Correlation between Overconfidence and Learning Motivation in Postgraduate Infection Prevention and Control Training
Abstract
1. Introduction
- -
- HCW’s self-assessment, self-reported competencies, and knowledge of infection control methods;
- -
- Levels of the four SIMS-dimensions; and
- -
- Self-evaluation of adherence to the 5 WHO Hand Hygiene indications in terms of percentage.
2. Methods
2.1. Study Design and Variables
2.2. Measurements
- After moving a used patient bed (WHO 5)
- After contaminating your hand with urine (WHO 3)
- Before connecting an infusion to an IV line (WHO 2)
- After shaking hands with a patient (WHO 4)
- Before connecting a urinary catheter to a collection bag (WHO 2)
- After helping a patient up after a fall (WHO 4)
- Before shaking hands with a patient (WHO 1)
- Before positioning a patient on an operation table (WHO 1)
- After picking up a patient’s towel that has fallen to the ground in the lavatory (WHO 5)
2.3. Setting and Participants
2.4. Statistical Methods
3. Results
3.1. Description of the Sample
3.2. Hypotheses Testing
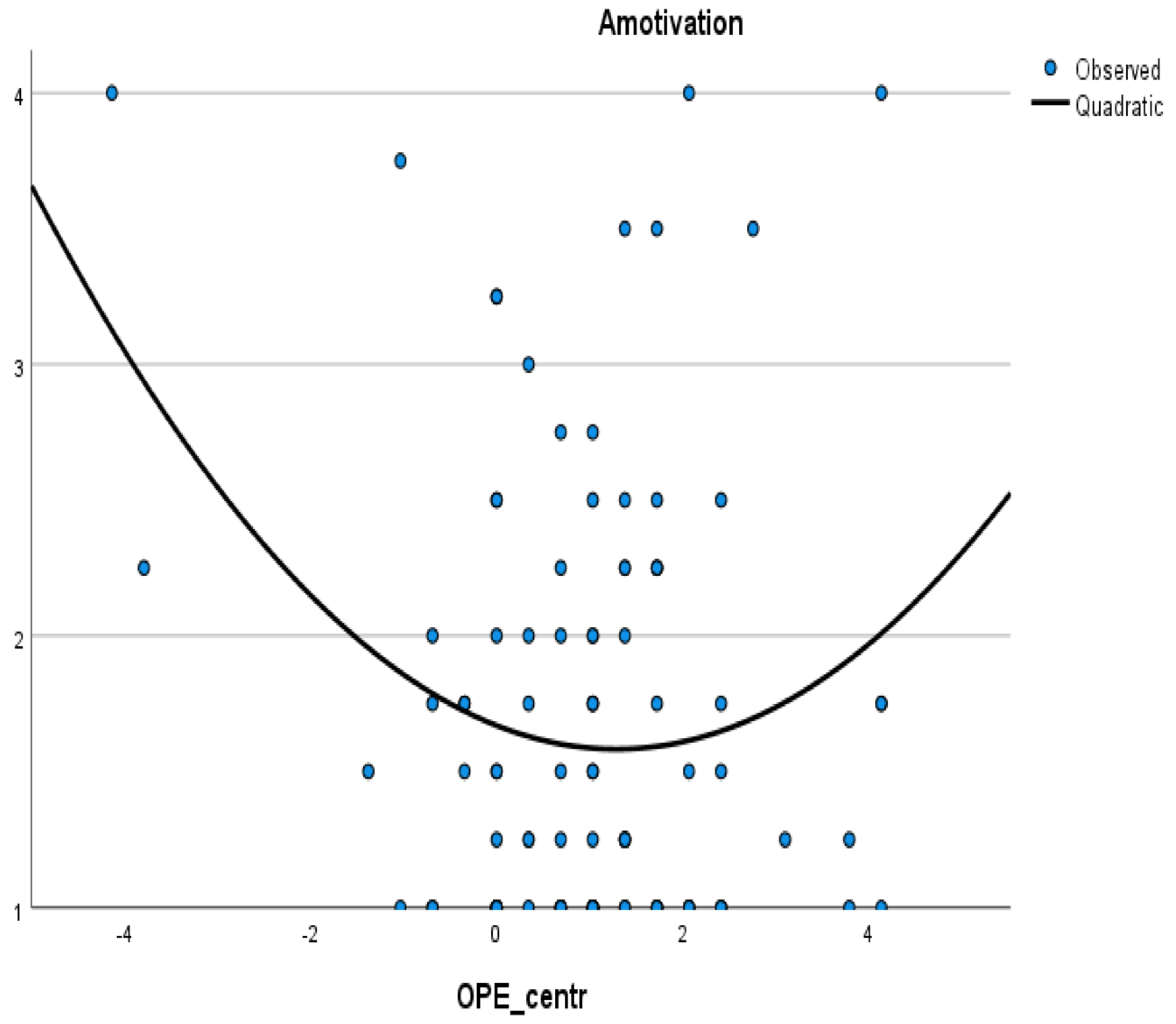
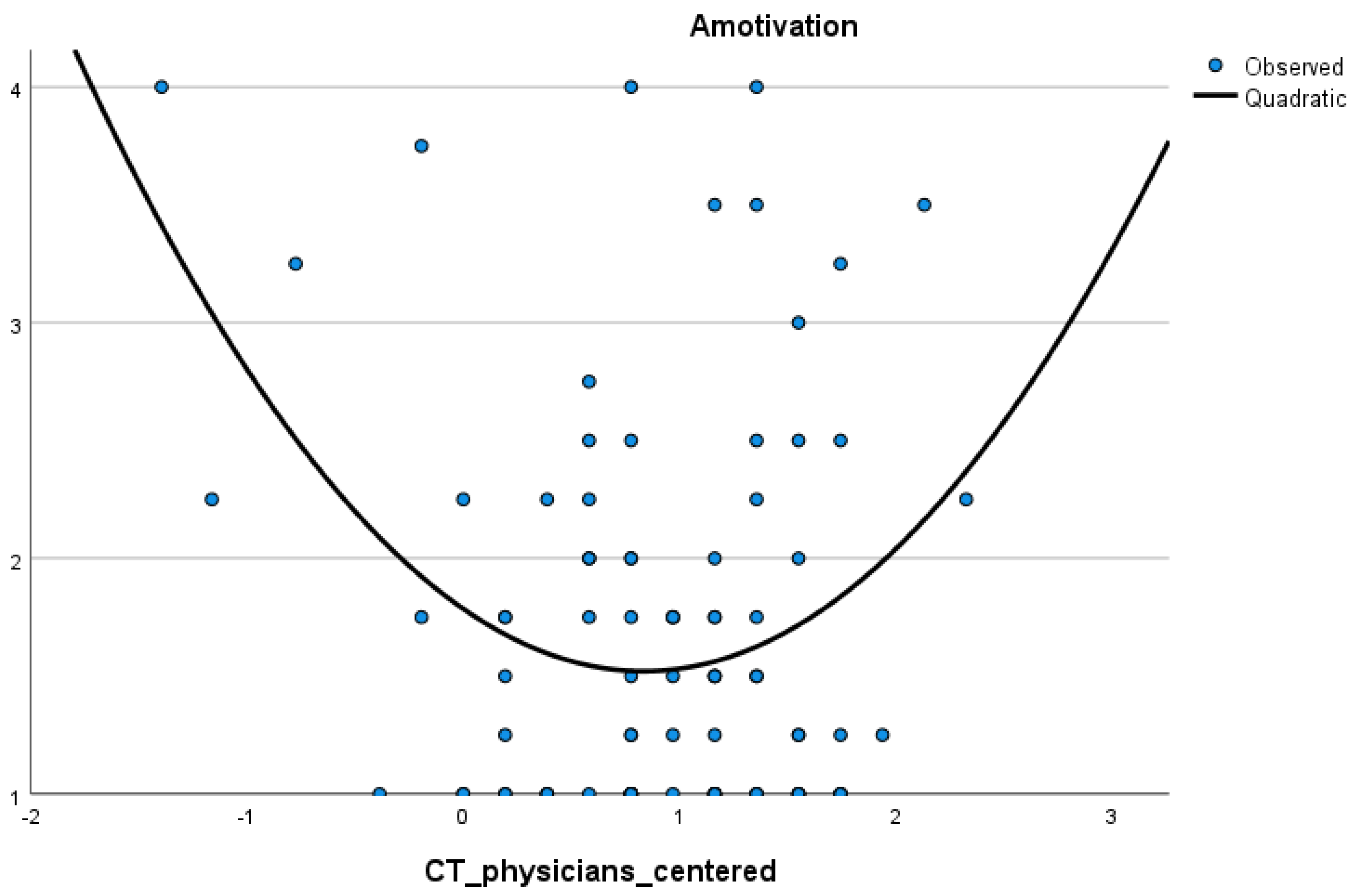
3.2.1. H1a and H1b: Correlations between Overplacement, Clinical Tribalism, and Amotivation
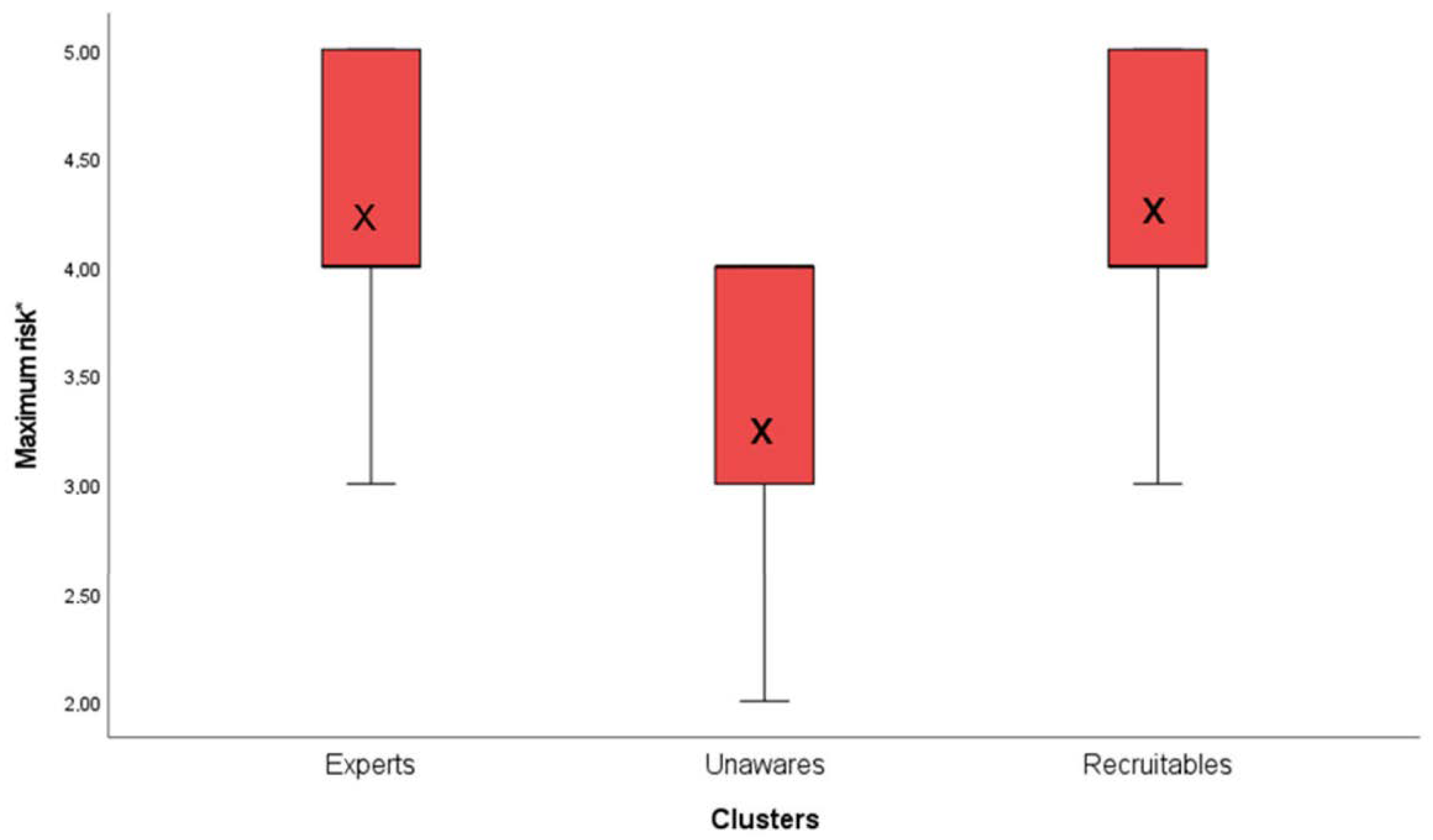
3.2.2. H2a: K-Means Cluster Analysis
3.2.3. H2b: External Validation of the Three-Cluster Solution: One-Way ANOVAs
3.3. Description of the Clusters
3.3.1. Cluster 1—“Experts”
3.3.2. Cluster 2—“Unawares”
3.3.3. Cluster 3—“Recruitables”
4. Discussion
4.1. Hypothesis H1a and H1b
4.2. Hypothesis H2a and H2b
- (a)
- Amotivated and highly overestimated persons partially aware of their inadequate competencies and with a poor understanding of the risks of incorrect hand hygiene (“Unawares”);
- (b)
- Persons with moderate overestimation, intermediate performance, well-motivated, and appropriate risk assessment (“Recruitables”); and
- (c)
- Highly motivated persons with real confidence in their skills, above-average performance in self-assessed adherence to protocols, and a thorough understanding of the risks of incorrect hand hygiene (“Experts”).
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mathai, E.; Allegranzi, B.; Kilpatrick, C.; Pittet, D. Prevention and control of health care-associated infections through improved hand hygiene. Indian J. Med. Microbiol. 2010, 28, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Movement, P.S. A Person-Centered Healthcare System Must Approach Improvement through the Eyes of the Patient and Family. Available online: https://patientsafetymovement.org/clinical-support-products-and-services/apss-blueprints/ (accessed on 1 November 2020).
- Pittet, D.; Allegranzi, B.; Boyce, J. The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infect. Control Hosp. Epidemiol. 2009, 30, 611–622. [Google Scholar] [CrossRef] [PubMed]
- Luangasanatip, N.; Hongsuwan, M.; Limmathurotsakul, D.; Lubell, Y.; Lee, A.S.; Harbarth, S.; Day, N.P.; Graves, N.; Cooper, B.S. Comparative efficacy of interventions to promote hand hygiene in hospital: Systematic review and network meta-analysis. BMJ 2015, 351, h3728. [Google Scholar] [CrossRef] [PubMed]
- McGuckin, M.; Storr, J.; Longtin, Y.; Allegranzi, B.; Pittet, D. Patient empowerment and multimodal hand hygiene promotion: A win-win strategy. Am. J. Med. Qual. 2011, 26, 10–17. [Google Scholar] [CrossRef][Green Version]
- Harris, M.M.; Yuan, J. “Oh, no, not another hand-washing in-service!”. Gastroenterol. Nurs. 1994, 16, 269–272. [Google Scholar] [CrossRef]
- Bushuven, S.; Dettenkofer, M.; Sippel, S.; Koenig, S.; Bushuven, S.; Schneider-Brachert, W. Speaking up behavior and cognitive bias in hand hygiene: Competences of German-speaking medical students. PLoS ONE 2020, 15, e0239444. [Google Scholar] [CrossRef]
- Allegranzi, B.; Pittet, D. Role of hand hygiene in healthcare-associated infection prevention. J. Hosp. Infect. 2009, 73, 305–315. [Google Scholar] [CrossRef]
- Dunning, D.; Heath, C.; Suls, J.M. Flawed Self-Assessment: Implications for Health, Education, and the Workplace. Psychol. Sci. Public Interest 2004, 5, 69–106. [Google Scholar] [CrossRef]
- Loughran, T.A.; Paternoster, R.; Piquero, A.R.; Fagan, J. “A Good Man Always Knows His Limitations”: The Role of Overconfidence in Criminal Offending. J. Res. Crime Delinq. 2012, 50, 327–358. [Google Scholar] [CrossRef]
- Malmendier, U.; Tate, G. CEO Overconfidence and Corporate Investment. J. Financ. 2005, 60, 2661–2700. [Google Scholar] [CrossRef]
- Sandroni, A.; Squintani, F. A survey on overconfidence, insurance and self-assessment training programs. 2004, unpublished report. Available online: https://warwick.ac.uk/fac/soc/economics/staff/fsquintani/research/survey_overconfidence.pdf. (accessed on 11 January 2022).
- Moore, D.A.; Healy, P.J. The trouble with overconfidence. Psychol. Rev. 2008, 115, 502–517. [Google Scholar] [CrossRef] [PubMed]
- Braithwaite, J.; Clay-Williams, R.; Vecellio, E.; Marks, D.; Hooper, T.; Westbrook, M.; Westbrook, J.; Blakely, B.; Ludlow, K. The basis of clinical tribalism, hierarchy and stereotyping: A laboratory-controlled teamwork experiment. BMJ Open 2016, 6, e012467. [Google Scholar] [CrossRef] [PubMed]
- Dunlosky, J.; Rawson, K. Overconfidence produces underachievement: Inaccurate self evaluations undermine students’ learning and retention. Learn. Instr. 2012, 22, 271–280. [Google Scholar] [CrossRef]
- Caris, M.G.; Kamphuis, P.G.A.; Dekker, M.; de Bruijne, M.C.; van Agtmael, M.A.; Vandenbroucke-Grauls, C. Patient Safety Culture and the Ability to Improve: A Proof of Concept Study on Hand Hygiene. Infect. Control Hosp. Epidemiol. 2017, 38, 1277–1283. [Google Scholar] [CrossRef] [PubMed]
- Pessoa-Silva, C.L.; Posfay-Barbe, K.; Pfister, R.; Touveneau, S.; Perneger, T.V.; Pittet, D. Attitudes and perceptions toward hand hygiene among healthcare workers caring for critically ill neonates. Infect. Control Hosp. Epidemiol. 2005, 26, 305–311. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Self-determination. Corsini Encycl. Psychol. 2010, 1–2. [Google Scholar] [CrossRef]
- Deci, E.L.; Ryan, R.M. Self-determination theory. In Handbook of Theories of Social Psychology; van Lange, P.A.M., Kruglanski, A.W., Higgins, E.T., Eds.; Sage Publications Ltd: Newbury Park, CA, USA, 2012. [Google Scholar]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Springer Science & Business Media: Berlin/Heidelberg, Germany, 1985. [Google Scholar]
- Ryan, R.M.; Deci, E.L. Intrinsic and extrinsic motivations: Classic definitions and new directions. Contemp. Educ. Psychol. 2000, 25, 54–67. [Google Scholar] [CrossRef]
- Howard, J.L.; Bureau, J.; Guay, F.; Chong, J.X.Y.; Ryan, R.M. Student Motivation and Associated Outcomes: A Meta-Analysis From Self-Determination Theory. Perspect. Psychol. Sci. 2021, 16, 1300–1323. [Google Scholar] [CrossRef]
- Østerlie, O.; Løhre, A.; Haugan, G. The Situational Motivational Scale (SIMS) in physical education: A validation study among Norwegian adolescents. Cogent Educ. 2019, 6, 1603613. [Google Scholar] [CrossRef]
- Chiozza, M.L.; Ponzetti, C. FMEA: A model for reducing medical errors. Clin. Chim. Acta 2009, 404, 75–78. [Google Scholar] [CrossRef]
- Ball, H.L. Conducting Online Surveys. J. Hum. Lact. 2019, 35, 413–417. [Google Scholar] [CrossRef] [PubMed]
- Freund, R.J.; Littell, R.C.; Creighton, L. Regression Using JMP; SAS Institute: Cary, NC, USA, 2003. [Google Scholar]
- Field, A. Discovering Statistics Using IBM SPSS Statistics; Sage: Newbury Park, CA, USA, 2013. [Google Scholar]
- Flachaire, E. Bootstrapping heteroskedastic regression models: Wild bootstrap vs. pairs bootstrap. Comput. Stat. Data Anal. 2005, 49, 361–376. [Google Scholar] [CrossRef]
- Peterson, A.D.; Ghosh, A.P.; Maitra, R. Merging K-means with hierarchical clustering for identifying general-shaped groups. Stat 2018, 7, e172. [Google Scholar] [CrossRef] [PubMed]
- Sambandam, R. Cluster Analysis Gets Complicated. Mark. Res. 2003, 15, 16–21. [Google Scholar]
- Formann, A.K. Die Latent-Class-Analyse: Einführung in Theorie und Anwendung; Beltz: Weinheim, Germany, 1984. [Google Scholar]
- Rousseeuw, P.J. Silhouettes: A graphical aid to the interpretation and validation of cluster analysis. J. Comput. Appl. Math. 1987, 20, 53–65. [Google Scholar] [CrossRef]
- Zhang, G. A Parametric Bootstrap Approach for One-Way ANOVA under Unequal Variances with Unbalanced Data. Commun. Stat. Simul. Comput. 2015, 44, 827–832. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Statistisches Bundesamt. Gesundheit; Gesundheitspersonal. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Gesundheitspersonal/_inhalt.html (accessed on 11 November 2021).
- Statistisches Bundesamt. 3,63 Millionen Beschäftigte Im Gesundheitswesen Haben Direkten Patientenkontakt. Pressemitteilung Nr. N085 vom 23. December 2020. Available online: https://www.destatis.de/DE/Presse/Pressemitteilungen/2020/12/PD20_N085_224.html;jsessionid=589CD1F809E04A0452AE17EDDAD453B4.live742 (accessed on 11 November 2020).
- DiDiodato, G. An alternative methodology for interpretation and reporting of hand hygiene compliance data. Am. J. Infect. Control 2012, 40, 332–335. [Google Scholar] [CrossRef]
- Australian Health Ministers’ Advisory Council. National Hand Hygiene Audit Data—Latest Data Now Available. Available online: https://www.safetyandquality.gov.au/our-work/infection-prevention-and-control/national-hand-hygiene-initiative/national-audits-and-hhcapp/national-hand-hygiene-audit-data-latest-data-now-available (accessed on 11 January 2022).
- Legault, L.; Green-Demers, I.; Pelletier, L. Why do high school students lack motivation in the classroom? Toward an understanding of academic amotivation and the role of social support. J. Educ. Psychol. 2006, 98, 567. [Google Scholar] [CrossRef]
- Vlachopoulos, S.P.; Katartzi, E.S.; Kontou, M.G. Fitting Multidimensional Amotivation into the Self-Determination Theory Nomological Network: Application in School Physical Education. Meas. Phys. Educ. Exerc. Sci. 2013, 17, 40–61. [Google Scholar] [CrossRef]
- Allan, B.A.; Autin, K.L.; Duffy, R.D. Self-Determination and Meaningful Work: Exploring Socioeconomic Constraints. Front. Psychol. 2016, 7, 71. [Google Scholar] [CrossRef] [PubMed]
- Scheithauer, S.; Batzer, B.; Dangel, M.; Passweg, J.; Widmer, A. Workload even affects hand hygiene in a highly trained and well-staffed setting: A prospective 365/7/24 observational study. J. Hosp. Infect. 2017, 97, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Scheithauer, S.; Oude-Aost, J.; Heimann, K.; Haefner, H.; Schwanz, T.; Waitschies, B.; Kampf, G.; Orlikowsky, T.; Lemmen, S.W. Hand hygiene in pediatric and neonatal intensive care unit patients: Daily opportunities and indication- and profession-specific analyses of compliance. Am. J. Infect. Control 2011, 39, 732–737. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, C.H. Impact of nosocomial infections on hospital costs. Hosp. Formul. 1993, 28 (Suppl. S1), 51–54. [Google Scholar]
- Gálvez-Vargas, R.; Bueno-Cavanillas, A.; García-Martín, M. Epidemiology, therapy and costs of nosocomial infection. Pharmacoeconomics 1995, 7, 128–140. [Google Scholar] [CrossRef]
- Williams, B.W.; Byrne, P.D.; Welindt, D.; Williams, M.V. Miller’s Pyramid and Core Competency Assessment: A Study in Relationship Construct Validity. J. Contin. Educ. Health Prof. 2016, 36, 295–299. [Google Scholar] [CrossRef]
- Schwappach, D.L.; Gehring, K. Silence that can be dangerous: A vignette study to assess healthcare professionals’ likelihood of speaking up about safety concerns. PLoS ONE 2014, 9, e104720. [Google Scholar] [CrossRef]
- Lutze, B.; Chaberny, I.F.; Graf, K.; Krauth, C.; Lange, K.; Schwadtke, L.; Stahmeyer, J.; von Lengerke, T. Intensive care physicians’ and nurses’ perception that hand hygiene prevents pathogen transmission: Belief strength and associations with other cognitive factors. J. Health Psychol. 2017, 22, 89–100. [Google Scholar] [CrossRef]
- Sahay, S.; Panja, S.; Ray, S.; Rao, B.K. Diurnal variation in hand hygiene compliance in a tertiary level multidisciplinary intensive care unit. Am. J. Infect. Control 2010, 38, 535–539. [Google Scholar] [CrossRef]
- Khazaal, Y.; van Singer, M.; Chatton, A.; Achab, S.; Zullino, D.; Rothen, S.; Khan, R.; Billieux, J.; Thorens, G. Does Self-Selection Affect Samples’ Representativeness in Online Surveys? An Investigation in Online Video Game Research. J. Med. Internet Res. 2014, 16, e164. [Google Scholar] [CrossRef] [PubMed]
- Cole, M. Using a motivational paradigm to improve handwashing compliance. Nurse Educ. Pract. 2006, 6, 156–162. [Google Scholar] [CrossRef] [PubMed]
- Bortz, J.; Döring, N. Forschungsmethoden und Evaluation für Human-und Sozialwissenschaftler; 3. überarbeitete Auflage; Springer GmbH: Heidelberg, Germany, 2002. [Google Scholar]
- Von Lengerke, T.; Lutze, B.; Graf, K.; Krauth, C.; Lange, K.; Schwadtke, L.; Stahmeyer, J.; Chaberny, I.F. Psychosocial determinants of self-reported hand hygiene behaviour: A survey comparing physicians and nurses in intensive care units. J. Hosp. Infect. 2015, 91, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Salibian-Barrera, M.; Zamar, R.H. Bootstrapping robust estimates of regression. Ann. Stat. 2002, 30, 556–582. [Google Scholar] [CrossRef]
| Characteristic | n (%) | Mean (Standard Deviation) | |
|---|---|---|---|
| Age (years) | 103 | 36.43 (17.31) | |
| Gender | Male | 21 (20.4%) | |
| Female | 79 (76.7%) | ||
| Divers/transgender/trans identical | 1 (1%) | ||
| Profession | Nurses | 51 (49.5%) | |
| Physicians | 12 (11.7%) | ||
| Paramedics | 3 (3.2%) | ||
| Others | 36 (35%) | ||
| Professional training | Completed | 99 (93.2%) | |
| Trainee | 4 (3.9%) | ||
| Workplace | Ambulant | 7 (6.8%) | |
| Primary hospitals | |||
| Secondary hospitals | 17 (16.5%) | ||
| Tertiary hospitals | 36 (35%) | ||
| (University hospitals) | 19 (18.4%) |
| Variable | Pearson Correlation ® | Intrinsic Motivation | Identified Regulation | External Regulation | Amotivation | Self-Assessment | Overplacement | Clinical Tribalism Nurses vs. Paramedics | Clinical Tribalism Nurses vs. Physicians | Indicated Situations (WHO) | Non-Indicated Situations (WHO) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% BCa Confidence Interval | |||||||||||
| Intrinsic motivation | - | ||||||||||
| Identified regulation | r BCa 95% | 0.77 ** {0.70–0.85] | - | ||||||||
| External regulation | r BCa 95% | −0.47 ** {−0.62–0.65] | −0.51 ** [−0.26–0.39] | - | |||||||
| Amotivation | r BCa 95% | −0.55 ** [−0.68–−0.81} | −0.71 ** [−0.89–−0.59] | 0.35 ** [−0.31–0.09] | - | ||||||
| Self-assessment of own proficiencies | r BCa 95% | 0.16 [−0.04–0.40] | 0.12 [−0.34–0.28] | −0.09 [−0.31–0.09] | 0.092 [−0.34–0.23] | - | |||||
| Overplacement | r BCa 95% | 0.13 [−0.12–0.42] | 0.12 [−0.14–0.48] | 0.03 [−0.16–0.18] | −0.04 [−0.39–0.27] | 0.48 ** [0.22–0.67] | - | ||||
| Clinical tribalism nurses vs. paramedics | r BCa 95% | 0.03 [−0.19–0.25] | −0.04 [−0.22–0.26] | 0.06 [−0.20–0.26] | 0.03 [−0.17–0.23] | 0.32 ** [0.06–0.46] | 0.33 ** [0.17–0.50] | - | |||
| Clinical tribalism nurses vs. physicians | r BCa 95% | 0.10 [−0.12–0.36] | 0.17 [−0.06–0.47] | 0.12 [−0.07–0.26] | −0.11 [−0.44–0.16] | 0.40 ** [0.06–0.50] | 0.25 * [−0.06–0.50] | 0.46 ** [0.27–0.63] | - | ||
| Indicated situations (WHO) | r BCa 95% | −0.01 [−0.23–0.22] | −0.005 [−0.17–0.19] | −0.23 [−0.44–0.02] | 0.16 [−0.05–0.34] | 0.19 [−0.04–0.42] | −0.13 [−0.30–0.06] | 0.11 [−0.09–0.29] | 0.07 [−0.13–0.27] | ||
| Non-Indicated situations (WHO) | r BCa 95% | −0.20 [−0.38–−0.02] | −0.10 [−0.30–0.09] | 0.03 [−0.21–0.26] | 0.16 [0.003–0.32] | 0.24 [0.04–0.44] | −0.05 [−0.22–0.11] | −0.09 [−0.29–0.09] | 0.08 [−0.10–0.24] | 0.50 ** | - |
| Mean Values of the Dependent Variable in Clusters | (A) Cluster | (B) Cluster | (A)–(B) Difference between Means | BCa 95% Confidence Interval Lower | BCa 95% Confidence Interval Upper |
|---|---|---|---|---|---|
| Experts (M1 = 4.17) | Experts | Unawares | 0.79 * | 0.30 | 1.30 |
| Experts | Recruitables | −0.04 | −0.41 | 0.34 | |
| Unawares (M2 = 3.38) | Unawares | Experts | −0.79 * | −1.27 | −0.33 |
| Unawares | Recruitables | −0.83 * | −1.32 | −0.41 | |
| Recruitables M3 = 4.20 | Recruitables | Experts | 0.04 | −0.34 | 0.41 |
| Recruitables | Unawares | 0.83 * | 0.35 | 1.35 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trifunovic-Koenig, M.; Bushuven, S.; Gerber, B.; Otto, B.; Dettenkofer, M.; Salm, F.; Fischer, M.R. Correlation between Overconfidence and Learning Motivation in Postgraduate Infection Prevention and Control Training. Int. J. Environ. Res. Public Health 2022, 19, 5763. https://doi.org/10.3390/ijerph19095763
Trifunovic-Koenig M, Bushuven S, Gerber B, Otto B, Dettenkofer M, Salm F, Fischer MR. Correlation between Overconfidence and Learning Motivation in Postgraduate Infection Prevention and Control Training. International Journal of Environmental Research and Public Health. 2022; 19(9):5763. https://doi.org/10.3390/ijerph19095763
Chicago/Turabian StyleTrifunovic-Koenig, Milena, Stefan Bushuven, Bianka Gerber, Baerbel Otto, Markus Dettenkofer, Florian Salm, and Martin R. Fischer. 2022. "Correlation between Overconfidence and Learning Motivation in Postgraduate Infection Prevention and Control Training" International Journal of Environmental Research and Public Health 19, no. 9: 5763. https://doi.org/10.3390/ijerph19095763
APA StyleTrifunovic-Koenig, M., Bushuven, S., Gerber, B., Otto, B., Dettenkofer, M., Salm, F., & Fischer, M. R. (2022). Correlation between Overconfidence and Learning Motivation in Postgraduate Infection Prevention and Control Training. International Journal of Environmental Research and Public Health, 19(9), 5763. https://doi.org/10.3390/ijerph19095763







