Joint Effects of Socioeconomic Position, Race/Ethnicity, and Gender on COVID-19 Mortality among Working-Age Adults in the United States
Abstract
:1. Background
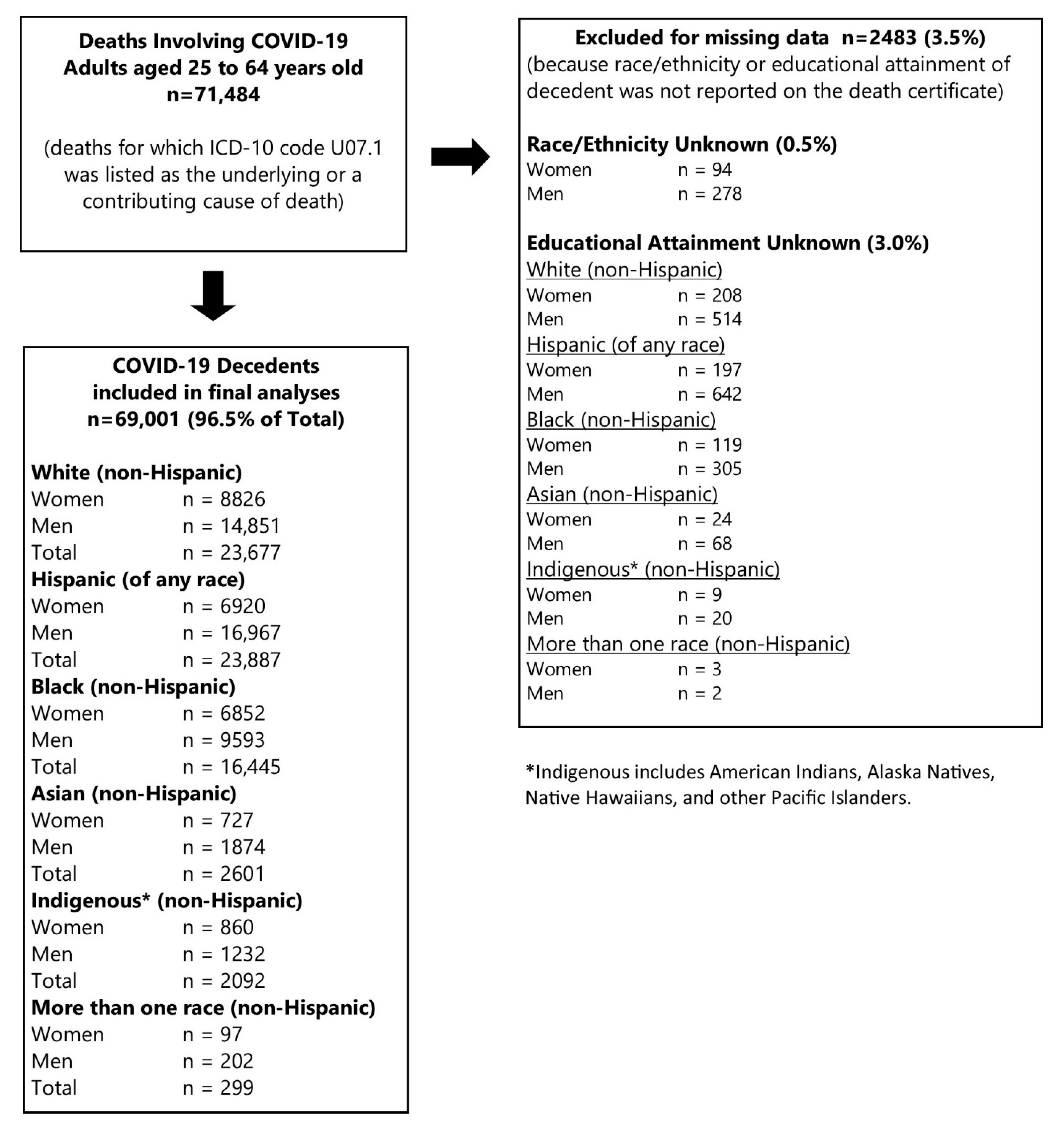
2. Data and Methods
2.1. Population at Risk
2.2. Measurement of Socioeconomic Position
2.3. COVID-19 Deaths
2.4. Population Denominators
2.5. Death Rate Calculations
2.6. Socioeconomic Position and Occupation Distributions
2.7. Analytic Methods
3. Results
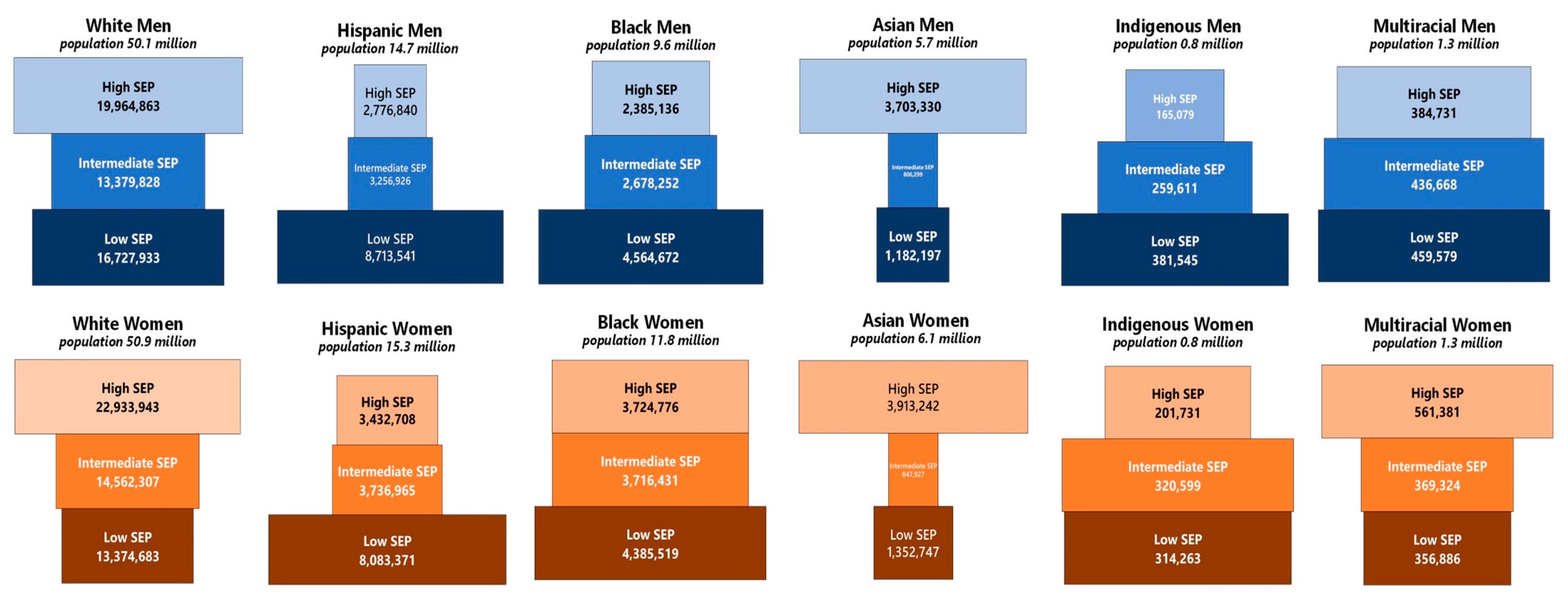
3.1. Socioeconomic Position Distribution of the Population at Risk
3.2. Socioeconomic Position and COVID-19 Mortality: Total Population
3.3. Socioeconomic Position and COVID-19 Mortality by Gender
3.4. Socioeconomic Position and COVID-19 Mortality by Race and Hispanic Ethnicity
3.5. Disparities in COVID-19 Mortality: Independent and Joint Effects of Socioeconomic Position, Gender, and Race/Ethnicity
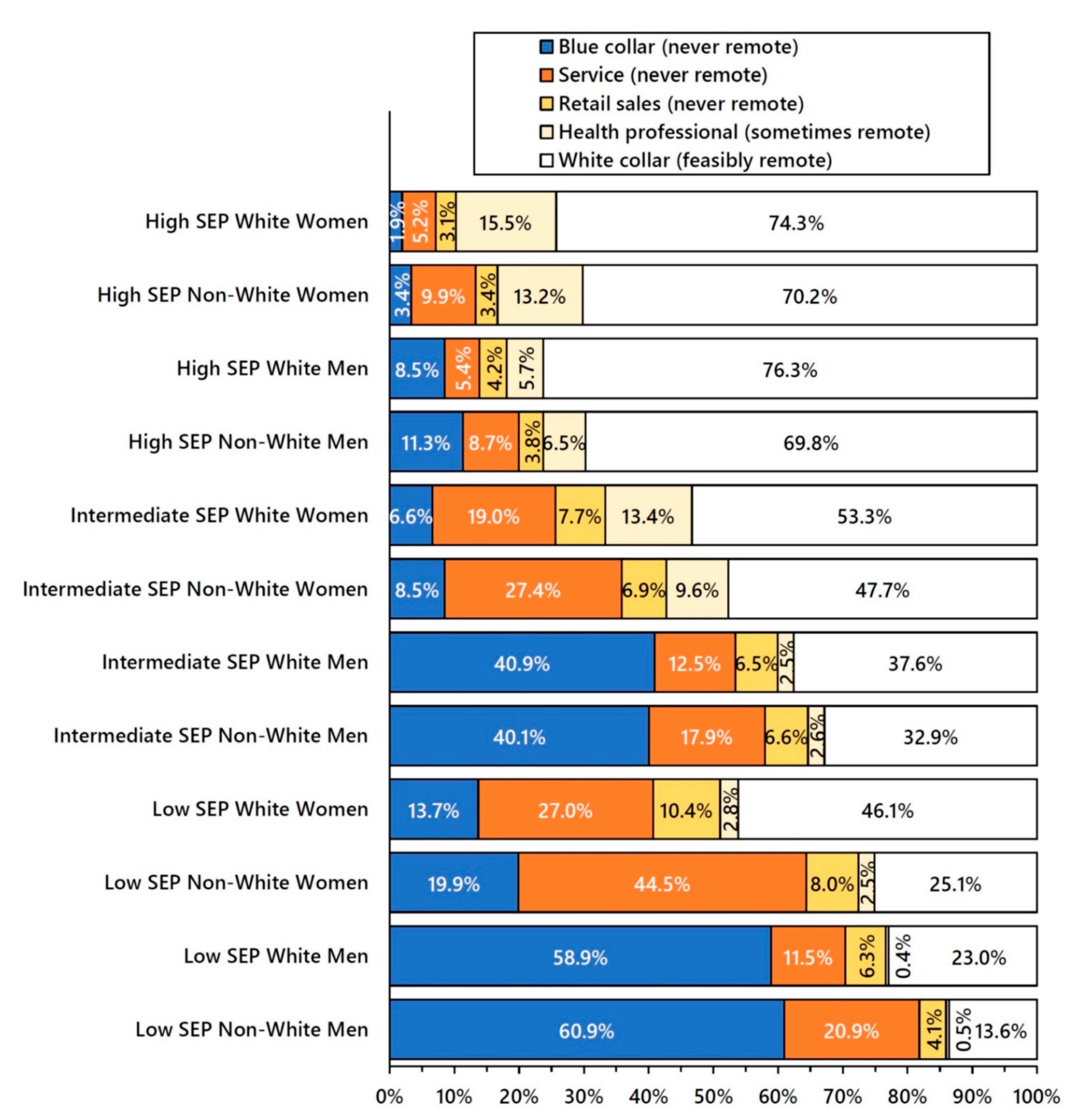
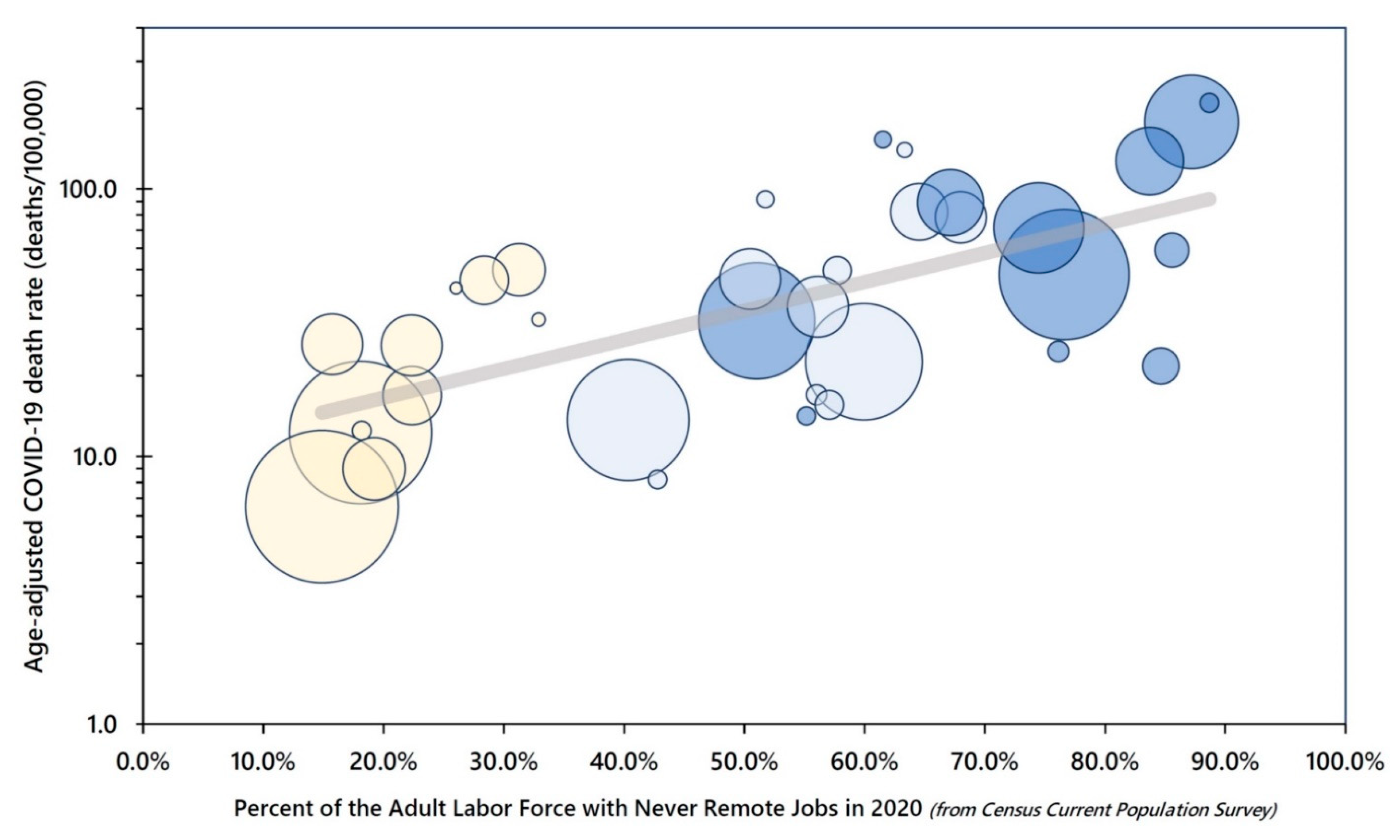
3.6. Working-Class Jobs and Never Remote Work by Socioeconomic Position, Gender, and Race/Ethnicity
4. Discussion
4.1. COVID-19 Case Fatality
4.2. Study Limitations and Public Health Data Gaps
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnson, K.D.; Harris, C.; Cain, J.K.; Hummer, C.; Goyal, H.; Perisetti, A. Pulmonary and Extra-Pulmonary Clinical Manifestations of COVID-19. Front. Med. 2020, 7, 526. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, A.; Pemmasani, G.; Yandrapalli, S.; Frishman, W.H. Cardiovascular and Cerebrovascular Complications with COVID-19. Cardiol. Rev. 2021, 29, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Zheng, K.I.; Feng, G.; Liu, W.Y.; Targher, G.; Byrne, C.D.; Zheng, M.H. Extrapulmonary complications of COVID-19: A multisystem disease? J. Med. Virol. 2021, 93, 323–335. [Google Scholar] [CrossRef] [PubMed]
- White-Dzuro, G.; Gibson, L.E.; Zazzeron, L.; White-Dzuro, C.; Sullivan, Z.; Diiorio, D.A.; Low, S.A.; Chang, M.G.; Bittner, E.A. Multisystem effects of COVID-19: A concise review for practitioners. Postgrad. Med. 2021, 133, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Nassau, D.E.; Best, J.C.; Kresch, E.; Gonzalez, D.C.; Khodamoradi, K.; Ramasamy, R. Impact of the SARS-CoV-2 virus on male reproductive health. BJU Int. 2021, 129, 145–150. [Google Scholar] [CrossRef]
- Sudre, C.H.; Murray, B.; Varsavsky, T.; Graham, M.S.; Penfold, R.S.; Bowyer, R.C.; Pujol, J.C.; Klaser, K.; Antonelli, M.; Canas, L.S.; et al. Attributes and predictors of long COVID. Nat. Med. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Michelen, M.; Manoharan, L.; Elkheir, N.; Cheng, V.; Dagens, A.; Hastie, C.; O’Hara, M.; Suett, J.; Dahmash, D.; Bugaeva, P.; et al. Characterising long COVID: A living systematic review. BMJ Glob. Health 2021, 6, e005427. [Google Scholar] [CrossRef]
- Wang, C.C.; Prather, K.A.; Sznitman, J.; Jimenez, J.L.; Lakdawala, S.S.; Tufekci, Z.; Marr, L.C. Airborne transmission of respiratory viruses. Science 2021, 373, 6558. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Jimenez, J.L.; Prather, K.A.; Tufekci, Z.; Fisman, D.; Schooley, R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet 2021, 397, 1603–1605. [Google Scholar] [CrossRef]
- Tang, J.W.; Marr, L.C.; Milton, D.K. Aerosols should not be defined by distance travelled. J. Hosp. Infect. 2021, 115, 131–132. [Google Scholar] [CrossRef]
- Coleman, K.K.; Tay, D.J.W.; Sen Tan, K.; Ong, S.W.X.; Son, T.T.; Koh, M.H.; Chin, Y.Q.; Nasir, H.; Mak, T.M.; Chu, J.J.H.; et al. Viral Load of SARS-CoV-2 in Respiratory Aerosols Emitted by COVID-19 Patients while Breathing, Talking, and Singing. Clin. Infect. Dis. 2021, ciab691. [Google Scholar] [CrossRef] [PubMed]
- Morawska, L.; Allen, J.; Bahnfleth, W.; Bluyssen, P.M.; Boerstra, A.; Buonanno, G.; Cao, J.; Dancer, S.J.; Floto, A.; Franchimon, F.; et al. A paradigm shift to combat indoor respiratory infection. Science 2021, 372, 689–691. [Google Scholar] [CrossRef] [PubMed]
- Wright, E.O. Class Counts: Comparative Studies in Class Analysis; Cambridge University Press: New York, NY, USA, 1997. [Google Scholar]
- Oliver, M.N.; Muntaner, C. Researching Health Inequities Among African Americans: The Imperative to Understand Social Class. Int. J. Health Serv. 2005, 35, 485–498. [Google Scholar] [CrossRef] [PubMed]
- Krieger, N.; Rowley, D.L.; Herman, A.A.; Avery, B.; Phillips, M.T. Racism, sexism, and social class: Implications for studies of health, disease, and well-being. Am. J. Prev. Med. 1993, 9 (Suppl. 6), 82–122. [Google Scholar] [CrossRef]
- Kokkinen, L.; Muntaner, C.; Koskinen, A.; Väänänen, A. Occupational class, capitalist class advantage and mortality among working-age men. J. Epidemiol. Community Health 2020, 74, 3–6. [Google Scholar] [CrossRef]
- Muntaner, C.; Solar, O.; Vanroelen, C.; Martínez, J.M.; Vergara, M.; Santana, V.; Castedo, A.; Kim, I.-H.; Benach, J. Unemployment, informal work, precarious employment, child labor, slavery, and health inequalities: Pathways and mechanisms. Int. J. Health Serv. 2010, 40, 281–295. [Google Scholar] [CrossRef]
- Graham, H. Unequal Lives: Health and Socioeconomic Inequalities; Open University Press: Berkshire, UK, 2007. [Google Scholar]
- Krieger, N. Workers are people too: Societal aspects of occupational health disparities—An ecosocial perspective. Am. J. Ind. Med. 2010, 53, 104–115. [Google Scholar] [CrossRef]
- Krieger, N.; Fee, E. Measuring Social Inequalities in Health in the United States: A Historical Review, 1900–1950. In Embodying Inequality: Epidemiologic Perspectives; Krieger, N., Ed.; Baywood Publishing Company, Inc.: Amityville, NY, USA, 2005; pp. 5–78. [Google Scholar]
- Pickett, K.E.; Wilkinson, R.G. Income inequality and health: A causal review. Soc. Sci. Med. 2015, 128, 316–326. [Google Scholar] [CrossRef]
- Syme, S.; Berkman, L. Social class, susceptibility and sickness. Am. J. Epidemiol. 1976, 104, 1–8. [Google Scholar] [CrossRef]
- Winkleby, M.A.; Fortmann, S.P.; Barrett, D.C. Social class disparities in risk factors for disease: Eight-year prevalence patterns by level of education. Prev. Med. 1990, 19, 1–12. [Google Scholar] [CrossRef]
- Whiteis, D.G. Third world medicine in first world cities: Capital accumulation, uneven development and public health. Soc. Sci. Med. 1998, 47, 795–808. [Google Scholar] [CrossRef]
- Singh-Manoux, A.; Marmot, M. Role of socialization in explaining social inequalities in health. Soc. Sci. Med. 2005, 60, 2129–2133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, D.R. The health of men: Structured inequalities and opportunities. Am. J. Public Health 2003, 93, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Landsbergis, P.A.; Grzywacz, J.G.; LaMontagne, A.D. Work organization, job insecurity, and occupational health disparities. Am. J. Ind. Med. 2014, 57, 495–515. [Google Scholar] [CrossRef]
- Quinn, M.M.; Sembajwe, G.; Stoddard, A.M.; Kriebel, D.; Krieger, N.; Sorensen, G.; Hartman, C.; Naishadham, D.; ScD, E.M.B. Social disparities in the burden of occupational exposures: Results of a cross-sectional study. Am. J. Ind. Med. 2007, 50, 861–875. [Google Scholar] [CrossRef]
- Williams, D.R. Race, socioeconomic status, and health: The added effects of racism and discrimination. Ann. N. Y. Acad. Sci. 1999, 896, 173–188. [Google Scholar] [CrossRef]
- Whitacre, R.; Oni-Orisan, A.; Gaber, N.; Martinez, C.; Buchbinder, L.; Herd, D.; Holmes, S.M. COVID-19 and the political geography of racialisation: Ethnographic cases in San Francisco, Los Angeles and Detroit. Glob. Public Health 2021, 16, 1396–1410. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Goldblatt, P.; Herd, E.; Morrison, J. Build Back Fairer: The COVID-19 Marmot Review. In The Pandemic, Socioeconomic and Health Inequalities in England; University College London Institute of Health Equity: London, UK, 2020; Available online: https://www.instituteofhealthequity.org/resources-reports/build-back-fairer-the-covid-19-marmot-review.
- National Center for Health Statistics. Ad Hoc Deaths by Educational Attainment, 2019–2020 [Dataset]; National Center for Health Statistics: Hyattsville, MD, USA, 2021. Available online: https://data.cdc.gov/NCHS/AH-Deaths-by-Educational-Attainment-2019-2020/4ueh-89p9.
- National Center for Health Statistics. Technical Notes: Provisional Death Counts for Coronavirus Disease (COVID-19); National Center for Health Statistics: Hyattsville MD, USA, 2020. Available online: https://www.cdc.gov/nchs/nvss/vsrr/covid19/tech_notes.htm.
- LaVeist, T.A. On the study of race, racism, and health: A shift from description to explanation. Int. J. Health Serv. 2000, 30, 217–219. [Google Scholar] [CrossRef]
- Burden-Stelly, C.; Modern, U.S. Racial Capitalism: Some Theoretical Insights. Mon. Rev. 2020, 72, 201–203. [Google Scholar]
- Chowkwanyun, M.; Reed, A.L. Racial Health Disparities and Covid-19—Caution and Context. N. Engl. J. Med. 2020, 383, 201–203. [Google Scholar] [CrossRef]
- Smedley, A.; Smedley, B.D. Race as biology is fiction, racism as a social problem is real: Anthropological and historical perspectives on the social construction of race. Am. Psychol. 2005, 60, 16–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, D.R.; Lavizzo-Mourey, R.; Warren, R.C. The concept of race and health status in America. Public Health Rep. 1994, 109, 26–41. [Google Scholar] [PubMed]
- Krieger, N.; Williams, D.R.; Moss, N.E. Measuring Social Class in US Public Health Research: Concepts, Methodologies, and Guidelines. Annu. Rev. Public Health 1997, 18, 341–378. [Google Scholar] [CrossRef] [Green Version]
- Tolson, G.; Barnes, J.; Gay, G.; Kowaleski, K.L. The 1989 Revision of the U.S. Standard Certificates and Reports; National Center for Health Statistics: Hyattsville MD, USA, 1991; Volume 28, pp. 1–34. Available online: https://www.cdc.gov/nchs/data/series/sr_04/sr04_028.pdf.
- Sarah, F.; Miriam, K.; Renae, R.; Steven Ruggles, J.; Robert, W.; Westberry, M. Integrated Public Use Microdata Series, Current Population Survey: Version 9.0 [Dataset]; IPUMS: Minneapolis, MN, USA, 2021. [Google Scholar] [CrossRef]
- Bureau of the Census. 2020 Annual Social and Economic (ASEC) Supplement Technical Documentation; 2021. Available online: https://www2.census.gov/programs-surveys/cps/techdocs/cpsmar20.pdf.
- Rothbaum, J.; Bee, A. Coronavirus Infects Surveys, Too: Survey Nonresponse Bias and the Coronavirus Pandemic; United States Census Bureau: Washington, DC, USA, 2021. Available online: https://www.census.gov/library/working-papers/2020/demo/SEHSD-WP2020-10.html.
- Kaikkonen, R.; Rahkonen, O.; Lallukka, T.; Lahelma, E. Physical and psychosocial working conditions as explanations for occupational class inequalities in self-rated health. Eur. J. Public Health 2009, 19, 458–463. [Google Scholar] [CrossRef]
- Krieger, N.; Waterman, P.D.; Hartman, C.; Bates, L.M.; Stoddard, A.M.; Quinn, M.M.; Sorensen, G.; Barbeau, E.M. Social hazards on the job: Workplace abuse, sexual harassment, and racial discrimination--a study of Black, Latino, and White low-income women and men workers in the United States. Int. J. Health Serv. 2006, 36, 51–85. [Google Scholar] [CrossRef] [PubMed]
- Muntaner, C. Digital Platforms, Gig Economy, Precarious Employment, and the Invisible Hand of Social Class. Int. J. Health Serv. 2018, 48, 597–600. [Google Scholar] [CrossRef] [PubMed]
- Fielding-Miller, R.K.; Sundaram, M.E.; Brouwer, K. Social determinants of COVID-19 mortality at the county level. PLoS ONE 2020, 15, e0240151. [Google Scholar] [CrossRef]
- AFL-CIO. Death on the Job: The Toll of Neglect: A National and State-by-State Profile of Worker Safety and Health in the United States; AFL-CIO: Washington, DC, USA, 2021; Available online: https://aflcio.org/reports/death-job-toll-neglect-2020.
- Michaels, D.; Wagner, G.R. Halting Workplace COVID-19 Transmission: An Urgent Proposal to Protect American Workers; The Century Foundation: New York, NY, USA, 2020; Available online: https://tcf.org/content/report/halting-workplace-covid-19-transmission-urgent-proposal-protect-american-workers/.
- Marable, M. How Capitalism Underdeveloped Black America; South End Press: Boston, MA, USA, 1983. [Google Scholar]
- Laster Pirtle, W.N. Racial Capitalism: A Fundamental Cause of Novel Coronavirus (COVID-19) Pandemic Inequities in the United States. Health Educ. Behav. 2020, 47, 504–508. [Google Scholar] [CrossRef]
- McClure, E.S.; Vasudevan, P.; Bailey, Z.; Patel, S.; Robinson, W.R. Racial Capitalism Within Public Health-How Occupational Settings Drive COVID-19 Disparities. Am. J. Epidemiol. 2020, 189, 1244–1253. [Google Scholar] [CrossRef]
- Williams, D.R.; Mohammed, S.A.; Leavell, J.; Collins, C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Ann. N. Y. Acad. Sci. 2010, 1186, 69–101. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Glymour, M.; Riley, A.; Balmes, A.; Duchowny, K.; Harrison, R.; Matthay, E.; Bibbins-Domingo, K. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through October 2020. PLoS ONE 2021, 16, e0252454. [Google Scholar] [CrossRef] [PubMed]
- Lan, F.Y.; Wei, C.F.; Hsu, Y.T.; Christiani, D.C.; Kales, S.N. Work-related COVID-19 transmission in six Asian countries/areas: A follow-up study. PLoS ONE 2020, 15, e0233588. [Google Scholar] [CrossRef] [PubMed]
- Fiscella, K.; Sanders, M.R. Racial and Ethnic Disparities in the Quality of Health Care. Annu. Rev. Public Health 2016, 37, 375–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mays, V.M.; Cochran, S.D.; Sprague, A.; Heymann, J. Social Justice Is Not the COVID-19 Vaccine Alone: It Is Addressing Structural Racism Through Social Policies That Shape Health. Am. J. Public Health 2021, 111, S75–S79. [Google Scholar] [CrossRef]
- Gehlbach, D.; Vázquez, E.; Ortiz, G.; Li, E.; Sánchez, C.B.; Rodríguez, S.; Pozar, M.; Cheney, A.M. COVID-19 Testing and Vaccine Hesitancy in Latinx Farm-Working Communities in The Eastern Coachella Valley. Res. Sq. 2021, 1–17. [Google Scholar] [CrossRef]
- Pathak, E.B.; Garcia, R.B.; Menard, J.M.; Salemi, J.L. Out-of-Hospital COVID-19 Deaths: Consequences for Quality of Medical Care and Accuracy of Cause of Death Coding. Am. J. Public Health 2021, 111, S101–S106. [Google Scholar] [CrossRef]
- McNicholas, C.; Rhinehart, L.; Poydock, M.; Shierholz, H.; Perez, D. Why Unions are Good for Workers—Especially in a Crisis Like COVID-19; Economic Policy Institute: Washington, DC, USA, 2020; Available online: https://files.epi.org/pdf/204014.pdf.
- Dennerlein, J.T.; Burke, L.; Sabbath, E.L.; Williams, J.A.R.; Peters, S.; Wallace, L.; Karapanos, M.; Sorensen, G. An Integrative Total Worker Health Framework for Keeping Workers Safe and Healthy during the COVID-19 Pandemic. Hum. Factors 2020, 62, 689–696. [Google Scholar] [CrossRef]

| Demographic Groups | Low SEP | Intermediate SEP | High SEP |
|---|---|---|---|
| Population at risk | 59.9 million | 44.4 million | 64.1 million |
| Total Study Population | |||
| COVID-19 deaths | 46,966 | 13,614 | 8421 |
| Age-adjusted mortality rate | 72.2/100,000 | 30.4/100,000 | 14.6/100,000 |
| SEP rate ratio (95% CI) | 4.94 (4.82–5.05) | 2.08 (2.02–2.14) | 1.0 (referent) |
| By Reported Gender | |||
| Women | |||
| COVID-19 deaths | 15,708 | 5535 | 3039 |
| Age-adjusted mortality rate | 50.4/100,000 | 22.8/100,000 | 10.0/100,000 |
| SEP rate ratio (95% CI) | 5.06 (4.87–5.26) | 2.29 (2.19–2.39) | 1.0 (referent) |
| Men | |||
| COVID-19 deaths | 31,258 | 8079 | 5382 |
| Age-adjusted mortality rate | 92.1/100,000 | 39.5/100,000 | 19.8/100,000 |
| SEP rate ratio (95% CI) | 4.65 (4.52–4.79) | 1.99 (1.93–2.06) | 1.0 (referent) |
| By Reported Race/Ethnicity | |||
| White, non-Hispanic | |||
| COVID-19 deaths | 14,587 | 5344 | 3746 |
| Age-adjusted mortality rate | 40.6/100,000 | 17.8/100,000 | 9.3/100,000 |
| SEP rate ratio (95% CI) | 4.37 (4.21–4.53) | 1.92 (1.84–2.00) | 1.0 (referent) |
| Hispanic | |||
| COVID-19 deaths | 19,174 | 3173 | 1540 |
| Age-adjusted mortality rate | 125.0/100,000 | 57.0/100,000 | 32.9/100,000 |
| SEP rate ratio (95% CI) | 3.80 (3.61–4.00) | 1.73 (1.63–1.84) | 1.0 (referent) |
| Black, non-Hispanic | |||
| COVID-19 deaths | 10,544 | 3912 | 1989 |
| Age-adjusted mortality rate | 105.9/100,000 | 59.0/100,000 | 33.8/100,000 |
| SEP rate ratio (95% CI) | 3.14 (2.99–3.29) | 1.75 (1.66–1.84) | 1.0 (referent) |
| Asian, non-Hispanic | |||
| COVID-19 deaths | 1149 | 497 | 955 |
| Age-adjusted mortality rate | 38.5/100,000 | 32.1/100,000 | 17.7/100,000 |
| SEP rate ratio (95% CI) | 2.18 (2.00–2.38) | 1.82 (1.63–2.03) | 1.0 (referent) |
| Indigenous, non-Hispanic | |||
| COVID-19 deaths | 1353 | 602 | 137 |
| Age-adjusted mortality rate | 182.1/100,000 | 113.4/100,000 | 37.2/100,000 |
| SEP rate ratio (95% CI) | 4.90 (4.11–5.84) | 3.05 (2.53–3.67) | 1.0 (referent) |
| Multirace/Other, non-Hispanic | |||
| COVID-19 deaths | 159 | 86 | 54 |
| Age-adjusted mortality rate | 20.0/100,000 | 12.9/100,000 | 8.7/100,000 |
| SEP rate ratio (95% CI) | 2.32 (1.70–3.15) | 1.49 (1.06–2.10) | 1.0 (referent) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pathak, E.B.; Menard, J.M.; Garcia, R.B.; Salemi, J.L. Joint Effects of Socioeconomic Position, Race/Ethnicity, and Gender on COVID-19 Mortality among Working-Age Adults in the United States. Int. J. Environ. Res. Public Health 2022, 19, 5479. https://doi.org/10.3390/ijerph19095479
Pathak EB, Menard JM, Garcia RB, Salemi JL. Joint Effects of Socioeconomic Position, Race/Ethnicity, and Gender on COVID-19 Mortality among Working-Age Adults in the United States. International Journal of Environmental Research and Public Health. 2022; 19(9):5479. https://doi.org/10.3390/ijerph19095479
Chicago/Turabian StylePathak, Elizabeth B., Janelle M. Menard, Rebecca B. Garcia, and Jason L. Salemi. 2022. "Joint Effects of Socioeconomic Position, Race/Ethnicity, and Gender on COVID-19 Mortality among Working-Age Adults in the United States" International Journal of Environmental Research and Public Health 19, no. 9: 5479. https://doi.org/10.3390/ijerph19095479
APA StylePathak, E. B., Menard, J. M., Garcia, R. B., & Salemi, J. L. (2022). Joint Effects of Socioeconomic Position, Race/Ethnicity, and Gender on COVID-19 Mortality among Working-Age Adults in the United States. International Journal of Environmental Research and Public Health, 19(9), 5479. https://doi.org/10.3390/ijerph19095479







