Association between Chronotype and Sleep Quality among Chinese College Students: The Role of Bedtime Procrastination and Sleep Hygiene Awareness
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.2.1. Chronotype
2.2.2. Bedtime Procrastination
2.2.3. Sleep Quality
2.2.4. Sleep Hygiene Awareness
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Data
3.2. Pearson’s Correlation Results
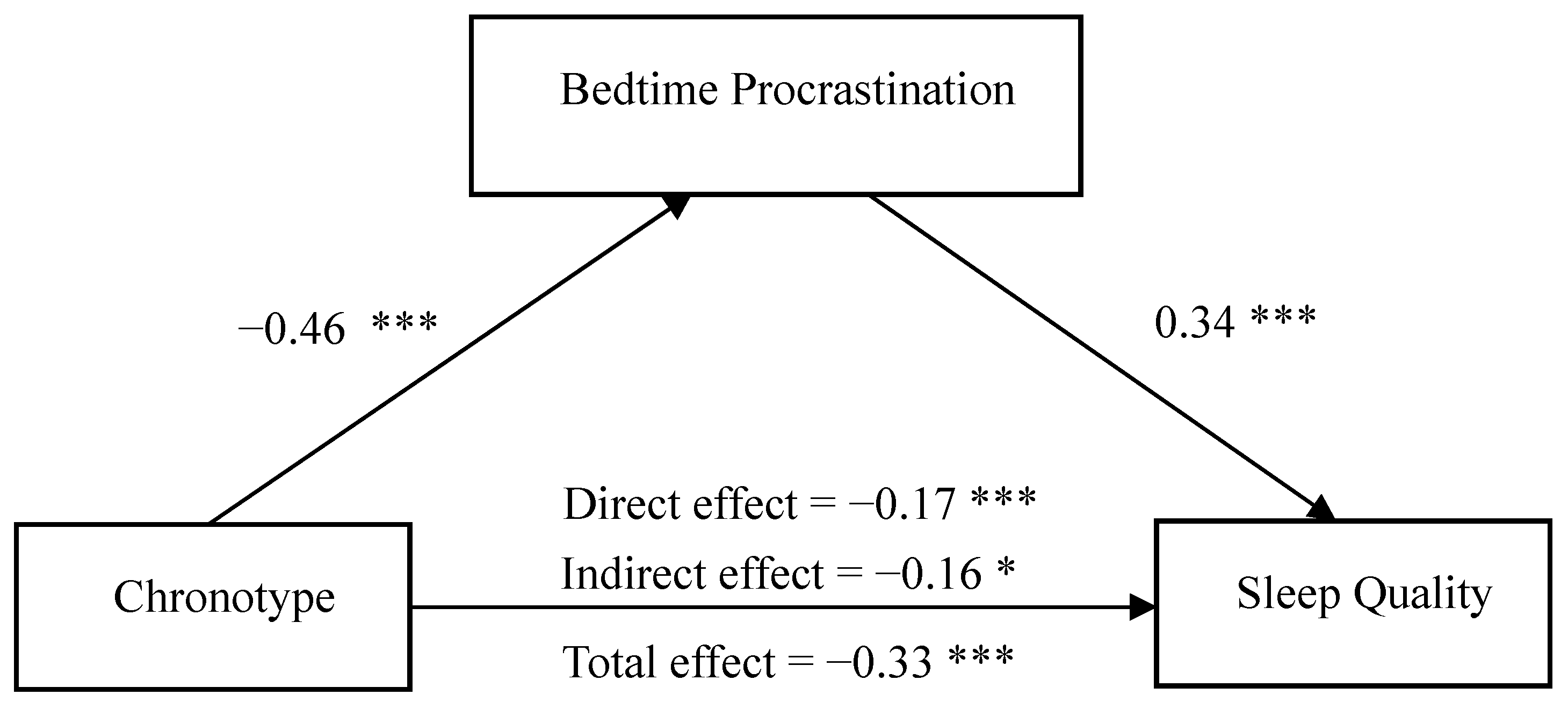
3.3. Mediation Analysis
3.4. Moderation Analysis
4. Discussion
5. Limitations and Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rique, G.; Filho, G.; Ferreira, A.; Sousa-Muoz, R.L.D. Relationship between chronotype and quality of sleep in medical students at the federal university of paraiba, brazil. Sleep Sci. 2014, 7, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Adan, A.; Archer, S.N.; Hidalgo, M.P.; Di Milia, L.; Natale, V.; Randler, C. Circadian typology: A comprehensive review. Chronobiol. Int. 2012, 29, 1153–1175. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.M.; Jankowski, K.S.; Khan, M.H.A. Morningness-eveningness preference and shift in chronotype during COVID-19 as predictors of mood and well-being in university students. Pers. Indiv. Differ. 2022, 191, 111581. [Google Scholar] [CrossRef] [PubMed]
- Monk, T.H.; Buysse, D.K.; Potts, J.M.; DeGrazia, J.N.; Kupfer, D.J. Morningness–eveningness and lifestyle regularity. Chronobiol. Int. 2004, 21, 435–443. [Google Scholar] [CrossRef]
- Choi, H.J.; Lee, Y.J.; Yoo, Y.J.; Cho, Y.W.; Moon, H.-J. The effects of chronotype and social jetlag on medical students. Sleep Biol. Rhythm. 2019, 17, 269–276. [Google Scholar] [CrossRef]
- Au, J.; Reece, J. The relationship between chronotype and depressive symptoms: A meta-analysis. J. Affect. Disord. 2017, 218, 93–104. [Google Scholar] [CrossRef]
- Jankowski, K.S.; Linke, M. Angry night birds: Emotionality, activity and sociability temperament in adolescent chronotypes. Chronobiol. Int. 2020, 37, 652–659. [Google Scholar] [CrossRef]
- Gobin, C.M.; Banks, J.B.; Fins, A.I.; Tartar, J.L. Poor sleep quality is associated with a negative cognitive bias and decreased sustained attention. J. Sleep Res. 2015, 24, 535–542. [Google Scholar] [CrossRef]
- Merikanto, I.; Kortesoja, L.; Benedict, C.; Chung, F.; Cedernaes, J.; Espie, C.A.; Bjorvatn, B. Evening-types show highest increase of sleep and mental health problems during the COVID-19 pandemic—Multinational study on 19267 adults. Sleep 2022, 45, zsab216. [Google Scholar] [CrossRef]
- Wehr, T.A. The durations of human melatonin secretion and sleep respond to changes in daylength (photoperiod). J. Clin. Endocrinol. Metabol. 1991, 73, 1276–1280. [Google Scholar] [CrossRef]
- Goelema, M.S.; Regis, M.; Haakma, R.; van den Heuvel, E.R.; Markopoulos, P.; Overeem, S. Determinants of perceived sleep quality in normal sleepers. Behav. Sleep Med. 2019, 17, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Hairston, I.S.; Shpitalni, R. Procrastination is linked with insomnia symptoms: The moderating role of morningness-eveningness. Pers. Indiv. Differ. 2016, 101, 50–56. [Google Scholar] [CrossRef]
- Vollmer, C.; Jankowski, K.S.; Díaz-Morales, J.F.; Itzek-Greulich, H.; Randler, C. Morningness–eveningness correlates with sleep time, quality, and hygiene in secondary school students: A multilevel analysis. Sleep Med. 2017, 30, 151–159. [Google Scholar] [CrossRef]
- Dijk, D.J.; Lockley, S.W. Invited Review: Integration of human sleep-wake regulation and circadian rhythmicity. J. Appl. Physiol. 2002, 92, 852–862. [Google Scholar] [CrossRef] [PubMed]
- Selvi, Y.; Aydin, A.; Gulec, M.; Boysan, M.; Besiroglu, L.; Ozdemir, P.G.; Kilic, S. Comparison of dream anxiety and subjective sleep quality between chronotypes. Sleep Biol. Rhythm. 2012, 10, 14–22. [Google Scholar] [CrossRef]
- Zhu, Y.Y.; Ma, X.Q.; Tang, Z.Y.; Yang, M.Q. Impact of Chronotype on Symptoms of Depression in College Students: A Moderate Mediation Model. Stud. Psychol. Behav. 2021, 19, 657–664. [Google Scholar]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef]
- Kroese, F.M.; de Ridder, D.T.D.; Evers, C.; Adriaanse, M.A. Bedtime procrastination: Introducing a new area of procrastination. Front. Psychol. 2014, 5, 611. [Google Scholar] [CrossRef]
- Roenneberg, T.; Wirz-Justice, A.; Merrow, M. Life between clocks: Daily temporal patterns of human chronotypes. J. Biol. Rhythm. 2003, 18, 80. [Google Scholar] [CrossRef]
- Kadzikowska-Wrzosek, R. Insufficient sleep among adolescents: The role of bedtime procrastination, chronotype and autonomous vs. controlled motivational regulations. Curr. Psychol. 2018, 39, 1031–1040. [Google Scholar] [CrossRef]
- Kadzikowska-Wrzosek, R. Self-regulation and bedtime procrastination: The role of self-regulation skills and chronotype. Pers. Indiv. Differ. 2018, 128, 10–15. [Google Scholar] [CrossRef]
- Kühnel, J.; Syrek, C.J.; Dreher, A. Why don’ t you go to bed on time? A daily diary study on the relationships between chronotype, self-control resources and the phenomenon of bedtime procrastination. Front. Psychol. 2018, 9, 77. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Morales, J.F.; Delgado, P.; Escribano, C.; Collado, M.J.; Randler, C. Sleep beliefs and chronotype among adolescents: The effect of a sleep education program. Biol. Rhythm. Res. 2012, 43, 397–412. [Google Scholar] [CrossRef]
- Milfont, T.L.; Schwarzenthal, M. Explaining why larks are future-oriented and owls are present-oriented: Self-control mediates the chronotype–time perspective relationships. Chronobiol. Int. 2014, 31, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Stolarski, M.; Ledzińska, M.; Matthews, G. Morning is tomorrow, evening is today: Relationships between chronotype and time perspective. Biol. Rhythm. Res. 2013, 44, 181–196. [Google Scholar] [CrossRef]
- Li, L.; Sun, H.M. Review of research on bedtime procrastination. China J. Health Psychol. 2020, 28, 316–320. [Google Scholar]
- Parker, B.J.; Plank, R.E. A uses and gratifications perspective on the internet as a new information source. Lat. Am. Bus. Rev. 2020, 18, 43–49. [Google Scholar]
- Zhang, M.X.; Wu, A.M.S. Effects of smartphone addiction on sleep quality among Chinese university students: The mediating role of self-regulation and bedtime procrastination. Addict. Behav. 2020, 111, 106552. [Google Scholar] [CrossRef]
- Kroese, F.M.; Evers, C.; Adriaanse, M.A.; de Ridder, D.T. Bedtime procrastination: A self-regulation perspective on sleep insufficiency in the general population. J. Health Psychol. 2016, 21, 853–862. [Google Scholar] [CrossRef]
- Nauts, S.; Kamphorst, B.A.; Sutu, A.E.; Poortvliet, R.; Anderson, J.H. Aversive bedtime routines as a precursor to bedtime procrastination. Eur. Health Psychol. 2016, 18, 80–85. [Google Scholar]
- You, Z.Q.; Xu, Y.; Zhang, L.; Sun, X.J. The Predictive Effect of Self-Control on Sleep Quality: The Mediating Role of Rumination and Bedtime Procrastination. Chin. J. Appl. Psychol. 2020, 26, 75–82. [Google Scholar]
- Perlis, M.; Aloia, M.; Kuhn, B. Behavioral Treatments for Sleep Disorders; Elsevier Inc.: London, UK, 2011. [Google Scholar]
- Lacks, P.; Rotert, M. Knowledge and practice of sleep hygiene techniques in insomniacs and good sleepers. Behav. Res. Ther. 1986, 24, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.M.; Lin, S.C.; Hsu, S.C.; Cheng, C.P. Maladaptive sleep hygiene practices in good sleepers and patients with insomnia. J. Health Psychol. 2010, 15, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Al-Kandari, S.; Alsalem, A.; Al-Mutairi, S.; Al-Lumai, D.; Dawoud, A.; Moussa, M. Association between sleep hygiene awareness and practice with sleep quality among Kuwait University students. Sleep Health 2017, 3, 342–347. [Google Scholar] [CrossRef]
- Brown, F.C.; Buboltz, W.C.; Soper, B. Relationship of Sleep Hygiene Awareness, Sleep Hygiene Practices, and Sleep Quality in University Students. Behav. Med. 2002, 28, 33–38. [Google Scholar] [CrossRef]
- Huo, J.X.; Yang, C.Y.; Zhang, L.X. The effects of college students sleep hygiene knowledge, beliefs and behaviors on sleep quality in Baotou. Health Med. Res. 2010, 7, 1–7. [Google Scholar]
- Ballot, O.; Daviaux, Y.; Sanz-Arigita, E.J.; Ivers, H.; Micoulaud-Franchi, J.A.; Bioulac, S.; Altena, E. Emotion coping strategies and dysfunctional sleep-related beliefs are associated with objective sleep problems in young adults with insomnia. Sleep Med. 2021, 88, 180–186. [Google Scholar] [CrossRef]
- Adan, A.; Fabbri, M.; Natale, V.; Prat, G. Sleep Beliefs Scale (SBS) and circadian typology. J. Sleep Res. 2006, 15, 125–132. [Google Scholar] [CrossRef]
- Saxvig, I.W.; Evanger, L.N.; Pallesen, S.; Hysing, M.; Sivertsen, B.; Gradisar, M.; Bjorvatn, B. Circadian typology and implications for adolescent sleep health. Results from a large, cross-sectional, school-based study. Sleep Med. 2021, 83, 63–70. [Google Scholar] [CrossRef]
- Jefferson, C.D.; Drake, C.L.; Scofield, H.M.; Myers, E.; McClure, T.; Roehrs, T.; Roth, T. Sleep hygiene practices in a population-based sample of insomniacs. Sleep 2005, 28, 611–615. [Google Scholar] [CrossRef]
- Lundh, L.G.; Broman, J.E. Insomnia as an interaction between sleep-interfering and sleep interpreting processes. J. Psychosom. Res. 2000, 49, 299–310. [Google Scholar] [CrossRef] [PubMed]
- Murawski, B.; Wade, L.; Plotnikoff, R.C.; Lubans, D.R.; Duncan, M.J. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Med. Rev. 2018, 40, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Perrault, A.A.; Pomares, F.B.; Smith, D.; Cross, N.E.; Gong, K.; Maltezos, A.; Dang-Vu, T.T. Effects of cognitive behavioral therapy for insomnia on subjective and objective measures of sleep and cognition. Sleep Med. 2022, 97, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; van Egmond, L.; Partinen, M.; Lange, T.; Benedict, C. A narrative review of interventions for improving sleep and reducing circadian disruption in medical inpatients. Sleep Med. 2019, 59, 42–50. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar]
- Zhang, B.; Hao, Y.L.; Rong, R.G. The reliability and validity of Chinese version morningness/ eveningness questionnaire. Chin. J. Clin. Psychol. 2006, 15, 856–858. [Google Scholar]
- Ma, X.H.; Zhu, L.W.; Guo, J.; Zhao, Y.; Fu, Y.M.; Mu, L. Reliability and Validity of the Bedtime Procrastination Scale in Chinese College Students. Chin. J. Clin. Psychol. 2021, 29, 717–720. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. J. Psychiatr. Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Liu, X.C.; Tang, M.Q.; Hu, L.; Wang, A.Z.; Wu, H.X.; Zhao, G.F.; Gao, C.N.; Li, W.S. Reliability and validity of the Pittsburgh sleep quality index. Chin. J. Psychiatry 1996, 29, 103–107. [Google Scholar]
- Pan, J.Y. The Diagnosis and Management of Sleep Disorders; South China University of Technology Press: Guangzhou, China, 2001. [Google Scholar]
- Zhang, Y.G.; Yu, C.H.; Li, J.Y. Correlation of sleep quality with sleep hygiene awareness, beliefs and attitudes about sleep in patients with lung cancer. Guangxi Med. J. 2019, 41, 1749–1752. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Hayes, A.F.; Matthes, J. Computational procedures for probing interactions in OLS and logistic regression: SPSS and SAS implementations. Behav. Res. Methods 2009, 41, 924–936. [Google Scholar] [CrossRef] [PubMed]
- Gaina, A.; Sekine, M.; Kanayama, H.; Takashi, Y.; Hu, L.; Kagamimori, S. Morning-evening preference: Sleep pattern spectrum and lifestyle habits among Japanese junior high school pupils. Chronobiol. Int. 2006, 23, 606–621. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.X.; Liang, G.; Li, D.L.; Liu, M.X.; Yin, Z.Y.; Li, Y.Z.; Pan, C.W. Association between parental control and depressive symptoms among college freshmen in China: The chain mediating role of chronotype and sleep quality. J. Affect. Disord. 2022, 317, 256–264. [Google Scholar] [CrossRef] [PubMed]
- Vitale, J.A.; Roveda, E.; Montaruli, A.; Galasso, L.; Weydahl, A.; Caumo, A.; Carandente, F. Chronotype influences activity circadian rhythm and sleep: Differences in sleep quality between weekdays and weekend. Chronobiol. Int. 2015, 32, 405–415. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.J.; Hasler, B.P. Chronotype and mental health: Recent advances. Curr. Psychiatry Rep. 2018, 20, 59. [Google Scholar] [CrossRef]
- Barclay, N.L.; Eley, T.C.; Buysse, D.J.; Archer, S.N.; Gregory, A.M. Diurnal preference and sleep quality: Same genes? A study of young adult twins. Chronobiol. Int. 2010, 27, 278–296. [Google Scholar] [CrossRef]
- Ong, J.C.; Huang, J.S.; Kuo, T.F.; Manber, R. Characteristics of insomniacs with self-reported morning and evening chronotypes. J. Clin. Sleep Med. 2007, 3, 289–294. [Google Scholar] [CrossRef]
- Yun, J.A.; Ahn, Y.S.; Jeong, K.S.; Joo, E.J.; Choi, K.S. The relationship between chronotype and sleep quality in Korean firefighters. Clin. Psychopharmacol. Neurosci. 2015, 13, 201–208. [Google Scholar] [CrossRef]
- Lian, S.; Liu, Q.Q.; Sun, X.J.; Zhou, Z.K. Mobile Phone Addiction and College Students’Procrastination: Analysis of a Moderated Mediation Model. Psychol. Dev. Educ. 2018, 34, 595–604. [Google Scholar]
- Nauts, S.; Kamphorst, B.A.; Stut, W.; Ridder, D.T.D.D.; Anderson, J.H. The explanations people give for going to bed late: A qualitative study of the varieties of bedtime procrastination. Behav. Sleep Med. 2019, 17, 753–762. [Google Scholar] [CrossRef]
- Valshtein, T.J.; Oettingen, G.; Gollwitzer, P.M. Using mental contrasting with implementation intentions to reduce bedtime procrastination: Two randomized trials. Psychol. Health 2019, 35, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.H. The research of college students’ sleep health consciousness and habits. Acta Univ. Med. Nanjing 2013, 55, 134–138. [Google Scholar]
- Kawasaki, Y.; Akamatsu, R.; Fujiwara, Y.; Omori, M.; Sugawara, M.; Yamazaki, Y.; Kobayashi, T. Later chronotype is associated with unhealthful plant-based diet quality in young Japanese women. Appetite 2021, 166, 105468. [Google Scholar] [CrossRef] [PubMed]
- Shimura, A.; Hideo, S.; Takaesu, Y.; Nomura, R.; Komada, Y.; Inoue, T. Comprehensive assessment of the impact of life habits on sleep disturbance, chronotype, and daytime sleepiness among high-school students. Sleep Med. 2018, 44, 12–18. [Google Scholar] [CrossRef]
- Feng, Y.; Meng, D.; Guo, J.; Zhao, Y.; Ma, X.; Zhu, L.; Mu, L. Bedtime procrastination in the relationship between self-control and depressive symptoms in medical students: From the perspective of sex differences. Sleep Med. 2022, 95, 84–90. [Google Scholar] [CrossRef]
- Türkarslan, K.K.; Okay, D.; Çevrim, M.; Bozo, Ö. Life is short, stay awake: Death anxiety and bedtime procrastination. J. Gen. Psychol. 2020, 147, 43–61. [Google Scholar] [CrossRef]
- Sirois, F.M.; Nauts, S.; Molnar, D.S. Self-Compassion and Bedtime Procrastination: An Emotion Regulation Perspective. Mindfulness 2019, 10, 434–445. [Google Scholar] [CrossRef]
- Bartel, K.A.; Gradisar, M.; Williamson, P. Protective and risk factors for adolescent sleep: A meta-analytic review. Sleep Med. Rev. 2015, 21, 72–85. [Google Scholar] [CrossRef]
- Woods, H.C.; Scott, H. Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. J. Adolesc. 2016, 51, 41–49. [Google Scholar] [CrossRef]
- Seoane, H.A.; Moschetto, L.; Orliacq, F.; Orliacq, J.; Serrano, E.; Perez-Lloret, S. Sleep disruption in medicine students and its relationship with impaired academic performance: A systematic review and meta-analysis. Sleep Med. Rev. 2020, 53, 101333. [Google Scholar] [CrossRef]


| Characteristics | n (%) |
|---|---|
| Gender | |
| Male | 808 (28.6%) |
| Female | 2014 (71.4%) |
| Age | |
| <20 | 1311 (46.5%) |
| ≥20 | 1511 (53.5%) |
| Grade | |
| Freshman | 866 (30.7%) |
| Sophomore | 1108 (39.2%) |
| Junior | 629 (22.3%) |
| Senior | 180 (6.4%) |
| Postgraduate | 39 (1.4%) |
| Chronotype | |
| Morning-type | 765 (27.1%) |
| Intermediate-type | 1880 (66.6%) |
| Evening-type | 177 (6.3%) |
| Variables | Morning-Type | Intermediate-Type | Evening-Type | F | p-Value |
|---|---|---|---|---|---|
| Bedtime procrastination | 2.56 ± 0.62 | 3.00 ± 0.60 | 3.61 ± 0.61 | 254.67 | <0.001 |
| PSQI total score | 4.53 ± 2.64 | 5.99 ± 2.73 | 7.56 ± 3.20 | 116.37 | <0.001 |
| Subjective sleep quality | 0.83 ± 0.65 | 1.16 ± 0.71 | 1.41 ± 0.82 | 81.11 | <0.001 |
| Sleep disturbance | 0.84 ± 0.58 | 0.98 ± 0.55 | 1.08 ± 0.60 | 20.69 | <0.001 |
| Sleep efficiency | 0.41 ± 0.72 | 0.51 ± 0.81 | 0.69 ± 0.97 | 9.63 | <0.001 |
| Sleep latency | 1.03 ± 0.87 | 1.35 ± 0.95 | 1.71 ± 1.08 | 45.93 | <0.001 |
| Sleep duration | 0.45 ± 0.54 | 0.58 ± 0.56 | 0.66 ± 0.67 | 18.83 | <0.001 |
| Hypnotic medication | 0.03 ± 0.25 | 0.05 ± 0.29 | 0.12 ± 0.49 | 6.59 | <0.01 |
| Daytime dysfunction | 0.94 ± 0.85 | 1.36 ± 0.88 | 1.88 ± 0.95 | 101.46 | <0.001 |
| Sleep hygiene awareness | 55.80 ± 10.55 | 55.71 ± 8.57 | 56.10 ± 7.14 | 0.16 | 0.849 |
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| 1. Gender | — | — | — | ||||
| 2. Age | 19.77 | 1.41 | 0.12 *** | — | |||
| 3. MEQ | 53.95 | 7.65 | 0.09 *** | 0.01 | — | ||
| 4. BPS | 2.92 | 0.66 | −0.08 *** | 0.01 | −0.47 *** | — | |
| 5. PSQI | 5.69 | 2.85 | −0.07 *** | 0.06 ** | −0.33 *** | 0.42 *** | — |
| 6. SHA | 55.76 | 9.08 | −0.09 *** | −0.24 | −0.02 | −0.03 | 0.06 ** |
| Predictors | Model 1 (PSQI) | Model 2 (BPS) | Model 3 (PSQI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| β | t | 95% CI | β | t | 95% CI | β | t | 95% CI | |
| Gender | −0.04 | −2.48 * | [−0.18, −0.20] | −0.04 | −2.18 * | [−0.15, −0.01] | −0.03 | −1.88 | [−0.14, 0.00] |
| Age | 0.07 | 3.98 *** | [0.03, 0.08] | 0.02 | 1.37 | [−0.01, 0.04] | 0.06 | 3.74 *** | [0.02, 0.07] |
| MEQ | −0.33 | −18.28 *** | [−0.36, −0.29] | −0.46 | −27.60 *** | [−0.50, −0.43] | −0.17 | −8.89 *** | [−0.21, −0.13] |
| BPS | 0.34 | 17.79 *** | [0.30, 0.38] | ||||||
| R2 | 0.11 121.18 *** | 0.22 261.61 *** | 0.20 180.16 *** | ||||||
| F | |||||||||
| Variables | Model 1 (Outcome: BPS) | Model 2 (Outcome: PSQI) | ||||||
|---|---|---|---|---|---|---|---|---|
| β | SE | t | 95% CI | β | SE | t | 95% CI | |
| Gender | −0.04 | 0.04 | −2.54 * | [−0.08, −0.01] | −0.02 | 0.04 | −1.43 | [−0.06, 0.01] |
| Age | 0.02 | 0.01 | 1.44 | [−0.01, 0.06] | 0.06 | 0.01 | 3.76 *** | [0.03, 0.10] |
| MEQ | −0.45 | 0.02 | −27.15 *** | [−0.49, −0.42] | −0.17 | 0.02 | −8.87 *** | [−0.21, −0.13] |
| SHA | −0.02 | 0.02 | −0.97 | [−0.05, 0.02] | 0.06 | 0.02 | 3.41 ** | [0.03, 0.09] |
| MEQ × SHA | −0.11 | 0.02 | −6.57 *** | [−0.14, −0.08] | 0.05 | 0.02 | 2.73 ** | [0.02, 0.09] |
| BPS | 0.35 | 0.02 | 17.30 *** | [0.31, 0.39] | ||||
| BPS × SHA | 0.01 | 0.02 | 0.36 | [−0.03, 0.05] | ||||
| R2 | 0.23 169.62 *** | 0.21 107.47 *** | ||||||
| F | ||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Y.; Huang, J.; Yang, M. Association between Chronotype and Sleep Quality among Chinese College Students: The Role of Bedtime Procrastination and Sleep Hygiene Awareness. Int. J. Environ. Res. Public Health 2023, 20, 197. https://doi.org/10.3390/ijerph20010197
Zhu Y, Huang J, Yang M. Association between Chronotype and Sleep Quality among Chinese College Students: The Role of Bedtime Procrastination and Sleep Hygiene Awareness. International Journal of Environmental Research and Public Health. 2023; 20(1):197. https://doi.org/10.3390/ijerph20010197
Chicago/Turabian StyleZhu, Yingying, Jiahao Huang, and Minqi Yang. 2023. "Association between Chronotype and Sleep Quality among Chinese College Students: The Role of Bedtime Procrastination and Sleep Hygiene Awareness" International Journal of Environmental Research and Public Health 20, no. 1: 197. https://doi.org/10.3390/ijerph20010197
APA StyleZhu, Y., Huang, J., & Yang, M. (2023). Association between Chronotype and Sleep Quality among Chinese College Students: The Role of Bedtime Procrastination and Sleep Hygiene Awareness. International Journal of Environmental Research and Public Health, 20(1), 197. https://doi.org/10.3390/ijerph20010197





