Abstract
Introduction: The autonomic nervous system plays a vital role in the modulation of many vital bodily functions, one of which is sleep and wakefulness. Many studies have investigated the link between autonomic dysfunction and sleep cycles; however, few studies have investigated the links between short-term sleep health, as determined by the Pittsburgh Quality of Sleep Index (PSQI), such as subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction, and autonomic functioning in healthy individuals. Aim: In this cross-sectional study, the aim was to investigate the links between short-term sleep quality and duration, and heart rate variability in 60 healthy individuals, in order to provide useful information about the effects of stress and sleep on heart rate variability (HRV) indices, which in turn could be integrated into biological models for wearable devices. Methods: Sleep parameters were collected from participants on commencement of the study, and HRV was derived using an electrocardiogram (ECG) during a resting and stress task (Trier Stress Test). Result: Low-frequency to high-frequency (LF:HF) ratio was significantly higher during the stress task than during the baseline resting phase, and very-low-frequency and high-frequency HRV were inversely related to impaired sleep during stress tasks. Conclusion: Given the ubiquitous nature of wearable technologies for monitoring health states, in particular HRV, it is important to consider the impacts of sleep states when using these technologies to interpret data. Very-low-frequency HRV during the stress task was found to be inversely related to three negative sleep indices: sleep quality, daytime dysfunction, and global sleep score.
1. Introduction
Autonomic control of inter-beat heart rate is modulated by the two branches of the autonomic nervous system: the sympathetic and parasympathetic arms. As such, analysis of fluctuations in heart rate over time, obtained via a non-invasive electrocardiogram, provides useful information regarding autonomic functioning. This measurement is known as heart rate variability (HRV). The clinical utility of heart rate variability was first realised in the late 1980s, when reduced HRV was found to be a robust clinical predictor of mortality post myocardial infarction [1]. Since then, many disease states have been investigated using heart rate variability. In particular, diseases that are associated with impaired or dysregulated autonomic control, such as renal failure, diabetes, and heart failure, have been linked with reduced or impaired HRV.
The autonomic nervous system plays a vital role in the modulation of many vital bodily functions, one of which is sleep and wakefulness. Many studies have investigated the link between autonomic dysfunction and sleep cycles; however, few studies have investigated the links between short-term sleep health, as determined by sleep length, quality, etc., and autonomic functioning in healthy individuals. Oftentimes, research has focused on cohorts suffering from insomnia and/or autonomic impairment [2,3,4], or used endpoints known to be predictors of impaired autonomic control, such as hypertension [5,6,7,8] or obstructive sleep apnoea [9,10,11,12,13], rather than direct assessment of short-term sleep quality and HRV. The literature has suggested that impaired autonomic functioning is associated with chronic insomnia, which may reflect physiological hyperarousal. This is supported by the current theoretic models for sleep initiation and maintenance disorders [14]. Research, however, is unclear as to whether isolated sleep disturbances influence autonomic function. Of the studies that have been conducted [15,16,17,18,19,20], there remains no clear consensus regarding the link between sleep quality and HRV parameters, in particular during resting and stress states.
The human body responds to acute stress via a cascade of hormonal [21,22], immune-mediated [23,24,25], and autonomic [26,27,28] processes that culminate in an acutely advantageous biological response. This transient response is generally short-lived and provides a momentary reservoir of biological resources that can be utilised in order to mitigate the internal or external stressor [28]. Over time, repeated exposure to stressful events can induce chronic activation of the stress response, via the hypothalamic–pituitary–adrenal (HPA) axis [29]. This chronic hypothalamic–pituitary–adrenal-axis (HPA-axis) activation has been implicated in numerous disease processes, such as depression [30], heart disease [31], hypertension [32], and cancer [33,34,35,36]. Although research has generally focused on the links between impaired sleep and cardiac health in patients with various diseases, little research has been conducted into the acute impacts of impaired sleep quality on cardiac parameters within a healthy population. This is particularly pertinent research when we consider the current widespread availability of technologies that can record both cardiac and sleep data. Numerous wearable technologies exist with the capabilities of recording HRV data; however, the real-time clinical significance of this information is yet to be fully elucidated. Further, the impact of stress on HRV, and the effect of sleep quality on HRV indices, remain important considerations when utilising HRV as a real-time predictor of stress and health.
In the current study, the aim was to investigate the links between sleep quality and duration, and HRV in 60 healthy participants, in order to provide useful information about the effects of stress and sleep on HRV indices. The a priori hypotheses were that (1) global sleep score would be inversely related to high-frequency HRV during both resting and stress tasks; (2) daytime dysfunction would be inversely related to resting very-low-frequency heart rate variability; (3) reported sleep quality during the stress task would be inversely related to very-low-frequency (VLF) HRV.
2. Materials and Methods
2.1. Participants and Sampling
A cross-sectional study design was used to examine the relationship between HRV and sleep quality in 60 healthy participants aged between 18–45 years. Participants were recruited from the general community via online advertisements. Prior to inclusion, an in-house-designed lifestyle questionnaire adapted from the Lifestyle Appraisal Questionnaire (LAQ) [37] was utilised to screen participants for medication use, alcohol intake (over 1.6 standard drinks a day), smoking habits (over 10 cigarettes a day), and chronic disease/illness. Participants were excluded if they answered affirmatively to any of the screening questions mentioned above. Participants were asked to refrain from consuming coffee and alcohol for 24 h prior, and from smoking cigarettes for 12 h prior to the study. Further, participants were required to have had a minimum of 8 h sleep in the evening preceding the study.
Two participants were excluded from the study, one due to taking a calcium channel blocker, and one due to the inability to stay for the duration of the study, with two further participants recruited to fill the gaps; there were no further participants excluded. The total number of participants was 62, with analysis conducted on 60 participants (Figure 1). The study had institutional ethics approval from the University of Technology Sydney Human Research Ethics Committee, and all participants provided signed informed consent prior to the commencement of the study.
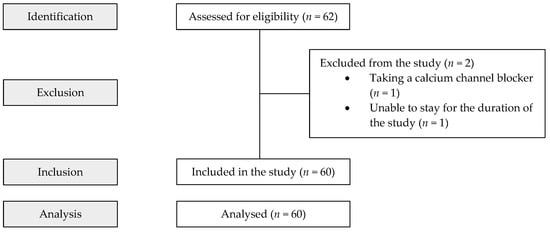
Figure 1.
STROBE participant flow diagram.
2.2. Experimental Procedures
At the commencement and conclusion of each session, blood pressure (BP) measurements were taken three times with an automated blood pressure monitor (Omron IA1B, Kyoto, Japan), and averaged to confirm inclusion into the study (BP < 160/100 mmHg). Following BP collection, in-house-designed questionnaires were used to collect demographic, lifestyle, and work-related data. Additionally, the general health questionnaire (GHQ) was also utilised to assess general psychological wellbeing whilst the Pittsburgh Quality of Sleep Index was employed to assess self-reported sleep quality. Nineteen individual items are compiled to produce seven “component” scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. The addition of these scores for each of the seven components yields a global PSQI score. The PSQI has been shown to yield strong internal homogeneity, consistency (test–retest reliability), and validity [38].
The Trier Social Stress Test (TSST) [39] was then utilised to elicit a controlled stress response in participants. For this section of the study, participants underwent a 15 min resting baseline session, followed by the TSST, which consisted of a 5 min preparation/anticipation task where participants were required to prepare a short speech, followed by a 5 min public speaking task, and finally a 5 min mental arithmetic task. The TSST is one of the most well-accepted laboratory techniques to induce acute stress in experimental settings and has been repeatedly shown to reliably provoke hypothalamic–pituitary–adrenal-axis activation [39,40,41,42,43,44,45]. In fact, of the numerous stress-inducing laboratory protocols, meta-analysis has suggested that TSST is the most useful and appropriately standardised protocol for studies of stress assessment and stress hormone reactivity [40].
During baseline and each component of the TSST, 3-lead ECG data were captured using disposable Ag/AgCl electrodes placed on the participant’s upper torso under each clavicle on the coracoid processes, and one just below the sternum over the xiphoid process [46]. Following completion of the TSST, three further BP readings were obtained, which were then averaged.
2.3. ECG Data Processing
Raw ECG data were processed utilising the Kubios HRV Premium software (Version 3.1.0, Kubios Oy, Kuopio, Finland) to generate HRV parameters. Frequency domain HRV deconstructs the variance in beat-to-beat heart rate (HR) into its underlying components at different frequencies using fast-Fourier transforms (FFTs). It should be highlighted that the calculation of frequency domain HRV requires a certain level of “stationarity”, i.e., the mean and variance of the ECG signal do not vary significantly at different points during the electrocardiogram. In order to meet this requirement, data were collected over 5 min intervals and averaged to produce reliable HRV frequency domain data. Further, all data were assessed to ensure sinus rhythm prior to transformation. Frequency domain activity was calculated using Welch’s periodogram method [47] for the following HRV frequency bands: low-frequency (LF) power (0.04–0.15 Hz), high-frequency (HF) power (0.15–0.4 Hz), and total power (TP), as well as the LF:HF ratio. It should be noted that in the process of deriving these variables, the automatic artefact correction process of the Kubios software [48], as well as the smoothness priors method [49] of trend component rejection, were utilised, and HRV data were log-transformed prior to analysis where relevant.
2.4. Statistical Analysis
Statistical analysis was performed using SPSS Version 23.0 (SPSS Inc.; Chicago, IL, USA) with statistical significance defined as p < 0.05. Data were initially subject to descriptive statistics. Dependent sample t-tests were utilised in order to determine significant differences in HRV parameters between the resting phase and stress task. As multiple comparisons were made, a Holm–Bonferroni correction was then applied to avoid type I errors with the family-wise α (a) level set at 0.05. Following that, partial Pearson’s correlation analysis (controlling for age and body mass index (BMI)) was utilised to determine associations between HRV parameters and sleep factors (as determined by the PSQI) during the baseline and stress task (TSST). Where three or more significant relationships to a dependent variable were found (after Bonferroni correction), a multiple linear regression analysis was utilised to further examine the relationship between HRV and dependent variables.
3. Results
3.1. Participant Descriptions
This study consisted of 60 participants (male n = 33; female n = 27), with demographic information provided in Table 1. The average age of participants was 28.9 ± 8.8 (years ± SD), with an average body mass index of 23.1 ± 3.4 kg/m2. Average pre-study (baseline systolic blood pressure (SBP) was 116.0 ± 14.4, and pre-study diastolic blood pressure (DBP) was 76.1 ± 9.2. Average post study SBP was 119.5 ± 13.6 and post-study DBP was 80.7 ± 8.81.

Table 1.
Demographics of study participants (n = 60).
3.2. Comparison in Cardiac Parameters between Baseline and Stress Task
Significant differences were identified between certain cardiac parameters during the baseline (resting) phase and the stress task (Table 2). SBP (p = 0.001), DBP (p ≤ 0.001), LF (p = 0.006), HF (p ≤ 0.001), and ratio (p = 0.012) were significantly higher during the stress task.

Table 2.
Comparison of cardiac parameters between baseline (resting) and stress task (n = 60).
3.3. Correlations between Sleep Quality and HRV
Partial correlations (controlling for age and BMI) were undertaken between HRV parameters during the baseline (resting) phase and stress task and self-reported sleep qualities (as measured by the PSQI) (Table 3). No significant correlations were identified during the baseline (resting) phase and the various subscales of the PSQI. During the stress task, VLF HRV was inversely correlated to daytime dysfunction (p = 0.001), subjective sleep quality (p = 0.007), and global sleep score (p = 0.018). HF n.u. during the stress task was inversely correlated to sleep latency (p = 0.013) and global sleep score (p = 0.014). Total power during the stress task was inversely correlated to daytime dysfunction (p = 0.003), subjective sleep quality (p = 0.014), and global sleep score (p = 0.019). Finally, LF:HF ratio during the stress task was positively correlated to sleep latency (p = 0.045).

Table 3.
Partial correlations (controlling for age and BMI) between sleep quality (as measured by the PSQI) and heart rate variability (n = 60).
3.4. Multiple Regressions
A multiple regression was performed when three or more independent variables were correlated to one dependent variable (after a Bonferroni correction). Daytime dysfunction, subjective sleep quality, and global sleep score significantly predicted VLF during the stress task (F(3, 55) = 2.84, p = 0.046, R = 0.37, R2 = 0.143; adjusted R2 = 0.09). Together, the independent variables explain 36.6% of the variability in VLF during the stress task (Table 4). None of the individual variables added significantly to the prediction.

Table 4.
Multiple regression analysis VLF during the stress task.
After Bonferroni correction, daytime dysfunction, subjective sleep quality, and global sleep scores were entered into a multiple linear regression to predict TP during the stress task; however, the model was not significant (F(3, 55) = 2.5, p = 0.073, R = 0.34, R2 = 0.12; adjusted R2 = 0.07).
4. Discussion
The present study examined relationships between sleep quality indices as determined by the PSQI (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction) and heart rate variability parameters during resting and stress states. Very-low-frequency HRV during the stress task was found to be inversely related to three negative sleep indices: sleep quality, daytime dysfunction, and global sleep score. That is, the poorer an individual’s sleep quality, and the greater the effect on their daytime function, the lower the VLF HRV during the stress task. Many studies have suggested that the renin–angiotensin system contributes significantly to VLF [50,51,52]. Further, studies have shown that impaired sleep (i.e., obstructive sleep apnoea) is linked with nocturnal renin–angiotensin-system (RAS) activation [53,54], and thus may be reflected in increased nocturnal VLF HRV [55]. Nocturnal RAS activation has subsequently been shown to reduce daytime RAS activation, which may account for the findings of this study [56]. Individuals who experience nocturnal RAS activation may then exhibit augmented RAS activation in response to stress, resulting in lower VLF HRV.
This study also identified significant rise in systolic and diastolic blood pressure during the stress task, when compared with the resting state. It is well accepted that the TSST reliably increases cardiovascular activity, such as heart rate and blood pressure.
LF:HF ratio was significantly higher during the stress task than during the baseline resting phase. Research supports an increase in sympathetic nervous system activation during a stress task, and a synchronised parasympathetic withdrawal [57]. The sympathetic shift proves advantageous during the stress response, mobilising biological reserves, increasing blood flow to large muscle groups and vital organs, and promoting efficient respiratory and cardiac function [58].
High-frequency HRV was found to be inversely related to sleep latency and global sleep score during the stress task. This may suggest that individuals who experience impaired night-time sleep exhibit a sympathetic predominance during waking hours. This is supported by the literature, with studies showing that compromised sleep durations and patterns are associated with higher daytime heart rate [59], blood pressure [60], and stress [61].
Due to the cross-sectional nature of the study, only short-term variations in HRV could be assessed. Further research implementing longer-term measurements in HRV could be a value. This study utilised the PSQI to assess sleep disturbance in the previous one month. Future research may benefit from assessment of an individual’s sleep habits over a longer period of time, and, further, by utilising objective sleep measures such as polysomnography. A larger sample size may also increase the robustness of future studies.
A limitation of the study was that ECG data for HRV were collected over 5 min intervals and averaged for calculation of frequency domain HRV to establish stationarity. Given that data are averaged, significant data reflective of short-term stress may have not been accounted for, which, in the context of sleep, is important due to short blips of stress-related HRV changes during sleep, such as with night-terrors.
5. Conclusions
The aim of this study was to investigate the possible impacts of short-term sleep disturbances on HRV parameters during resting and stress states. The present study identified unique relationships between impaired sleep and stress-state HRV. Given the ubiquitous nature of wearable technologies for monitoring health states, it is important to consider the impacts of varied biology conditions when using these technologies to interpret data.
Author Contributions
Conceptualisation, S.L. and T.C.; methodology, S.L. and T.C.; validation, S.L. and T.C.; formal analysis S.L. and T.C.; investigation, T.C. and B.A.H.; resources, S.L., T.C. and B.A.H.; data curation, T.C. and B.A.H.; writing—original draft preparation, T.C.; writing—review and editing, T.C., B.A.H., P.N., D.S., C.-T.L., C.S.M., R.C.-B., J.W.M. and S.L.; visualisation, T.C., B.A.H. and S.L.; supervision, S.L.; project administration, S.L.; funding acquisition, P.N., D.S., C.-T.L., C.S.M., R.C.-B., J.W.M. and S.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the NSW Defence Innovation Network and NSW State Government, grant number DINPP2019 S1-06, StressWatch Project.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the University of Technology Sydney (2014000110, 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available currently due to storage on site at the University of Technology, as stipulated in the Ethics application.
Acknowledgments
We thank the NSW Defence Innovation Network and NSW State Government for financial support of the StressWatch project through grant DINPP2019 S1-06. We also acknowledge the use of FitBit products to obtain heart rate data during this study. The authors also acknowledge the Neuroscience Research Unit, School of Life Sciences, The University of Technology Sydney, where this research was conducted, and the participants for their time and interest.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kleiger, R.E.; Miller, J.P.; Bigger, J.T., Jr.; Moss, A.J. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am. J. Cardiol. 1987, 59, 256–262. [Google Scholar] [CrossRef]
- Schwartz, S.; Anderson, W.M.; Cole, S.R.; Cornoni-Huntley, J.; Hays, J.C.; Blazer, D. Insomnia and heart disease: A review of epidemiologic studies. J. Psychosom. Res. 1999, 47, 313–333. [Google Scholar] [CrossRef]
- Nilsson, P.; Nilsson, J.Å.; Hedblad, B.; Berglund, G. Sleep disturbance in association with elevated pulse rate for prediction of mortality–consequences of mental strain? J. Intern. Med. 2001, 250, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Mallon, L.; Broman, J.E.; Hetta, J. Sleep complaints predict coronary artery disease mortality in males: A 12-year follow-up study of a middle-aged Swedish population. J. Intern. Med. 2002, 251, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Phillips, B.; Bůžková, P.; Enright, P.; Group CHSR. Insomnia did not predict incident hypertension in older adults in the cardiovascular health study. Sleep 2009, 32, 65–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanfranchi, P.A.; Pennestri, M.-H.; Fradette, L.; Dumont, M.; Morin, C.M.; Montplaisir, J. Nighttime blood pressure in normotensive subjects with chronic insomnia: Implications for cardiovascular risk. Sleep 2009, 32, 760–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, C.R.; Knutson, K.L.; Rathouz, P.J.; Sidney, S.; Liu, K.; Lauderdale, D.S. Short sleep duration and incident coronary artery calcification. JAMA 2008, 300, 2859–2866. [Google Scholar]
- Gangwisch, J.E.; Heymsfield, S.B.; Boden-Albala, B.; Buijs, R.M.; Kreier, F.; Pickering, T.G.; Rundle, A.G.; Zammit, G.K.; Malaspina, D. Short sleep duration as a risk factor for hypertension: Analyses of the first National Health and Nutrition Examination Survey. Hypertension 2006, 47, 833–839. [Google Scholar] [CrossRef] [Green Version]
- Wiklund, U.; Olofsson, B.; Franklin, K.; Blom, H.; Bjerle, P.; Niklasson, U. Autonomic cardiovascular regulation in patients with obstructive sleep apnoea: A study based on spectral analysis of heart rate variability. Clin. Physiol. 2000, 20, 234–241. [Google Scholar] [CrossRef]
- Sequeira, V.C.C.; Bandeira, P.M.; Azevedo, J.C.M. Heart rate variability in adults with obstructive sleep apnea: A systematic review. Sleep Sci. 2019, 12, 214. [Google Scholar] [CrossRef]
- Ucak, S.; Dissanayake, H.U.; Sutherland, K.; de Chazal, P.; Cistulli, P.A. Heart rate variability and obstructive sleep apnea: Current perspectives and novel technologies. J. Sleep Res. 2021, 30, e13274. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Kim, S.Y.; Wu, H.W.; Hwang, G.-S.; Kim, H.J. Clinical implication of heart rate variability in obstructive sleep apnea syndrome patients. J. Craniofac. Surg. 2015, 26, 1592–1595. [Google Scholar] [CrossRef] [PubMed]
- Urbanik, D.; Gać, P.; Martynowicz, H.; Poręba, M.; Podgórski, M.; Negrusz-Kawecka, M.; Mazur, G.; Sobieszczańska, M.; Poręba, R. Obstructive sleep apnea as a predictor of reduced heart rate variability. Sleep Med. 2019, 54, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Riemann, D.; Spiegelhalder, K.; Feige, B.; Voderholzer, U.; Berger, M.; Perlis, M.; Nissen, C. The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Med. Rev. 2010, 14, 19–31. [Google Scholar] [CrossRef]
- Bourdillon, N.; Jeanneret, F.; Nilchian, M.; Albertoni, P.; Ha, P.; Millet, G.P. Sleep deprivation deteriorates heart rate variability and photoplethysmography. Front. Neurosci. 2021, 15, 310. [Google Scholar] [CrossRef]
- Stein, P.K.; Pu, Y. Heart rate variability, sleep and sleep disorders. Sleep Med. Rev. 2012, 16, 47–66. [Google Scholar] [CrossRef]
- Tobaldini, E.; Nobili, L.; Strada, S.; Casali, K.R.; Braghiroli, A.; Montano, N. Heart rate variability in normal and pathological sleep. Front. Physiol. 2013, 4, 294. [Google Scholar] [CrossRef] [Green Version]
- Elsenbruch, S.; Harnish, M.J.; Orr, W.C. Heart rate variability during waking and sleep in healthy males and females. Sleep 1999, 22, 1067–1571. [Google Scholar] [CrossRef] [Green Version]
- Bonnet, M.H.; Arand, D. Heart rate variability in insomniacs and matched normal sleepers. Psychosom. Med. 1998, 60, 610–615. [Google Scholar] [CrossRef]
- Ewing, D.; Neilson, J.; Shapiro, C.; Stewart, J.; Reid, W. Twenty four hour heart rate variability: Effects of posture, sleep, and time of day in healthy controls and comparison with bedside tests of autonomic function in diabetic patients. Heart 1991, 65, 239–244. [Google Scholar] [CrossRef] [Green Version]
- Charmandari, E.; Tsigos, C.; Chrousos, G. Endocrinology of the stress response. Annu. Rev. Physiol. 2005, 67, 259–284. [Google Scholar] [CrossRef] [PubMed]
- Holsboer, F.; Ising, M. Stress hormone regulation: Biological role and translation into therapy. Annu. Rev. Psychol. 2010, 61, 81–109. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, A.; Flanigan, M.E.; McEwen, B.S.; Russo, S.J. Aggression, social stress, and the immune system in humans and animal models. Front. Behav. Neurosci. 2018, 12, 56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pruett, S.B. Stress and the immune system. Pathophysiology 2003, 9, 133–153. [Google Scholar] [CrossRef]
- Khansari, D.N.; Murgo, A.J.; Faith, R.E. Effects of stress on the immune system. Immunol. Today 1990, 11, 170–175. [Google Scholar] [CrossRef]
- Christensen, J.S.; Wild, H.; Kenzie, E.S.; Wakeland, W.; Budding, D.; Lillas, C. Diverse autonomic nervous system stress response patterns in childhood sensory modulation. Front. Integr. Neurosci. 2020, 14, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henry, J.P. Biological basis of the stress response. Integr. Physiol. Behav. Sci. 1992, 27, 66–83. [Google Scholar] [CrossRef]
- Tonhajzerova, I.; Mestanik, M. New perspectives in the model of stress response. Physiol. Res. 2017, 66, S173. [Google Scholar] [CrossRef]
- Foley, P.; Kirschbaum, C. Human hypothalamus–pituitary–adrenal axis responses to acute psychosocial stress in laboratory settings. Neurosci. Biobehav. Rev. 2010, 35, 91–96. [Google Scholar] [CrossRef]
- Robles, T.F.; Glaser, R.; Kiecolt-Glaser, J.K. Out of balance: A new look at chronic stress, depression, and immunity. Curr. Dir. Psychol. Sci. 2005, 14, 111–115. [Google Scholar] [CrossRef]
- Vitaliano, P.P.; Scanlan, J.M.; Zhang, J.; Savage, M.V.; Hirsch, I.B.; Siegler, I.C. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosom. Med. 2002, 64, 418–435. [Google Scholar] [CrossRef] [PubMed]
- Spruill, T.M. Chronic psychosocial stress and hypertension. Curr. Hypertens. Rep. 2010, 12, 10–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim-Fuchs, C.; Le, C.P.; Pimentel, M.A.; Shackleford, D.; Ferrari, D.; Angst, E.; Hollande, F.; Sloan, E.K. Chronic stress accelerates pancreatic cancer growth and invasion: A critical role for beta-adrenergic signaling in the pancreatic microenvironment. Brain Behav. Immun. 2014, 40, 40–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, X.; Zhang, Y.; He, Z.; Yin, K.; Li, B.; Zhang, L.; Xu, Z. Chronic stress promotes gastric cancer progression and metastasis: An essential role for ADRB2. Cell Death Dis. 2019, 10, 788. [Google Scholar] [CrossRef] [Green Version]
- Saul, A.N.; Oberyszyn, T.; Daugherty, C.; Kusewitt, D.; Jones, S.; Jewell, S.; Malarkey, W.B.; Lehman, A.; Lemeshow, S.; Dhabhar, F.S. Chronic stress and susceptibility to skin cancer. J. Natl. Cancer Inst. 2005, 97, 1760–1767. [Google Scholar] [CrossRef] [Green Version]
- Thaker, P.H.; Lutgendorf, S.K.; Sood, A.K. The neuroendocrine impact of chronic stress on cancer. Cell Cycle 2007, 6, 430–433. [Google Scholar] [CrossRef] [Green Version]
- Craig, A.; Hancock, K.; Craig, M. The lifestyle appraisal questionnaire: A comprehensive assessment of health and stress. Psychol. Health 1996, 11, 331–343. [Google Scholar] [CrossRef]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Kirschbaum, C.; Pirke, K.-M.; Hellhammer, D.H. The ‘Trier Social Stress Test’–a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology 1993, 28, 76–81. [Google Scholar] [CrossRef]
- Dickerson, S.S.; Kemeny, M.E. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol. Bull. 2004, 130, 355. [Google Scholar] [CrossRef] [Green Version]
- Kudielka, B.M.; Hellhammer, D.H.; Kirschbaum, C. Ten Years of Research with the Trier Social Stress Test-Revisited. In Social Neuroscience: Integrating Biological and Psychological Explanations of Social Behavior; Harmon-Jones, E., Winkielman, P., Eds.; The Guilford Press: New York, NY, USA, 2007; pp. 56–83. [Google Scholar]
- Tyrka, A.; Wier, L.; Anderson, G.; Wilkinson, C.; Price, L.; Carpenter, L. Temperament and response to the trier social stress test. Acta Psychiatr. Scand. 2007, 115, 395–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goodman, W.K.; Janson, J.; Wolf, J.M. Meta-analytical assessment of the effects of protocol variations on cortisol responses to the Trier Social Stress Test. Psychoneuroendocrinology 2017, 80, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.P.; Kennedy, P.J.; Cryan, J.F.; Dinan, T.G.; Clarke, G. Biological and psychological markers of stress in humans: Focus on the Trier Social Stress Test. Neurosci. Biobehav. Rev. 2014, 38, 94–124. [Google Scholar] [CrossRef] [PubMed]
- Fries, E.; Hellhammer, D.H.; Hellhammer, J. Attenuation of the hypothalamic–pituitary–adrenal axis responsivity to the Trier Social Stress Test by the benzodiazepine alprazolam. Psychoneuroendocrinology 2006, 31, 1278–1288. [Google Scholar] [CrossRef]
- Combatalade, D. Basics of Heart Rate Variability Applied to Psychophysiology; Thought Technology Ltd.: Montreal, QC, Canada, 2013. [Google Scholar]
- Welch, P. The use of fast Fourier transform for the estimation of power spectra: A method based on time averaging over short, modified periodograms. IEEE Trans. Audio Electroacoust. 1967, 15, 70–73. [Google Scholar] [CrossRef] [Green Version]
- Tarvainen, M.P.; Niskanen, J.-P.; Lipponen, J.A.; Ranta-Aho, P.O.; Karjalainen, P.A. Kubios HRV–heart rate variability analysis software. Comput. Methods Programs Biomed. 2014, 113, 210–220. [Google Scholar] [CrossRef]
- Tarvainen, M.P.; Ranta-Aho, P.O.; Karjalainen, P.A. An advanced detrending method with application to HRV analysis. IEEE Trans. Biomed. Eng. 2002, 49, 172–175. [Google Scholar] [CrossRef]
- Van Roon, A.M.; Mulder, L.J.; Althaus, M.; Mulder, G. Introducing a baroreflex model for studying cardiovascular effects of mental workload. Psychophysiology 2004, 41, 961–981. [Google Scholar] [CrossRef]
- Taylor, J.A.; Carr, D.L.; Myers, C.W.; Eckberg, D.L. Mechanisms underlying very-low-frequency RR-interval oscillations in humans. Circulation 1998, 98, 547–555. [Google Scholar] [CrossRef] [Green Version]
- Berntson, G.G.; Thomas Bigger, J., Jr.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, J.P.; Stone, P.H.; et al. Heart rate variability: Origins, methods, and interpretive caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef]
- Lucini, D.; Norbiato, G.; Clerici, M.; Pagani, M. Hemodynamic and autonomic adjustments to real life stress conditions in humans. Hypertension 2002, 39, 184–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaegi, D.M.; Halamek, L.P.; Van Hare, G.F.; Howard, S.K.; Dubin, A.M. Effect of mental stress on heart rate variability: Validation of simulated operating and delivery room training modules. Pediatr. Res. 1999, 45, 77. [Google Scholar] [CrossRef] [Green Version]
- Zalucky, A.A.; Nicholl, D.D.M.; Hanly, P.J.; Poulin, M.J.; Turin, T.C.; Walji, S.; Handley, G.B.; Raneri, J.K.; Sola, D.Y.; Ahmed, S.B. Nocturnal hypoxemia severity and renin–angiotensin system activity in obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 2015, 192, 873–880. [Google Scholar] [CrossRef]
- Hanly, P.J.; Ahmed, S.B. Sleep apnea and the kidney: Is sleep apnea a risk factor for chronic kidney disease? Chest 2014, 146, 1114–1122. [Google Scholar] [CrossRef]
- Hjortskov, N.; Rissén, D.; Blangsted, A.K.; Fallentin, N.; Lundberg, U.; Søgaard, K. The effect of mental stress on heart rate variability and blood pressure during computer work. Eur. J. Appl. Physiol. 2004, 92, 84–89. [Google Scholar] [CrossRef]
- Everly, G.S.; Lating, J.M. The anatomy and physiology of the human stress response. In A Clinical Guide to the Treatment of the Human Stress Response; Springer: Berlin/Heidelberg, Germany, 2019; pp. 19–56. [Google Scholar]
- Lusardi, P.; Mugellini, A.; Preti, P.; Zoppi, A.; Derosa, G.; Fogari, R. Effects of a restricted sleep regimen on ambulatory blood pressure monitoring in normotensive subjects. Am. J. Hypertens. 1996, 9, 503–505. [Google Scholar] [CrossRef] [Green Version]
- Tochikubo, O.; Ikeda, A.; Miyajima, E.; Ishii, M. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension 1996, 27, 1318–1324. [Google Scholar] [CrossRef]
- Âkerstedt, T. Psychosocial stress and impaired sleep. Scand. J. Work Environ. Health 2006, 32, 493–501. [Google Scholar] [CrossRef] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).