Investigation of Psychological Stress and Sleep Quality of Emergency Medical Technicians in Taiwan Fire Department during the COVID-19 Pandemic
Abstract
1. Introduction
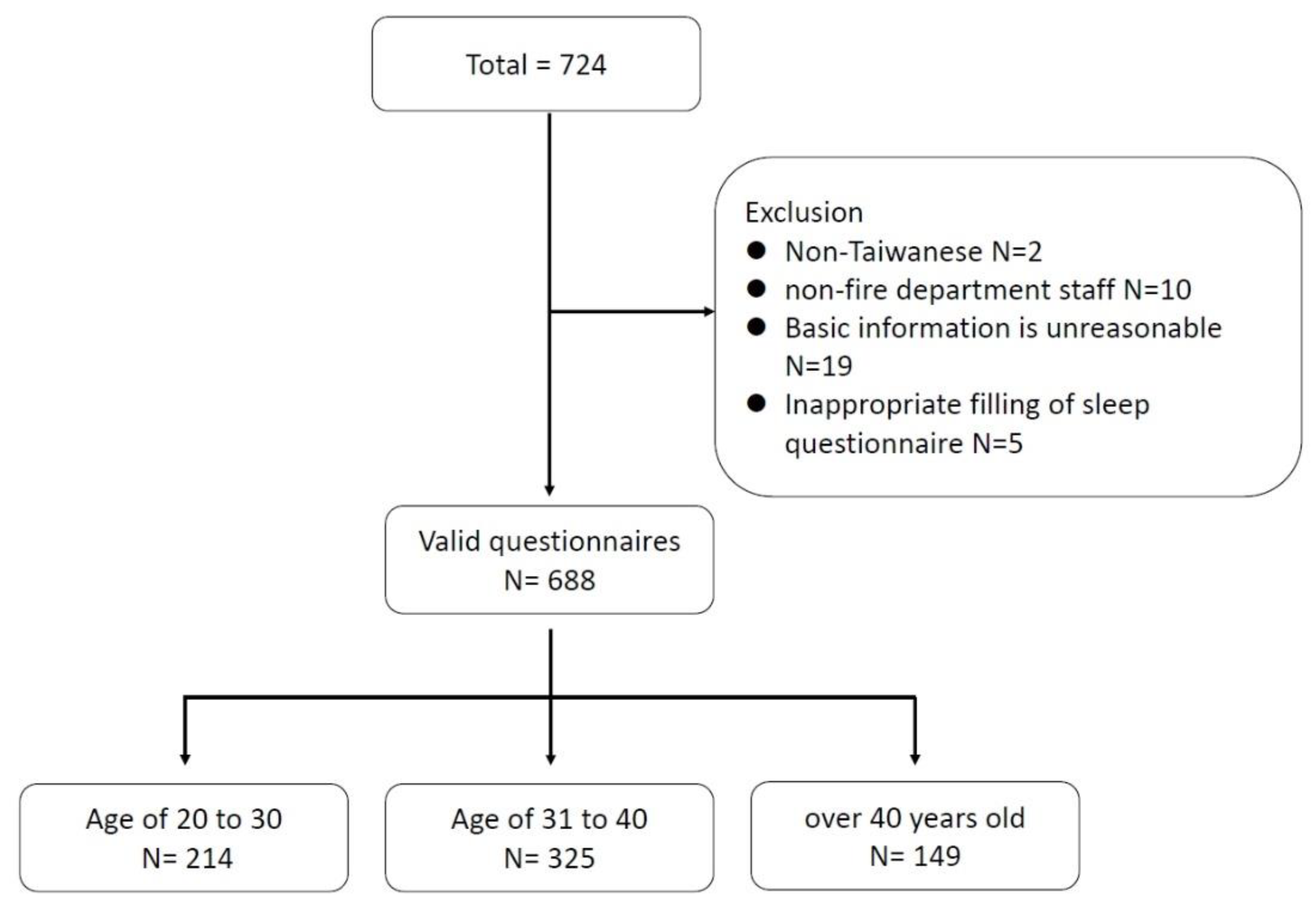
2. Materials and Methods
2.1. Questionnaire Background
2.2. Questionnaire Design
2.3. DASS-21
2.4. Variables
2.5. PSQI
2.6. AUDIT
2.7. Statistics
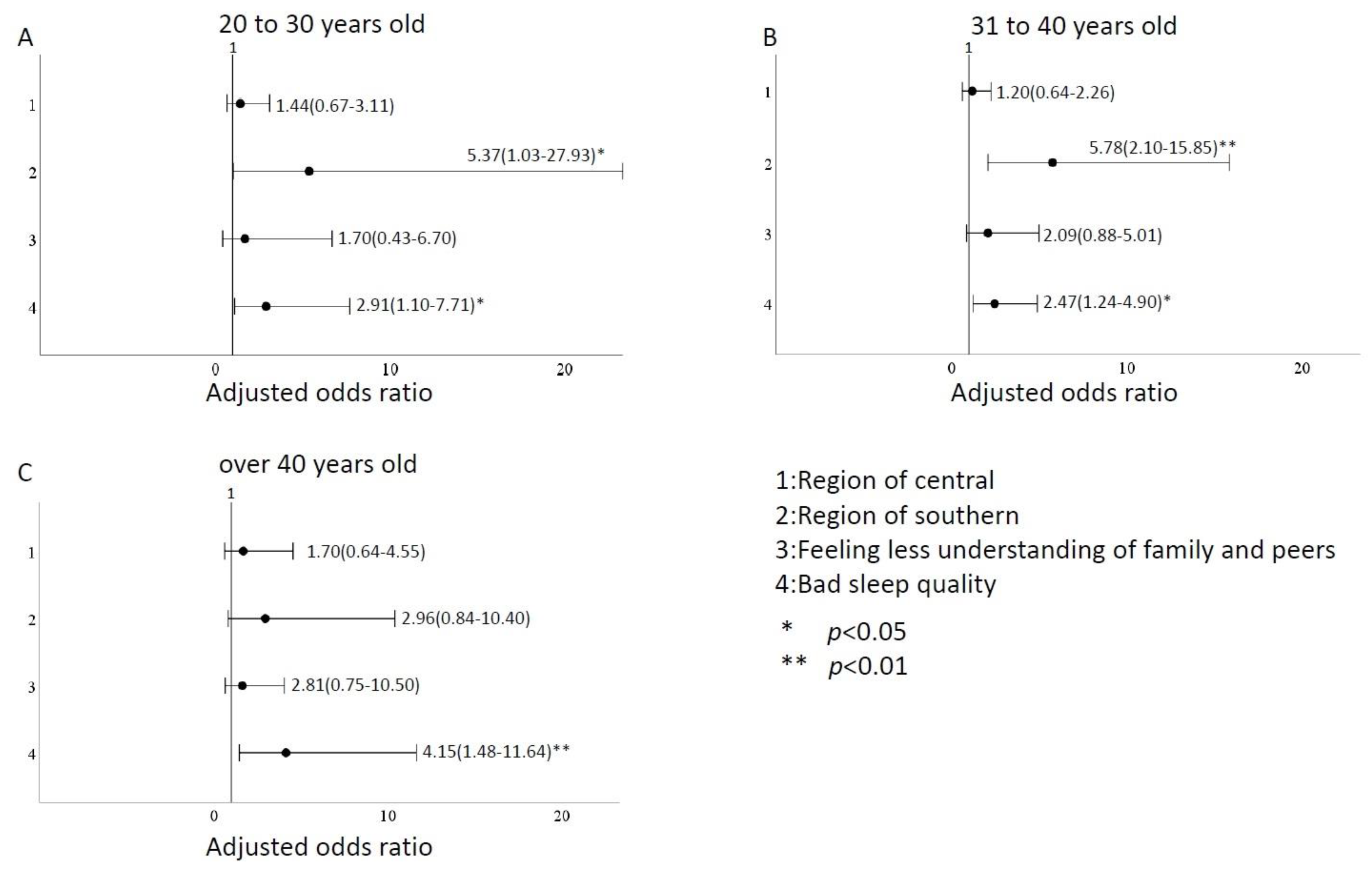
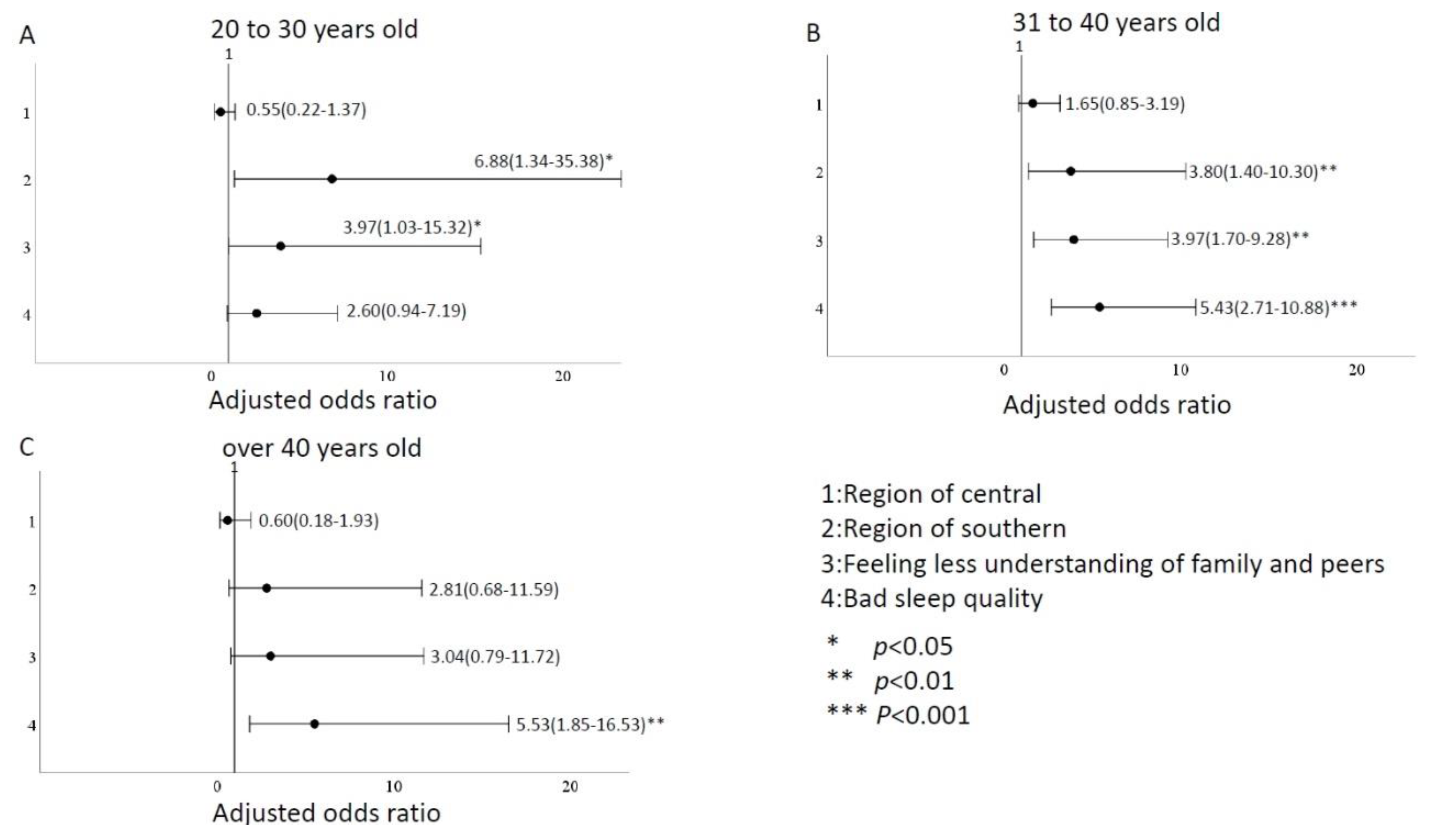
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549. [Google Scholar] [CrossRef] [PubMed]
- García-Iglesias, J.J.; Gómez-Salgado, J.; Martín-Pereira, J.; Fagundo-Rivera, J.; Ayuso-Murillo, D.; Martínez-Riera, J.R.; Ruiz-Frutos, C. Impact of SARS-CoV-2 (COVID-19) on the mental health of healthcare professionals: A systematic review. Rev. Esp. Salud. Publica. 2020, 94, e202007088. [Google Scholar] [PubMed]
- Soto-Cámara, R.; Navalpotro-Pascual, S.; Jiménez-Alegre, J.J.; García-Santa-Basilia, N.; Onrubia-Baticón, H.; Navalpotro-Pascual, J.M.; Thuissard, I.J.; Fernández-Domínguez, J.J.; Matellán-Hernández, M.P.; Pastor-Benito, E.; et al. Influence of the Cumulative Incidence of COVID-19 Cases on the Mental Health of the Spanish Out-of-Hospital Professionals. J. Clin. Med. 2022, 11, 2227. [Google Scholar] [CrossRef] [PubMed]
- Eftekhar Ardebili, M.; Naserbakht, M.; Bernstein, C.; Alazmani-Noodeh, F.; Hakimi, H.; Ranjbar, H. Healthcare providers experience of working during the COVID-19 pandemic: A qualitative study. Am. J. Infect. Control. 2021, 49, 547–554. [Google Scholar] [CrossRef]
- Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Wessely, S. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ 2020, 368, m1211. [Google Scholar] [CrossRef]
- McAlonan, G.M.; Lee, A.M.; Cheung, V.; Cheung, C.; Tsang, K.W.; Sham, P.C.; Chua, S.E.; Wong, J.G. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry 2007, 52, 241–247. [Google Scholar] [CrossRef]
- Tam, C.W.; Pang, E.P.; Lam, L.C.; Chiu, H.F. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004, 34, 1197–1204. [Google Scholar] [CrossRef]
- Lehmann, M.; Bruenahl, C.A.; Lowe, B.; Addo, M.M.; Schmiedel, S.; Lohse, A.W.; Schramm, C. Ebola and psychological stress of health care professionals. Emerg. Infect. Dis. 2015, 21, 913–914. [Google Scholar] [CrossRef]
- Matua, G.A.; Wal, D.M. Living Under the Constant Threat of Ebola: A Phenomenological Study of Survivors and Family Caregivers During an Ebola Outbreak. J. Nurs. Res. 2015, 23, 217–224. [Google Scholar] [CrossRef]
- Chew, N.W.; Lee, G.K.; Tan, B.Y.; Jing, M.; Goh, Y.; Ngiam, N.J.; Yeo, L.L.; Ahmad, A.; Khan, F.A.; Shanmugam, G.N.; et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain. Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef]
- Hummel, S.; Oetjen, N.; Du, J.; Posenato, E.; De Almeida, R.M.; Losada, R.; Ribeiro, O.; Frisardi, V.; Hopper, L.; Rashid, A.; et al. Mental Health Among Medical Professionals During the COVID-19 Pandemic in Eight European Countries: Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e24983. [Google Scholar] [CrossRef] [PubMed]
- Lange, T.; Dimitrov, S.; Born, J. Effects of sleep and circadian rhythm on the human immune system. Ann. N. Y. Acad. Sci. 2010, 1193, 48–59. [Google Scholar] [CrossRef] [PubMed]
- Yao, K.W.; Yu, S.; Cheng, S.P.; Chen, I.J. Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults. J Nurs. Res. 2008, 16, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Abdellah, M.M.; Khalil, M.F.; Alhafiz, A. Prevalence of Poor Sleep Quality Among Physicians During the COVID-19 Pandemic. Cureus 2021, 13, e12948. [Google Scholar] [CrossRef]
- Alnofaiey, Y.H.; Alshehri, H.A.; Alosaimi, M.M.; Alswat, S.H.; Alswat, R.H.; Alhulayfi, R.M.; Alghamdi, M.A.; Alsubaie, R.M. Sleep disturbances among physicians during COVID-19 pandemic. BMC Res. Notes 2020, 13, 493. [Google Scholar] [CrossRef]
- Brito-Marques, J.; Franco, C.M.R.; Brito-Marques, P.R.; Martinez, S.C.G.; Prado, G.F.D. Impact of COVID-19 pandemic on the sleep quality of medical professionals in Brazil. Arq. Neuropsiquiatr. 2021, 79, 149–155. [Google Scholar] [CrossRef]
- Kim-Godwin, Y.S.; Lee, M.H.; Logan, J.G.; Liu, X. Factors Influencing Sleep Quality among Female Staff Nurses during the Early COVID-19 Pandemic in the United States. Int. J. Environ. Res. Public Health 2021, 18, 4827. [Google Scholar] [CrossRef]
- Saracoglu, K.T.; Simsek, T.; Kahraman, S.; Bombaci, E.; Sezen, Ö.; Saracoglu, A.; Demirhan, R. The Psychological Impact of COVID-19 Disease is more Severe on Intensive Care Unit Healthcare Providers: A Cross-sectional Study. Clin. Psychopharmacol. Neurosci. 2020, 18, 607–615. [Google Scholar] [CrossRef]
- Tosun, A.; Tosun, H.; Odul Ozkaya, B.; Erdogan, Z.; Gul, A. Sleep Quality and Depression Level in Nurses in COVID-19 Pandemic. Omega (Westport) 2022, 302228221123159. [Google Scholar] [CrossRef]
- Bilgic, S.; Celikkalp, U.; Misirli, C. Stress level and sleep quality of nurses during the COVID-19 pandemic. Work 2021, 70, 1021–1029. [Google Scholar] [CrossRef]
- Eksi, A.; Gumussoy, S.; Utanir Altay, S.; Kirazli, G. Effect of the COVID-19 pandemic on violence against pre-hospital emergency health workers. Work 2022, 73, 1103–1108. [Google Scholar] [CrossRef] [PubMed]
- Hitch, D.; Booth, S.; Wynter, K.; Said, C.M.; Haines, K.; Rasmussen, B.; Holton, S. Worsening general health and psychosocial wellbeing of Australian hospital allied health practitioners during the COVID-19 pandemic. Aust. Health Rev. 2022. [Google Scholar] [CrossRef] [PubMed]
- Labrague, L.J. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. J. Nurs. Manag. 2021, 29, 1893–1905. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Ponce, D.; Amat-Traconis, M.A.; Cala-Rosabal, L.Y.; Chapan-Xolio, E.; Valenzuela-Velazquez, L.; Lecourtois-Amezquita, M.G. Psychological repercussions on nursing staff due to the COVID-19 pandemic: A cross-sectional study. J. Healthc. Qual. Res. 2022. [Google Scholar] [CrossRef]
- Vujanovic, A.A.; Lebeaut, A.; Leonard, S. Exploring the impact of the COVID-19 pandemic on the mental health of first responders. Cogn. Behav. Ther. 2021, 50, 320–335. [Google Scholar] [CrossRef]
- Greenberg, N.; Weston, D.; Hall, C.; Caulfield, T.; Williamson, V.; Fong, K. Mental health of staff working in intensive care during COVID-19. Occup. Med. (Lond.) 2021, 71, 62–67. [Google Scholar] [CrossRef]
- Lamb, D.; Gnanapragasam, S.; Greenberg, N.; Bhundia, R.; Carr, E.; Hotopf, M.; Razavi, R.; Raine, R.; Cross, S.; Dewar, A.; et al. Psychosocial impact of the COVID-19 pandemic on 4378 UK healthcare workers and ancillary staff: Initial baseline data from a cohort study collected during the first wave of the pandemic. Occup. Environ. Med. 2021, 78, 801–808. [Google Scholar] [CrossRef]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Babor, T.F.; Higgins-Biddle, J.C.; Saunders, J.B.; Monteiro, M.G. The Alcohol Use Disorders Identification Test; World Health Organization: Geneva, Switzerland, 2001; pp. 1–37.
- Mockel, L.; Gerhard, A.; Mohr, M.; Armbrust, C.I.; Mockel, C. Prevalence of pain, analgesic self-medication and mental health in German prehospital emergency medical service personnel: A nationwide survey pilot-study. Int. Arch. Occup. Environ. Health 2021, 94, 1975–1982. [Google Scholar] [CrossRef]
- Sabbaghi, M.; Miri, K.; Kahi, R.; Nia, M.N. Investigation of stress, anxiety, and depression levels of Pre Emergency Medicine personnel in eastern Iran during the COVID-19 pandemic. BMC Emerg. Med. 2022, 22, 97. [Google Scholar] [CrossRef] [PubMed]
- Varghese, A.; George, G.; Kondaguli, S.V.; Naser, A.Y.; Khakha, D.C.; Chatterji, R. Decline in the mental health of nurses across the globe during COVID-19: A systematic review and meta-analysis. J. Glob. Health 2021, 11, 05009. [Google Scholar] [CrossRef] [PubMed]
- Zheng, R.; Zhou, Y.; Fu, Y.; Xiang, Q.; Cheng, F.; Chen, H.; Xu, H.; Wu, X.; Feng, M.; Ye, L.; et al. Prevalence and associated factors of depression and anxiety among nurses during the outbreak of COVID-19 in China: A cross-sectional study. Int. J. Nurs. Stud. 2021, 114, 103809. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Liu, P.; Lei, G.F.; Tong, L.; Wang, H.; Zhang, X.Q. Sleep Quality and the Depression-Anxiety-Stress State of Frontline Nurses Who Perform Nucleic Acid Sample Collection During COVID-19: A Cross-Sectional Study. Psychol. Res. Behav. Manag. 2021, 14, 1889–1900. [Google Scholar] [CrossRef] [PubMed]
- Demartini, B.; Nistico, V.; D’Agostino, A.; Priori, A.; Gambini, O. Early Psychiatric Impact of COVID-19 Pandemic on the General Population and Healthcare Workers in Italy: A Preliminary Study. Front. Psychiatry 2020, 11, 561345. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.; Shakespeare-Finch, J.; Shochet, I. Organizational belongingness mediates the relationship between sources of stress and posttrauma outcomes in firefighters. Psychol. Trauma 2016, 8, 343–347. [Google Scholar] [CrossRef]
- Pinto, R.J.; Henriques, S.P.; Jongenelen, I.; Carvalho, C.; Maia, A.C. The Strongest Correlates of PTSD for Firefighters: Number, Recency, Frequency, or Perceived Threat of Traumatic Events? J. Trauma Stress 2015, 28, 434–440. [Google Scholar] [CrossRef]
- Stanley, I.H.; Hom, M.A.; Hagan, C.R.; Joiner, T.E. Career prevalence and correlates of suicidal thoughts and behaviors among firefighters. J. Affect Disord. 2015, 187, 163–171. [Google Scholar] [CrossRef]
- Steyn, R.; Vawda, N.; Wyatt, G.E.; Williams, J.K.; Madu, S.N. Posttraumatic stress disorder diagnostic criteria and suicidal ideation in a South African Police sample. Afr. J. Psychiatry (Johannesbg.) 2013, 16, 19–22. [Google Scholar] [CrossRef][Green Version]
- Bossarte, R.M.; Knox, K.L.; Piegari, R.; Altieri, J.; Kemp, J.; Katz, I.R. Prevalence and characteristics of suicide ideation and attempts among active military and veteran participants in a national health survey. Am. J. Public Health 2012, 102 (Suppl. 1), S38–S40. [Google Scholar] [CrossRef]
- Ursano, R.J.; Heeringa, S.G.; Stein, M.B.; Jain, S.; Raman, R.; Sun, X.; Chiu, W.T.; Colpe, L.J.; Fullerton, C.S.; Gilman, S.E.; et al. Prevalence and correlates of suicidal behavior among new soldiers in the U.S. Army: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Depress. Anxiety 2015, 32, 3–12. [Google Scholar] [CrossRef] [PubMed]

| Variable | Depression | Anxiety | Stress | ||||
|---|---|---|---|---|---|---|---|
| Mean (IQR) | p-Value | Mean (IQR) | p-Value | Mean (IQR) | p-Value | ||
| All | 11.4 (12.0) | 9.5 (12.0) | 14.5 (14.0) | ||||
| Region | North, East, and Islands N = 390 (56.7%) | 11.4 (14.5) | 0.032 * | 9.3 (12.0) | 0.012 * | 14.6 (14.0) | 0.015 * |
| Central N = 217 (31.5%) | 10.7 (14.0) | 8.8 (12.0) | 13.4 (16.0) | ||||
| Southern N = 81 (11.8%) | 13.3(13.0) | 12.0 (13.0) | 17.0 (17.0) | ||||
| Age | 20–30 years N = 214 (31.1%) | 8.4 (14.0) | <0.001 *** | 7.0 (10.0) | <0.001 *** | 11.7 (14.0) | <0.001 *** |
| 31–40 years N = 325 (47.2%) | 12.6 (14.0) | 10.4 (12.0) | 15.8 (14.0) | ||||
| >40 years N = 149 (21.7%) | 13.1 (12.0) | 10.6 (12.0) | 15.8 (15.0) | ||||
| Gender | Woman N = 36 (5.2%) | 13.5 (8.0) | 0.031 * | 11.7 (10.0) | 0.011 * | 17.0 (8.0) | 0.045 * |
| Male N = 652 (94.8%) | 11.3 (14.0) | 9.3 (12.0) | 14.4 (14.0) | ||||
| Marital status | Single N = 288 (41.9%) | 10.6 (14.0) | 0.067 | 8.6 (12.0) | 0.038 * | 13.5 (14.0) | 0.067 |
| Divorce N = 20 (2.9%) | 11.6 (15.0) | 9.8 (11.0) | 15.4 (18.5) | ||||
| Married N = 380 (55.2%) | 12.0 (14.0) | 10.1 (12.0) | 15.3 (14.0) | ||||
| Level of education | High school N = 21 (3.1%) | 8.3 (13.0) | 0.078 | 7.8 (11.0) | 0.123 | 12.0 (15.0) | 0.242 |
| College N = 270 (39.2%) | 10.6 (14.0) | 8.7 (6.0) | 13.9 (14.0) | ||||
| University N = 261 (37.9%) | 11.9 (14.0) | 10.1 (12.0) | 15.1 (14.0) | ||||
| Masters and Doctorate N = 136 (19.8%) | 12.5 (12.0) | 9.9 (12.0) | 15.0 (14.0) | ||||
| History of disease | No N = 674 (98.0%) | 11.4 (12.0) | 0.075 | 9.5 (12.0) | 0.601 | 14.5 (14.0) | 0.698 |
| Yes N = 14 (2.0%) | 12.9 (18.0) | 8.1 (9.5) | 15.6 (19.5) | ||||
| Any history of psychiatric illness in the past | No N = 680 (98.8%) | 11.4 (14.0) | 0.551 | 9.4 (12.0) | 0.133 | 14.5 (14.0) | 0.220 |
| Yes N = 8 (1.2%) | 13.0 (11.0) | 14.5 (20.5) | 18.3 (11.5) | ||||
| Work experience | ≤5 years 216 (31.4%) | 8.1 (12.0) | <0.001 *** | 7.2 (10.0) | <0.001 *** | 11.5 (14.0) | <0.001 *** |
| 6–10 years N = 155 (22.5%) | 12.4 (14.0) | 10.0 (12.0) | 15.2 (14.0) | ||||
| 10–15 years N = 165 (24.0%) | 13.9 (14.0) | 11.2 (12.0) | 17.0 (14.0) | ||||
| ≥15 years N = 152 (22.1%) | 12.4 (14.0) | 10.3 (14.0) | 15.4 (12.0) | ||||
| Living with family members under the age of 18 | No N = 384 (55.8%) | 10.2 (14.0) | <0.001 *** | 8.3 (10.0) | <0.001 *** | 13.2 (16.0) | <0.001 *** |
| Yes N = 304 (44.2%) | 12.9 (14.0) | 10.9 (12.0) | 16.1 (16.0) | ||||
| Living with family members over the age of 65 | No N = 502 (73.0%) | 11.0 (14.0) | 0.080 | 9.2 (12.0) | 0.112 | 14.0 (14.0) | 0.016 * |
| Yes N = 186 (27.0%) | 12.4 (14.0) | 10.3 (12.0) | 15.8 (14.0) | ||||
| Variable | Depression | Anxiety | Stress | ||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | p-Value | Mean ± SD | p-Value | Mean ± SD | p-Value | ||
| Average working hours per week | ≤72 h N = 95 (13.8%) | 8.7(12.0) | 0.013 * | 7.7(6.0) | 0.014 * | 11.8(16.0) | 0.005 ** |
| 72~96 h N = 400 (58.1%) | 11.6(12.0) | 9.2(12.0) | 14.5(12.0) | ||||
| >96 h N = 193 (28.1%) | 12.4 (14.0) | 10.9(12.0) | 15.8(16.0) | ||||
| The work unit is dedicated to transporting confirmed or suspected infected patients | No N = 509 (74.0%) | 11.5 (14.0) | 0.720 | 9.6(12.0) | 0.866 | 14.4(15.0) | 0.467 |
| Yes N = 179 (26.0%) | 11.1 (12.0) | 9.1(12.0) | 14.9(12.0) | ||||
| Transport or interact with this many suspected or COVID-19-positive patients | ≤20 N = 454 (66.0%) | 10.4 (14.0) | <0.001 *** | 8.8(12.0) | 0.003 ** | 13.2(14.0) | <0.001 *** |
| 21~40 N = 158 (23.0%) | 12.8 (14.0) | 10.7(12.0) | 16.4(12.0) | ||||
| >40 N = 76 (11.0%) | 14.5 (13.5) | 11.0(8.0) | 18.2(12.0) | ||||
| Did you contract the severe acute respiratory syndrome (SARS) in 2002? | No N = 571 (83.0%) | 11.2 (14.0) | 0.260 | 9.3(12.0) | 0.496 | 14.5(14.0) | 0.976 |
| Yes N = 117 (17.0%) | 12.4 (14.0) | 10.1(14.0) | 14.8(16.0) | ||||
| Do you worry about spreading the disease to your family due to work during the COVID-19 pandemic? | No N = 85 (12.4%) | 7.7 (14.0) | <0.001 *** | 5.9 (10.0) | <0.001 *** | 8.9 (9.0) | <0.001 *** |
| Yes N = 603 (87.6%) | 11.9 (14.0) | 10.0 (10.0) | 15.3 (14.0) | ||||
| Do you want to find alternate accommodation and temporarily live apart from your family because of your work during the COVID-19 pandemic? | No N = 388 (56.4%) | 10.2 (14.0) | <0.001 *** | 8.2 (8.0) | <0.001 *** | 12.8 (14.0) | <0.001 *** |
| Yes N = 300 (43.6%) | 13.0 (14.0) | 11.1 (12.0) | 16.7 (16.0) | ||||
| Have you experienced violence because of work? | No N = 560 (81.4%) | 10.2 (14.0) | <0.001 *** | 8.4 (12.0) | <0.001 *** | 13.3 (14.0) | <0.001 *** |
| Yes N = 128 (18.6%) | 16.6 (17.5) | 13.9 (14.0) | 19.8 (16.0) | ||||
| Have you suffered from stigmatization because of your work? | No N = 533 (77.5%) | 9.9 (14.0) | <0.001 *** | 8.2 (12.0) | <0.001 *** | 12.8 (14.0) | <0.001 *** |
| Yes N=155 (22.5%) | 16.7 (16.0) | 13.7 (12.0) | 20.4 (14.0) | ||||
| Are you worried about the frequent reports of COVID-19 in the media? | No N = 342 (49.7%) | 10.7 (14.0) | 0.092 | 8.8 (12.0) | 0.024 * | 13.5 (16.0) | 0.014 * |
| Yes N = 346 (50.3%) | 12.1 (12.0) | 10.1 (10.5) | 15.5 (14.0) | ||||
| Are you concerned about the increased number of COVID-19-positive patients or deaths? | No N = 246 (35.8%) | 9.4 (14.0) | <0.001 *** | 7.2 (10.0) | <0.001 *** | 11.1 (12.5) | <0.001 *** |
| Yes N = 442 (64.2%) | 12.5 (14.0) | 10.7 (12.0) | 16.4 (16.0) | ||||
| Do you worry about the lack of personal protective equipment, which increases the risk of exposure when attending work? | No N = 270 (39.2%) | 9.0 (14.0) | <0.001 *** | 7.1 (10.0) | <0.001 *** | 11.5 (12.5) | <0.001 *** |
| Yes N = 418 (60.8%) | 13.0 (14.0) | 11.0 (12.0) | 16.4 (14.0) | ||||
| Are you worried about the lack of a COVID-19 vaccine? | No N = 381 (55.4%) | 10.7 (14.0) | 0.057 | 8.8 (12.0) | 0.018 * | 13.5 (14.0) | 0.002 ** |
| Yes N = 307 (44.6%) | 12.3 (14.0) | 10.3 (12.0) | 15.8 (14.0) | ||||
| Are you worried about the lack of drugs to treat COVID-19? | No N = 288 (41.9%) | 9.9 (14.0) | 0.001 ** | 8.1 (10.0) | <0.001 *** | 12.6 (13.5) | <0.001 *** |
| Yes N = 400 (58.1%) | 12.5 (14.0) | 10.4 (12.0) | 15.9 (14.0) | ||||
| Do you believe the understanding and support of your family members or peers have diminished due to the pandemic? | No N = 607 (88.2%) | 10.4 (14.0) | <0.001 *** | 8.5 (12.0) | <0.001 *** | 13.5 (14.0) | <0.001 *** |
| Yes N = 81 (11.8%) | 18.7 (16.0) | 16.4 (17.0) | 22.4 (16.0) | ||||
| Drinking problem | No N = 511 (79.5%) | 10.9 (14.0) | 0.015 * | 8.8 (12.0) | <0.001 *** | 13.9 (14.0) | 0.004 ** |
| Yes N = 177 (25.7%) | 12.9 (14.0) | 11.3 (12.0) | 16.3 (15.0) | ||||
| Sleep quality | Good N = 547 (79.5%) | 9.4 (12.0) | <0.001 *** | 7.9 (10.0) | <0.001 *** | 12.5 (14.0) | <0.001 *** |
| Bad N = 141 (20.5%) | 19.3 (14.0) | 15.7 (14.0) | 22.2 (16.0) | ||||
| Variable | Univariable | Multivariable | |||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Region | North, East, and Islands | Reference | Reference | ||
| Central | 1.05 (0.75–1.47) | 0.787 | 1.36 (0.90–2.05) | 0.142 | |
| Southern | 1.96 (1.21–3.17) | 0.006 ** | 2.63 (1.47–4.72) | 0.001 ** | |
| Age | 20–30 years | Reference | Reference | ||
| 31–40 years | 2.33 (1.61–3.39) | <0.001 *** | 1.56 (0.88–2.77) | 0.128 | |
| >40 years | 2.73 (1.76–4.24) | <0.001 *** | 1.96 (0.90–4.27) | 0.092 | |
| Gender | Woman | Reference | Reference | ||
| Man | 0.61 (0.31–1.20) | 0.153 | 0.64 (0.29–1.42) | 0.273 | |
| Marital status | Single | Reference | Reference | ||
| Divorce | 1.16 (0.46–2.93) | 0.751 | 0.35 (0.11–1.09) | 0.070 | |
| Married | 1.43 (1.04–1.95) | 0.027 * | 0.67 (0.39–1.15) | 0.148 | |
| Level of education | High school | Reference | Reference | ||
| College | 1.16 (0.45–2.97) | 0.76 | 0.88 (0.30–2.55) | 0.806 | |
| University | 1.68 (0.66–4.29) | 0.281 | 1.10 (0.38–3.21) | 0.866 | |
| Masters and Doctorate | 1.53 (0.58–4.04) | 0.388 | 0.70 (0.23–2.16) | 0.535 | |
| History of disease | No | Reference | Reference | ||
| Yes | 1.43 (0.50–4.13) | 0.505 | 1.46 (0.42–5.10) | 0.555 | |
| Any history of psychiatric illness in the past? | No | Reference | Reference | ||
| Yes | 1.43 (0.35–5.76) | 0.616 | 1.16 (0.24–5.67) | 0.860 | |
| Work experience | ≤5 years | Reference | Reference | ||
| 6–10 years | 2.14 (1.38–3.30) | 0.001 ** | 2.16 (1.26–3.71) | 0.005 ** | |
| 10–15 years | 2.97 (1.94–4.55) | <0.001 *** | 3.01 (1.53–5.93) | 0.001 ** | |
| ≥15 years | 2.21 (1.43–3.43) | <0.001 *** | 1.76 (0.81–3.84) | 0.154 | |
| Living with family members under the age of 18 | No | Reference | Reference | ||
| Yes | 1.57 (1.16–2.13) | 0.004 ** | 0.97 (0.61–1.54) | 0.891 | |
| Living with family members over the age of 65 | No | Reference | Reference | ||
| Yes | 1.45 (1.03–2.03) | 0.034 * | 1.29 (0.87–1.93) | 0.211 | |
| Average working hours per week | ≤72 h | Reference | Reference | ||
| 72~96 h | 1.70 (1.05–2.75) | 0.030 * | 1.76 (1.00–3.07) | 0.049 * | |
| >96 h | 1.75 (1.04–2.95) | 0.035 * | 1.66 (0.90–3.06) | 0.103 | |
| Transport or interact with this many suspected or COVID-19-positive patients | ≤20 | Reference | Reference | ||
| 21~40 | 1.45 (1.00–2.09) | 0.047 * | 1.39 (0.91–2.13) | 0.133 | |
| >40 | 2.08 (1.28–3.40) | 0.003 ** | 1.57 (0.88–2.81) | 0.129 | |
| Do you worry about spreading the disease to your family due to work during the COVID-19 pandemic? | No | Reference | Reference | ||
| Yes | 1.70 (1.04–2.77) | 0.034 * | 1.35 (0.74–2.46) | 0.325 | |
| Have you experienced violence because of work? | No | Reference | Reference | ||
| Yes | 2.28 (1.55–3.37) | <0.001 *** | 1.42 (0.87–2.33) | 0.165 | |
| Have you suffered from stigmatization because of your work? | No | Reference | Reference | ||
| Yes | 2.34 (1.62–3.36) | <0.001 *** | 1.09 (0.67–1.76) | 0.729 | |
| Do you worry about the lack of personal protective equipment, which increases the risk of exposure when attending work? | No | Reference | Reference | ||
| Yes | 1.73 (1.26–2.38) | 0.001 ** | 1.06 (0.70–1.57) | 0.792 | |
| Are you worried about the lack of drugs to treat COVID-19? | No | Reference | Reference | ||
| Yes | 1.38 (1.01–1.88) | 0.043 * | 0.96 (0.65–1.42) | 0.832 | |
| Do you believe the understanding and support of your family members or peers have diminished due to the pandemic? | No | Reference | Reference | ||
| Yes | 4.25 (2.55–7.08) | <0.001 *** | 2.72 (1.50–4.92) | 0.001 *** | |
| Drinking problem | No | Reference | Reference | ||
| Yes | 1.45 (1.03–2.04) | 0.035 * | 1.13 (0.76–1.69) | 0.546 | |
| Sleep quality | Good | Reference | Reference | ||
| Bad | 5.73 (3.78–8.68) | <0.001 *** | 5.04 (3.18–7.99) | <0.001 *** | |
| Variable | Univariable | Multivariable | |||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Region | North, East, and Islands | Reference | Reference | ||
| Central | 0.97 (0.69–1.36) | 0.861 | 1.24 (0.84–1.84) | 0.288 | |
| Southern | 1.88 (1.16–3.06) | 0.011 * | 2.77 (1.54–4.99) | 0.001 ** | |
| Age | 20–30 years | Reference | Reference | ||
| 31–40 years | 2.11 (1.48–3.03) | <0.001 *** | 1.77 (1.01–3.10) | 0.046 | |
| >40 years | 2.37 (1.54–3.65) | <0.001 *** | 2.00 (0.93–4.28) | 0.075 | |
| Gender | Woman | Reference | Reference | ||
| Man | 0.34 (0.17–0.71) | 0.004 ** | 0.28 (0.12–0.65) | 0.003 *** | |
| Marital status | Single | Reference | Reference | ||
| Divorce | 1.87 (0.75–4.64) | 0.180 | 1.09 (0.36–3.28) | 0.884 | |
| Married | 1.46 (1.07–2.00) | 0.016 * | 0.79 (0.47–1.36) | 0.398 | |
| Level of education | High school | Reference | Reference | ||
| College | 1.67 (0.66–4.28) | 0.282 | 1.46 (0.50–4.29) | 0.492 | |
| University | 1.81 (0.71–4.63) | 0.216 | 1.13 (0.38–3.33) | 0.832 | |
| Masters and Doctorate | 1.44 (0.55–3.80) | 0.458 | 0.62 (0.20–1.93) | 0.408 | |
| History of disease | No | Reference | Reference | ||
| Yes | 0.91 (0.31–2.64) | 0.859 | 0.73 (0.21–2.55) | 0.622 | |
| Any history of psychiatric illness in the past? | No | Reference | Reference | ||
| Yes | 2.04 (0.48–8.59) | 0.333 | 2.24 (0.45–11.06=9) | 0.323 | |
| Work experience | ≤5 years | Reference | Reference | ||
| 6–10 years | 1.91 (1.25–2.91) | 0.003 ** | 1.50 (0.89–2.53) | 0.131 | |
| 10–15 years | 2.63 (1.73–3.99) | <0.001 *** | 1.85 (0.96–3.58) | 0.069 | |
| ≥15 years | 2.03 (1.33–3.11) | 0.001 ** | 1.28 (0.60–2.72) | 0.534 | |
| Living with family members under the age of 18 | No | Reference | |||
| Yes | 1.67 (1.24–2.27) | 0.001 ** | 1.05 (0.66–1.66) | 0.835 | |
| Average working hours per week | ≤72 h | Reference | Reference | ||
| 72~96 h | 1.51 (0.95–2.41) | 0.08 | 1.66 (0.97–2.84) | 0.066 | |
| >96 h | 1.70 (1.03–2.82) | 0.039 * | 1.85 (1.03–3.33) | 0.041 * | |
| Transport or interact with this many suspected or COVID-19-positive patients | ≤20 | Reference | Reference | ||
| 21~40 | 1.42 (0.98–2.04) | 0.061 | 1.35 (0.89–2.05) | 0.154 | |
| >40 | 1.95 (1.19–3.18) | 0.008 *** | 1.45 (0.81–2.60) | 0.206 | |
| Do you worry about spreading the disease to your family due to work during the COVID-19 pandemic? | No | Reference | Reference | ||
| Yes | 2.47 (1.49–4.08) | <0.001 *** | 1.68 (0.90–3.14) | 0.103 | |
| Do you want to find alternate accommodation and temporarily live apart from your family because of your work during the COVID-19 pandemic? | No | Reference | Reference | ||
| Yes | 1.63 (1.20–2.21) | 0.002 ** | 1.06 (0.74–1.52) | 0.763 | |
| Have you experienced violence because of work? | No | Reference | Reference | ||
| Yes | 2.69 (1.80–4.01) | <0.001 *** | 1.57 (0.96–2.55) | 0.071 | |
| Have you suffered from stigmatization because of your work? | No | Reference | Reference | ||
| Yes | 2.88 (1.98–4.18) | <0.001 *** | 1.37 (0.85–2.20) | 0.193 | |
| Are you concerned about the increased number of COVID-19-positive patients or deaths? | No | Reference | Reference | ||
| Yes | 1.88 (1.36–2.59) | <0.001 *** | 1.12 (0.74–1.70) | 0.584 | |
| Do you worry about the lack of personal protective equipment, which increases the risk of exposure when attending work? | No | Reference | Reference | ||
| Yes | 2.19 (1.59–3.00) | <0.001 *** | 1.33 (0.89–1.99) | 0.163 | |
| Are you worried about the lack of a COVID-19 vaccine? | No | Reference | Reference | ||
| Yes | 1.44 (1.06–1.94) | 0.019 * | 0.96 (0.67–1.39) | 0.828 | |
| Are you worried about the lack of drugs to treat COVID-19? | No | Reference | Reference | ||
| Yes | 1.81 (1.33–2.46) | <0.001 *** | 1.24 (0.82–1.87) | 0.303 | |
| Do you believe the understanding and support of your family members or peers have diminished due to the pandemic? | No | Reference | Reference | ||
| Yes | 3.78 (2.26–6.33) | <0.001 *** | 2.03 (1.11–3.68) | 0.021 * | |
| Drinking problem | No | Reference | Reference | ||
| Yes | 1.68 (1.19–2.37) | <0.003 *** | 1.39 (0.94–2.06) | 0.096 | |
| Sleep quality | Good | Reference | Reference | ||
| Bad | 3.29 (2.22–4.88) | <0.001 *** | 2.44 (1.57–3.81)- | <0.001 *** | |
| Variable | Univariable | Multivariable | |||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Region | North, East and Islands | Reference | Reference | ||
| Central | 0.80 (0.55–1.16) | 0.243 | 1.00 (0.64–1.56) | 0.999 | |
| Southern | 1.71 (1.05–2.79) | 0.031 * | 2.78 (1.50–5.14) | 0.001 ** | |
| Age | 20–30 years | Reference | Reference | ||
| 31–40 years | 1.73 (1.17–2.55) | 0.006 ** | 1.25 (0.67–2.34) | 0.486 | |
| >40 years | 1.66 (1.04–2.64) | 0.033 ** | 1.13 (0.48–2.64) | 0.785 | |
| Gender | Woman | Reference | Reference | ||
| Man | 0.69 (0.34–1.37) | 0.284 | 0.69 (0.30–1.59) | 0.387 | |
| Marital status | Single | Reference | Reference | ||
| Divorce | 0.88 (0.31–2.51) | 0.814 | 0.49 (0.13–1.78) | 0.278 | |
| Married | 1.34 (0.96–1.88) | 0.084 | 0.94 (0.52–1.70) | 0.837 | |
| Level of education | High school | Reference | Reference | ||
| College | 1.32 (0.47–3.74) | 0.597 | 0.93 (0.28–3.11) | 0.911 | |
| University | 1.57 (0.56–4.44) | 0.392 | 0.88 (0.26–2.97) | 0.840 | |
| Masters and Doctorate | 1.43 (0.49–4.16) | 0.512 | 0.61 (0.17–2.15) | 0.438 | |
| History of disease | No | Reference | Reference | ||
| Yes | 1.25 (0.42–3.79) | 0.689 | 1.47 (0.38–5.67) | 0.581 | |
| Any history of psychiatric illness in the past? | No | Reference | Reference | ||
| Yes | 2.27 (0.56–9.16) | 0.250 | 2.16 (0.43–10.76) | 0.347 | |
| Work experience | ≤5 years | Reference | Reference | ||
| 6–10 years | 1.68 (1.06–2.65) | 0.028 * | 1.29 (0.72–2.31) | 0.395 | |
| 10–15 years | 1.95 (1.25–3.05) | 0.003 ** | 1.58 (0.77–3.27) | 0.214 | |
| ≥15 years | 1.58 (0.99–2.51) | 0.054 | 1.11 (0.48–2.58) | 0.813 | |
| Living with family members under the age of 18 | No | Reference | Reference | ||
| Yes | 1.53 (1.10–2.11) | 0.011 * | 0.95 (0.57–1.58) | 0.841 | |
| Average working hours per week | ≤72 h | Reference | Reference | ||
| 72~96 h | 1.67 (0.97–2.85) | 0.063 | 1.61 (0.85–3.05) | 0.141 | |
| >96 h | 2.09 (1.18–3.71) | 0.012 * | 1.92 (0.97–3.81) | 0.061 | |
| Transport or interact with this many suspected or COVID-19-positive patients | ≤20 | Reference | Reference | ||
| 21~40 | 1.82 (1.24–2.66) | 0.002 ** | 1.60 (1.02–2.51) | 0.040 * | |
| >40 | 1.94 (1.17–3.21) | 0.01 * | 1.20 (0.97–3.81) | 0.571 | |
| Do you worry about spreading the disease to your family due to work during the COVID-19 pandemic? | No | Reference | Reference | ||
| Yes | 3.02 (1.60–5.69) | 0.001 ** | 1.89 (0.87–4.11) | 0.110 | |
| Do you want to find alternate accommodation and temporarily live apart from your family because of your work during the COVID-19 pandemic? | No | Reference | Reference | ||
| Yes | 2.21 (1.59–3.07) | <0.001 *** | 1.38 (0.93–2.06) | 0.111 | |
| Have you experienced violence because of work? | No | Reference | Reference | ||
| Yes | 2.78 (1.88–4.13) | <0.001 *** | 1.49 (0.89–2.47) | 0.127 | |
| Have you suffered from stigmatization because of your work? | No | Reference | Reference | ||
| Yes | 3.24 (2.24–4.70) | <0.001 *** | 1.40 (0.85–2.29) | 0.186 | |
| Are you concerned about the increased number of COVID-19-positive patients or deaths? | No | Reference | Reference | ||
| Yes | 2.35 (1.63–3.39) | <0.001 *** | 1.56 (0.97–2.52) | 0.065 | |
| Do you worry about the lack of personal protective equipment, which increases the risk of exposure when attending work? | No | Reference | Reference | ||
| Yes | 2.07 (1.45–2.93) | <0.001 *** | 1.06 (0.68–1.67) | 0.795 | |
| Are you worried about the lack of a COVID-19 vaccine? | No | Reference | Reference | ||
| Yes | 1.45 (1.04–2.00) | 0.026 * | 1.02 (0.68–1.53) | 0.930 | |
| Are you worried about the lack of drugs to treat COVID-19? | No | ||||
| Yes | 1.77 (1.26–2.48) | 0.001 ** | 0.98 (0.62–1.56) | 0.947 | |
| Do you believe the understanding and support of your family members or peers have diminished due to the pandemic? | No | Reference | Reference | ||
| Yes | 6.06 (3.68–10.00) | <0.001 *** | 3.27 (1.83–5.86) | <0.001 *** | |
| Drinking problem | No | Reference | Reference | ||
| Yes | 1.44 (1.00–2.06) | 0.049 * | 1.04 (0.68–1.60) | 0.843 | |
| Sleep quality | Good | Reference | Reference | ||
| Bad | 5.02 (3.39–7.42) | <0.001 *** | 4.34 (2.76–6.82) | <0.001 *** | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, C.-Y.; Sun, J.-T.; Chang, H.-P.; Chen, Y.-L.; Pei, D.; Liang, Y.-J. Investigation of Psychological Stress and Sleep Quality of Emergency Medical Technicians in Taiwan Fire Department during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 137. https://doi.org/10.3390/ijerph20010137
Cheng C-Y, Sun J-T, Chang H-P, Chen Y-L, Pei D, Liang Y-J. Investigation of Psychological Stress and Sleep Quality of Emergency Medical Technicians in Taiwan Fire Department during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2023; 20(1):137. https://doi.org/10.3390/ijerph20010137
Chicago/Turabian StyleCheng, Chiao-Yin, Jen-Tang Sun, Hung-Pin Chang, Yen-Lin Chen, Dee Pei, and Yao-Jen Liang. 2023. "Investigation of Psychological Stress and Sleep Quality of Emergency Medical Technicians in Taiwan Fire Department during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 20, no. 1: 137. https://doi.org/10.3390/ijerph20010137
APA StyleCheng, C.-Y., Sun, J.-T., Chang, H.-P., Chen, Y.-L., Pei, D., & Liang, Y.-J. (2023). Investigation of Psychological Stress and Sleep Quality of Emergency Medical Technicians in Taiwan Fire Department during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 20(1), 137. https://doi.org/10.3390/ijerph20010137









