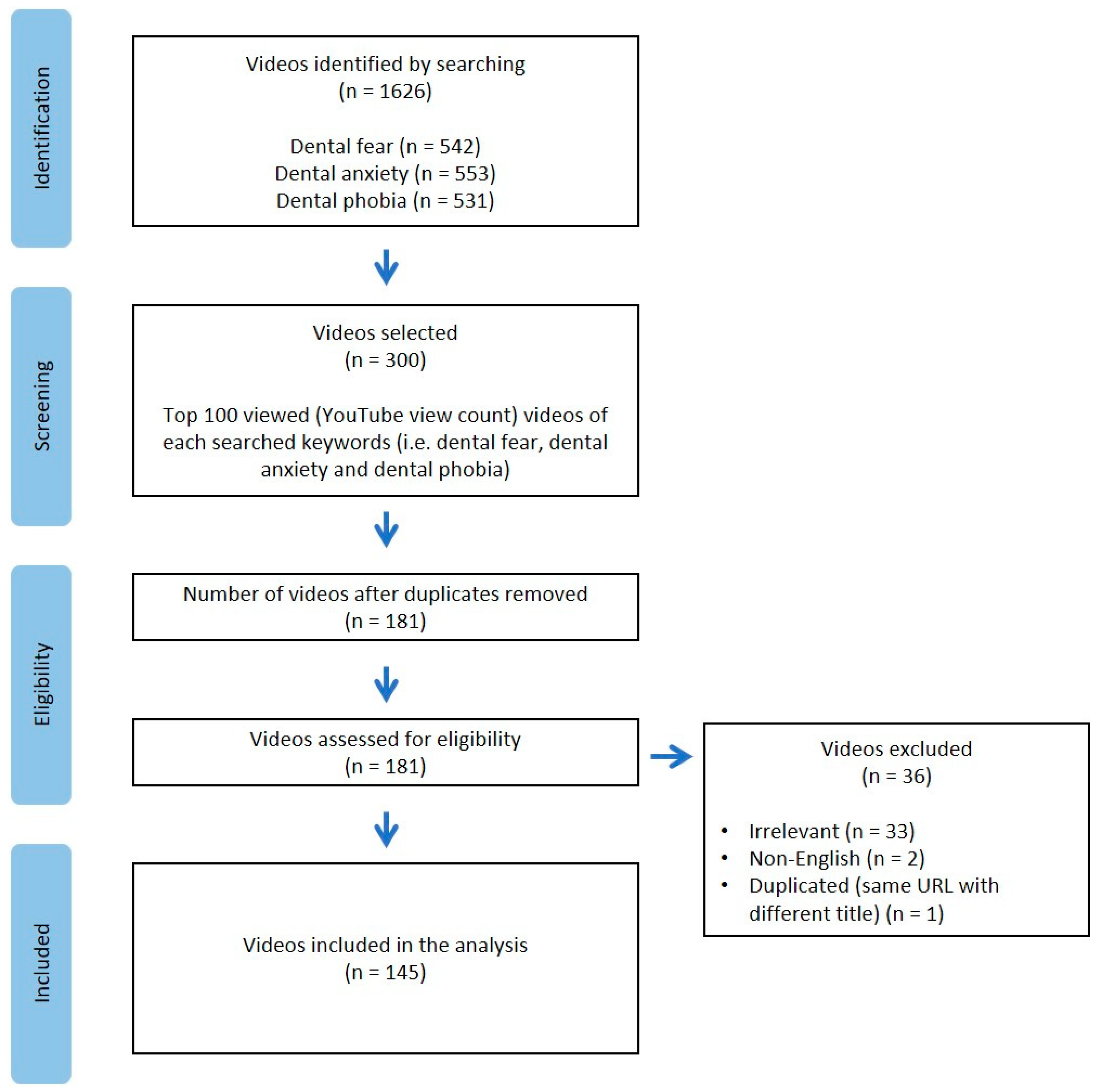
2.1. Information Sources, Search Strategy, and Eligibility Criteria
2.2. Video Selection
2.3. Data Extraction
2.4. Statistical Analysis
3. Results
3.1. Video Metric
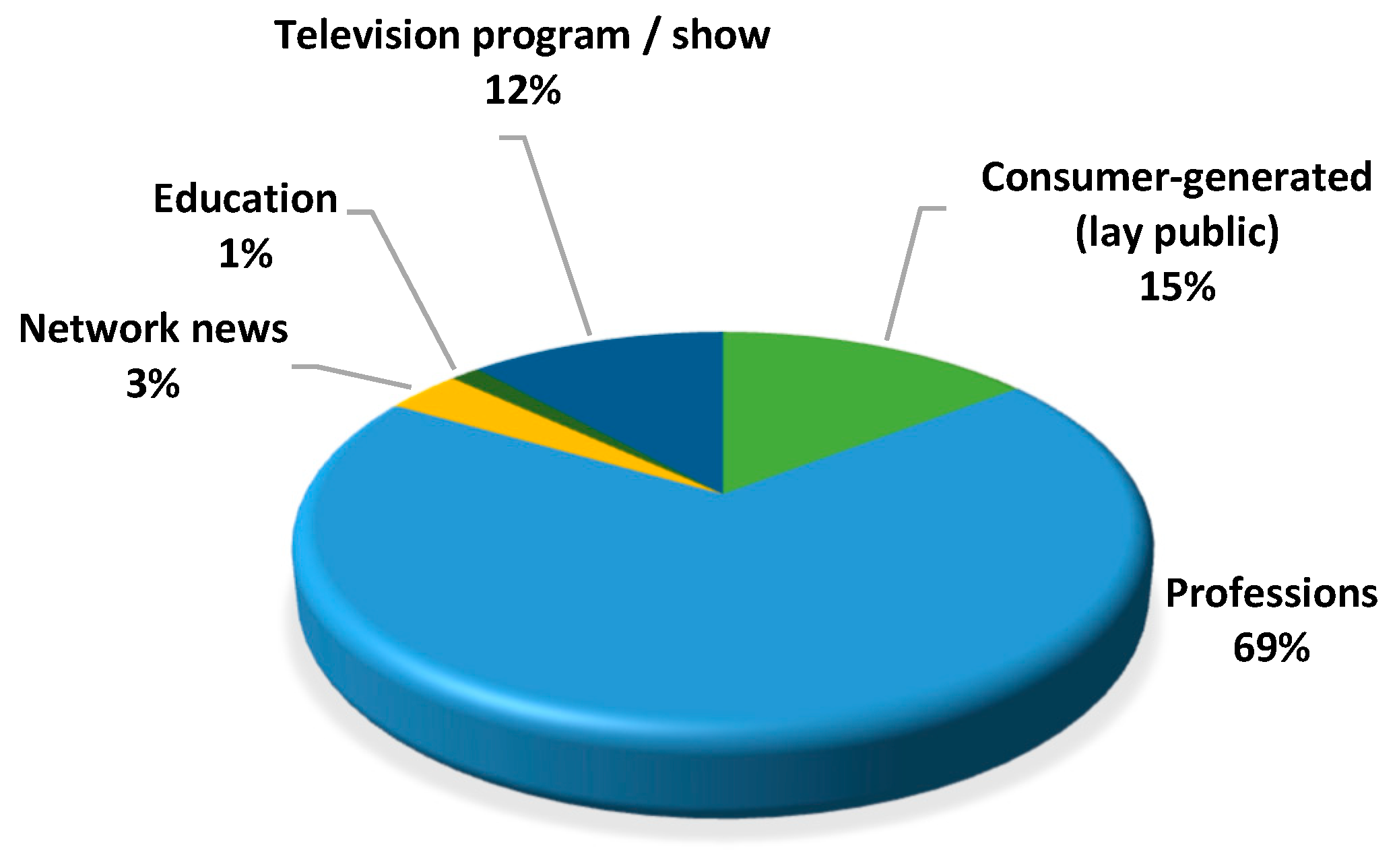
3.2. Sources of Video
3.3. Video Content Related to Dental Fear, Dental Anxiety, and Dental Phobia
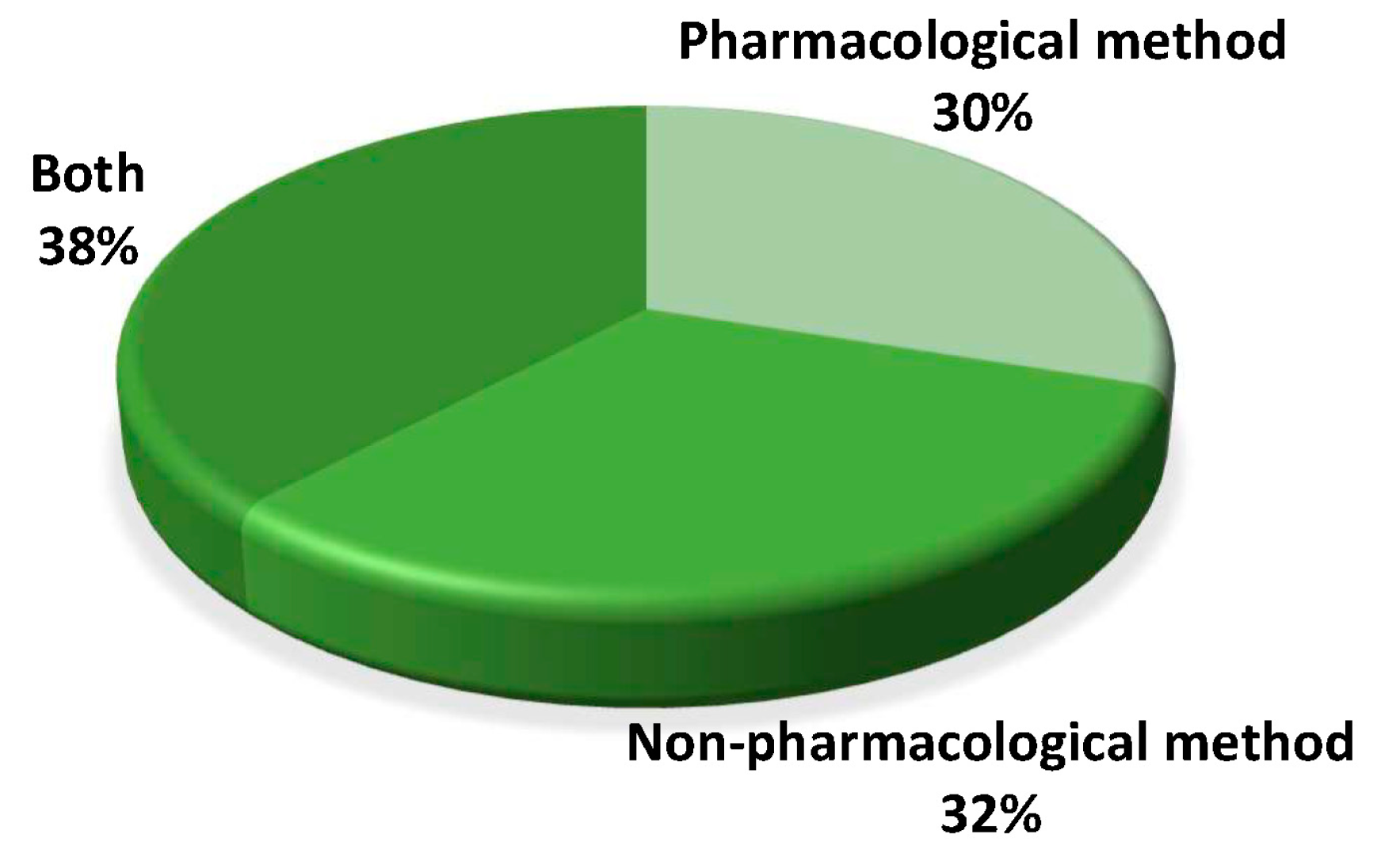
3.4. Video Content Related to Management of Dental Fear, Dental Anxiety, and Dental Phobia
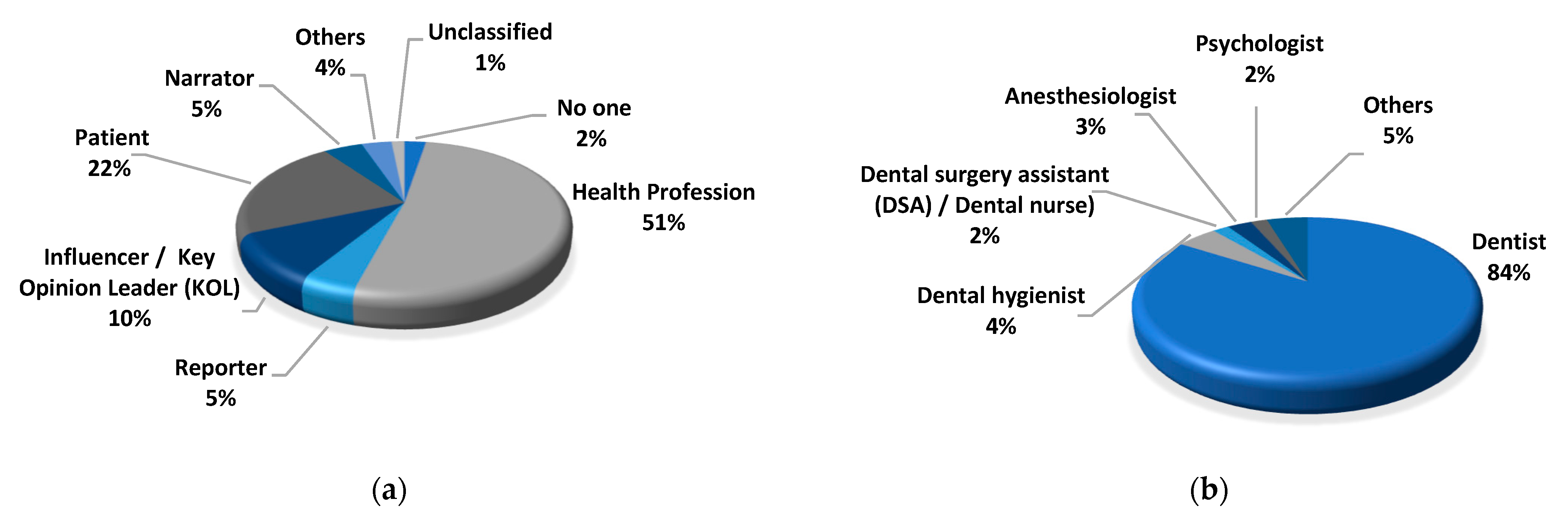
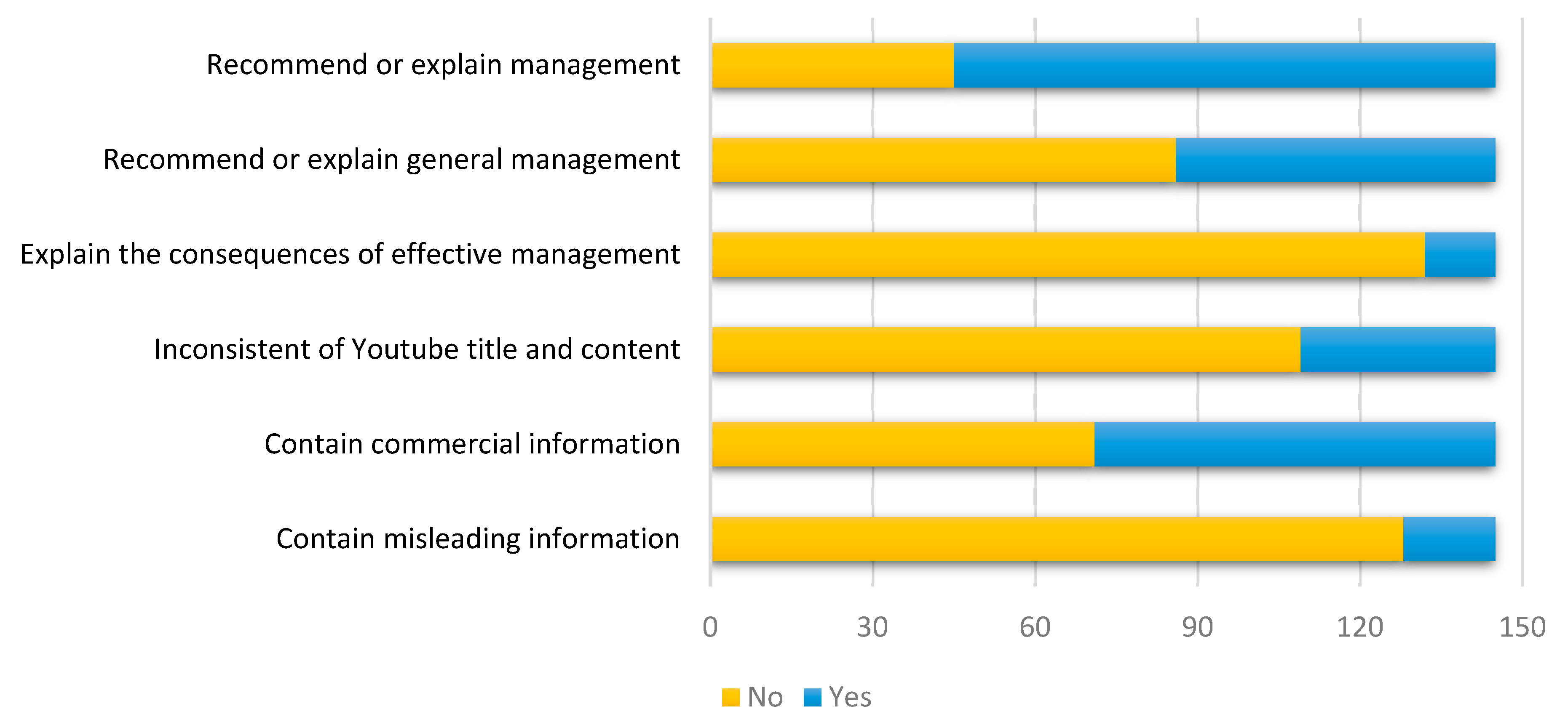
3.5. Features of Video Presentation Format and Content
3.6. Video Statistics
4. Discussion
- Misinformation: People with dental fear or anxiety being exposed to videos of dental procedures would be beneficial.Truth: Not everyone would have their dental fear or anxiety alleviated after watching such videos. See [33]. Some might become more anxious.
- Misinformation: All psychological and non-pharmacological treatments were grouped as “cognitive-behavioral interventions” (CBI).Truth: CBI is a psychological intervention.
- Misinformation: Dental fear and dental phobia are the same thing.Truth: They differ in severity and phobia leads to avoidance behavior.
- Misinformation: “Specific dental phobia”.Truth: Such a term has yet to be established in the literature.
- Misinformation: A video title said there were new drugs that could help dental anxiety.Truth: The drug actually replaced injection (helped with anesthesia) without targeting anxiety.
- Misinformation: Dental phobia is actually a diagnosis in the Diagnostic and Statistical Manual (DSM).Truth: Some people believed that dental phobia could be an example of specific phobia listed in DSM, but dental phobia itself is not listed in DSM.
- Misinformation: Laughing gas is not sedation.Truth: Laughing gas (nitrous oxide) is used for inhalation sedation.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beaton, L.; Freeman, R.; Humphris, G. Why are people afraid of the dentist? Observations and explanations. Med. Princ. Pract. 2014, 23, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Bastani, P.; Manchery, N.; Samadbeik, M.; Ha, D.H.; Do, L.G. Digital Health in Children’s Oral and Dental Health: An Overview and a Bibliometric Analysis. Children 2022, 9, 1039. [Google Scholar] [CrossRef] [PubMed]
- Grisolia, B.M.; Dos Santos, A.P.P.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef]
- Silveira, E.R.; Cademartori, M.G.; Schuch, H.S.; Armfield, J.A.; Demarco, F.F. Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. J. Dent. 2021, 108, 103632. [Google Scholar] [CrossRef] [PubMed]
- Locker, D. Psychosocial consequences of dental fear and anxiety. Community Dent. Oral Epidemiol. 2003, 31, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Zinke, A.; Hannig, C.; Berth, H. Comparing oral health in patients with different levels of dental anxiety. Head Face Med. 2018, 14, 25. [Google Scholar] [CrossRef] [PubMed]
- McGrath, C.; Bedi, R. The association between dental anxiety and oral health-related quality of life in Britain. Community Dent. Oral Epidemiol. 2004, 32, 67–72. [Google Scholar] [CrossRef]
- Svensson, L.; Hakeberg, M.; Wide, U. Dental pain and oral health-related quality of life in individuals with severe dental anxiety. Acta Odontol. Scand. 2018, 76, 401–406. [Google Scholar] [CrossRef]
- Armfield, J.M. How do we measure dental fear and what are we measuring anyway? Oral Health Prev. Dent. 2010, 8, 107–115. [Google Scholar]
- Gujjar, K.R.; Van Wijk, A.; Kumar, R.; De Jongh, A. Are technology-based interventions effective in reducing dental anxiety in children and adults? A systematic review. J. Evid. Based Dent. Pract. 2019, 19, 140–155. [Google Scholar] [CrossRef]
- Hoffmann, B.; Erwood, K.; Ncomanzi, S.; Fischer, V.; O’Brien, D.; Lee, A. Management strategies for adult patients with dental anxiety in the dental clinic: A systematic review. Aust. Dent. J. 2022, 67, S3–S13. [Google Scholar] [CrossRef] [PubMed]
- Wong, N.S.M.; Yeung, A.W.K.; Li, K.Y.; Mcgrath, C.P.; Leung, Y.Y. Non-pharmacological interventions for reducing fear and anxiety in patients undergoing third molar extraction under local anesthesia: Systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2022, 19, 11162. [Google Scholar] [CrossRef] [PubMed]
- Freeman, R. Barriers to accessing dental care: Patient factor. Br. Dent. J. 1999, 187, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Oosterink, F.M.; De Jongh, A.; Hoogstraten, J. Prevalence of dental fear and phobia relative to other fear and phobia subtypes. Eur. J. Oral Sci. 2009, 117, 135–143. [Google Scholar] [CrossRef]
- Lueken, U.; Kruschwitz, J.D.; Muehlhan, M.; Siegert, J.; Hoyer, J.; Wittchen, H.-U. How specific is specific phobia? Different neural response patterns in two subtypes of specific phobia. Neuroimage 2011, 56, 363–372. [Google Scholar] [CrossRef]
- Van Houtem, C.; Aartman, I.; Boomsma, D.; Ligthart, L.; Visscher, C.; De Jongh, A. Is dental phobia a blood-injection-injury phobia? Depress. Anxiety 2014, 31, 1026–1034. [Google Scholar] [CrossRef]
- Bürklein, S.; Brodowski, C.; Fliegel, E.; Jöhren, H.P.; Enkling, N. Recognizing and differentiating dental anxiety from dental phobia in adults: A systematic review based on the German guideline” Dental anxiety in adults”. Quintessence Int. 2021, 52, 360–373. [Google Scholar]
- Strieder, A.P.; Oliveira, T.M.; Rios, D.; Cruvinel, A.F.P.; Cruvinel, T. Is there a relationship of negative oral health beliefs with dental fear and anxiety regarding diverse dental patient groups? A systematic review and meta-analysis. Clin. Oral Investig. 2019, 23, 3613–3621. [Google Scholar] [CrossRef]
- Madathil, K.C.; Rivera-Rodriguez, A.J.; Greenstein, J.S.; Gramopadhye, A.K. Healthcare information on YouTube: A systematic review. Health Inform. J. 2015, 21, 173–194. [Google Scholar] [CrossRef]
- Li, H.O.-Y.; Bailey, A.; Huynh, D.; Chan, J. YouTube as a source of information on COVID-19: A pandemic of misinformation? BMJ Glob. Health 2020, 5, e002604. [Google Scholar] [CrossRef]
- Abukaraky, A.; Hamdan, A.A.; Ameera, M.-N.; Nasief, M.; Hassona, Y. Quality of YouTube TM videos on dental implants. Med. Oral Patol. Oral Cir. Bucal. 2018, 23, e463–e468. [Google Scholar] [CrossRef] [PubMed]
- Kılınç, D.D.; Sayar, G. Assessment of reliability of YouTube videos on orthodontics. Turk. J. Orthod. 2019, 32, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Hamzah, S.; Yiu, C.K.Y.; McGrath, C.; King, N.M. Dental fear and anxiety in children and adolescents: Qualitative study using YouTube. J. Med. Internet Res. 2013, 15, e2290. [Google Scholar] [CrossRef]
- Perez, A.; Green, J.L.; Starchuk, C.; Senior, A.; Compton, S.M.; Gaudet-Amigo, G.; Lai, H.; Linke, B.; Patterson, S. Dental faculty and student views of didactic and clinical assessment: A qualitative description study. Eur. J. Dent. Educ. 2020, 24, 628–636. [Google Scholar] [CrossRef] [PubMed]
- Debreceny, R.S.; Wang, T.; Zhou, M. Research in social media: Data sources and methodologies. J. Inf. Syst. 2019, 33, 1–28. [Google Scholar] [CrossRef]
- Burghardt, S.; Koranyi, S.; Magnucki, G.; Strauss, B.; Rosendahl, J. Non-pharmacological interventions for reducing mental distress in patients undergoing dental procedures: Systematic review and meta-analysis. J. Dent. 2018, 69, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Wide Boman, U.; Carlsson, V.; Westin, M.; Hakeberg, M. Psychological treatment of dental anxiety among adults: A systematic review. Eur. J. Oral Sci. 2013, 121, 225–234. [Google Scholar] [CrossRef]
- Cai, H.; Xi, P.; Zhong, L.; Chen, J.; Liang, X. Efficacy of aromatherapy on dental anxiety: A systematic review of randomised and quasi-randomised controlled trials. Oral Dis. 2021, 27, 829–847. [Google Scholar] [CrossRef]
- Charnock, D.; Shepperd, S.; Needham, G.; Gann, R. DISCERN: An instrument for judging the quality of written consumer health information on treatment choices. J. Epidemiol. Community Health 1999, 53, 105–111. [Google Scholar] [CrossRef]
- Silberg, W.M.; Lundberg, G.D.; Musacchio, R.A. Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor—Let the reader and viewer beware. JAMA 1997, 277, 1244–1245. [Google Scholar] [CrossRef]
- Azer, S.A. Are DISCERN and JAMA suitable instruments for assessing YouTube videos on thyroid cancer? Methodological concerns. J. Cancer Educ. 2020, 35, 1267–1277. [Google Scholar] [CrossRef] [PubMed]
- Drozd, B.; Couvillon, E.; Suarez, A. Medical YouTube videos and methods of evaluation: Literature review. JMIR Med. Educ. 2018, 4, e8527. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.K.; Chau, A.W.; Leung, W.K. The effect of pre-operative information in relieving anxiety in oral surgery patients. Community Dent. Oral Epidemiol. 2004, 32, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Kiley, R. Does the internet harm health? Some evidence exists that the internet does harm health. BMJ Br. Med. J. 2002, 324, 238–239. [Google Scholar] [CrossRef]
- Neuman, W.R.; Guggenheim, L. The evolution of media effects theory: A six-stage model of cumulative research. Commun. Theory 2011, 21, 169–196. [Google Scholar] [CrossRef]
- Burns, L.E.; Abbassi, E.; Qian, X.; Mecham, A.; Simeteys, P.; Mays, K.A. YouTube use among dental students for learning clinical procedures: A multi-institutional study. J. Dent. Educ. 2020, 84, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Fu, M.W.; Kalaichelvan, A.; Liebman, L.S.; Burns, L.E. Exploring predoctoral dental student use of YouTube as a learning tool for clinical endodontic procedures. J. Dent. Educ. 2022, 86, 726–735. [Google Scholar] [CrossRef]


| Metric | Mean (SD) | Min; Max | n (%) |
|---|---|---|---|
| View count | 141,025.68 (1,352,257.81) | 740; 16,394,106 | |
| ≤1000 | 5 (3.5%) | ||
| 1001–10,000 | 87 (60.0%) | ||
| 10,001–100,000 | 45 (31.0%) | ||
| 100,001–1,000,000 | 7 (4.8%) | ||
| 1,000,001–10,000,000 | 0 (0%) | ||
| >10,000,000 | 1 (0.7%) | ||
| Like count | 1253.8 (8707.04) | 0; 95,000 | |
| ≤100 | 104 (71.7%) | ||
| 101–1000 | 32 (22.1%) | ||
| 1001–10,000 | 6 (4.1%) | ||
| >10,000 | 3 (2.1%) | ||
| Comment count | 164.72 (1246.61) | 0; 14,052 | |
| ≤100 | 118 (81.4%) | ||
| 101–1000 | 9 (6.2%) | ||
| 1001–10,000 | 2 (1.4%) | ||
| >10,000 | 1 (0.7%) | ||
| Function turned off | 15 (10.3%) | ||
| Channel subscriber count | 427,695.93 (3,174,516.33) | 0; 36,600,000 | |
| ≤100 | 30 (20.7%) | ||
| 101–1000 | 26 (17.9%) | ||
| 1001–10,000 | 33 (22.7%) | ||
| 10,001–100,000 | 32 (22.1%) | ||
| 100,001–1,000,000 | 20 (13.8%) | ||
| 1,000,001–10,000,000 | 3 (2.1%) | ||
| >10,000,000 | 1 (0.7%) | ||
| Duration (s) | 398 (503.6) | 15; 2423 | |
| ≤100 | 35 (24.1%) | ||
| 101–1000 | 95 (65.5%) | ||
| >1000 | 15 (10.4%) |
| Metric | Like Count | Comment Count | Duration (s) | Channel Subscriber Count |
|---|---|---|---|---|
| View count | 0.916 ** (p < 0.001) | 0.987 ** (p < 0.001) | −0.049 (p = 0.560) | −0.004 (p = 0.965) |
| Like count | 0.910 (p < 0.001) | −0.059 (p = 0.483) | 0.017 (p = 0.843) | |
| Comment count | −0.035 (p = 0.694) | 0.021 (p = 0.817) | ||
| Duration (s) | 0.050 (p = 0.554) |
| No. of Videos (n) | % (of 145 Videos) | |
|---|---|---|
| Prevalence | ||
| Yes | 19 | 13.1% |
| No | 126 | 86.9% |
| Description | ||
| Yes | 11 | 7.6% |
| No | 134 | 92.4% |
| Diagnostic criteria | ||
| Yes | 1 | 0.7% |
| No | 144 | 99.3% |
| Symptoms | ||
| Yes | 37 | 25.5% |
| No | 108 | 74.5% |
| Etiology | ||
| Yes | 63 | 43.5% |
| No | 82 | 56.5% |
| Effect | ||
| Yes | 37 | 25.5% |
| No | 108 | 74.5% |
| Categories | Themes | Examples |
|---|---|---|
| Cognitive Factors | ||
| Perceived lack of control | “Most adults also fear a lack of control” “I don’t like the feeling of being out of control” “The dentist made me feel powerless” “I feel helpless in the dental chair” | |
| Behavioral Factors | ||
| Conditioned by direct trauma | “Unpleasant childhood experience in the dental chair” “Traumatic experience” “When the dentist leans the chair back, some bad experiences popped up” “When I walk to the dental office, the noise of the drill throws me off and it’s scary” | |
| Conditioned by modeling | “My sister was crying on the dental chair” “They may learn the behavior from observing their parents” | |
| Conditioned by verbal instruction | “Heard a story about other people’s bad experiences” “My parents told me that my uncle died at the dentist. He was given some anesthetic and he never woke back up” “There were plenty of absolute horror stories tell you how everything went wrong and that doesn’t exactly encourage you to make an appointment” |
| Categories | Themes | Examples a |
|---|---|---|
| Physiological Responses | ||
| Heart rate increase | “My chest feels lie it closes up” “Pounding in my chest” “Racing heartbeat” | |
| Blood pressure increase | “Their blood pressure will increase” | |
| Breathing rate increase | “Breath heavily” “Feelings of suffocation” “I need to work out my breathing and calm myself” | |
| Sweating | “I was sweating” “Sweaty palms” | |
| Shaky | “I was shaky when doing so” | |
| Stomachache | “Pit in my stomach” “Pitting of stomach that butterfly kind of feeling” | |
| Nausea | “Feeling nauseous” “Urge to gag or vomit before dental treatment” | |
| Dizziness | “Feel dizzy” | |
| Behavioral Responses | ||
| Avoidance of dental visit | “They always schedule appointment but not show up” “I avoid call to the dentist, it was stressful for me” “Delay going to the dentist” “They don’t often present to a dentist until they have a problem” | |
| Search for alternative | “Taking over-the counter pain medications to manage the pain” | |
| Hesitation | “I stand in front of the door of the dental office but not going in” “Debating whether or not I should head back” | |
| Being sleepless | “I’m not able to sleep” “Sleep badly” | |
| Nightmares | “I have nightmares from the dentist” | |
| Extreme behaviors | “I grabbed the dentist hand to stop him” “I wasn’t flossing every day, because I found that even flossing made me kind of look in my mouth and think about my dental state” “Refuse to be reclined in the dental chair” | |
| Crying | “I sit in the car and cry, because being there made me so afraid” | |
| Cognitive Responses | ||
| Irrational thought | “I found that even flossing made me think about the dentist, I know it is irrational” “I was feeling vulnerable and thinking I’m going to die” |
| Categories | Stimuli |
|---|---|
| Dangerous/life-threatening/body injury stimuli | Needle Sound of the drill Injections Pain Numb Blood |
| Neutral stimuli | Dental chair Smells of dental office Dental equipment Dentist (white coat syndrome) |
| Psychosocial factors | Unpleasant childhood experience Stories about other people’s bad experiences Embarrassment Being judged by the dentist (Judgment) Fear of unknown/uncertainty/lack of control Anxiety issue from parents |
| Type of Pharmacological Method | n | % (of 145) |
|---|---|---|
| Oral medication | 27 | 18.6 |
| Intravenous sedation | 27 | 18.6 |
| Inhalation sedation | 24 | 16.6 |
| Local anesthesia | 12 | 8.3 |
| Just sedation (did not mention which type of sedation) | 12 | 8.3 |
| General anesthesia | 11 | 7.6 |
| Supplements | 2 | 1.4 |
| Types of Non-pharmacological Method a | n | % (of 145) |
|---|---|---|
| Distraction | 51 | 35.2 |
| Listen to music (n = 24) | ||
| Watch TV or video (n = 19) | ||
| Virtual reality (n = 5) | ||
| Listen to audio book (n = 1) | ||
| Listen to a podcast (n = 1) | ||
| Play games with smart glasses (n = 1) | ||
| Relaxation | 16 | 11.0 |
| Breathing (n = 15) | ||
| Muscle (n = 1) | ||
| Hypnosis | 6 | 4.1 |
| Meditation | 6 | 4.1 |
| Aromatherapy/essential oil | 5 | 3.4 |
| Enhanced information | 4 | 2.8 |
| Desensitization | 2 | 1.4 |
| General clinical practice | 72 | 49.7 |
| Signaling (n = 21) | ||
| Tell-show-do (n = 12) | ||
| Sensory-adapted dental environment (n = 11) | ||
| With family member/friend accompany (n = 8) | ||
| Positive reinforcement (n = 7) | ||
| Body contact (n = 6) | ||
| Comfort object (n = 5) | ||
| Wearing dark glasses (n = 2) | ||
| Others b | 7 | 4.8 |
| Categories | Examples |
|---|---|
| For patients | Communicate openly (figure out what specifically triggered fear) Schedule appointment at an earlier time Avoid researching information on the internet |
| For dental practitioners | Communication (figure out what specifically triggered fear) Building a trusting relationship Show compassion/empathy/reassurance Discuss with patients before treatment Acknowledge patient’s anxiety Allow patients to ask questions Make general body language Make eye contact Active listening |
| Presentation Format of Videos | No. of Videos (n) | % (of 145 Videos) |
|---|---|---|
| Audio | ||
| Yes | 145 | 100% |
| No | 0 | 0% |
| Verbal explanation | ||
| Yes | 139 | 95.9% |
| No | 6 | 4.1% |
| Text assistance | ||
| Yes | 36 | 24.8% |
| No | 108 | 74.5% |
| Have patient demonstration of dental fear anxiety phobia management | ||
| Yes | 28 | 19.3% |
| No | 117 | 80.7% |
| Groups of Video | |||
|---|---|---|---|
| With Misleading Information (%) | Without Misleading Information (%) | p-Value | |
| Source of video | 0.158 | ||
| Lay public | 23.8 | 76.2 | |
| Professions a | 9.0 | 91.0 | |
| Others b | 12.5 | 87.5 | |
| Informant | 0.684 | ||
| Health professions | 12.5 | 87.5 | |
| Non-health professions | 10.2 | 89.8 | |
| Number of views | 0.004 | ||
| High view | 19.4 | 80.6 | |
| Low view c | 4.1 | 95.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wong, N.S.M.; Yeung, A.W.K.; McGrath, C.P.; Leung, Y.Y. Qualitative Evaluation of YouTube Videos on Dental Fear, Anxiety and Phobia. Int. J. Environ. Res. Public Health 2023, 20, 750. https://doi.org/10.3390/ijerph20010750
Wong NSM, Yeung AWK, McGrath CP, Leung YY. Qualitative Evaluation of YouTube Videos on Dental Fear, Anxiety and Phobia. International Journal of Environmental Research and Public Health. 2023; 20(1):750. https://doi.org/10.3390/ijerph20010750
Chicago/Turabian StyleWong, Natalie Sui Miu, Andy Wai Kan Yeung, Colman Patrick McGrath, and Yiu Yan Leung. 2023. "Qualitative Evaluation of YouTube Videos on Dental Fear, Anxiety and Phobia" International Journal of Environmental Research and Public Health 20, no. 1: 750. https://doi.org/10.3390/ijerph20010750
APA StyleWong, N. S. M., Yeung, A. W. K., McGrath, C. P., & Leung, Y. Y. (2023). Qualitative Evaluation of YouTube Videos on Dental Fear, Anxiety and Phobia. International Journal of Environmental Research and Public Health, 20(1), 750. https://doi.org/10.3390/ijerph20010750







