Burnout Syndrome and Related Factors in Mexican Police Workforces
Abstract
:1. Introduction
2. Materials and Methods
Analysis of Sociodemographic, Work, and Health Factors
3. Results
3.1. Mexico Police Workforce Characterization
3.2. Characteristics of Burnout Syndrome in the Population
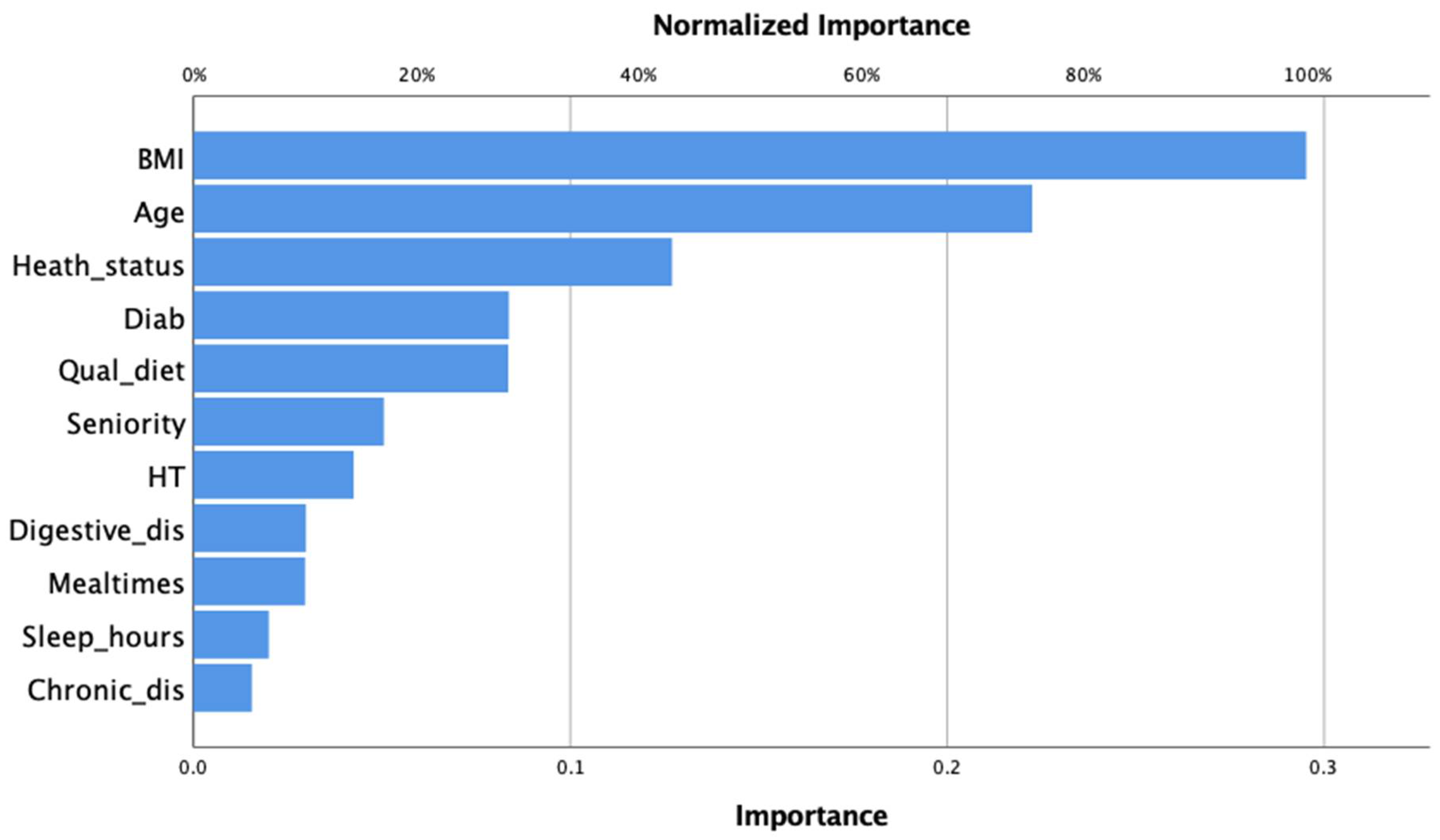
3.3. Multilayer Perceptron Neuronal Network of BO and Related Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leka, S.; Griffiths, A.; Cox, T.; WHO. Work Organisation and Stress: Systematic Problem Approaches for Employers, Managers and Trade Union Representatives, 1st ed.; WHO: Geneva, Switzerland, 2003. [Google Scholar]
- Fernando, Z.T. Validación del Cuestionario de Subtipos Clínicos de Burnout BCSQ-36 en Personal de Atención Primaria; Universidad de Zaragoza: Zaragoza, Spain, 2016. [Google Scholar]
- Corredor Pinzón, N.E.; Marín Torres, L. Burnout en miembros de la Policía Nacional de Colombia: Un análisis crítico. Sinapsis 2013, 5, 62–73. [Google Scholar]
- Danhof-Pont, M.B.; van Veen, T.; Zitman, F.G. Biomarkers in burnout: A systematic review. J. Psychosom. Res. 2011, 70, 505–524. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Organ. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Gil-Monte, P.R. Factorial validity of the Maslach Burnout Inventory (MBI-HSS) among Spanish professionals. Rev. Saude Publica 2005, 39, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Weber, A.; Jaekel-Reinhard, A. Burnout Syndrome: A Disease of Modern Societies? Occup. Med. 2000, 50, 512–517. [Google Scholar] [CrossRef] [Green Version]
- Bayes, A.; Tavella, G.; Parker, G. The biology of burnout: Causes and consequences. World J. Biol. Psychiatry 2021, 22, 686–698. [Google Scholar] [CrossRef]
- Police, Court and Prison Personnel Statistics. Eurosat, Statistics Explained. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Police,_court_and_prison_personnel_statistics&oldid=540991#cite_note-2 (accessed on 26 April 2022).
- 2019 Crime United States: Police Employee Data; Federal Bureau of Investigation: Uniform Crime Reporting Program. Available online: https://ucr.fbi.gov/crime-in-the-u.s/2019/crime-in-the-u.s.-2019/topic-pages/police-employee-data (accessed on 26 April 2022).
- Kappeler, V.E.; Eastern, K.U. Critical Issues in Police Civil Liabitity, 4th ed.; Waveland Press, Inc.: Long Grove, IL, USA, 2006; ISBN 978-1-57766-441-3. [Google Scholar]
- Collins, P.A.; Gibbs, A.C.C. Stress in police officers: A study of the origins, prevalence and severity of stress-related symptoms within a county police force. Occup. Med. 2003, 53, 256–264. [Google Scholar] [CrossRef] [Green Version]
- Galanis, P.; Fragkou, D.; Katsoulas, T.A. Risk factors for stress among police officers: A systematic literature review. Work 2021, 68, 1255–1272. [Google Scholar] [CrossRef]
- Wu, X.; Liu, Q.; Li, Q.; Tian, Z.; Tan, H. Health-Related Quality of Life and Its Determinants among Criminal Police Officers. Int. J. Environ. Res. Public Health 2019, 16, 1398. [Google Scholar] [CrossRef] [Green Version]
- Skogstad, M.; Skorstad, M.; Lie, A.; Conradi, H.S.; Heir, T.; Weisæth, L. Work-related post-traumatic stress disorder. Occup. Med. 2013, 63, 175–182. [Google Scholar] [CrossRef] [Green Version]
- Irizar, P.; Puddephatt, J.A.; Gage, S.H.; Fallon, V.; Goodwin, L. The prevalence of hazardous and harmful alcohol use across trauma-exposed occupations: A meta-analysis and meta-regression. Drug Alcohol Depend. 2021, 226, 108858. [Google Scholar] [CrossRef]
- Stanley, I.H.; Hom, M.A.; Joiner, T.E. A systematic review of suicidal thoughts and behaviors among police officers, firefighters, EMTs, and paramedics. Clin. Psychol. Rev. 2016, 44, 25–44. [Google Scholar] [CrossRef] [Green Version]
- Brunault, P.; Lebigre, K.; Idbrik, F.; Maugé, D.; Adam, P.; El Ayoubi, H.; Hingray, C.; Barrault, S.; Grall-Bronnec, M.; Ballon, N.; et al. Posttraumatic Stress Disorder Is a Risk Factor for Multiple Addictions in Police Officers Hospitalized for Alcohol. Eur. Addict. Res. 2019, 25, 198–206. [Google Scholar] [CrossRef]
- Di Nota, P.M.; Anderson, G.S.; Ricciardelli, R.; Carleton, R.N.; Groll, D. Mental disorders, suicidal ideation, plans and attempts among Canadian police. Occup. Med. 2020, 70, 183–190. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, J.S. Personal problems of the police officer: A plea for action. In Job Stress and Police Officer; Government Printing Office: Washington, DC, USA, 1975. [Google Scholar]
- Kroes, W.H. Society’s Victim—The Policeman—An Analysis of Job Stress in Policing; U.S. Department of Justice: Springfield, IL, USA, 1976.
- Stratton, J.G. Police stress: An overview. Police Chief 1978, 4, 58–62. [Google Scholar]
- Shiozaki, M.; Miyai, N.; Morioka, I.; Utsumi, M.; Koike, H.; Arita, M.; Miyashita, K. Assessment of the risk of ischemic heart disease and its relevant factors among Japanese police officers. Sangyo Eiseigaku Zasshi 2013, 55, 115–124. [Google Scholar] [CrossRef] [Green Version]
- Ganesh, K.S.; Naresh, A.G.V.; Bammigatti, C. Prevalence and Risk Factors of Hypertension Among Male Police Personnel in Urban Puducherry, India. Kathmandu Univ. Med. J. 2014, 12, 242–246. [Google Scholar] [CrossRef] [Green Version]
- Franke, W.D.; Cox, D.F.; Schultz, D.P.; Anderson, D.F. Coronary heart disease risk factors in employees of Iowa’s Department of Public Safety compared to a cohort of the general population. Am. J. Ind. Med. 1997, 31, 733–737. [Google Scholar] [CrossRef]
- Wirth, M.D.; Andrew, M.E.; Burchfiel, C.M.; Burch, J.B.; Fekedulegn, D.; Hartley, T.A.; Charles, L.E.; Violanti, J.M. Association of shiftwork and immune cells among police officers from the Buffalo Cardio-Metabolic Occupational Police Stress study. Chronobiol. Int. 2017, 34, 721–731. [Google Scholar] [CrossRef]
- Yates, J.D.; Aldous, J.W.F.; Bailey, D.P.; Chater, A.M.; Mitchell, A.C.S.; Richards, J.C. The Prevalence and Predictors of Hypertension and the Metabolic Syndrome in Police Personnel. Int. J. Environ. Res. Public Health 2021, 18, 6728. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística y Geografía. Encuesta Nacional de Estándales y Capacitación Profesional Policial; Instituto Nacional de Estadística y Geografía: Mexico, Mexico, 2018. [Google Scholar]
- Anshel, M.H. A Conceptual Model and Implications for Coping with Stressful Events in Police Work. Crim. Justice Behav. 2000, 27, 375–400. [Google Scholar] [CrossRef]
- Wirth, T.; Mette, J.; Prill, J.; Harth, V.; Nienhaus, A. Working conditions, mental health and coping of staff in social work with refugees and homeless individuals: A scoping review. Health Soc. Care Community 2019, 27, e257–e269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De la Fuente Solana, E.I.; Aguayo Extremera, R.; Vargas Pecino, C.; Cañadas de la Fuente, G.R. Prevalence and risk factors of burnout syndrome among Spanish police officers. Psicothema 2013, 25, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Harizanova, S.N.; Tarnovska, T.H. Professional Burnout Syndrome Among Correctional Facility Officers. Folia Med. 2013, 55, 73–79. [Google Scholar] [CrossRef] [Green Version]
- Briones Mella, D.; Kinkead Boutin, A.P. Burnout and Coping Strategies in Male Staff from National Police in Valparaíso, Chile. Iran. J. Public Health 2013, 42, 950–959. [Google Scholar]
- Dean, A.; Sullivan, K.; Soe, M. OpenEpi: Open Source Epidemiologic Statistics for Public Health; ScienceOpen, Inc.: Burlington, MA, USA, 2013. [Google Scholar]
- INEGI. Recursos Humanos Para la Seguridad Pública. In Censo Nacional de Gobierno, Seguridad Pública y Sistemas Penitenciarios. Estatales; Instituto Nacional de Estadística y Geografía. Aguascalientes, Mexico. 2015. Available online: https://www.inegi.org.mx/programas/cngspspe/2015/ (accessed on 22 February 2022).
- Miguel Sánchez-Nieto, J. Frequency of Burnout in Officers From Mexico City. Liberabit 2012, 18, 69–74. [Google Scholar]
- Olivares-Fauendez, V.E.; Mena-Miranda, L.; Jelvez-Wilker, C.; Macia-Sepulveda, F. Validez factorial del Maslach Burnout Inventory Human Services (MBI-HSS) en profesionales chilenos. Univ. Psychol. 2014, 13, 145–159. [Google Scholar] [CrossRef] [Green Version]
- Maslach, C.; Jackson, S.; Leiter, M. The Maslach Burnout Inventory Manual. In Evaluating Stress: A Book of Resources; Scarecrow Press: Maryland, MA, USA, 1997; pp. 191–218. [Google Scholar]
- Beltrán, C.A.; Moreno, M.P. Edad, síndrome de agotamiento profesional (burnout), apoyo social y autoestima en agentes de tránsito, México. Rev. Colomb. Psiquiatr. 2010, 39, 510–522. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística y Geografía. Censo Nacional de Gobiernos Municipales y Demarcaciones Territoriales de la Ciudad de México: Documento de Diseño; Instituto Nacional de Estadística y Geografía: Aguascalientes, Mexico, 2021. [Google Scholar]
- Márquez, M.A.; Galiana, L.; Oliver, A.; Sansó, N. The impact of a mindfulness-based intervention on the quality of life of Spanish national police officers. Health Soc. Care Community 2021, 29, 1491–1501. [Google Scholar] [CrossRef]
- Kop, N.; Euwema, M.; Schaufeli, W. Burnout, job stress and violent behaviour among Dutch police officers. Work Stress 1999, 13, 326–340. [Google Scholar] [CrossRef]
- Magalhães Guimarães, L.A.; Mayer, V.M.; Vieira Bueno, H.P.; Teixeira Minari, M.R.; Ferreira Martins, L. Síndrome de Bournout e qualidade de vida de policiais militares e civis. Rev. Sul-Am. Psicol. 2018, 2, 98–122. [Google Scholar]
- Yang, L.; Duan, D.; Duan, C.; Li, Z.; Liu, Y. Health status analysis of Guangzhou traffic police officers in 2013. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2014, 32, 418–420. [Google Scholar]
- Zarrinpar, A.; Chaix, A.; Panda, S. Daily Eating Patterns and Their Impact on Health and Disease. Trends Endocrinol. Metab. 2016, 27, 69–83. [Google Scholar] [CrossRef] [Green Version]
- Gil-Calderón, J.; Alonso-Molero, J.; Dierssen-Sotos, T.; Gómez-Acebo, I.; Llorca, J. Burnout syndrome in Spanish medical students. BMC Med. Educ. 2021, 21, 231. [Google Scholar] [CrossRef]
- Hernández-Martín, L.; Fernández-Calvo, B.; Ramos, F.; Contador, I. El síndrome de burnout en funcionarios de vigilancia de un centro penitenciario. Int. J. Clin. Health Psycology 2006, 6, 599–611. [Google Scholar]
- Montero-Marín, J.; García-Campayo, J. A newer and broader definition of burnout: Validation of the “Burnout Clinical Subtype Questionnaire (BCSQ-36)”. BMC Public Health 2010, 10, 302. [Google Scholar] [CrossRef] [Green Version]
- Leiter, M.P. Burnout As A Developmental Process: Consideration Of Models. In Professional Burnout; Schaufeli, W.B., Maslach, C., Maslach, C., Eds.; Taylor & Francis: London, UK, 1993; p. 14. [Google Scholar]
- Silva, D.d.e.; Merces, M.C.d.; Coelho, J.M.F.; Reis, D.A.; D’Oliveira, D., Jr. Relação entre burnout e obesidade: Revisão integrativa da literatura. Res. Soc. Dev. 2021, 10, e374101321387. [Google Scholar] [CrossRef]
- Chu, B.; Marwaha, K.; Sanvictores, T.; Ayers, D. Physiology, Stress Reaction; StatPearls Publishing: Florida, FL, USA, 2022. [Google Scholar]
- Armenta-Hernández, O.; Maldonado-Macías, A.; Camacho-Alamilla, M.D.R.; Serrano-Rosa, M.Á.; Baez-Lopez, Y.A.; Balderrama-Armendariz, C.O. The Relationship Between the Burnout Syndrome Dimensions and Body Mass Index as a Moderator Variable on Obese Managers in the Mexican Maquiladora Industry. Front. Psychol. 2021, 12, 540426. [Google Scholar] [CrossRef]
- Peterson, U.; Demerouti, E.; Bergström, G.; Samuelsson, M.; Åsberg, M.; Nygren, Å. Burnout and physical and mental health among Swedish healthcare workers. J. Adv. Nurs. 2008, 62, 84–95. [Google Scholar] [CrossRef]
- Gómez-Alcaina, B.; Montero-Marin, J.; Demarzo, M.; Pereira, J.P.; Garcia-Campayo, J. Utilidad de los marcadores biológicos en la detección precoz y prevención del síndrome de burnout. Rev. Psicopatol. y Psicol. Clín. 2013, 18, 245–253. [Google Scholar]
- Noh, J. The Effect of Circadian and Sleep Disruptions on Obesity Risk. J. Obes. Metab. Syndr. 2018, 27, 78–83. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Li, Y.; Lv, H.; Jiang, R.; Zhao, P.; Zheng, X.; Wang, L.; Li, J.; Mao, F. The prevalence and correlates of burnout among Chinese preschool teachers. BMC Public Health 2020, 20, 160. [Google Scholar] [CrossRef] [Green Version]
- Moreno Jiménez, B.; Garrosa Hernández, E.; Benevides Pereira, A.M.; Gálvez Herrer, M. Estudios transculturales del Burnout: Los Estudios transculturales Brasil-España. Rev. Colomb. Psicol. 2003, 12, 9–18. [Google Scholar]
- Nord, W.R. Social exchange theory: An integrative approach to social conformity. Psychol. Bull. 1969, 71, 174–208. [Google Scholar] [CrossRef] [Green Version]
- Rakovec-Felser, Z. No Professional Burnout as the State and Process—What to Do? Coll. Antropol. 2011, 35, 577–585. [Google Scholar] [PubMed]
- Buunk, A.P.; Zurriaga, R.; Peíro, J.M. Social comparison as a predictor of changes in burnout among nurses. Anxiety Stress Coping 2010, 23, 181–194. [Google Scholar] [CrossRef]
| Dimension | Items | Scores Cut Point | ||
|---|---|---|---|---|
| Normal | Trait | Risk | ||
| Emotional Exhaustion (EE) | 1,2,3,6,8,13,14,16,20 | 0–18 | 19–26 | 27–54 |
| Depersonanization (DP) | 5,10,11,15,22 | 0–5 | 6–9 | 10–30 |
| Personal achievement (PA) | 4,7,9,12,17,18,19,21 | 0–33 | 34–39 | 40–48 |
| Characteristic | Data |
|---|---|
| Age, mean (SD) years | 39.93 (8.66) |
| Seniority, mean (SD) years | 11.64 (8.4) |
| Body Mass Index, mean (SD) | 29.12 (4.75) |
| Education | % (CI 95% lower–upper) |
| High School | 16.13 (11.52–20.74) |
| College | 60.48 (54.36–66.61) |
| Bachelor | 20.56 (15.5–25.63) |
| Postgraduate | 2.82 (0.75–4.9) |
| Marital status | |
| Single | 14.52 (10.1–19.89) |
| Married | 73.39 (67.85–78.93) |
| Divorced | 12.1 (8.01–16.18) |
| Sleeping Hours | |
| Less than 4 h | 16.47 (11.83–21.1) |
| 4 to 6 h | 66.67 (60.77–72.56) |
| 6 to 9 h | 16.87 (12.18–21.55) |
| Work Shifts | |
| 8 h | 10.04 (6.28–13.8) |
| 12 × 12 h | 10.44 (6.62–14.27) |
| 12 × 24 h | 14.86 (10.41–19.31) |
| 24 × 24 h | 55.82 (55.82–62.03) |
| Confined | 4.01 (1.56–6.47) |
| others | 4.82 (2.14–7.5) |
| Jurisdiction | |
| Municipal | 54.84 (48.6–61.08) |
| State | 36.29 (30.26–42.32) |
| federal | 8.47 (4.98–11.96) |
| Other | 0.4 (0–1.2) |
| Functions, | |
| Operative | 85.89 (81.52–90.25) |
| Administrative | 14.11 (9.75–18.48) |
| Health Status | |
| Poor Health Perc. | 43.17 (35.99–48.34) |
| Chron. Diseases | 19.68 (14.71–24.65) |
| Hypertension | 17.27 (12.54–22.00) |
| Diabetes | 9.24 (5.62–12.86) |
| Nutrition Status | |
| Poor Diet Quality | 68.95 (61.77–75.13) |
| Regular Mealtimes | 15.66 (11.12–20.21) |
| Digestive Disorders | 30.92 (25.14–36.7) |
| Scale | Score | |||
|---|---|---|---|---|
| Mean (SD) | Normal | Trait | Risk | |
| % (CI 95% Lower–Upper) | % (CI 95% Lower–Upper) | % (CI 95% Lower–Upper) | ||
| Burnout Syndrome | 69.35 (22.17) | 18.73 (14.65–22.85) a | 57.92 (52.77–63.14) b | 23.36 (18.91–27.81) c |
| Dimensions | ||||
| Emotional Exhaustion | 23.29 (0.89) | 43.02 (37.82–48.22) | 12.82 (9.31–16.34) | 44.16 (38.94–49.38) |
| Depersonalization | 11.38 (0.58) | 34.76 (29.75–39.76) | 15.95 (12.1–19.8) | 49.29 (44.03–54.54) |
| Personal Achievement | 34.62 (0.55) | 38.18 (33.07–43.28) | 20.8 (16.53–25.06) | 41.03 (35.85–46.20) |
| Emotional Exhaustion | Depersonalization | Personal Achievement | |
|---|---|---|---|
| Age | −0.192 | −0.179 | 0.189 |
| Seniority | 0.252 | 0.213 | −0.226 |
| BMI | 0.219 | 0.152 | −0.228 |
| Health Status | −0.569 | −0.555 | 0.387 |
| Diet Quality | −0.441 | −0.428 | 0.351 |
| Since age and seniority were correlated, age was corrected for seniority, and seniority was corrected for age. All correlations were significant at the level of 0.01 | |||
| Emotional Exhaustion | Depersonalization | Personal Achievement | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean diff | p | Mean (SD) | Mean diff | p | Mean (SD) | Mean diff | p | ||
| Chronic diseases | Presence | 31.20 (15.26) | 8.464 | 0.002 | 16.22 (8.94) | 5.204 | 0.001 | 32.29 (9.24) | −3.354 | 0.036 |
| Absence | 22.74 (17.38) | 11.02 (9.89) | 35.64 (10.13) | |||||||
| Hypertension | Presence | 30.44 (17.25) | 7.296 | 0.012 | 15.95 (10.28) | 4.725 | 0.004 | 32.21 (10.75) | −3.349 | 0.046 |
| Absence | 23.15 (17.07) | 11.23 (9.66) | 35.56 (9.8) | |||||||
| Diabetes | Presence | 31.78 (15.15) | 8.128 | 0.031 | 14.65 (9.25) | 2.873 | 0.186 | 31.87 (8.91) | −3.427 | 0.119 |
| Absence | 23.65 (17.35) | 11.78 (9.96) | 35.30 (10.1) | |||||||
| Digestive disorders | Presence | 33.68 (15.88) | 13.447 | <0.001 | 17.43 (9.52) | 7.768 | <0.001 | 31.23 (10.33) | −5.468 | <0.001 |
| Absence | 20.23 (16.34) | 9.66 (9.15) | 36.70 (9.46) | |||||||
| Regular mealtimes | Yes | 18.67 (16.64) | −6.805 | 0.024 | 8.51 (8.86) | −4.187 | 0.015 | 39.13 (9.59) | 4.919 | 0.005 |
| No | 25.47 (17.23) | 12.70 (9.98) | 34.21 (9.94) | |||||||
| Sleep quality | <4 h | 30.63 (16.02) | 5.345, 15.801 * | 0.16 | 15.95 (9.5) | 3.668, 8.666 * | 0.076 | 32.37 (10.32) | −1.761, −8.539 * | 0.551 |
| 4–6 h | 25.29 (16.88) | −5.345, 10.456 * | 0.16 | 12.28 (9.76) | −3.668, 4.997 * | 0.076 | 34.13 (9.95) | 1.761, −6.778 * | 0.551 | |
| 6–9 h | 14.83 (16.37) | −15.801 *, −10.456 * | 0.001 | 7.29 (9.16) | −8.666 *, −4.997 * | <0.001 | 40.90 (7.77) | 8.539 *, 6.778 * | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres-Vences, I.N.; Pérez-Campos Mayoral, E.; Mayoral, M.; Pérez-Campos, E.L.; Martínez-Cruz, M.; Torres-Bravo, I.; Alpuche, J. Burnout Syndrome and Related Factors in Mexican Police Workforces. Int. J. Environ. Res. Public Health 2022, 19, 5537. https://doi.org/10.3390/ijerph19095537
Torres-Vences IN, Pérez-Campos Mayoral E, Mayoral M, Pérez-Campos EL, Martínez-Cruz M, Torres-Bravo I, Alpuche J. Burnout Syndrome and Related Factors in Mexican Police Workforces. International Journal of Environmental Research and Public Health. 2022; 19(9):5537. https://doi.org/10.3390/ijerph19095537
Chicago/Turabian StyleTorres-Vences, Irene N., Eduardo Pérez-Campos Mayoral, Miguel Mayoral, Eduardo Lorenzo Pérez-Campos, Margarito Martínez-Cruz, Iban Torres-Bravo, and Juan Alpuche. 2022. "Burnout Syndrome and Related Factors in Mexican Police Workforces" International Journal of Environmental Research and Public Health 19, no. 9: 5537. https://doi.org/10.3390/ijerph19095537
APA StyleTorres-Vences, I. N., Pérez-Campos Mayoral, E., Mayoral, M., Pérez-Campos, E. L., Martínez-Cruz, M., Torres-Bravo, I., & Alpuche, J. (2022). Burnout Syndrome and Related Factors in Mexican Police Workforces. International Journal of Environmental Research and Public Health, 19(9), 5537. https://doi.org/10.3390/ijerph19095537







