Clinical Outcomes Associated with SARS-CoV-2 Co-Infection with Rhinovirus and Adenovirus in Adults—A Retrospective Matched Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Setting
2.2. Matching Process
2.3. Clinical Outcome Assessment
2.4. Baseline Laboratory Biomarker Assessment
2.5. Statistical Analysis
3. Results
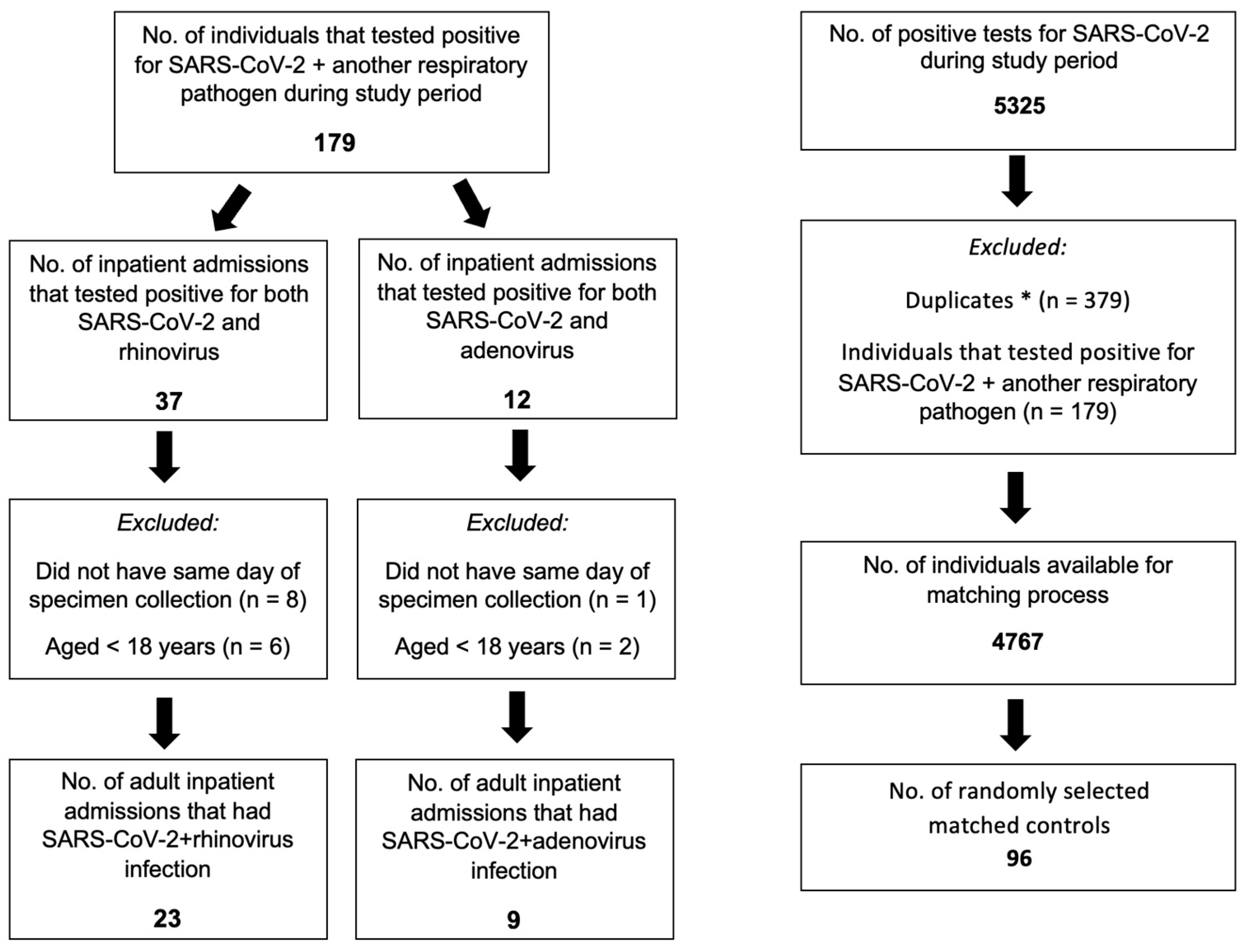
3.1. Study Disposition
3.2. Baseline Characteristics of Patients with SARS-CoV-2 + Rhinovirus Co-Infection
3.3. Baseline Characteristics of Patients with SARS-CoV-2 + Adenovirus Co-Infection
3.4. Clinical Outcomes for Patients with SARS-CoV-2 + Rhinovirus Co-Infection
3.5. Laboratory Biomarkers for Patients with SARS-CoV-2 + Rhinovirus Co-Infection
3.6. Clinical Outcomes for Patients with SARS-CoV-2 + Adenovirus Co-Infection
3.7. Laboratory Biomarkers for Patients with SARS-CoV-2 + Adenovirus Co-Infection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Olsen, S.J.; Winn, A.K.; Budd, A.P.; Prill, M.M.; Steel, J.; Midgley, C.M.; Kniss, K.; Burns, E.; Rowe, T.; Foust, A.; et al. Changes in Influenza and Other Respiratory Virus Activity During the COVID-19 Pandemic—United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1013–1019. [Google Scholar] [CrossRef] [PubMed]
- Burki, T.K. Double threat of COVID-19 and influenza. Lancet Respir. Med. 2020, 8, e97. [Google Scholar] [CrossRef] [PubMed]
- Aghbash, P.S.; Eslami, N.; Shirvaliloo, M.; Baghi, H.B. Viral coinfections in COVID-19. J. Med. Virol. 2021, 93, 5310–5322. [Google Scholar] [CrossRef]
- Gomez, G.B.; Mahé, C.; Chaves, S.S. Uncertain effects of the pandemic on respiratory viruses. Science 2021, 372, 1043–1044. [Google Scholar] [CrossRef] [PubMed]
- Noh, J.Y.; Seong, H.; Yoon, J.G.; Song, J.Y.; Cheong, H.J.; Kim, W.J. Social Distancing against COVID-19: Implication for the Control of Influenza. J. Korean Med. Sci. 2020, 35, e182. [Google Scholar] [CrossRef]
- Kim, S.; Park, J.O.; Lee, H.A.; Park, H.A.; Lee, C.A.; Wang, S.J.; Jung, E.J. Unintended beneficial effects of COVID-19 on influenza-associated emergency department use in Korea. Am. J. Emerg. Med. 2022, 59, 1–8. [Google Scholar] [CrossRef]
- Tang, H.J.; Lai, C.C.; Chao, C.M. The Collateral Effect of COVID-19 on the Epidemiology of Airborne/Droplet-Transmitted Notifiable Infectious Diseases in Taiwan. Antibiotics 2022, 11, 478. [Google Scholar] [CrossRef]
- Rubin, R. Influenza’s Unprecedented Low Profile During COVID-19 Pandemic Leaves Experts Wondering What This Flu Season Has in Store. JAMA 2021, 326, 899. [Google Scholar] [CrossRef]
- Kim, M.C.; Kweon, O.J.; Lim, Y.K.; Choi, S.H.; Chung, J.W.; Lee, M.K. Impact of social distancing on the spread of common respiratory viruses during the coronavirus disease outbreak. Chan RWY, editor. PLoS ONE 2021, 16, e0252963. [Google Scholar]
- Alosaimi, B.; Naeem, A.; Hamed, M.E.; Alkadi, H.S.; Alanazi, T.; Al Rehily, S.S.; Almutairi, A.Z.; Zafar, A. Influenza co-infection associated with severity and mortality in COVID-19 patients. Virol. J. 2021, 18, 127. [Google Scholar] [CrossRef]
- Zhu, X.; Ge, Y.; Wu, T.; Zhao, K.; Chen, Y.; Wu, B.; Zhu, F.; Zhu, B.; Cui, L. Co-infection with respiratory pathogens among COVID-2019 cases. Virus Res. 2020, 285, 198005. [Google Scholar] [CrossRef] [PubMed]
- Alosaimi, B.; Hamed, M.E.; Naeem, A.; Alsharef, A.A.; AlQahtani, S.Y.; AlDosari, K.M.; Alamri, A.A.; Al-Eisa, K.; Khojah, T.; Assiri, A.M.; et al. MERS-CoV infection is associated with downregulation of genes encoding Th1 and Th2 cytokines/chemokines and elevated inflammatory innate immune response in the lower respiratory tract. Cytokine 2020, 126, 154895. [Google Scholar] [CrossRef] [PubMed]
- Swets, M.C.; Russell, C.D.; Harrison, E.M.; Docherty, A.B.; Lone, N.; Girvan, M.; Hardwick, H.E.; Visser, L.G.; Openshaw, P.J.; Groeneveld, G.H.; et al. SARS-CoV-2 co-infection with influenza viruses, respiratory syncytial virus, or adenoviruses. Lancet 2022, 399, 1463–1464. [Google Scholar] [CrossRef]
- Stowe, J.; Tessier, E.; Zhao, H.; Guy, R.; Muller-Pebody, B.; Zambon, M.; Andrews, N.; Ramsay, M.; Lopez Bernal, J. Interactions between SARS-CoV-2 and Influenza and the impact of coinfection on disease severity: A test negative design. Int. J. Epidemiol. 2021, 50, 1124–1133. [Google Scholar] [CrossRef] [PubMed]
- Nowak, M.D.; Sordillo, E.M.; Gitman, M.R.; Paniz Mondolfi, A.E. Coinfection in SARS-CoV-2 infected patients: Where are influenza virus and rhinovirus/enterovirus? J. Med. Virol. 2020, 92, 1699–1700. [Google Scholar] [CrossRef]
- Echenique, I.A.; Chan, P.A.; Chapin, K.C.; Andrea, S.B.; Fava, J.L.; Mermel, L.A. Clinical Characteristics and Outcomes in Hospitalized Patients with Respiratory Viral Co-Infection during the 2009 H1N1 Influenza Pandemic. Semple MG, editor. PLoS ONE 2013, 8, e60845. [Google Scholar] [CrossRef]
- Dadashi, M.; Khaleghnejad, S.; Elkhichi, P.A.; Goudarzi, M.; Goudarzi, H.; Taghavi, A.; Vaezjalali, M.; Hajikhani, B. COVID-19 and Influenza Co-infection: A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 681469. [Google Scholar] [CrossRef]
- Kim, E.H.; Nguyen, T.Q.; Casel, M.A.; Rollon, R.; Kim, S.M.; Kim, Y.I.; Yu, K.M.; Jang, S.G.; Yang, J.; Poo, H.; et al. Coinfection with SARS-CoV-2 and Influenza A Virus Increases Disease Severity and Impairs Neutralizing Antibody and CD4+ T Cell Responses. J. Virol. 2022, 96, e01873-21. [Google Scholar] [CrossRef]
- Wu, X.; Cai, Y.; Huang, X.; Yu, X.; Zhao, L.; Wang, F.; Li, Q.; Gu, S.; Xu, T.; Li, Y.; et al. Co-infection with SARS-CoV-2 and Influenza A Virus in Patient with Pneumonia, China. Emerg. Infect. Dis. 2020, 26, 1324–1326. [Google Scholar] [CrossRef]
- Yue, H.; Zhang, M.; Xing, L.; Wang, K.; Rao, X.; Liu, H.; Tian, J.; Zhou, P.; Deng, Y.; Shang, J. The epidemiology and clinical characteristics of co-infection of SARS-CoV-2 and influenza viruses in patients during COVID-19 outbreak. J. Med. Virol. 2020, 92, 2870–2873. [Google Scholar] [CrossRef]
- Cheng, Y.; Ma, J.; Wang, H.; Wang, X.; Hu, Z.; Li, H.; Zhang, H.; Liu, X. Co-infection of influenza A virus and SARS-CoV-2: A retrospective cohort study. J. Med. Virol. 2021, 93, 2947–2954. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.; Wang, H.; Su, Z.; Li, W.; Yang, D.; Deng, F.; Chen, J. Co-infection of SARS-CoV-2 and Influenza virus in Early Stage of the COVID-19 Epidemic in Wuhan, China. J. Infect. 2020, 81, e128–e129. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Chen, F.; Wu, K.; Wang, J.; Li, F.; Huang, S.; Lu, J.; Huang, J.; Liu, H.; Zhou, R.; et al. Clinical and virological impact of single and dual infections with influenza A (H1N1) and SARS-CoV-2 in adult inpatients. PLoS Negl. Trop. Dis. 2021, 15, e0009997. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.; Upadhyay, P.; Reddy, J.; Granger, J. SARS-CoV-2 respiratory co-infections: Incidence of viral and bacterial co-pathogens. Int. J. Infect. Dis. 2021, 105, 617–620. [Google Scholar] [CrossRef] [PubMed]
- Castillo, E.M.; Coyne, C.J.; Brennan, J.J.; Tomaszewski, C.A. Rates of coinfection with other respiratory pathogens in patients positive for coronavirus disease 2019 (COVID-19). J. Am. Coll. Emerg. Physicians Open 2020, 1, 592–596. [Google Scholar] [CrossRef]
- Kim, D.; Quinn, J.; Pinsky, B.; Shah, N.H.; Brown, I. Rates of Co-infection Between SARS-CoV-2 and Other Respiratory Pathogens. JAMA 2020, 323, 2085. [Google Scholar] [CrossRef]
- Fisher, R.A. Statistical Methods for Research Workers. In Breakthroughs in Statistics; Kotz, S., Johnson, N.L., Eds.; Springer Series in Statistics; Springer: New York, NY, USA, 1992; pp. 66–70. Available online: http://link.springer.com/10.1007/978-1-4612-4380-9_6 (accessed on 1 November 2022).
- Ho, D.E.; Imai, K.; King, G.; Stuart, E.A. MatchIt: Nonparametric Preprocessing for Parametric Causal Inference. J. Stat. Softw. 2011, 42, 1–28. Available online: http://www.jstatsoft.org/v42/i08/ (accessed on 1 November 2022). [CrossRef]
- R Core Team. R: A Langauge and Environment for Statistical Computing; R Studio for Statistical Computing: Vienna, Austria, 2022; Available online: https://www.R-project.org/ (accessed on 22 June 2022).
- Goka, E.; Vallely, P.; Mutton, K.; Klapper, P. Influenza A viruses dual and multiple infections with other respiratory viruses and risk of hospitalisation and mortality: Influenza A and respiratory viral co-infections. Influenza Other Respir. Viruses 2013, 7, 1079–1087. [Google Scholar] [CrossRef]
- Feldman, C.; Anderson, R. The role of co-infections and secondary infections in patients with COVID-19. Pneumonia 2021, 13, 5. [Google Scholar] [CrossRef]
- Chekuri, S.; Szymczak, W.A.; Goldstein, D.Y.; Nori, P.; Marrero Rolon, R.; Spund, B.; Singh-Tan, S.; Mohrmann, L.; Assa, A.; Southern, W.N.; et al. SARS-CoV-2 coinfection with additional respiratory virus does not predict severe disease: A retrospective cohort study. J. Antimicrob. Chemother. 2021, 76 (Suppl. S3), iii12–iii19. [Google Scholar] [CrossRef]
- Samprathi, M.; Jayashree, M. Biomarkers in COVID-19: An Up-To-Date Review. Front. Pediatr. 2021, 8, 607647. [Google Scholar] [CrossRef] [PubMed]
- Toraih, E.A.; Elshazli, R.M.; Hussein, M.H.; Elgaml, A.; Amin, M.; El-Mowafy, M.; El-Mesery, M.; Ellythy, A.; Duchesne, J.; Killackey, M.T.; et al. Association of cardiac biomarkers and comorbidities with increased mortality, severity, and cardiac injury in COVID-19 patients: A meta-regression and decision tree analysis. J. Med. Virol. 2020, 92, 2473–2488. [Google Scholar] [CrossRef] [PubMed]
- Moon, A.M.; Barritt, A.S. Elevated Liver Enzymes in Patients with COVID-19: Look, but Not Too Hard. Dig. Dis. Sci. 2021, 66, 1767–1769. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.; Huang, C.; Fei, L.; Li, Q.; Chen, L. Dynamic Changes in Liver Function Tests and Their Correlation with Illness Severity and Mortality in Patients with COVID-19: A Retrospective Cohort Study. Clin. Interv. Aging 2021, 16, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Fernandez Carrillo, C.; Perello, C.; Llop, E.; Garcia-Samaniego, J.; Romero, M.; Mostaza, J.M.; Ibanez, L.; Bañares Cañizares, R.; Bighelli, F.; Uson Peron, C.; et al. Mild ast elevation as an early sign of COVID-19 severity in a multicenter Madrid cohort. Rev. Esp. Enferm. Dig. 2021, 113, 780–786. Available online: https://online.reed.es/fichaArticulo.aspx?iarf=688764742237-417273191161 (accessed on 22 October 2022). [CrossRef]
- Liu, Z.; Hu, D.; Li, J.; Xia, Q.; Gong, Y.; Li, Z.; Wu, Q.; Yi, M.; Huang, Y.; Wu, M.; et al. Prognostic Potential of Liver Enzymes in Patients with COVID-19 at the Leishenshan Hospital in Wuhan. Front. Cell. Infect. Microbiol. 2021, 11, 636999. [Google Scholar] [CrossRef]
- Wang, G.; Wu, C.; Zhang, Q.; Wu, F.; Yu, B.; Lv, J.; Li, Y.; Li, T.; Zhang, S.; Wu, C.; et al. C-Reactive Protein Level May Predict the Risk of COVID-19 Aggravation. Open Forum Infect. Dis. 2020, 7, ofaa153. [Google Scholar] [CrossRef]
- Motta, J.C.; Gómez, C.C. Adenovirus and novel coronavirus (SARS-Cov2) coinfection: A case report. IDCases 2020, 22, e00936. [Google Scholar] [CrossRef]
- Qiu, S.; Zeng, G.; Li, P.; Li, X.; Liu, H.; Du, X.; Liu, H.; Zhang, H.; Xiang, X.; Wang, H.; et al. Pneumonia Patients Caused by Co-infection with SARS-CoV-2 and Human Adenovirus in China. Front. Med. 2021, 8, 735779. [Google Scholar] [CrossRef]
| Overall | SARS-CoV-2 + Rhinovirus n = 23 | SARS-CoV-2 n = 69 | p-Value |
|---|---|---|---|
| Age | 77 | 75 | 0.71 |
| [IQR] | [52–86] | [53–81] | |
| Patient Sex | - | ||
| Female | 10 (43.5%) | 30 (43.5%) | |
| Male | 13 (56.5%) | 39 (56.5%) | |
| Race/Ethnicity | - | ||
| Non-Hispanic White | 8 (34.8%) | 24 (34.8%) | |
| Hispanic or Latino | 9 (39.1%) | 27 (39.1%) | |
| Non-Hispanic Black | 2 (8.7%) | 6 (8.7%) | |
| Other/Unknown | 4 (17.4%) | 12 (17.4%) | |
| Time Period | - | ||
| December 2020–January 2021 | 3 (13.0%) | 9 (13.0%) | |
| February 2021–June 2021 | 3 (13.0%) | 9 (13.0%) | |
| July 2021–December 2021 | 10 (43.5%) | 30 (43.5%) | |
| January 2022–March 2022 | 7 (30.4%) | 21 (30.4%) | |
| Oxygen Support * | 0.05 | ||
| Room Air | 13 (56.5%) | 41 (59.4%) | |
| Low Flow | 6 (26.1%) | 26 (37.7%) | |
| High Flow | 4 (17.4%) | 2 (2.9%) | |
| No. of Elixhauser Comorbidities | 0.219 | ||
| 0 | 2 (8.7%) | 12 (17.4%) | |
| 1–3 | 8 (34.8%) | 27 (39.1%) | |
| 4–6 | 6 (26.1%) | 22 (31.9%) | |
| ≥7 | 7 (30.4%) | 8 (11.6%) | |
| COVID-19 Vaccination Status ** | 1.00 | ||
| No | 14 (60.9%) | 43 (62.3%) | |
| Yes | 9 (39.1%) | 26 (37.7%) | |
| Remdesivir Use *** | 0.231 | ||
| No | 14 (60.9%) | 31 (44.9%) | |
| Yes | 9 (39.1%) | 38 (55.1%) | |
| Corticosteroid Use *** | 0.608 | ||
| No | 6 (26.1%) | 24 (34.8%) | |
| Yes | 17 (73.9%) | 45 (65.2%) |
| Overall | SARS-CoV-2 + Adenovirus n = 9 | SARS-CoV-2 n = 27 | p-Value |
|---|---|---|---|
| Age | 50 | 58 | 0.80 |
| [IQR] | [48–76] | [42–72] | |
| Patient Sex | - | ||
| Female | 2 (22.2%) | 6 (22.2%) | |
| Male | 7 (77.8%) | 21 (77.8%) | |
| Race/Ethnicity | - | ||
| Non-Hispanic White | 4 (44.4%) | 12 (44.4%) | |
| Hispanic or Latino | 3 (33.3%) | 9 (33.3%) | |
| Non-Hispanic Black | 1 (11.1%) | 3 (11.1%) | |
| Other/Unknown | 1 (11.1%) | 3 (11.1%) | |
| Time Period | - | ||
| December 2020–January 2021 | 6 (66.7%) | 18 (66.7%) | |
| February 2021–June 2021 | 1 (11.1%) | 3 (11.1%) | |
| July 2021–December 2021 | 1 (11.1%) | 3 (11.1%) | |
| January 2022–March 2022 | 1 (11.1%) | 3 (11.1%) | |
| Oxygen Support * | 0.146 | ||
| Room Air | 3 (33.3%) | 17 (63.0) | |
| Low Flow | 6 (66.7%) | 10 (37.0%) | |
| High Flow | 0 (0%) | 0 (0%) | |
| No. of Elixhauser Comorbidities | 0.946 | ||
| 0 | 3 (33.3%) | 6 (22.2%) | |
| 1–3 | 3 (33.3%) | 11 (40.7%) | |
| 4–6 | 2 (22.2%) | 6 (22.2%) | |
| ≥7 | 1 (11.1%) | 4 (14.8%) | |
| COVID-19 Vaccination Status ** | 0.558 | ||
| No | 9 (100%) | 24 (88.9%) | |
| Yes | 0 (0%) | 3 (11.1%) | |
| Remdesivir Use *** | 0.252 | ||
| No | 2 (22.2%) | 13 (48.2%) | |
| Yes | 7 (77.8%) | 14 (51.9%) | |
| Corticosteroid Use *** | 0.223 | ||
| No | 1 (11.1%) | 10 (37.0%) | |
| Yes | 8 (88.9%) | 17 (63.0%) |
| Total n = 92 | SARS-CoV-2 + Rhinovirus n = 23 | SARS-CoV-2 n = 69 | p-Value | |
|---|---|---|---|---|
| 30-day all-cause mortality | 0.02 | |||
| No | 76 (82.6%) | 15 (65.2%) | 61 (88.4%) | |
| Yes | 16 (17.4%) | 8 (34.8%) | 8 (11.6%) | |
| 30-day all-cause readmission * | n = 83 | n = 19 | n = 64 | 0.66 |
| No | 76 (91.6%) | 17 (89.5%) | 59 (92.2%) | |
| Yes | 7 (8.4%) | 2 (10.5%) | 5 (7.8%) | |
| ICU admission ** | n = 91 | n = 23 | n = 68 | 0.17 |
| No | 85 (93.4%) | 20 (87.0%) | 65 (95.6%) | |
| Yes | 6 (6.6%) | 3 (13.0%) | 3 (4.4%) | |
| Mechanical Ventilation | 0.26 | |||
| No | 88 (95.7%) | 21 (91.3%) | 67 (97.1%) | |
| Yes | 4 (4.3%) | 2 (8.7%) | 2 (2.9%) |
| SARS-CoV-2 + Rhinovirus | SARS-CoV-2 | p-Value | |
|---|---|---|---|
| Room Air | 0.242 | ||
| No | 11 (84.6%) | 39 (95.1%) | |
| Yes | 2 (15.4%) | 2 (4.9%) | |
| Low Flow | 0.310 | ||
| No | 4 (66.7%) | 22 (84.6%) | |
| Yes | 2 (33.3%) | 4 (15.4%) | |
| High Flow | - | ||
| No | 0 (0%) | 0 (0%) | |
| Yes | 4 (100%) | 2 (100%) |
| Overall | SARS-CoV-2 + Rhinovirus n = 23 | SARS-CoV-2 n = 69 | p-Value |
|---|---|---|---|
| ALT | n = 21 | n = 58 | 0.03 |
| Median (IU/L) | 13 | 24 | |
| [IQR] | [9–27] | [16–40] | |
| AST | n = 21 | n = 58 | 0.04 |
| Median (IU/L) | 25 | 36 | |
| [IQR] | [18–34] | [25–53] | |
| CRP | n = 16 | n = 53 | 0.02 |
| Median (mg/L) | 34.86 | 94.68 | |
| [IQR] | [11.62–87.42] | [43.25–142.02] | |
| Creatinine | n = 23 | n = 66 | 0.99 |
| Median (mg/dL) | 0.94 | 0.90 | |
| [IQR] | [0.60–1.47] | [0.74–1.27] | |
| D-dimer | n = 15 | n = 50 | 0.49 |
| Median (ng/mL) | 269 | 384 | |
| [IQR] | [180–721] | [240–592] | |
| TLC | n = 23 | n = 66 | 0.16 |
| Median (×109/L) | 0.9 | 0.8 | |
| [IQR] | [0.5–1.7] | [0.5–1.2] | |
| Platelets | n = 23 | n = 67 | 0.63 |
| Median (×109/L) | 223 | 198 | |
| [IQR] | [152–274] | [154–273] | |
| WBC | n = 23 | n = 67 | 0.95 |
| Median (×109/L) | 7.4 | 6.9 | |
| [IQR] | [4.1–9.3] | [5.6–9.0] |
| Total n = 36 | SARS-CoV-2 + Adenovirus n = 9 | SARS-CoV-2 n = 27 | p-Value | |
|---|---|---|---|---|
| 30-day all-cause mortality | 0.56 | |||
| No | 33 (91.7%) | 9 (100%) | 24 (88.9%) | |
| Yes | 3 (8.3%) | 0 (0%) | 3 (11.1%) | |
| 30-day all-cause readmission * | n = 32 | n = 9 | n = 23 | 0.54 |
| No | 29 (90.6%) | 9 (100%) | 20 (87.0%) | |
| Yes | 3 (9.4%) | 0 (0%) | 3 (13.0%) | |
| ICU admission | 0.58 | |||
| No | 31 (86.1%) | 7 (77.8%) | 24 (88.9%) | |
| Yes | 5 (13.9%) | 2 (22.2%) | 3 (11.1%) | |
| Mechanical Ventilation | 1.00 | |||
| No | 32 (88.9%) | 8 (88.9%) | 24 (88.9%) | |
| Yes | 4 (11.1%) | 1 (11.1%) | 3 (11.1%) |
| Overall | SARS-CoV-2 + Adenovirus n = 9 | SARS-CoV-2 n = 27 | p-Value |
|---|---|---|---|
| ALT | n = 8 | n = 26 | 0.33 |
| Median (IU/L) | 38.5 | 28.5 | |
| [IQR] | [21–78.5] | [18–35] | |
| AST | n = 8 | n = 26 | 0.97 |
| Median (IU/L) | 36 | 29.5 | |
| [IQR] | [19–40] | [21–41] | |
| CRP | n = 7 | n = 18 | 0.59 |
| Median (mg/dL) | 88.92 | 85.59 | |
| [IQR] | [36.55–299.01] | [33.52–189.70] | |
| Creatinine | n = 9 | n = 27 | 0.73 |
| Median (mg/dL) | 0.77 | 0.80 | |
| [IQR] | [0.72–1.14] | [0.64–1.05] | |
| D-dimer | n = 8 | n = 17 | 0.50 |
| Median (ng/mL) | 272.5 | 302 | |
| [IQR] | [169.50–449] | [279–479] | |
| TLC | n = 9 | n = 26 | 0.65 |
| Median (×109/L) | 1.2 | 1.0 | |
| [IQR] | [0.6–1.3] | [0.4–1.2] | |
| Platelets | n = 9 | n = 27 | 0.38 |
| Median (×109/L) | 181 | 206 | |
| [IQR] | [132–223] | [150–258] | |
| WBC | n = 9 | n = 27 | 0.16 |
| Median (×109/L) | 7.2 | 6 | |
| [IQR] | [6.9–8.3] | [5–8] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tran, Q.-L.; Benitez, G.; Shehadeh, F.; Kaczynski, M.; Mylonakis, E. Clinical Outcomes Associated with SARS-CoV-2 Co-Infection with Rhinovirus and Adenovirus in Adults—A Retrospective Matched Cohort Study. Int. J. Environ. Res. Public Health 2023, 20, 646. https://doi.org/10.3390/ijerph20010646
Tran Q-L, Benitez G, Shehadeh F, Kaczynski M, Mylonakis E. Clinical Outcomes Associated with SARS-CoV-2 Co-Infection with Rhinovirus and Adenovirus in Adults—A Retrospective Matched Cohort Study. International Journal of Environmental Research and Public Health. 2023; 20(1):646. https://doi.org/10.3390/ijerph20010646
Chicago/Turabian StyleTran, Quynh-Lam, Gregorio Benitez, Fadi Shehadeh, Matthew Kaczynski, and Eleftherios Mylonakis. 2023. "Clinical Outcomes Associated with SARS-CoV-2 Co-Infection with Rhinovirus and Adenovirus in Adults—A Retrospective Matched Cohort Study" International Journal of Environmental Research and Public Health 20, no. 1: 646. https://doi.org/10.3390/ijerph20010646
APA StyleTran, Q.-L., Benitez, G., Shehadeh, F., Kaczynski, M., & Mylonakis, E. (2023). Clinical Outcomes Associated with SARS-CoV-2 Co-Infection with Rhinovirus and Adenovirus in Adults—A Retrospective Matched Cohort Study. International Journal of Environmental Research and Public Health, 20(1), 646. https://doi.org/10.3390/ijerph20010646







