The Clinical Benefits of a Dynamic vs. Static Component as Part of a Comprehensive Warm-Up for Recreational Sports Players with Clinical Histories of Hamstring Injuries: A Randomized Clinical Trial
Abstract
1. Introduction
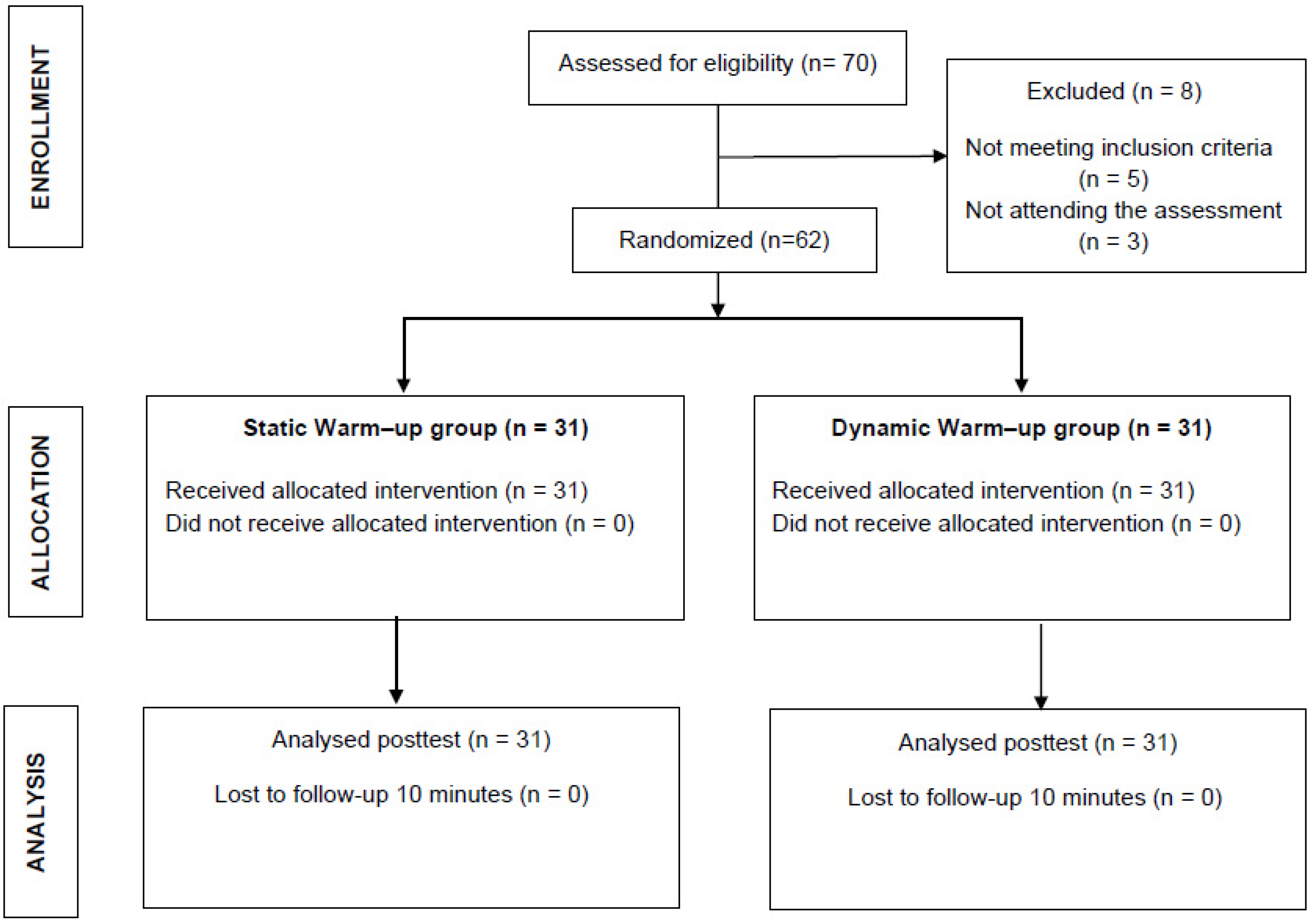
2. Materials and Methods
2.1. Design and Setting
2.2. Participants
2.3. Intervention
2.4. Outcomes
2.4.1. Primary Outcomes
2.4.2. Secondary Outcome
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
4. Discussion
4.1. Limitations
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gogte, K.; Srivastav, P.; Miyaru, G.B. Effect of Passive, Active and Combined Warm up on Lower Limb Muscle Performance and Dynamic Stability in Recreational Sports Players. J. Clin. Diagn. Res. 2017, 11, YC05–YC08. [Google Scholar] [CrossRef] [PubMed]
- Hedrick, A. Physiological responses to warm-up. J. Strength Cond. Res. 1992, 14, 25–27. [Google Scholar]
- O’Sullivan, K.; Murray, E.; Sainsbury, D. The effect of warm-up, static stretching and dynamic stretching on hamstring flexibility in previously injured subjects. BMC Musculoskelet. Disord. 2009, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Magalhães, T.; Ribeiro, F.; Pinheiro, A.; Oliveira, J. Warming-up before sporting activity improves knee position sense. Phy. Ther. Sport 2010, 11, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Ayala, F.; Calderon-Lopez, A.; Delgado-Gosálbez, J.C.; Parra-Sanchez, S.; Pomares-Noguera, C.; Hernandez-Sanchez, S.; Lopez-Valenciano, A.; Croix, M.D.S. Acute Effects of Three Neuromuscular Warm-Up Strategies on Several Physical Performance Measures in Football Players. PLoS ONE 2017, 12, e0169660. [Google Scholar] [CrossRef] [PubMed]
- Nouni-Garcia, R.; Carratala-Munuera, C.; Orozco-Beltran, D.; Lopez-Pineda, A.; Asensio-Garcia, M.R.; Gil-Guillen, V.F. Clinical benefit of the FIFA 11 programme for the prevention of hamstring and lateral ankle ligament injuries among amateur soccer players. Inj. Prev. 2018, 24, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Malanga, G.; Yan, N.; Stark, J. Mechanisms and efficacy of heat and cold therapies for musculoskeletal injury. Postgrad. Med. 2015, 127, 57–65. [Google Scholar] [CrossRef]
- Cosgray, N.; Lawrance, S.E.; Mestrich, J.D.; Martin, S.E.; Whalen, R.L. Effect of Heat Modalities on Hamstring Length: A Comparison of Pneumatherm, Moist Heat Pack, and a Control. J. Orthop. Sports Phys. Ther. 2004, 34, 377–384. [Google Scholar] [CrossRef]
- Nuzzo, J.L.; Barry, B.K.; Gandevia, S.C.; Taylor, J.L. Acute strength training increases responses to stimulation of corticospinal axons. Med. Sci. Sports Exerc. 2016, 48, 139–150. [Google Scholar] [CrossRef]
- Blazevich, A.J.; Gill, N.D.; Kvorning, T.; Kay, A.D.; Goh, A.; Hilton, B.; Drinkwater, E.J.; Behm, D.G. No Effect of Muscle Stretching within a Full, Dynamic Warm-up on Athletic Performance. Med. Sci. Sports Exerc. 2018, 50, 1258–1266. [Google Scholar] [CrossRef]
- Petersen, J.; Hölmich, P. Evidence based prevention of hamstring injuries in sport. Br. J. Sports Med. 2005, 39, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Woods, C.; Hawkins, R.D.; Maltby, S.; Hulse, M.; Thomas, A.; Hodson, A. The Football Association Medical Research Programme: An audit of injuries in professional football--analysis of hamstring injuries. Br. J. Sports Med. 2004, 38, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Van Mechelen, W. Prevention of running injuries by warm-up, cool-down, and stretching exercises. Am. J. Sports Med. 1993, 21, 711–719. [Google Scholar] [CrossRef]
- Reid, J.C.; Greene, R.; Young, J.D.; Hodgson, D.D.; Blazevich, A.J.; Behm, D.G. The effects of different durations of static stretching within a comprehensive warm-up on voluntary and evoked contractile properties. Eur. J. Appl. Physiol. 2018, 118, 1427–1445. [Google Scholar] [CrossRef] [PubMed]
- Mueller-Wohlfahrt, H.W.; Haensel, L.; Mithoefer, K.; Ekstrand, J.; English, B.; McNally, S. Terminology and classification of muscle injuries in sport: The Munich consensus statement. Br. J. Sports Med. 2013, 47, 342–350. [Google Scholar] [CrossRef]
- Behm, D.G.; Blazevich, A.J.; Kay, A.D.; McHugh, M. Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: A systematic review. Appl. Physiol. Nutr. Metab. 2016, 41, 1–11. [Google Scholar] [CrossRef]
- De Ridder, R.; De Blaiser, C.; Verrelst, R.; De Saer, R.; Desmet, A.; Schuermans, J. Neurodynamic sliders promote flexibility in tight hamstring syndrome. Eur. J. Sports Sci. 2020, 20, 973–980. [Google Scholar] [CrossRef]
- Ramírez-Vélez, R.; García Sánchez, A.; Martínez Betancourt, C.; Galeano, C.P.; Ortega, J.; Alban, C.L.; Zúñiga, R.A. Efectos de dos métodos de termoterapia sobre la respuesta vascular aguda y parámetros hemodinámicos en un grupo de sujetos sanos. Radiología 2012, 54, 513–519. [Google Scholar] [CrossRef]
- Salgado, E.; Ribeiro, F.; Oliveira, J. Joint-position sense is altered by football pre-participation warm-up exercise and match induced fatigue. Knee 2015, 22, 243–248. [Google Scholar] [CrossRef]
- Gajdosik, R.L.; Lusin, G. Reliability of an active knee extension test. Phys. Ther. 1983, 63, 1085–1088. [Google Scholar] [CrossRef]
- Ferreira, E.A.; Duarte, M.; Maldonado, E.P.; Burke, T.N.; Marques, A.P. Postural assessment software (PAS/SAPO): Validation and reliabiliy. Clinics 2010, 65, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Turner, J.A.; Romano, J.M.; Fisher, L.D. Comparative reliability and validity of chronic pain intensity measures. Pain 1999, 83, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Vanderweeën, L.; Oostendorp, R.A.; Vaes, P.; Duquet, W. Pressure algometry in manual therapy. Man. Ther. 1996, 1, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Chesterton, L.S.; Sim, J.; Wright, C.C.; Foster, N.E. Interrater reliability of algometry in measuring pressure pain thersholds in healthy humans, using multiple raters. Clin. J. Pain 2007, 23, 760–766. [Google Scholar] [CrossRef]
- Simons, D.G.; Travell, J.C.; Simons, L.S. Travell and Simons’ Myo- fascial Pain and Dysfunction: The Trigger Point Manual; Williams & Wilkins: Baltimore, MD, USA, 1999; Volume 1. [Google Scholar]
- McCray, R.; Patton, N. Pain Relief at Trigger Points: A Comparison of Moist Heat and Shortwave Diathermy. J. Orthop. Sports Phys. Ther. 1984, 5, 175–178. [Google Scholar] [CrossRef]
- Springer, S.; Kelman, D.; Brand, M.; Gottlieb, U. Knee Position Sense: Does Time Interval Target Angle Affect Position Accuracy? J. Phys. Ther. Sci 2017, 29, 1760–1765. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Science, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Heiderscheit, B.C.; Serry, M.A.; Silder, A.; Chumanov, E.S.; Thelen, D.G. Hamstring strain injuries: Recommendations for diagnosis, rehabilitation and injury prevention. J. Orthop. Sports Phys. Ther. 2010, 40, 67–81. [Google Scholar] [CrossRef]
- Cheng, A.J.; Willis, S.J.; Zinner, C.; Chaillou, T.; Ivarsson, N.; Ortenblad, N. Post-exercise recovery of contractile function and endurance in humans and mice is accelerated by heating and slowed by cooling skeletal muscle. J. Physiol. 2017, 595, 7413–7426. [Google Scholar] [CrossRef]
- Nakano, J.; Yamabayashi, C.; Scott, A.; Reid, W.D. The effect of heat applied with stretch to increase range of motion: A systematic review. Phys. Ther. Sport 2012, 13, 180–188. [Google Scholar] [CrossRef]
- Ostrowski, J.; Collin Herb, C.; Scifers, J.; Gonzalez, T.; Jennings, A.; Breton, D. Comparison of muscle temperatura increase produced by moist hot pack and thermoStim Probe. J. Sport Rehabil. 2019, 28, 459–463. [Google Scholar] [CrossRef]
- Sawyer, P.; Uhl, T.; Mattacola, C.; Johnson, D.; Yates, J. Effects of Moist Heat on Hamstring Flexibility and Muscle Temperature. J. Strength Cond. Res. 2003, 17, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Rosario, J.L.; Foletto, A. Comparative study of stretching modalities in healthy women: Heating and application time. J. Bodyw. Mov. Ther. 2015, 19, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Funk, D.; Swank, A.; Adams, K.; Treolo, D. Efficacy of Moist Heat Pack Application Over Static Stretching on Hamstring Flexibility. J. Strength Cond. Res. 2001, 15, 123–126. [Google Scholar] [PubMed]
- Olivencia, O.; Godinez, J.M.; Dages, J.; Duda, C.; Kaplan, K.; Kolber, M.J. The reliability and minimal detectable change of the ely and active knee extension tests. Int. J. Sports Phys. Ther. 2020, 15, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Shamsi, M.; Mirzaei, M.; Khabiri, S. Universal goniometer and electrogoniometer intra-examiner reliability in measuring the knee range of motion during active knee extension test in patients with chronic low back pain with short hamstring muscle. BMC Sports Sci. Med. Rehabil. 2019, 11, 4. [Google Scholar] [CrossRef]
- Boyd, B.S.; Wanek, L.; Gray, A.T.; Topp, K.S. Mechanosensitivity of the Lower Extremity Nervous System During Straight-Leg Raise Neurodynamic Testing in Healthy Individuals. J. Orthop. Sports Phys. Ther. 2009, 39, 780–790. [Google Scholar] [CrossRef]
- Hatano, G.; Suzuki, S.; Matsuo, S.; Kataura, S.; Yokoi, K.; Fukaya, T.; Fujiwara, M.; Asai, Y.; Iwata, M. Hamstring Stiffness Returns More Rapidly After Static Stretching Than Range of Motion, Stretch Tolerance, and Isometric Peak Torque. J. Sport Rehabil. 2019, 28, 325–331. [Google Scholar] [CrossRef]
- Kouzaki, K.; Nakazato, K.; Mizuno, M.; Yonechi, T.; Higo, Y.; Kubo, Y.; Kono, T.; Hiranuma, K. Sciatic Nerve Conductivity is impaired by hamstring strain injuries. Int. J. Sports Med. 2017, 38, 803–808. [Google Scholar] [CrossRef]
- Wang, Y.; Li, S.; Zhang, Y.; Chen, Y.; Yan, F.; Han, L.; Ma, Y. Heat and cold therapy reduce pain in patients with delayed onset muscle soreness: A systematic review and meta-analysis of 32 randomized controlled trials. Phys. Ther. Sport 2021, 48, 177–187. [Google Scholar] [CrossRef]
- Vaegter, H.B.; Dørge, D.B.; Schmidt, K.S.; Jensen, A.H.; Graven-Nielsen, T. Test-Retest Reliabilty of Exercise-Induced Hypoalgesia After Aerobic Exercise. Pain Med. 2018, 19, 2212–2222. [Google Scholar] [CrossRef]
- Jiang, Y.P.; Li, J.; Li, J. Effects of intermittent versus continuous cold and heat therapy in patients after mandible osteotomy. Chin. J. Nurs. 2013, 48, 777–778. [Google Scholar]
- Daneshjoo, A.; Mokhtar, A.H.; Rahnama, N.; Yusof, A. The effects of comprehensive warm up programs on propioception, static and dynamic balance on male soccer players. PLoS ONE 2012, 7, e51568. [Google Scholar] [CrossRef]
- Walsh, G.S. Effect of static and dynamic muscle stretching as part of warm up procedures on knee joint proprioception and strength. Hum. Mov. Sci. 2017, 55, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Proske, U. Exercise, fatigue and proprioception: A retrospective. Exp. Brain Res. 2019, 237, 2447–2459. [Google Scholar] [CrossRef] [PubMed]


| Total (n = 62) | SW (n = 31) | DW (n = 31) | p-Value | |
|---|---|---|---|---|
| Age | 21.1 ± 2.03; 21 [3] | 21.1 ± 2.26; 21 [4] | 21.1 ± 2.12; 21 [3] | 0.853 * |
| Gender (Male/Female) | 52 (84%)/10 (18%) | 25 (81%)/6 (19%) | 27 (87%)/4 (13%) | 0.49 † |
| Lower limb dominance (right/left) | 59(95%)/3 (5%) | 29 (94%)/2 (6%) | 30 (97%)/1 (3%) | 0.96 † |
| Height (cm) | 176 ± 0.09; 175 [0.08] | 173 ± 0,07; 173 [0.07] | 178 ± 0.10; 176 [0.15] | 0.189 * |
| Weight (kg) | 75.91 ± 17.04; 73.5 [15.50] | 77.50 ± 21.33; 71 [13.50] | 74.32 ± 11.60; 76 [12.50] | 0.648 * |
| BMI (kg/cm2) | 24.56 ± 5.06; 23.72 [2.75] | 25.69 ± 6.63; 23.48 [4.87] | 23.43 ± 2.43; 23.75 [2.62] | 0.339 * |
| RoM (°) | 44.36 ± 8.51; 45.9 [10.13] | 45.33 ± 8.96; 46.84 [10.89] | 43.38 ± 8.0; 45.32 [9.59] | 0.371 * |
| Stretching Tolerance (VAS 0–100 mm) | 51.8 ± 15.2; 55 [2] | 50 ± 16.9; 50 [20] | 53.5 ± 13.3; 60 [20] | 0.363 * |
| PPT (kg/cm2) | 5.25 ± 1.71; 5.22 [1.97] | 5.6 ± 1.9; 5.5 [1.95] | 4.9 ± 1.36; 4.75 [2.10] | 0.116 * |
| JPS (°) | 6.7 ± 3.73; 6.88 [5.78] | 6.8 ± 4.2; 6.66 [5.74] | 6.7 ± 3.2; 7.3 [5.9] | 0.899 * |
| Sport practice (h/week) | 9.71 ± 3.92; 8 [6] | 9.33 ± 3.88; 8 [6] | 10.10 ± 4.02; 10 [7] | 0.517 * |
| Sport Discipline Running (%) | 26/62 (42%) | 12/26 (46%) | 14/26 (54%) | 0.89 † |
| Cycling (%) | 16/62 (26%) | 9/16 (56%) | 7/16 (44%) | 0.78 † |
| Football (%) | 18/62 (29%) | 8/18 (45%) | 10/18 (55%) | 0.98 † |
| Tennis (%) | 2/62 (3%) | 1/2 (3%) | 1/2 (3%) | 0.99 † |
| Group | Baseline–Immediately After | Immediately After–10 min Follow-Up | Baseline–10 min Follow-Up | |||
|---|---|---|---|---|---|---|
| Baseline | Immediately After | 10 min Follow-Up | Within-Group Mean Changes | Within-Group Mean Changes | Within-Group Mean Changes | |
| RoM (°) | ||||||
| SW | 45.3 ± 8.96 | 46.9 ± 9.67 | 47.4 ± 9.41 | 1.6 [0.2–3.4] (−) | 0.5 [−1.6–0.8] (−) | 2.1 [0.4–3.7] * (0.23) |
| DW | 43.4 ± 8.01 | 44.8 ± 9.2 | 43.7 ± 7.40 | 1.4 [0.4–3.3] (−) | 1.1 [0.1–2.3] (−) | 0.3 [−2.4–1.8] (−) |
| Stretching Tolerance (VAS 0–100 mm) | ||||||
| SW | 50.0 ± 16.9 | 36.1 ± 17.0 | 42.6 ± 18.4 | 13.9 [8.9–18.8] ** (0.82) | 6.5 [1.8–11.0] * (0.36) | 7.4 [2.3–12.5] * (0.41) |
| DW | 53.5 ± 13.3 | 38.7 ± 19.1 | 44.8 ± 16.7 | 14.8 [9.4–20.2] ** (0.9) | 6.1 [1.8–10.4] * (0.34) | 8.7 [3.2–14.1] * (0.57) |
| PPT (kg/cm2) | ||||||
| SW | 5.6 ± 1.9 | 6.7 ± 1.81 | 6.2 ± 1.84 | 1.1 [0.6–1.5] ** (0.6) | 0.5 [0.08–0.9] * (0.27) | 0.6 [0.1–1.1] * (0.32) |
| DW | 4.9 ± 1.36 | 6.6 ± 1.95 | 5.9 ± 1.40 | 1.7 [1.2–2.1] ** (1.01) | 0.7 [0.1–1.3] * (0.41) | 1 [0.5–1.4] ** (0.72) |
| JPS (°) | ||||||
| SW | 6.8 ± 4.22 | 5.5 ± 2.87 | 5.8 ± 3.64 | 1.3 [−0.5–3.0] (−) | 0.3 [−1.6–1.0] (−) | 1 [0.6–2.6] (−) |
| DW | 6.7 ± 3.2 | 5.2 ± 2.3 | 5.7 ± 2.73 | −1.5 [−0.3–2.6] * (0.53) | 0.5 [−1.6–0.6] (−) | 1 [0.4–2.3] (−) |
| Immediately After | Mean Differences Between-Groups | 10 min Follow-Up | Mean Differences Between-Groups | ||
|---|---|---|---|---|---|
| RoM (°) | SW | 46.9 ± 9.67 | 2.1 [−2.4–6.7] | 47.4 ± 9.41 | 3.7 [0.6–7.9] |
| DW | 44.8 ± 9.2 | 43.7 ± 7.40 | |||
| Stretching Tolerance (VAS 0–100 mm) | SW | 36.1 ± 17.0 | 2.6 [−11.7–6.6] | 42.6 ± 18.4 | 2.2 [−11.2–6.7] |
| DW | 38.7 ± 19.1 | 44.8 ± 16.7 | |||
| PPT (kg/cm2) | SW | 6.7 ± 1.81 | 0.1 [−0.8–1.0] | 6.2 ± 1.84 | 0.3 [−0.5–1.1] |
| DW | 6.6 ± 1.95 | 5.9 ± 1.40 | |||
| JPS (°) | SW | 5.5 ± 2.87 | 0.3 [−1.05–1.6] | 5.8 ± 3.64 | 0.1 [−1.5–1.7] |
| DW | 5.2 ± 2.3 | 5.7 ± 2.73 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutierrez-Coronado, J.; López-Bueno, L.; Cardero-Durán, M.d.l.A.; Albornoz-Cabello, M.; Toledo-Marhuenda, J.V.; Hernández-Sánchez, S.; Dueñas, L.; Marques-Sule, E.; Morral, A.; Espejo-Antúnez, L. The Clinical Benefits of a Dynamic vs. Static Component as Part of a Comprehensive Warm-Up for Recreational Sports Players with Clinical Histories of Hamstring Injuries: A Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2023, 20, 744. https://doi.org/10.3390/ijerph20010744
Gutierrez-Coronado J, López-Bueno L, Cardero-Durán MdlA, Albornoz-Cabello M, Toledo-Marhuenda JV, Hernández-Sánchez S, Dueñas L, Marques-Sule E, Morral A, Espejo-Antúnez L. The Clinical Benefits of a Dynamic vs. Static Component as Part of a Comprehensive Warm-Up for Recreational Sports Players with Clinical Histories of Hamstring Injuries: A Randomized Clinical Trial. International Journal of Environmental Research and Public Health. 2023; 20(1):744. https://doi.org/10.3390/ijerph20010744
Chicago/Turabian StyleGutierrez-Coronado, Javier, Laura López-Bueno, María de los Angeles Cardero-Durán, Manuel Albornoz-Cabello, Jose Vicente Toledo-Marhuenda, Sergio Hernández-Sánchez, Lirios Dueñas, Elena Marques-Sule, Antoni Morral, and Luis Espejo-Antúnez. 2023. "The Clinical Benefits of a Dynamic vs. Static Component as Part of a Comprehensive Warm-Up for Recreational Sports Players with Clinical Histories of Hamstring Injuries: A Randomized Clinical Trial" International Journal of Environmental Research and Public Health 20, no. 1: 744. https://doi.org/10.3390/ijerph20010744
APA StyleGutierrez-Coronado, J., López-Bueno, L., Cardero-Durán, M. d. l. A., Albornoz-Cabello, M., Toledo-Marhuenda, J. V., Hernández-Sánchez, S., Dueñas, L., Marques-Sule, E., Morral, A., & Espejo-Antúnez, L. (2023). The Clinical Benefits of a Dynamic vs. Static Component as Part of a Comprehensive Warm-Up for Recreational Sports Players with Clinical Histories of Hamstring Injuries: A Randomized Clinical Trial. International Journal of Environmental Research and Public Health, 20(1), 744. https://doi.org/10.3390/ijerph20010744








