Behavioral and Cultural Insights, a Nationwide Study Based on Repetitive Surveys of WHO Behavioral Insights Tool in Greece Regarding COVID-19 Pandemic and Vaccine Acceptance
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Protocol
2.2. Development of Surveys
2.3. Variables
2.4. Questionnaire
2.5. Data Analysis
3. Results
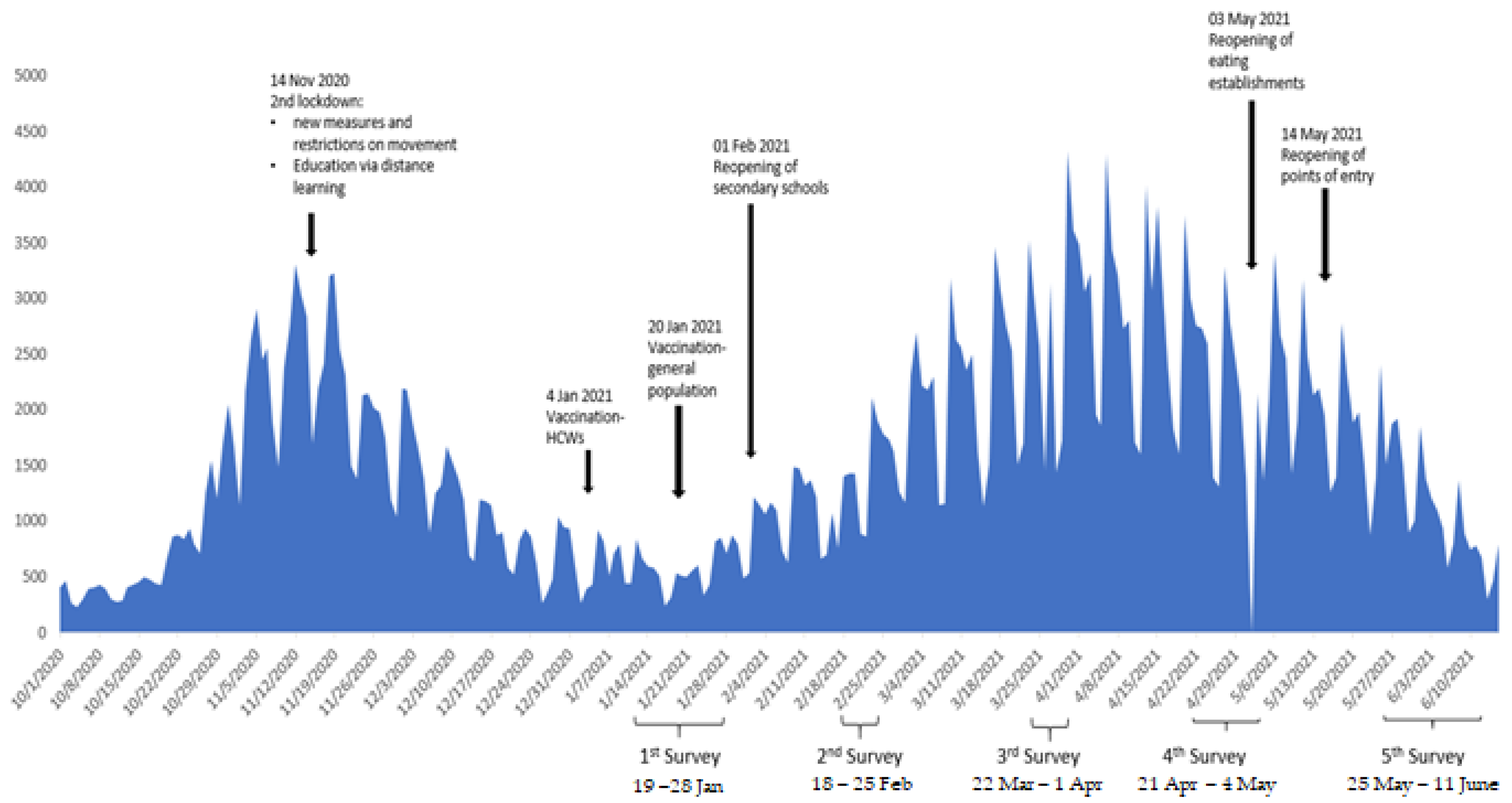
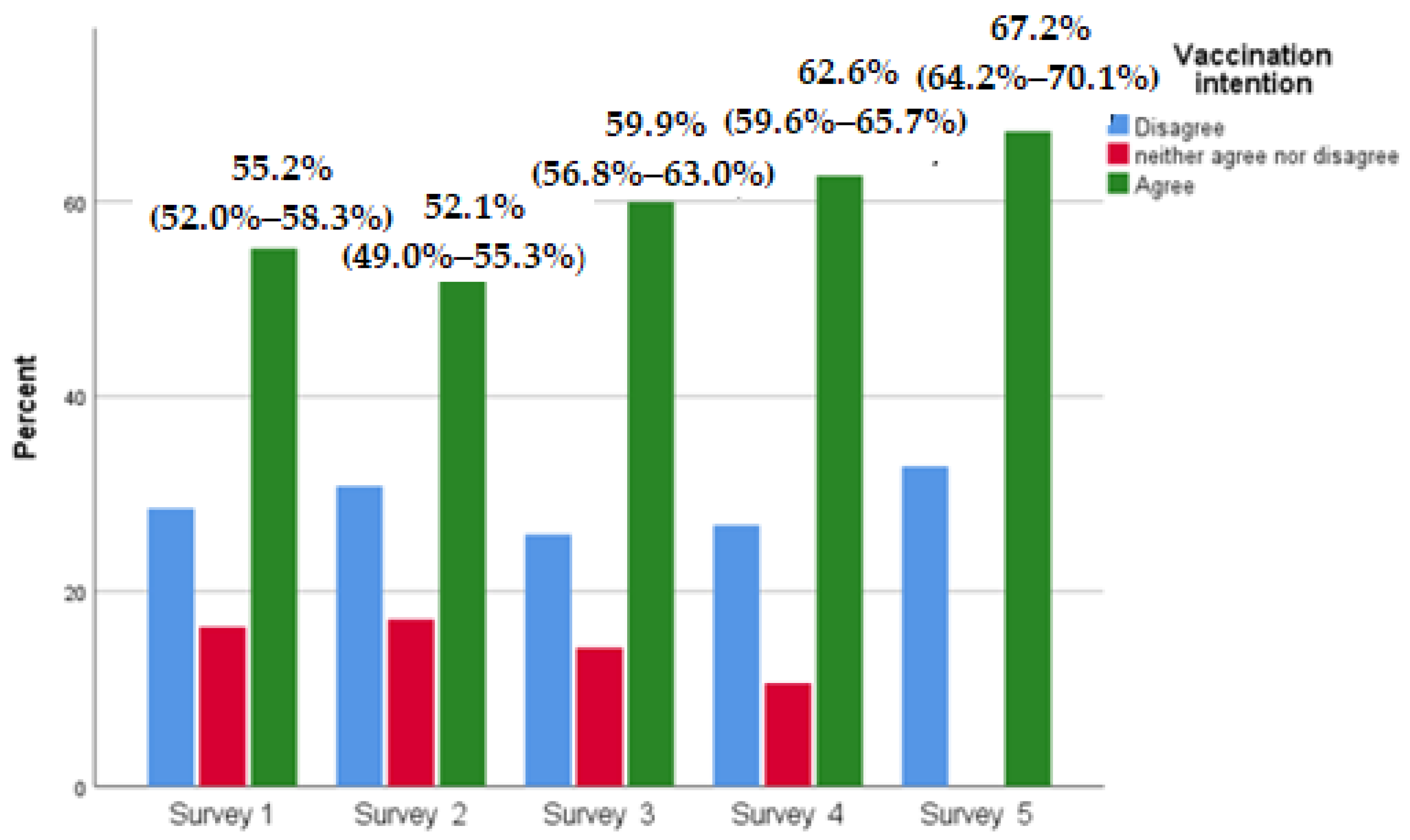
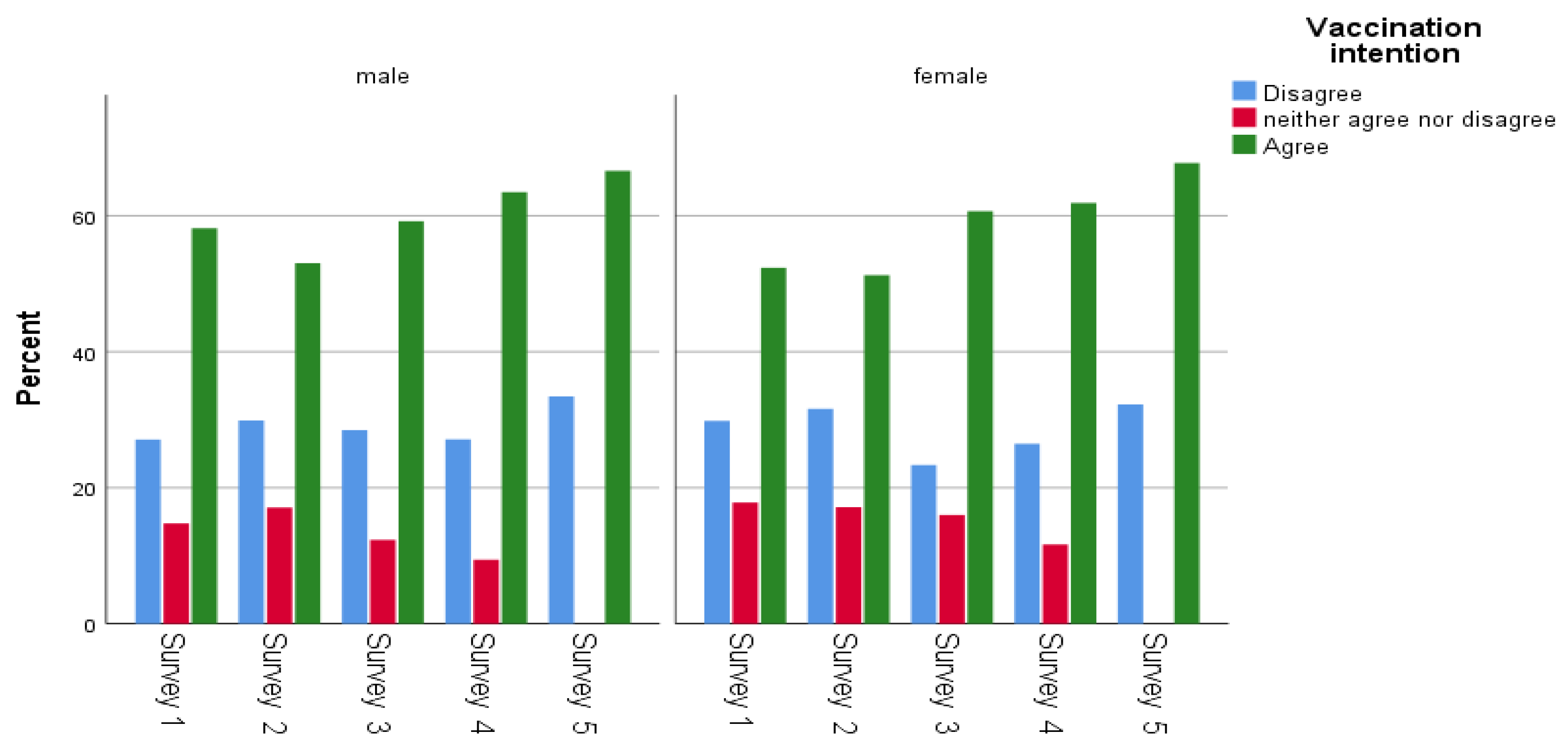
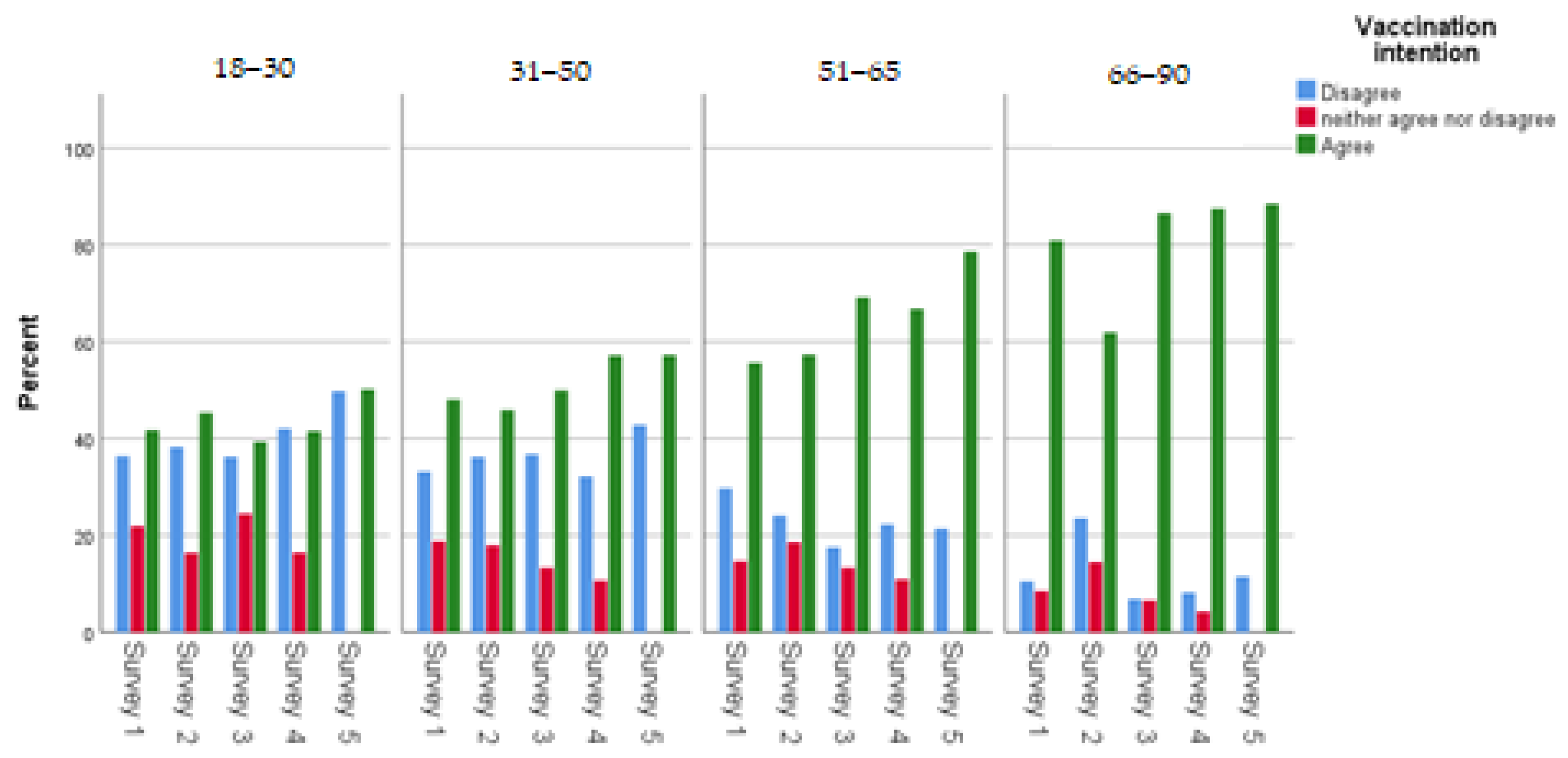
3.1. Trends in Vaccination Intention
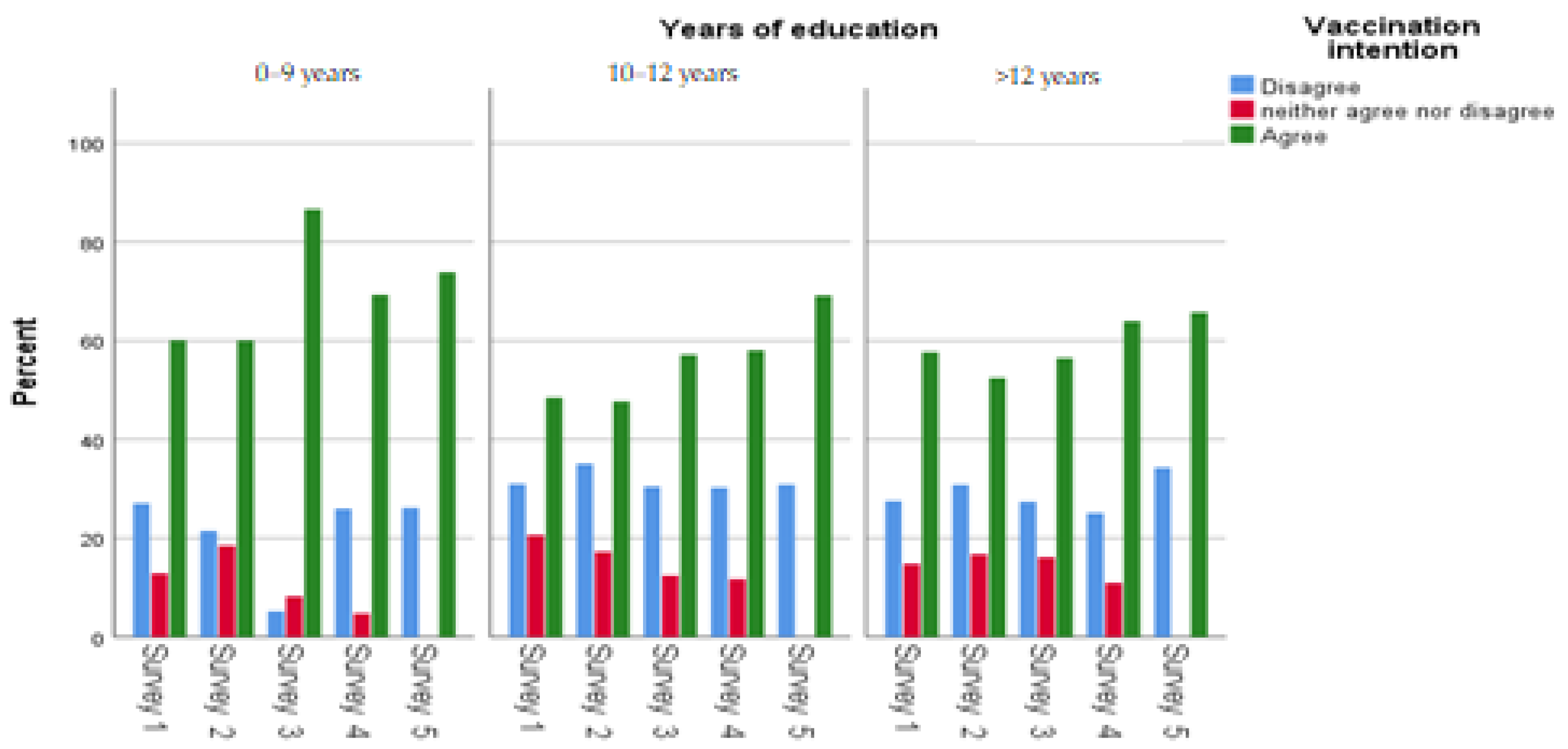
3.2. Socio-Demographic Characteristics
3.3. COVID-19 Infection Status
3.4. Prevention, Knowledge and Behaviours
3.5. Factor Analysis
3.6. Multivariate Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19—11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 8 December 2021).
- Εθνικός Oργανισμός Δημόσιας Υγείας. Aποφάσεις. Available online: https://eody.gov.gr/decisions/ (accessed on 6 July 2022).
- Wake, A.D. Knowledge, Attitude, Practice, and Associated Factors Regarding the Novel Coronavirus Disease 2019 (COVID-19) Pandemic. Infect Drug Resist. 2020, 13, 3817–3832. Available online: https://pubmed.ncbi.nlm.nih.gov/33149627/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Mouchtouri, V.A.; Agathagelidou, E.; Kofonikolas, K.; Rousou, X.; Dadouli, K.; Pinaka, O.; Agathocleous, E.; Anagnostopoulou, L.; Chatziligou, C.; Christoforidou, E.P.; et al. Nationwide Survey in Greece about Knowledge, Risk Perceptions, and Preventive Behaviors for COVID-19 during the General Lockdown in April 2020. Int. J. Environ. Res. Public Health 2020, 17, 8854. Available online: https://pubmed.ncbi.nlm.nih.gov/33260789/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Bruine de Bruin, W.; Bennett, D. Relationships Between Initial COVID-19 Risk Perceptions and Protective Health Behaviors: A National Survey. Am. J. Prev. Med. 2020, 59, 157. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Hu, R.; Yin, L.; Yuan, X.; Tang, H.; Luo, L.; Chen, M.; Huang, D.; Wang, Y.; Yu, A.; et al. Knowledge, Attitudes and Practices of the Chinese Public with Respect to Coronavirus Disease (COVID-19): An Online Cross-Sectional Survey. BMC Public Health 2020, 20, 1816. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-020-09961-2 (accessed on 3 August 2022). [CrossRef]
- Yang, K.; Liu, H.; Ma, L.; Wang, S.; Tian, Y.; Zhang, F.; Li, Z.; Song, Y.; Jiang, X. Knowledge, attitude and practice of residents in the prevention and control of COVID-19: An online questionnaire survey. J. Adv. Nurs. 2021, 77, 1839–1855. [Google Scholar] [CrossRef]
- Caserotti, M.; Girardi, P.; Rubaltelli, E.; Tasso, A.; Lotto, L.; Gavaruzzi, T. Associations of COVID-19 Risk Perception with Vaccine Hesitancy over Time for Italian Residents. Soc. Sci. Med. 2021, 272, 113688. Available online: https://pubmed.ncbi.nlm.nih.gov/33485215/ (accessed on 3 August 2022). [CrossRef]
- Wang, K.; Wong, E.L.-Y.; Ho, K.-F.; Cheung, A.W.-L.; Yau, P.S.-Y.; Dong, D.; Wong, S.Y.-S.; Yeoh, E.-K. Change of Willingness to Accept COVID-19 Vaccine and Reasons of Vaccine Hesitancy of Working People at Different Waves of Local Epidemic in Hong Kong, China: Repeated Cross-Sectional Surveys. Vaccines 2021, 9, 62. [Google Scholar] [CrossRef]
- Rodríguez-Blázquez, C.; Romay-Barja, M.; Falcón, M.; Ayala, A.; Forjaz, M.J. The COSMO-Spain Survey: Three First Rounds of the WHO Behavioral Insights Tool. Front. Public Health 2021, 9, 664. [Google Scholar] [CrossRef]
- Bailey, S.C.; Serper, M.; Opsasnick, L.; Persell, S.D.; O’Conor, R.; Curtis, L.M.; Benavente, J.Y.; Wismer, G.; Batio, S.; Eifler, M.; et al. Changes in COVID-19 Knowledge, Beliefs, Behaviors, and Preparedness Among High-Risk Adults from the Onset to the Acceleration Phase of the US Outbreak. J. Gen. Intern. Med. 2020, 35, 3285. [Google Scholar] [CrossRef]
- de Albuquerque Veloso Machado, M.; Roberts, B.; Wong, B.L.H.; van Kessel, R.; Mossialos, E. The Relationship Between the COVID-19 Pandemic and Vaccine Hesitancy: A Scoping Review of Literature Until August 2021. Front. Public Health 2021, 9, 1370. [Google Scholar] [CrossRef]
- Betsch, C.; Wieler, L.H.; Habersaat, K. Monitoring Behavioural Insights Related to COVID-19. Lancet 2020, 395, 1255–1256. Available online: https://pubmed.ncbi.nlm.nih.gov/32247323/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Summary WHO SAGE Conclusions and Recommendations on Vaccine Hesitancy-Guide-to-Tailoring-Immunization-Programmes-TIP.pdf. 2015. Available online: http://www.who.int/immunization/sage/meetings/2014/october/2_SAGE_Appendicies_Background_final.pdf?ua=12 (accessed on 3 August 2022).
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; MacDonald, N.; Manzo, M.N.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. Available online: https://pubmed.ncbi.nlm.nih.gov/25896383/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Rachiotis, G.; Mouchtouri, V.A.; Kremastinou, J.; Gourgoulianis, K.; Hadjichristodoulou, C. Low Acceptance of Vaccination Against the 2009 Pandemic Influenza a(H1N1) among Healthcare Workers in Greece. Eurosurveillance 2010, 15, 3. Available online: https://www.eurosurveillance.org/content/10.2807/ese.15.06.19486-en (accessed on 3 August 2022). [CrossRef]
- Mereckiene, J.; Cotter, S.; Weber, J.T.; Nicoll, A.; D’Ancona, F.; Lopalco, P.L.; Johansen, K.; Wasley, A.M.; Jorgensen, P.; Lévy-Bruhl, D.; et al. Influenza A(H1N1)pdm09 Vaccination Policies and Coverage in Europe. Euro Surveill. 2012, 17, 20064. Available online: https://pubmed.ncbi.nlm.nih.gov/22297139/ (accessed on 3 August 2022). [CrossRef]
- Hyland, P.; Vallières, F.; Hartman, T.K.; McKay, R.; Butter, S.; Bentall, R.P.; McBride, O.; Shevlin, M.; Bennett, K.; Mason, L.; et al. Detecting and Describing Stability and Change in COVID-19 Vaccine Receptibility in the United Kingdom and Ireland. PLoS ONE 2021, 16, e0258871. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258871 (accessed on 3 August 2022). [CrossRef]
- Caserotti, M.; Gavaruzzi, T.; Girardi, P.; Tasso, A.; Buizza, C.; Candini, V.; Zarbo, C.; Chiarotti, F.; Brescianini, S.; Calamandrei, G.; et al. Who Is Likely to Vacillate in their COVID-19 Vaccination Decision? Free-Riding Intention and Post-Positive Reluctance. Prev. Med. 2022, 154, 106885. Available online: https://pubmed.ncbi.nlm.nih.gov/34774880/ (accessed on 3 August 2022). [CrossRef]
- Maltezou, H.C.; Pavli, A.; Dedoukou, X.; Georgakopoulou, T.; Raftopoulos, V.; Drositis, I.; Bolikas, E.; Ledda, C.; Adamis, G.; Spyrou, A.; et al. Determinants of Intention to Get Vaccinated Against COVID-19 among Healthcare Personnel in Hospitals in Greece. Infect. Dis. Health 2021, 26, 189–197. Available online: https://pubmed.ncbi.nlm.nih.gov/33906828/ (accessed on 3 August 2022). [CrossRef]
- di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. Available online: https://pubmed.ncbi.nlm.nih.gov/33652829/ (accessed on 3 August 2022). [CrossRef]
- Nohl, A.; Afflerbach, C.; Lurz, C.; Brune, B.; Ohmann, T.; Weichert, V.; Zeiger, S.; Dudda, M. Acceptance of COVID-19 Vaccination among Front-Line Health Care Workers: A Nationwide Survey of Emergency Medical Services Personnel from Germany. Vaccines 2021, 9, 424. Available online: https://pubmed.ncbi.nlm.nih.gov/33922812/ (accessed on 3 August 2022). [CrossRef]
- Papagiannis, D.; Rachiotis, G.; Malli, F.; Papathanasiou, I.; Kotsiou, O.; Fradelos, E.; Giannakopoulos, K.; Gourgoulianis, K. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines 2021, 9, 200. Available online: https://pubmed.ncbi.nlm.nih.gov/33670913/ (accessed on 3 August 2022). [CrossRef]
- Papagiannis, D.; Malli, F.; Raptis, D.G.; Papathanasiou, I.V.; Fradelos, E.C.; Daniil, Z.; Rachiotis, G.; Gourgoulianis, K.I. Assessment of Knowledge, Attitudes, and Practices towards New Coronavirus (SARS-CoV-2) of Health Care Professionals in Greece before the Outbreak Period. Int. J. Env. Res. Public Health 2020, 17, 4925. Available online: https://pubmed.ncbi.nlm.nih.gov/32650614/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Marinos, G.; Lamprinos, D.; Georgakopoulos, P.; Patoulis, G.; Vogiatzi, G.; Damaskos, C.; Papaioannou, A.; Sofroni, A.; Pouletidis, T.; Papagiannis, D.; et al. Reported COVID-19 Vaccination Coverage and Associated Factors among Members of Athens Medical Association: Results from a Cross-Sectional Study. Vaccines 2021, 9, 1134. Available online: https://pubmed.ncbi.nlm.nih.gov/34696242/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Fotiadis, K.; Dadouli, K.; Avakian, I.; Bogogiannidou, Z.; Mouchtouri, V.A.; Gogosis, K.; Speletas, M.; Koureas, M.; Lagoudaki, E.; Kokkini, S.; et al. Factors Associated with Healthcare Workers’ (HCWs) Acceptance of COVID-19 Vaccinations and Indications of a Role Model towards Population Vaccinations from a Cross-Sectional Survey in Greece, May 2021. Int. J. Environ. Res. Public Health 2021, 18, 10558. Available online: https://www.mdpi.com/1660-4601/18/19/10558/htm (accessed on 3 August 2022). [CrossRef] [PubMed]
- Avakian, I.; Anagnostopoulos, L.; Rachiotis, G.; Fotiadis, K.; Mariolis, A.; Koureas, M.; Dadouli, K.; Papadopoulos, C.; Speletas, M.; Bakola, M.; et al. Prevalence and Predictors of COVID-19 Vaccination Acceptance among Greek Health Care Workers and Administrative Officers of Primary Health Care Centers: A Nationwide Study Indicating Aspects for a Role Model. Vaccines 2022, 10, 765. Available online: https://www.mdpi.com/2076-393X/10/5/765/htm (accessed on 3 August 2022). [CrossRef] [PubMed]
- WHO’s COVID-19 Guidance and Information for Health Workers and Administrators. Available online: https://www.who.int/teams/epi-win/health-workers-and-administrators#vaccination (accessed on 4 August 2022).
- Behavioural and Cultural Insights and COVID-19. Available online: https://www.who.int/europe/emergencies/situations/covid-19/behavioural-and-cultural-insights-and-covid-19 (accessed on 3 August 2022).
- CintTM. Digital Insights Gathering Platform. Available online: https://www.cint.com/ (accessed on 19 July 2022).
- Hellenic Telecommunications and Post Commission (EETT). Available online: https://www.eett.gr/opencms/opencms/EETT_EN/index.html (accessed on 19 July 2022).
- Press Release Survey on the Use of Information and Communication Technologies in Households and by Individuals-E-Commerce-Privacy and Protection of Personal Data: 2021. Hellenic Statistical Authority (ELSTAT). Available online: https://www.statistics.gr/documents/20181/c9e62cc5-a1a2-ef9a-1d69-68b989500e35 (accessed on 22 December 2022).
- Εθνικός Oργανισμός Δημόσιας Υγείας. Aρχική. Available online: https://eody.gov.gr/ (accessed on 19 July 2022).
- Survey Tool and Guidance: Rapid, Simple, Flexible Behavioural Insights on COVID-19: 29 July 2020. Available online: https://apps.who.int/iris/handle/10665/333549 (accessed on 19 July 2022).
- Petherick, A.; Goldszmidt, R.; Andrade, E.B.; Furst, R.; Hale, T.; Pott, A.; Wood, A. A Worldwide Assessment of Changes in Adherence to COVID-19 Protective Behaviours and Hypothesized Pandemic Fatigue. Nat. Hum. Behav. 2021, 5, 1145–1160. Available online: https://www.nature.com/articles/s41562-021-01181-x (accessed on 3 August 2022). [CrossRef]
- Haktanir, A.; Can, N.; Seki, T.; Kurnaz, M.F.; Dilmaç, B. Do We Experience Pandemic Fatigue? Current State, Predictors, and Prevention. Curr. Psychol. 2021, 41, 7314–7325. [Google Scholar] [CrossRef]
- Feng, Z.; Yang, J.; Xu, M.; Lin, R.; Yang, H.; Lai, L.; Wang, Y.; Wahner-Roedler, D.L.; Zhou, X.; Shin, K.-M.; et al. Dietary Supplements and Herbal Medicine for COVID-19: A Systematic Review of Randomized Control Trials. Clin. Nutr. ESPEN 2021, 44, 50. [Google Scholar] [CrossRef]
- Sypsa, V.; Roussos, S.; Engeli, V.; Paraskevis, D.; Tsiodras, S.; Hatzakis, A. Trends in COVID-19 Vaccination Intent, Determinants and Reasons for Vaccine Hesitancy: Results from Repeated Cross-Sectional Surveys in the Adult General Population of Greece during November 2020–June 2021. Vaccines 2022, 10, 470. [Google Scholar] [CrossRef]
- Ogilvie, G.S.; Gordon, S.; Smith, L.W.; Albert, A.; Racey, C.S.; Booth, A.; Gottschlich, A.; Goldfarb, D.; Murray, M.C.M.; Galea, L.A.M.; et al. Intention to Receive a COVID-19 Vaccine: Results from a Population-Based Survey in Canada. BMC Public Health 2021, 21, 1017. Available online: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-11098-9 (accessed on 3 August 2022). [CrossRef]
- Malik, A.A.; McFadden, S.A.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Ebrahimi, O.V.; Johnson, M.S.; Ebling, S.; Amundsen, O.M.; Halsøy, Ø.; Hoffart, A.; Skjerdingstad, N.; Johnson, S.U. Risk, Trust, and Flawed Assumptions: Vaccine Hesitancy During the COVID-19 Pandemic. Front. Public Health 2021, 9, 700213. [Google Scholar] [CrossRef] [PubMed]
- Bajos, N.; Spire, A.; Silberzan, L. The social specificities of hostility toward vaccination against COVID-19 in France. PLoS ONE 2022, 17, e0262192. [Google Scholar] [CrossRef] [PubMed]
- Katoto, P.D.M.C.; Parker, S.; Coulson, N.; Pillay, N.; Cooper, S.; Jaca, A.; Mavundza, E.; Houston, G.; Groenewald, C.; Essack, Z.; et al. Predictors of COVID-19 Vaccine Hesitancy in South African Local Communities: The VaxScenes Study. Vaccines 2022, 10, 353. [Google Scholar] [CrossRef]
- Yan, E.; Lai, D.W.L.; Lee, V.W.P. Predictors of Intention to Vaccinate against COVID-19 in the General Public in Hong Kong: Findings from a Population-Based, Cross-Sectional Survey. Vaccines 2021, 9, 696. [Google Scholar] [CrossRef]
- Soares, P.; Rocha, J.V.; Moniz, M.; Gama, A.; Laires, P.A.; Pedro, A.R.; Dias, S.; Leite, A.; Nunes, C. Factors Associated with COVID-19 Vaccine Hesitancy. Vaccines 2021, 9, 300. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.M.; Liu, L.; Sun, J.; Yan, W.; Yuan, K.; Zheng, Y.B.; Lu, Z.-A.; Liu, L.; Ni, S.-Y.; Su, S.-Z.; et al. Public Willingness and Determinants of COVID-19 Vaccination at the Initial Stage of Mass Vaccination in China. Vaccines 2021, 9, 1172. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Bendau, A.; Plag, J.; Petzold, M.B.; Ströhle, A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021, 97, 107724. [Google Scholar] [CrossRef]
- Kourlaba, G.; Kourkouni, E.; Maistreli, S.; Tsopela, C.-G.; Molocha, N.-M.; Triantafyllou, C.; Koniordou, M.; Kopsidas, I.; Chorianopoulou, E.; Maroudi-Manta, S.; et al. Willingness of Greek general population to get a COVID-19 vaccine. Glob. Health Res. Policy 2021, 6, 1–10. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. COVID-19 Vaccine Tracker. Available online: https://qap.ecdc.europa.eu/public/extensions/COVID-19/vaccine-tracker.html#uptake-tab (accessed on 4 August 2022).
- Zintel, S.; Flock, C.; Arbogast, A.L.; Forster, A.; von Wagner, C.; Sieverding, M. Gender Differences in the Intention to Get Vaccinated Against COVID-19: A Systematic Review and Meta-Analysis. Z. Fur Gesundh. 2022, 1, 1–25. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8739532/#:~:text=Results,get%20vaccinated%20against%20COVID%2D19 (accessed on 3 August 2022). [CrossRef]
- Lee, M.; You, M. Direct and Indirect Associations of Media Use With COVID-19 Vaccine Hesitancy in South Korea: Cross-sectional Web-Based Survey. J. Med. Internet Res. 2022, 24, e32329. Available online: https://pubmed.ncbi.nlm.nih.gov/34870605/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Shimabukuro, T.T.; Kim, S.Y.; Myers, T.R.; Moro, P.L.; Oduyebo, T.; Panagiotakopoulos, L.; Marquez, P.L.; Olson, C.K.; Liu, R.; Chang, K.T.; et al. Preliminary Findings of mRNA Covid-19 Vaccine Safety in Pregnant Persons. N. Engl. J. Med. 2021, 384, 2273–2282. Available online: https://www.nejm.org/doi/full/10.1056/nejmoa2104983 (accessed on 3 August 2022). [CrossRef] [PubMed]
- Coronavirus Disease (COVID-19): Vaccines. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-(covid-19)-vaccines?adgroupsurvey=%7Badgroupsurvey%7D&gclid=CjwKCAjw46CVBhB1EiwAgy6M4guCBFzF-ChHUUyUiqnaDFRH4d0CZ18sOuiXNuQ2a1iM1VelhBRCNhoCkvIQAvD_BwE (accessed on 4 August 2022).
- Thomas, S.J.; Moreira, E.D., Jr.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Polack, F.P.; Zerbini, C.; et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine through 6 Months. N. Engl. J. Med. 2021, 385, 1761–1773. Available online: https://pubmed.ncbi.nlm.nih.gov/34525277/ (accessed on 3 August 2022). [CrossRef]
- Pormohammad, A.; Zarei, M.; Ghorbani, S.; Mohammadi, M.; Razizadeh, M.; Turner, D.; Turner, R. Efficacy and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Vaccines 2021, 9, 467. Available online: https://pubmed.ncbi.nlm.nih.gov/34066475/ (accessed on 3 August 2022). [CrossRef] [PubMed]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 Vaccine Hesitancy in a Representative Working-Age Population in France: A Survey Experiment Based on Vaccine Characteristics. Lancet Public Health 2021, 6, e210–e221. Available online: http://www.thelancet.com/article/S2468266721000128/fulltext (accessed on 3 August 2022). [CrossRef]
- Coulaud P julien Ablona, A.; Bolduc, N.; Fast, D.; Bertrand, K.; Ward, J.K.; Greyson, D.; Jauffret-Roustide, M.; Knight, R. COVID-19 Vaccine Intention among Young Adults: Comparative Results from a Cross-Sectional Study in Canada and France. Vaccine 2022, 40, 2442. [Google Scholar] [CrossRef]
- Wong, L.P.; Alias, H.; Danaee, M.; Ahmed, J.; Lachyan, A.; Cai, C.Z.; Lin, Y.; Hu, Z.; Tan, S.Y.; Lu, Y.; et al. COVID-19 Vaccination Intention and Vaccine Characteristics Influencing Vaccination Acceptance: A Global Survey of 17 Countries. Infect. Dis. Poverty 2021, 10, 122. Available online: https://pubmed.ncbi.nlm.nih.gov/34620243/ (accessed on 3 August 2022). [CrossRef]
- Marzo, R.R.; Sami, W.; Alam, Z.; Acharya, S.; Jermsittiparsert, K.; Songwathana, K.; Pham, N.T.; Respati, T.; Faller, E.M.; Baldonado, A.M.; et al. Hesitancy in COVID-19 Vaccine Uptake and Its Associated Factors among the General Adult Population: A Cross-Sectional Study in Six Southeast Asian Countries. Trop. Med. Health 2022, 50, 4. Available online: https://tropmedhealth.biomedcentral.com/articles/10.1186/s41182-021-00393-1 (accessed on 3 August 2022). [CrossRef]
- Dambadarjaa, D.; Altankhuyag, G.-E.; Chandaga, U.; Khuyag, S.-O.; Batkhorol, B.; Khaidav, N.; Dulamsuren, O.; Gombodorj, N.; Dorjsuren, A.; Singh, P.; et al. Factors Associated with COVID-19 Vaccine Hesitancy in Mongolia: A Web-Based Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 12903. Available online: https://pubmed.ncbi.nlm.nih.gov/34948511/ (accessed on 3 August 2022). [CrossRef]
- Saelee, R.; Zell, E.; Murthy, B.P.; Castro-Roman, P.; Fast, H.; Meng, L.; Shaw, L.; Gibbs-Scharf, L.; Chorba, T.; Harris, L.Q.; et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, December 14, 2020–January 31, 2022. MMWR Morb Mortal Wkly Rep. 2022, 71, 335–340. Available online: https://pubmed.ncbi.nlm.nih.gov/35239636/ (accessed on 4 August 2022). [CrossRef]
- Sun, Y.; Monnat, S.M. Rural-Urban and Within-Rural Differences in COVID-19 Vaccination Rates. J. Rural. Health 2022, 38, 916–922. [Google Scholar] [CrossRef] [PubMed]
- Delinasios, G.J.; Fragkou, P.C.; Gkirmpa, A.M.; Tsangaris, G.; Hoffman, R.M.; Anagnostopoulos, A.K. The Experience of Greece as a Model to Contain COVID-19 Infection Spread. Vivo 2021, 35, 1285–1294. Available online: https://iv.iiarjournals.org/content/35/2/1285 (accessed on 4 August 2022). [CrossRef] [PubMed]
- De Giorgio, A.; Kuvačić, G.; Maleš, D.; Vecchio, I.; Tornali, C.; Ishac, W.; Ramaci, T.; Barattucci, M.; Milavić, B. Willingness to Receive COVID-19 Booster Vaccine: Associations between Green-Pass, Social Media Information, Anti-Vax Beliefs, and Emotional Balance. Vaccines 2022, 10, 481. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological Characteristics Associated with COVID-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. Available online: https://www.nature.com/articles/s41467-020-20226-9 (accessed on 3 August 2022). [CrossRef]
- Shakeel, C.S.; Mujeeb, A.A.; Mirza, M.S.; Chaudhry, B.; Khan, S.J. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines 2022, 10, 110. Available online: https://www.mdpi.com/2076-393X/10/1/110/htm (accessed on 3 August 2022). [CrossRef]
- Attwell, K.; Lake, J.; Sneddon, J.; Gerrans, P.; Blyth, C.; Lee, J. Converting the maybes: Crucial for a successful COVID-19 vaccination strategy. PLoS ONE 2021, 16, e0245907. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0245907 (accessed on 3 August 2022). [CrossRef]
- Εθνικός Oργανισμός Δημόσιας Υγείας. Γρίπη και Εποχική Γρίπη. Available online: https://eody.gov.gr/disease/gripi-kai-epochiki-gripi/ (accessed on 3 August 2022).
- Status—ELSTAT. 17 December 2021. Available online: https://www.statistics.gr/en/home/ (accessed on 10 June 2021).
- Roma/Gypsies: A European Minority an International Report, Jean-Pierre Liegeois and Nicolae Gheorghe. Available online: https://minorityrights.org/publications/romagypsies-a-european-minority-october-1995/ (accessed on 19 December 2022).

| Survey | Vaccination Intention | Vaccination or Intention to Be Vaccinated | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Categories | 1 | 2 | 3 | 4 | 5 | Comparison between Surveys | (Surveys 1–4) | (Survey 5) | ||
| OR 95%CI | Sig. | OR 95%CI | Sig. | ||||||||
| Gender | Male | 488 (48.5) | 486 (48.5) | 486 (48.6) | 486 (48.6) | 486 (48.6) | 0.999 | 1.04 (0.88–1.22) | 0.687 | 1.04 (0.81–1.35) | 0.739 |
| Female | 517 (51.5) | 515 (51.5) | 514 (51.4) | 514 (51.4) | 514 (51.4) | Ref. | Ref. | ||||
| Age groups | 18–30 | 206 (20.5) | 199 (19.9) | 204 (20.4) | 202 (20.2) | 204 (20.4) | 0.907 | Ref. | Ref. | ||
| 31–50 | 334 (33.2) | 329 (32.9) | 348 (34.8) | 350 (35.0) | 356 (35.6) | 1.42 (1.12–1.80) | 0.004 | 1.50 (1.06–2.13) | 0.022 | ||
| 51–65 | 270 (26.9) | 267 (26.7) | 245 (24.5) | 238 (23.8) | 237 (23.7) | 2.54 (1.98–3.27) | <0.001 | 4.58 (3.05–6.88) | <0.001 | ||
| 66–90 | 196 (19.5) | 206 (20.5) | 206 (20.5) | 210 (21.0) | 203 (20.3) | 7.83 (5.75–10.66) | <0.001 | 10.28 (6.25–16.92) | <0.001 | ||
| Years of education | 0–9 years | 86 (8.5) | 131 (13.1) | 109 (10.9) | 98 (9.8) | 58 (5.8) | <0.001 | Ref. | Ref. | ||
| 10–12 years | 296 (29.5) | 280 (28.0) | 287 (28.7) | 312 (31.2) | 287 (28.7) | 0.45 (0.33–0.61) | <0.001 | 0.96 (0.53–1.73) | 0.878 | ||
| More than 12 | 623 (62.0) | 590 (58.9) | 605 (60.5) | 590 (59.0) | 654 (65.4) | 0.60 (0.45–0.81) | <0.001 | 0.77 (0.44–1.36) | 0.368 | ||
| Health professionals | 153 (15.2) | 156 (15.6) | 170 (17.0) | 180 (18.0) | 143 (14.3) | 0.169 | 0.86 (0.69–1.08) | 0.195 | 1.21 (0.84–1.75) | 0.309 | |
| Area of residence | Rural | 245 (24.4) | 244 (24.4) | 244 (24.4) | 244 (24.4) | 244 (24.4) | 0.999 | Ref. | Ref. | ||
| Urban | 760 (75.6) | 757 (75.6) | 756 (75.6) | 756 (75.6) | 756 (75.6) | 1.25 (1.04–1.51) | 0.020 | 1.01 (0.75–1.36) | 0.960 | ||
| Survey | Vaccination Intention | Vaccination or Intention to Be Vaccinated | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Categories | 1 | 2 | 3 | 4 | 5 | Comparison between Surveys | Surveys 1–4 | Survey 5 | ||
| OR 95%CI | Sig. | OR 95%CI | Sig. | |||||||
| Q14 (symptoms) (>5 correct answers) | 888 (88.4) | 892 (89.1) | 875 (87.5) | 907 (90.7) | 882 (88.2) | 0.201 | 2.24 (1.74–2.88) | <0.001 | 1.75 (1.19–2.56) | 0.004 |
| Q25. National recommendations to prevent COVID-19 infection are followed | 683 (68.0) | 594 (59.3) | 658 (65.9) | 628 (62.9) | 634 (63.4) | 0.001 | 18.52 (11.97–28.64) | <0.001 | 14.42 (5.86–35.48) | <0.001 |
| Frequently washed my hands with soap and water for at least 20 s | 931 (93.4) | 908 (91.6) | 926 (93.2) | 927 (93.7) | 914 (92.3) | 0.358 | 3.01 (2.19–4.14) | <0.001 | 2.78 (1.57–4.91) | <0.001 |
| Avoided touching my eyes, nose and mouth with unwashed hands | 903 (91.1) | 903 (91.5) | 894 (90.4) | 897 (90.3) | 907 (91.7) | 0.755 | 2.72 (2.08–3.54) | <0.001 | 4.63 (2.35–9.11) | <0.001 |
| Used disinfectants to clean hands when soap and water were not available | 958 (96.2) | 955 (96.4) | 958 (96.1) | 953 (96.1) | 947 (95.7) | 0.949 | 4.41 (2.90–6.71) | <0.001 | 3.33 (1.60–6.96) | 0.001 |
| Remained at home when I was sick or had a cold | 872 (94.8) | 844 (93.0) | 868 (94.1) | 871 (95.1) | 814 (90.5) | <0.001 | 2.63 (1.82–3.79) | <0.001 | 2.68 (1.42–5.06) | 0.002 |
| Used herbal supplements to prevent or treat COVID-19 | 335 (35.1) | 336 (36.5) | 289 (30.8) | 313 (33.5) | 282 (30.9) | 0.030 | 0.38 (0.26–0.55) | <0.001 | 0.37 (0.28–0.49) | <0.001 |
| Covered my mouth and/or nose when coughing or sneezing | 977 (97.6) | 971 (97.6) | 976 (98.1) | 976 (98.1) | 951 (95.9) | 0.009 | 2.78 (1.50–5.17) | <0.001 | 2.40 (1.17–4.91) | 0.014 |
| Being cautious when opening mail parcels and letters | 503 (55.2) | 497 (54.7) | 457 (50.8) | 530 (57.5) | 462 (52.1) | 0.038 | 2.30 (1.92–2.76 | <0.001 | 1.60 (1.22–2.11) | 0.001 |
| Vaccinated for influenza | 434 (45.5) | 343 (36.1) | 393 (42.0) | 454 (47.9) | 357 (38.3) | <0.001 | 7.80 (6.25–9.72) | <0.001 | 2.26 (1.72–2.98) | <0.001 |
| Wore a face mask | 975 (97.7) | 957 (96.7) | 971 (97.5) | 959 (97.1) | 962 (96.9) | 0.623 | 7.21 (4.12–12.62) | <0.001 | 4.04 (2.13–7.66) | <0.001 |
| Used antibiotics to prevent or treat COVID-19 | 129 (13.9) | 121 (13.2) | 110 (12.0) | 115 (12.5) | 122 (14.0) | 0.672 | 0.55 (0.42–0.73) | <0.001 | 0.45 (0.33–0.63) | <0.001 |
| Used homeopathic remedies to prevent or treat COVID-19 | 84 (9.2) | 89 (10.1) | 67 (7.5) | 88 (9.9) | 92 (10.7) | 0.189 | 0.51 (0.37–0.71) | <0.001 | 0.46 (0.32–0.67) | <0.001 |
| Ensured physical distancing in public areas | 920 (92.6) | 901 (90.8) | 892 (90.9) | 914 (92.6) | 890 (90.8) | 0.307 | 5.02 (3.73–6.75) | <0.001 | 19.74 (7.81–49.86) | <0.001 |
| Self-isolation | 695 (71.8) | 648 (68.3) | 717 (74.5) | 689 (71.8) | 627 (65.9) | <0.001 | 2.55 (2.13–3.06) | <0.001 | 2.28 (1.61–3.21) | <0.001 |
| Disinfected surfaces | 876 (87.7) | 868 (88.0) | 845 (85.3) | 847 (86.3) | 872 (88.3) | 0.221 | 1.95 (1.54–2.46) | <0.001 | 2.85 (1.76–4.61) | <0.001 |
| Consumed garlic, ginger and lemon | 311 (33.8) | 268 (30.6) | 264 (29.8) | 261 (28.7) | 225 (25.9) | 0.008 | 0.53 (0.44–0.64) | <0.001 | 0.59 (0.44–0.80) | 0.001 |
| Survey | Vaccination Intention | Vaccination or Intention to Be Vaccinated | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Categories The Kind of Information I Need the Most Relates to… | 1 | 2 | 3 | 4 | 5 | Comparison between Surveys | Surveys 1–4 | Survey 5 | ||
| OR 95%CI | Sig. | OR 95%CI | Sig. | |||||||
| how to protect myself and my family from COVID-19 | 885 (88.1) | 855 (85.4) | 884 (88.4) | 891 (89.1) | 870 (87.0) | 0.108 | 4.48 (3.51–5.71) | <0.001 | 2.43 (1.67–3.54) | <0.001 |
| the symptoms associated with COVID-19. | 848 (84.4) | 803 (80.2) | 814 (81.4) | 832 (83.2) | 823 (82.3) | 0.132 | 4.28 (3.47–5.29) | <0.001 | 2.19 (1.56–3.04) | <0.001 |
| people’s stories about how they deal with the pandemic situation | 590 (58.7) | 581 (58.0) | 592 (59.2) | 621 (62.1) | 594 (59.4) | 0.407 | 1.22 (1.03–1.44) | 0.023 | 0.71 (0.55–0.92) | 0.010 |
| about emerging evidence and scientific advancements in the development of vaccines or treatments for COVID-19. | 880 (87.6) | 863 (86.2) | 892 (89.2) | 880 (88.0) | 888 (88.8) | 0.272 | 9.81 (7.50–12.84) | <0.001 | 4.88 (3.16–7.56) | <0.001 |
| how to care for a person belonging to a vulnerable group | 843 (83.9) | 817 (81.6) | 824 (82.4) | 866 (86.6) | 804 (80.4) | 0.003 | 2.24 (1.81–2.77) | <0.001 | 2.08 (1.52–2.85) | <0.001 |
| how I can protect and ensure continuity of my children’s education | 575 (57.2) | 598 (59.7) | 556 (55.6) | 595 (59.5) | 615 (61.5) | 0.066 | 0.90 (0.76–1.06) | 0.212 | 1.01 (0.78–1.31) | 0.934 |
| The difference between COVID-19 and influenza | 820 (81.6) | 770 (76.9) | 773 (77.3) | 795 (79.5) | 782 (78.2) | 0.072 | 3.21 (2.64–3.90) | <0.001 | 2.89 (2.13–3.94) | <0.001 |
| about the evolution of the pandemic situation globally | 886 (88.2) | 843 (84.2) | 864 (86.4) | 853 (85.3) | 848 (84.8) | 0.093 | 4.91 (3.89–6.20) | <0.001 | 3.58 (2.49–5.14) | <0.001 |
| about the evolution of the pandemic situation in Greece | 886 (88.2) | 856 (85.5) | 899 (89.9) | 870 (87.0) | 878 (87.8) | 0.049 | 6.85 (5.29–8.87) | <0.001 | 3.44 (2.32–5.11) | <0.001 |
| informed about competent authorities’ decisions related to COVID19 public health measures | 892 (88.8) | 855 (85.4) | 872 (87.2) | 860 (86.0) | 831 (83.1) | 0.005 | 4.08 (3.20–5.19) | <0.001 | 2.43 (1.74–3.40) | <0.001 |
| how the pandemic can affect my financial situation | 854 (85.0) | 865 (86.4) | 869 (86.9) | 869 (86.9) | 835 (83.5) | 0.128 | 1.25 (0.98–1.58) | 0.069 | 1.13 (0.80–1.59) | 0.487 |
| how to maintain my mental health and well-being during isolation | 750 (74.6) | 773 (77.2) | 746 (74.6) | 769 (76.9) | 751 (75.1) | 0.474 | 1.58 (1.31–1.90) | <0.001 | 1.44 (1.08–1.93) | 0.013 |
| how to maintain my social contacts despite practicing physical distancing | 673 (67.0) | 660 (65.9) | 695 (69.5) | 710 (71.0) | 687 (68.7) | 0.112 | 1.33 (1.12–1.59) | 0.001 | 1.43 (1.09–1.88) | 0.009 |
| Variables | Vaccination Intention | ||
|---|---|---|---|
| Agree/Disagree | |||
| Sig. | aOR | 95% CI | |
| Age (years) | 0.016 | 1.011 | 1.002–1.019 |
| Gender (male/female) | <0.001 | 2.07 | 1.60–2.69 |
| Education (10–12/0–9 years) | 0.017 | 0.56 | 0.34-0.90 |
| Education (>12/0–9 years) | 0.627 | 0.89 | 0.56–1.42 |
| Chronic illness | 0.186 | 1.24 | 0.90–1.72 |
| Area of residence (>500,000/<500,000) | 0.145 | 1.22 | 0.94–1.58 |
| Knowledge of symptoms (>5/≤5) | 0.008 | 1.69 | 1.15–2.50 |
| Knowledge about prevention | 0.935 | 0.99 | 0.74–1.31 |
| Influenza vaccination | <0.001 | 4.84 | 3.61–6.50 |
| I follow the recommendations of my country’s authorities to prevent the spread of the new coronavirus (Agree/Disagree). | <0.001 | 3.97 | 1.90–8.29 |
| I follow the recommendations of my country’s authorities to prevent the spread of the new coronavirus (NAND/Disagree) | 0.001 | 1.63 | 1.24–2.14 |
| Mass media and Social media | <0.001 | 1.43 | 1.25–1.62 |
| HCWs and states’ instructions | <0.001 | 3.40 | 2.92–3.96 |
| Family’s, friends’ and colleagues’ opinion | 0.015 | 0.86 | 0.76–0.97 |
| My and my loved ones’ wellbeing and health system overload | <0.001 | 1.62 | 1.42–1.86 |
| Country’s economic recession | 0.013 | 1.19 | 1.04–1.36 |
| Personal financial problems | 0.001 | 0.79 | 0.69–0.90 |
| Losing my social life | 0.048 | 0.88 | 0.78–0.99 |
| Survey 4 | Ref. | ||
| Survey 1 | 0.004 | 0.60 | 0.42–0.85 |
| Survey 2 | 0.345 | 0.85 | 0.60–1.20 |
| Survey 3 | 0.628 | 1.09 | 0.77–1.55 |
| Variables | Vaccination or Intention to Be Vaccinated | ||
|---|---|---|---|
| Yes/No | |||
| Sig. | aOR | 95% CI | |
| Age (years) | <0.001 | 1.04 | 1.03–1.05 |
| Gender (male/female) | 0.008 | 1.66 | 1.14–2.40 |
| Education (10–12/0–9 years) | 0.189 | 1.74 | 0.76–3.96 |
| Education (>12/0–9 years) | 0.565 | 1.26 | 0.57–2.80 |
| Chronic illness | 0.582 | 0.88 | 0.57–1.37 |
| Area of residence (>500,000/<500,000) | 0.040 | 1.49 | 1.02–2.17 |
| Knowledge of symptoms (>5/≤5) | 0.542 | 0.84 | 0.49–1.46 |
| Influenza vaccination | <0.001 | 3.49 | 2.34–5.20 |
| I follow the recommendations of my country’s authorities to prevent the spread of the new coronavirus (Agree/Disagree) | 0.008 | 10.28 | 3.19–33.12 |
| I follow the recommendations of my country’s authorities to prevent the spread of the new coronavirus (NAND/Disagree) | <0.001 | 4.88 | 1.51–15.75 |
| HCWs, states’ instructions and public state mass media | <0.001 | 2.23 | 1.79–2.79 |
| Private owned Mass media and Social media | 0.599 | 1.05 | 0.88–1.26 |
| Family’s, friends’ and colleagues’ opinion | 0.048 | 0.83 | 0.68–1.00 |
| My and my loved ones’ wellbeing | 0.061 | 1.21 | 0.99–1.47 |
| Country’s economic recession and health system overload | 0.048 | 1.21 | 1.00–1.47 |
| Losing my social life | 0.688 | 0.96 | 0.79–1.17 |
| Personal financial problems | 0.010 | 0.77 | 0.63–0.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prezerakos, P.; Dadouli, K.; Agapidaki, E.; Kravvari, C.-M.; Avakian, I.; Peristeri, A.-M.; Anagnostopoulos, L.; Mouchtouri, V.A.; Fountoulakis, K.N.; Koupidis, S.; et al. Behavioral and Cultural Insights, a Nationwide Study Based on Repetitive Surveys of WHO Behavioral Insights Tool in Greece Regarding COVID-19 Pandemic and Vaccine Acceptance. Int. J. Environ. Res. Public Health 2023, 20, 216. https://doi.org/10.3390/ijerph20010216
Prezerakos P, Dadouli K, Agapidaki E, Kravvari C-M, Avakian I, Peristeri A-M, Anagnostopoulos L, Mouchtouri VA, Fountoulakis KN, Koupidis S, et al. Behavioral and Cultural Insights, a Nationwide Study Based on Repetitive Surveys of WHO Behavioral Insights Tool in Greece Regarding COVID-19 Pandemic and Vaccine Acceptance. International Journal of Environmental Research and Public Health. 2023; 20(1):216. https://doi.org/10.3390/ijerph20010216
Chicago/Turabian StylePrezerakos, Panagiotis, Katerina Dadouli, Eirini Agapidaki, Christina-Maria Kravvari, Ioanna Avakian, Athanasia-Marina Peristeri, Lemonia Anagnostopoulos, Varvara A. Mouchtouri, Konstantinos N. Fountoulakis, Sotirios Koupidis, and et al. 2023. "Behavioral and Cultural Insights, a Nationwide Study Based on Repetitive Surveys of WHO Behavioral Insights Tool in Greece Regarding COVID-19 Pandemic and Vaccine Acceptance" International Journal of Environmental Research and Public Health 20, no. 1: 216. https://doi.org/10.3390/ijerph20010216
APA StylePrezerakos, P., Dadouli, K., Agapidaki, E., Kravvari, C.-M., Avakian, I., Peristeri, A.-M., Anagnostopoulos, L., Mouchtouri, V. A., Fountoulakis, K. N., Koupidis, S., & Hadjichristodoulou, C. (2023). Behavioral and Cultural Insights, a Nationwide Study Based on Repetitive Surveys of WHO Behavioral Insights Tool in Greece Regarding COVID-19 Pandemic and Vaccine Acceptance. International Journal of Environmental Research and Public Health, 20(1), 216. https://doi.org/10.3390/ijerph20010216








