Predictors of Depression among Individuals Receiving the Basic Livelihood Security Program Benefits in Korea: A Study Based on the Sixth and Seventh Korea National Health and Nutrition Examination Survey (2013–2018)
Abstract
1. Introduction
2. Methods
2.1. Study Design
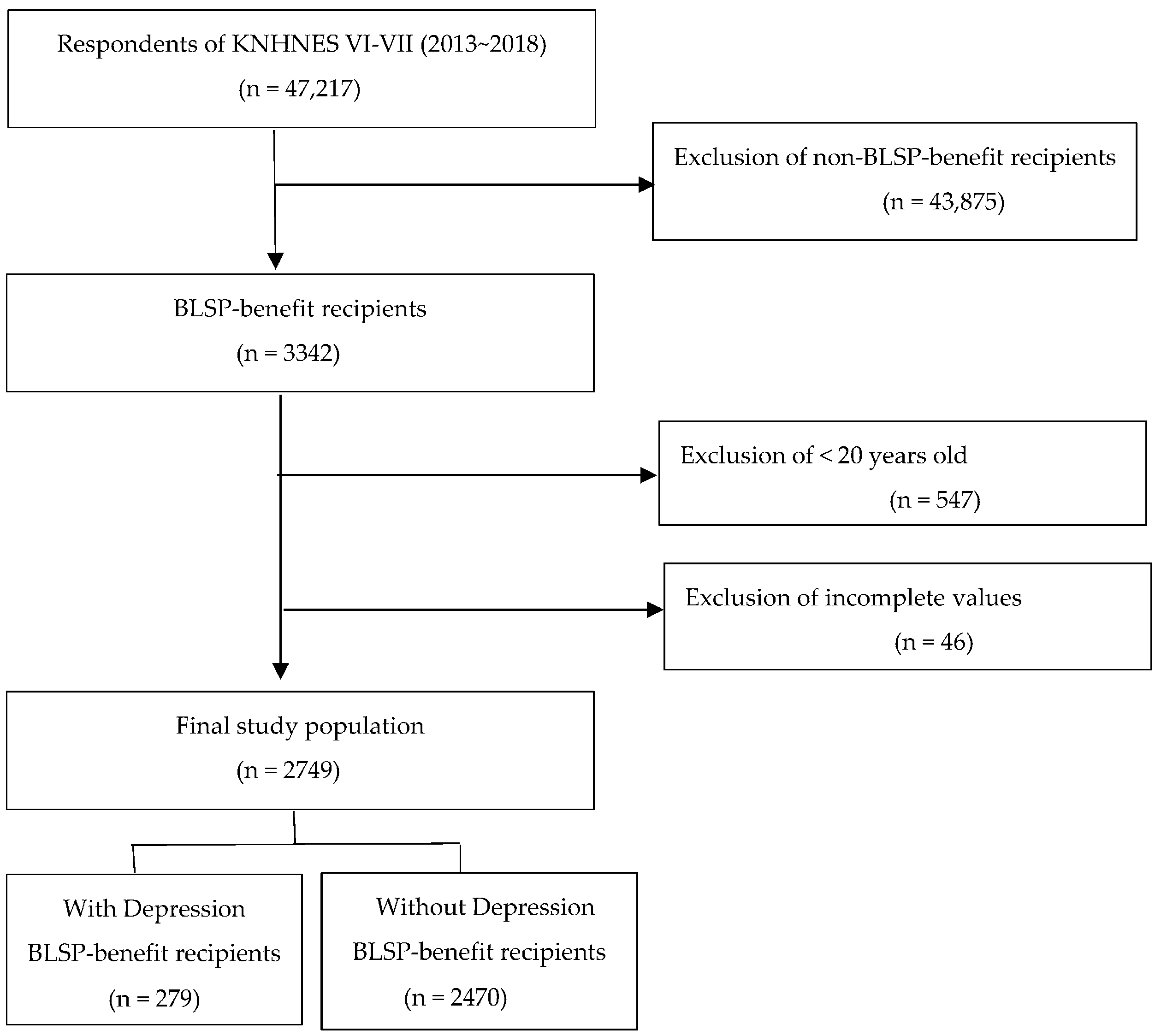
2.2. Study Population
2.3. Instruments
2.3.1. General Characteristics
2.3.2. Oral Health Practices
2.3.3. Depression Score: Patient Health Questionnaire-9
2.4. Ethical Considerations
2.5. Data Analysis
3. Results
3.1. General Characteristics of BLPS-Benefit Recipients according to Depression
3.2. Differences in Oral Health Practices according to Depression
3.3. Predictors of Depression in BLSP-Benefit Recipients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Marmot, M.G. Status syndrome: A challenge to medicine. JAMA 2006, 295, 304–1307. [Google Scholar] [CrossRef] [PubMed]
- The 4th Health Plan 2020 Trend Report 2017; Korea Health Promotion Institute: Seoul, Republic of Korea, 2016; pp. 10–13.
- Park, B.H. Comparative study of Speenhamland of England, family assistance plan of USA, and national basic livelihood security program of Korea. Soc. Welf. Policy 2016, 43, 159–189. [Google Scholar] [CrossRef]
- Basic Livelihood Security Program: Benefit Recipients & Payment. Available online: https://mohw.go.kr/eng/hs/hs0109.jsp?PAR_MENU_ID=1006&MENU_ID=100609 (accessed on 30 March 2022).
- Jeon, B.; Noguchi, H.; Kwon, S.; Ito, T.; Tamiya, N. Disability, poverty, and role of the basic livelihood security system on health services utilization among the elderly in South Korea. Soc. Sci. Med. 2017, 178, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Feng, Z.; Li, Q.; Zhou, L.; Chen, Z.; Yin, W. The relationship between depressive symptoms and activity of daily living disability among the elderly: Results from the China Health and Retirement Longitudinal Study (CHARLS). Public Health 2021, 198, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.W.; Haregu, T.N.; He, L.; Lu, S.; Katar, A.; Wang, H.; Zhang, L. The effect of multimorbidity on functional limitations and depression amongst middle-aged and older population in China: A nationwide longitudinal study. Age Ageing 2020, 50, 190–197. [Google Scholar] [CrossRef]
- Manchia, M.; Gathier, A.W.; Yapici-Eser, H.; Schmidt, M.V.; De Quervain, D.; Van Amelsvoort, T.; Vinkers, C.H. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves. Eur. Neuropsychopharmacol. 2022, 55, 22–83. [Google Scholar] [CrossRef]
- Park, S.G.; Lee, B.H. The study of psychological characteristics of the indigent population. Korean J. Couns. Psychother. 2004, 16, 813–824. [Google Scholar]
- Nuggerud-Galeas, S.; Oliván Blázquez, B.; Perez Yus, M.C.; Valle-Salazar, B.; Aguilar-Latorre, A.; Magallón Botaya, R. Factors associated with depressive episode recurrences in primary care: A retrospective, descriptive study. Front. Psychol. 2020, 11, 1230. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. 2022 Corona 19 National Mental Health Survey. Available online: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=372545 (accessed on 7 May 2022).
- Knorst, J.K.; Sfreddo, C.S.; de FMeira, G.; Zanatta, F.B.; Vettore, M.V.; Ardenghi, T.M. Socioeconomic status and oral health-related quality of life: A systematic review and meta-analysis. Community Dent. Oral Epidemiol. 2020, 49, 95–102. [Google Scholar] [CrossRef]
- Daly, B.; Batchelor, P.; Treasure, E.; Watt, R. Essential Dental Public Health; Oxford University Press: Oxford, UK, 2005; pp. 21–32. [Google Scholar]
- Spanemberg, J.C.; Cardoso, J.A.; Slob, E.M.G.B.; López-López, J. Quality of life related to oral health and its impact in adults. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 234–239. [Google Scholar] [CrossRef]
- Baniasadi, K.; Armoon, B.; Higgs, P.; Bayat, A.H.; Mohammadi Gharehghani, M.A.; Hemmat, M.; Schroth, R.J. The association of oral health status and socio-economic determinants with oral health-related quality of life among the elderly: A systematic review and meta-analysis. Int. J. Dent. Hyg. 2021, 19, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Skośkiewicz-Malinowska, K.; Malicka, B.; Ziętek, M.; Kaczmarek, U. Oral health condition and occurrence of depression in the elderly. Medicine 2018, 97, e12490. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.R.; Wee, H.; Kim, S.J. Lifestyle, depression, and health related quality of life among women in Jeju province. J. Korean Acad. Community Health Nurs. 2010, 21, 148–155. [Google Scholar] [CrossRef]
- Gazzaz, A.Z.; Carpiano, R.M.; Aleksejuniene, J. Socioeconomic status, social support, and oral health-risk behaviors in Canadian adolescents. J. Public Health Dent. 2021, 81, 316–326. [Google Scholar] [CrossRef]
- Maier, A.; Riedel-Heller, S.G.; Pabst, A.; Luppa, M. Risk factors and protective factors of depression in older people 65+. A systematic review. PLoS ONE 2021, 16, e0251326. [Google Scholar] [CrossRef]
- Oh, D.N.; Kim, C.G. The factor associated with depression in the elderly male: Based on the 5th Korea National Health and Nutrition Examination Survey. Korean J. Adult Nurs. 2015, 27, 583–593. [Google Scholar] [CrossRef]
- Lee, E.J. Association between health-related characteristics of the middle-aged between men and women, and oral health-related characteristics on depressive symptoms (PHQ-9). Korean J. Health Serv. Manag. 2017, 11, 179–188. [Google Scholar] [CrossRef]
- Jung, J.A.; Kim, J.; Seong, M.G. The effect of oral health status and oral health behaviors on depression and stress awareness in Korean adults: The 8th Korea National Health and Nutrition Examination Survey (2019). Health Welf. 2019, 23, 137–157. [Google Scholar] [CrossRef]
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Oh, K. Data resource profile: The Korea national health and nutrition examination survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef]
- Villarroel, M.A.; Terlizzi, E.P. Symptoms of Depression among Adults: United States, 2019; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD, USA, 2020.
- Brennan, D.S.; Spencer, A.J.; Roberts-Thomson, K.F. Socioeconomic and psychosocial associations with oral health impact and general health. Community Dent. Oral Epidermial 2019, 47, 32–39. [Google Scholar] [CrossRef]
- Solis, A.C.O.; Lotufo, R.F.M.; Pannuti, C.M.; Brunheiro, E.C.; Marques, A.H.; Lotufo-Neto, F. Association of periodontal disease to anxiety and depression symptoms, and psychosocial stress factors. J. Clin. Periodontol. 2004, 31, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A new depression diagnostic and severity measure. Psychiatr. Ann. 2002, 32, 509–521. [Google Scholar] [CrossRef]
- Han, C.S.; Jo, S.A.; Kwak, J.H.; Pae, C.U.; Steffens, D.; Jo, I.H.; Park, M.H. Validation of the patient health questionnaire-9 Korean version in the elderly population: The Ansan Geriatric study. Compr. Psychiatry 2008, 49, 218–223. [Google Scholar] [CrossRef]
- Park, S.H.; Jae, Y.M.; Jang, S.H.; Choi, J.H.; Lee, G.H. What physical activities can help you feel better? Analysis based on the 2016 korean national health and nutrition examination survey. Mood Emot. 2020, 18, 18–27. [Google Scholar] [CrossRef]
- WHO. Depression 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 13 September 2021).
- Choi, H.S.; Lee, J.E. Factors affecting depression in middle-aged and elderly men living alone: A cross-sectional path analysis model. Am. J. Men’s Health 2022, 16, 15579883221078134. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.R.; Park, J.H.; Park, H.Y. Analysis of factors affecting depression in older adults in South Korea. Int. J. Environ. Res. Public Health 2021, 18, 9887. [Google Scholar] [CrossRef] [PubMed]
- Chu, J.E.; Lee, J.M.; Cho, H.I.; Park, Y.J. Relationships between obesity, blood and urinary compositions, and dietary habits and depressed mood in Koreans at the age of 40, a life transition period. J. Nutr. Health 2013, 46, 261–275. [Google Scholar] [CrossRef][Green Version]
- Yang, Y.J. The study on the factors affecting depression experiences of local resident in Gwangju. J. Korea Entertain. Ind. Assoc. 2022, 16, 243–251. [Google Scholar] [CrossRef]
- Hur, J.Y.; Yi, Y.J.; Lee, K.J.; Lim, H.G. Effects of health characteristics on depression of elderly beneficiaries of the National Basic Livelihood Scheme. J. Korean Public Health Nurs. 2013, 27, 327–337. [Google Scholar] [CrossRef][Green Version]
- Lee, K.H. Oral health and oral health behavior as risk factors for depression. Sci. Emot. Sensib. 2021, 24, 17–26. [Google Scholar] [CrossRef]
- Won, S. The role of poverty on depression and self-rated health of older adults living alone: The mediating effect of social participation. J. Korea Acad. Indu. Coop. Soci. 2020, 21, 520–526. [Google Scholar] [CrossRef]
- Jang, S.A.; Kim, Y.S. Effects of stress and depression on oral health status of middle aged population on Korea. Hanyang Univ. J. Aging Soci. 2013, 4, 71–90. [Google Scholar]
- Lim, S.A. Relationship between oral health in adults and chewing difficulty: The 7th Korea National Health and Nutrition Examination Survey. J. Korean Soc. Dent. Hyg. 2021, 21, 383–391. [Google Scholar] [CrossRef]
| Variable | All (n = 2749) | With Depression (n = 279) | Without Depression (n = 2470) | χ2 or t | p |
|---|---|---|---|---|---|
| n (%) or Mean ± SD | |||||
| Age (years) | 56.26 ± 18.02 | 50.73 ± 22.10 | 50.33 ± 17.51 | 20.04 | <0.001 |
| 20–39 | 508 | 32 (11.5) | 476 (19.3) | ||
| 40–64 | 1064 | 142 (50.9) | 922 (37.3) | ||
| 65–74 | 584 | 62 (22.2) | 522 (21.1) | ||
| ≥75 | 593 | 43 (15.4) | 550 (22.3) | ||
| Sex | 13.39 | <0.001 | |||
| Male | 1047 | 75 (26.9) | 972 (39.4) | ||
| Female | 1702 | 204 (73.1) | 1498 (60.6) | ||
| Marital status | 5.21 | 0.022 | |||
| Married | 2203 | 238 (85.3) | 1965 (79.6) | ||
| Unmarried | 546 | 41 (14.7) | 505 (20.4) | ||
| Education level | 23.75 | <0.001 | |||
| Elementary school below | 1475 | 128 (45.9) | 1347 (54.5) | ||
| Middle school | 318 | 55 (19.7) | 263 (10.6) | ||
| High school | 660 | 73 (26.2) | 587 (23.8) | ||
| ≥College | 296 | 23 (8.2) | 273 (11.1) | ||
| Economic activity | 15.99 | <0.001 | |||
| Yes | 968 | 68 (24.4) | 900 (36.4) | ||
| No | 1781 | 211 (75.6) | 1570 (63.6) | ||
| Daily function | 59.30 | <0.001 | |||
| Good | 1972 | 161 (57.7) | 1811 (73.3) | ||
| Not good | 718 | 97 (34.8) | 621 (25.1) | ||
| Poor | 59 | 21 (7.5) | 38 (1.5) | ||
| Moderate-intensity physical activity | 8.14 | 0.004 | |||
| Yes | 169 | 28 (10.0) | 141 (5.7) | ||
| No | 2580 | 251 (90.0) | 2329 (94.3) | ||
| Smoking | 4.16 | 0.125 | |||
| Current Smoker | 857 | 74 (26.5) | 783 (31.7) | ||
| Ex-smoker | 478 | 46 (16.5) | 432 (17.5) | ||
| Non-smoker | 1414 | 159 (57.0) | 1255 (50.8) | ||
| Alcohol drinking | 0.70 | 0.403 | |||
| Yes | 2276 | 226 (81.0) | 2050 (83.0) | ||
| No | 473 | 53 (19.0) | 420 (17.0) | ||
| Perceived health status | 45.35 | <0.001 | |||
| Good | 424 | 17 (6.1) | 407 (16.5) | ||
| Moderate | 1074 | 85 (30.5) | 989 (40.4) | ||
| Poor | 1251 | 177 (63.4) | 1074 (43.5) | ||
| Perceived oral health status | 1.40 | 0.498 | |||
| Good | 134 | 10 (3.6) | 124 (5.0) | ||
| Moderate | 428 | 41 (14.7) | 387 (15.7) | ||
| Not good | 2187 | 228 (81.7) | 1959 (79.3) | ||
| PHQ-9 Score | 1.17 ± 0.44 | 1.48 ± 0.69 | 1.14 ± 0.39 | −0.89 | <0.001 |
| Minimal, 0–4 | 2356 | 178 (63.8) | 2178 (88.2) | ||
| Mild to moderate, 5–14 | 319 | 69 (24.7) | 250 (10.1) | ||
| Severe, ≥15 | 74 | 32 (11.5) | 42 (1.7) | ||
| Variable | All (n = 2749) | With Depression (n = 279) | Without Depression (n = 2470) | χ2 | p |
|---|---|---|---|---|---|
| n (%), M ± SD | n (%) | n (%) | |||
| Dental visit experience in a year | 5.76 | 0.016 | |||
| Yes | 532 (19.4) | 69 (24.7) | 463 (18.7) | ||
| No | 2217 (80.6) | 210 (75.3) | 2007 (81.3) | ||
| Using oral hygiene supplies | 7.26 | 0.007 | |||
| Yes | 878 (31.9) | 109 (39.1) | 769 (31.1) | ||
| No | 1871 (68.1) | 170 (60.9) | 1701 (68.9) | ||
| Preventive dental treatment (per year) | 2.71 | 0.099 | |||
| Yes | 438 (15.9) | 54 (19.4) | 2086 (84.5) | ||
| No | 2311 (84.1) | 225 (80.6) | 384 (15.5) | ||
| Frequency of tooth brushing (time/day) | 2.06 ± 1.22 | 10.34 | 0.006 | ||
| 0 | 370 (13.5) | 21 (7.5) | 349 (14.1) | ||
| 1–2 | 1439 (52.3) | 149 (53.4) | 1290 (52.2) | ||
| ≥3 | 940 (34.2) | 109 (39.1) | 831 (33.6) |
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Exp(B) | 95% CI | Exp(B) | 95% CI | |||
| Lower | Upper | Lower | Upper | |||
| Age | 1.45 | 1.07 | 1.97 | 1.37 | 1.01 | 1.87 |
| Sex † | 1.72 | 1.29 | 2.29 | 1.74 | 1.29 | 2.24 |
| Marital status† | 1.05 | 0.68 | 1.63 | 1.04 | 0.67 | 1.61 |
| Education † | 1.81 | 0.36 | 0.65 | 1.66 | 1.21 | 2.27 |
| Daily activities † | 0.75 | 0.55 | 1.01 | 0.89 | 0.63 | 1.32 |
| Moderate-intensity physical activity † | 0.47 | 0.30 | 0.74 | 0.47 | 0.30 | 0.73 |
| Economic activity † | 0.36 | 0.27 | 0.49 | 0.73 | 0.54 | 1.00 |
| Perceived health status † | 0.37 | 0.22 | 0.62 | 0.36 | 0.22 | 0.61 |
| Dental visit experience in past year † | 1.26 | 0.92 | 1.73 | |||
| Using oral hygiene supplies † | 1.20 | 0.90 | 1.58 | |||
| Frequency of tooth brushing † | 1.10 | 0.88 | 1.37 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, H.; Shim, J. Predictors of Depression among Individuals Receiving the Basic Livelihood Security Program Benefits in Korea: A Study Based on the Sixth and Seventh Korea National Health and Nutrition Examination Survey (2013–2018). Int. J. Environ. Res. Public Health 2023, 20, 194. https://doi.org/10.3390/ijerph20010194
Choi H, Shim J. Predictors of Depression among Individuals Receiving the Basic Livelihood Security Program Benefits in Korea: A Study Based on the Sixth and Seventh Korea National Health and Nutrition Examination Survey (2013–2018). International Journal of Environmental Research and Public Health. 2023; 20(1):194. https://doi.org/10.3390/ijerph20010194
Chicago/Turabian StyleChoi, Heejung, and Jaelan Shim. 2023. "Predictors of Depression among Individuals Receiving the Basic Livelihood Security Program Benefits in Korea: A Study Based on the Sixth and Seventh Korea National Health and Nutrition Examination Survey (2013–2018)" International Journal of Environmental Research and Public Health 20, no. 1: 194. https://doi.org/10.3390/ijerph20010194
APA StyleChoi, H., & Shim, J. (2023). Predictors of Depression among Individuals Receiving the Basic Livelihood Security Program Benefits in Korea: A Study Based on the Sixth and Seventh Korea National Health and Nutrition Examination Survey (2013–2018). International Journal of Environmental Research and Public Health, 20(1), 194. https://doi.org/10.3390/ijerph20010194






