General Health and Resilience of Breast Cancer Patients: The Mediator Role of Affective Well-Being
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Procedure
2.2. Participants
2.3. Instruments
2.4. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Ferlay, J.; Laversanne, M.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Tomorrow. International Agency for Research on Cancer, 2020. Available online: https://gco.iarc.fr/tomorrow (accessed on 1 February 2022).
- World Health Organization (WHO). Cancer. 2021. Available online: www.who.int/news-room/fact-sheets/detail/cancer (accessed on 1 February 2022).
- Spanish Society of Medical Oncology. Las Cifras del Cáncer en España 2021 [Cancer Data in Spain 2021]; Sociedad Española de Oncología Médica: Madrid, Spain, 2021; Available online: https://seom.org/prensa/el-cancer-en-cifras (accessed on 1 February 2022).
- Espinosa, M. Cáncer de Mama [Breast Cancer]. Rev. Méd. Sinerg. 2018, 2, 8–12. Available online: https://www.medigraphic.com/pdfs/sinergia/rms-2017/rms171b.pdf (accessed on 1 February 2022).
- Escudero-Castelán, A.; Valencia Ortiz, A.; Ruvalcaba Ledezma, J.; Ortega Andrade, N.; Bautista Díaz, M. Efectividad de Intervenciones Basadas en Mindfulness en Mujeres con Cáncer de Mama [Effectiveness of Mindfulness-Based Interventions in Women with Breast Cancer]. MediSur 2021, 19, 924–936. Available online: http://www.medisur.sld.cu/index.php/medisur/article/view/4997 (accessed on 1 February 2022).
- Enríquez Reyna, M.C.; Vargas Flores, M.D.L.A. Factores personales que afectan la calidad de vida de mujeres con cáncer de mama del noreste de México. [Personal factors that affect quality of life of women with breast cancer from the northeast of Mexico]. Hisp. Health Care Int. 2018, 16, 70–75. [Google Scholar] [CrossRef]
- Ho, P.J.; Gernaat, S.A.M.; Hartman, M.; Verkooijen, H.M. Health-related quality of life in Asian patients with breast cancer: A systematic review. BMJ Open 2018, 8, e020512. [Google Scholar] [CrossRef] [PubMed]
- Mejía-Rojas, M.; Contreras-Rengifo, A.; Hernández-Carrillo, M. Calidad de vida en mujeres con cáncer de mama sometidas a quimioterapia en Cali, Colombia. [Quality of life in women with breast cancer undergoing chemotherapy in Cali, Colombia]. Biomédica 2020, 40, 349–361. [Google Scholar] [CrossRef]
- Pastuñas Doicela, R.; Sanhueza Alvarado, O. Influencia de la autoeficacia en la incertidumbre y la calidad de vida de mujeres con cáncer de mama. Revisión integrativa [Influence of self-efficacy on uncertainty and quality of life of women with breast cancer. Integrative review]. Enfermería Cuid. Humaniz. 2021, 10, 124–144. [Google Scholar] [CrossRef]
- Valderrama, M.C.; Sánchez, R. Anxiety and depression disorders in relation to the quality of life of breast cancer patients with locally advanced or disseminated stage. Rev. Colomb. Psiquiatr. Engl. 2018, 47, 211–220. [Google Scholar] [CrossRef]
- Zelaya-Rivas, S. Intervenciones psicológicas en el tratamiento de la ansiedad en personas con cáncer de mama: Un metaanálisis [Psychological interventions in anxiety treatment in people with breast cancer: A meta-analysis]. Act. Psi. 2020, 34, 121–141. [Google Scholar] [CrossRef]
- Cerezo, M.V.; Blanca, M.J.; Ferragut, R. Personality profiles and psychological adjustment in breast cancer patients. Int. J. Environ. Res. Public Health 2020, 17, 9452. [Google Scholar] [CrossRef]
- Hashemi, S.-M.; Rafiemanesh, H.; Aghamohammadi, T.; Badakhsh, M.; Amirshahi, M.; Sari, M.; Behnamfar, N.; Roudini, K. Prevalence of anxiety among breast cancer patients: A systematic review and meta-analysis. Breast Cancer 2020, 27, 166–178. [Google Scholar] [CrossRef]
- De la Torre-Luque, A.; Cerezo, M.V.; López, E.; Sibole, J.V. Emotional distress among long-term breast cancer survivors: The role of insomnia and worry. Behav. Psychol. 2020, 28, 533–549. Available online: https://www.behavioralpsycho.com/wp-content/uploads/2020/12/09.De_la_Torre_28-3.pdf (accessed on 1 February 2022).
- Cerezo, M.V.; Rueda, P. Resiliencia y cáncer: Una relación necesaria [Resilience and cancer: A necessary relationship]. Psychol. Writ. 2020, 13, 90–97. [Google Scholar] [CrossRef]
- Dooley, L.N.; Slavich, G.M.; Moreno, P.I.; Bower, J.E. Strength through adversity: Moderate lifetime stress exposure is associated with psychological resilience in breast cancer survivors. Stress Health 2017, 33, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Zayas, A.; Gómez-Molinero, R.; Guil, R.; Gil-Olarte, P.; Jiménez Orozco, E. Relación entre la resiliencia y la satisfacción con la vida en una muestra de mujeres con cáncer de mama [Relationship between resilience and life satisfaction in a sample of women with breast cancer]. Rev. INFAD De Psicología. Int. J. Dev. Educ. Psychol. 2018, 3, 127–136. [Google Scholar] [CrossRef] [Green Version]
- Kugbey, N.; Asante, K.O.; Meyer-Weitz, A. Depression, anxiety and quality of life among women living with breast cancer in Ghana: Mediating roles of social support and religiosity. Support Care Cancer 2020, 28, 2581–2588. [Google Scholar] [CrossRef]
- Srivastava, J.; Kaushik, S.S.; Tewari, M.; Shukla, H.S. Mediating role of affective experiences in the relationship between perceived social support and life satisfaction among breast cancer patients. Indian J. Palliat Care 2021, 27, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Guil, R.; Ruiz-González, P.; Merchán-Clavellino, A.; Morales-Sánchez, L.; Zayas, A.; Gómez-Molinero, R. Breast cancer and resilience: The controversial role of perceived emotional intelligence. Front. Psychol. 2020, 11. Available online: https://www.frontiersin.org/article/10.3389/fpsyg.2020.595713 (accessed on 1 January 2022). [CrossRef]
- Zhou, K.; Ning, F.; Wang, W.; Li, X. The mediator role of resilience between psychological predictors and health-related quality of life in breast cancer survivors: A cross-sectional study. BMC Cancer 2022, 22, 57. [Google Scholar] [CrossRef]
- Cerezo, M.V.; Soria-Reyes, L.M.; Alarcón, R.; Blanca, M.J. The Satisfaction with Life Scale in breast cancer patients: Psychometric properties. Int. J. Clin. Health Psychol. 2022, 22, 2022. [Google Scholar] [CrossRef]
- Guil, R.; Zayas, A.; Gil-Olarte, P.; Guerrero, C.; González, S.; Mestre, J.M. Bienestar psicológico, optimismo y resiliencia en mujeres con cáncer de mama [Psychological well-being, optimism and resilience in women with breast cancer]. Psicooncología 2016, 13, 127–138. [Google Scholar] [CrossRef]
- Lorenzo-Seva, U.; Calderon, C.; Ferrando, P.J.; Del Mar Muñoz, M.; Beato, C.; Ghanem, I.; Castelo, B.; Carmona-Bayonas, A.; Hernandez, R.; Jimenez-Fonseca, P. Psychometric properties and factorial analysis of invariance of the Satisfaction with Life Scale (SWLS) in cancer patients. Qual. Life Res. 2019, 28, 1255–1264. [Google Scholar] [CrossRef] [Green Version]
- Badana, A.N.S.; Marino, V.R.; Templeman, M.E.; McMillan, S.C.; Tofthagen, C.S.; Small, B.J.; Haley, W.E. Understanding the roles of patient symptoms and subjective appraisals in well-being among breast cancer patients. Support. Care Cancer 2019, 27, 4245–4425. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Diener, E. Subjective Well-Being. In The Science of Well-Being; Diener, E., Ed.; Social Indicators Research Series; Springer: Berlin/Heidelberg, Germany, 2009; Volume 37. [Google Scholar] [CrossRef]
- George, J.M. Trait or estate affect. In Individual Differences and Behavior in Organizations; Murphy, K.R., Ed.; Jossey-Bass: San Francisco, CA, USA, 1996; pp. 145–147. [Google Scholar]
- Watson, D.; Tellegen, A. Toward a consensual structure of mood. Psychol. Bull. 1985, 54, 219–235. [Google Scholar] [CrossRef]
- Cipora, E.; Konieczny, M.; Karwat, I.D.; Roczniak, W.; Babuska-Roczniak, M. Surgical method of treatment and level of satisfaction with life among women diagnosed with breast cancer, according to time elapsed since performance of surgery. Ann. Agric. Sci. 2018, 25, 453–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alarcón, R.; Cerezo, M.V.; Hevilla, S.; Blanca, M.J. Psychometric properties of the Connor-Davidson Resilience Scale in women with breast cancer. Int. J. Clin. Health Psychol. 2020, 20, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, D.P.; Hillier, V.F. A scaled version of the General Health Questionnaire. Psychol. Med. 1979, 9, 139–145. [Google Scholar] [CrossRef]
- Tu, P.C.; Yeh, D.C.; Hsieh, H.C. Positive psychological changes after breast cancer diagnosis and treatment: The role of trait resilience and coping styles. J. Psychosoc. Oncol. 2020, 38, 156–170. [Google Scholar] [CrossRef]
- Garmezy, N. Resilience in children’s adaptation to negative life events and stressed environments. Pediatr. Ann. 1991, 20, 459–466. [Google Scholar] [CrossRef]
- Garmezy, N.; Masten, A.; Tellegen, A. The study of stress and competence in children: A building block for developmental psychopathology. Child Dev. 1984, 55, 97–111. [Google Scholar] [CrossRef]
- Padilla-Ruiz, M.; Ruiz-Román, C.; Pérez-Ruiz, E.; Rueda, A.; Redondo, M.; Rivas-Ruiz, F. Clinical and sociodemographic factors that may influence the resilience of women surviving breast cancer: Cross-sectional study. Support Care Cancer 2019, 27, 1279–1286. [Google Scholar] [CrossRef]
- Ruiz-González, P.; Zayas, A.; Morales-Sánchez, L.; Gil-Olarte, P.; Guil, R. Resiliencia como predictora de depresión en mujeres con cáncer de mama [Resilence as a predictor of depression in women with breast cancer]. Int. J. Dev. Educ. Psychol. 2019, 4, 1. Available online: https://www.redalyc.org/articulo.oa?id=349861666008 (accessed on 10 February 2022).
- Gallagher, M.W.; Long, L.J.; Richardson, A.; D’Souza, J.M. Resilience and coping in cancer survivors: The unique effects of optimism and mastery. Cognit. Ther. Res. 2019, 43, 32–44. [Google Scholar] [CrossRef]
- Lobo, A.; Pérez-Echeverría, M.J.; Artal, J. Validity of the scaled version of the General Health Questionnaire (GHQ-28) in a Spanish population. Psychol. Med. 1986, 16, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Nourbala, A.A.; Bagheri, Y.S.; Mohammad, K. The validation of general health questionnaire-28 as a psychiatric screening tool. Hakim Res. J. 2009, 11, 47–53. Available online: https://www.sid.ir/en/Journal/ViewPaper.aspx?ID=140345 (accessed on 10 February 2022).
- Mroczek, D.K.; Kolarz, C.M. The effect of age on positive and negative affect: A developmental perspective on happiness. J. Pers. Soc. Psychol. 1998, 75, 1333–1349. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Sills, L.; Stein, M.B. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. J. Trauma. Stress. 2007, 20, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Burga, I.; Sánchez, T.; Jaimes, J.E. Inteligencia emocional y resiliencia en pacientes con cáncer de mama en un hospital de Salud de Lima [Emotional intelligence and resilience in patients with breast cáncer in a Health hospital of Lima]. Rev. Investig. Apunt. Psicol. 2016, 1, 9–16. Available online: https://revistas.upeu.edu.pe/index.php/ri_apsicologia/article/view/864 (accessed on 10 February 2022).
- Aizpurua-Perez, I.; Perez-Tejada, J. Resilience in women with breast cancer: A systematic review. Eur. J. Oncol. Nurs. 2020, 49, 101854. [Google Scholar] [CrossRef] [PubMed]
- Cerezo, M.V.; Ortiz-Tallo, M.; Cardenal, V.; de la Torre-Luque, A. Positive psychology group intervention for breast cancer patients: A randomised trial. Psychol. Rep. 2014, 115, 44–64. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.H.; Chen, S.W.; Huang, W.T.; Chang, S.C.; Hsu, M.C. Effects of a psychoeducational intervention in patients with breast cancer undergoing chemotherapy. J. Nurs. Res. 2018, 26, 266–279. [Google Scholar] [CrossRef] [PubMed]
| Variables | N | % |
|---|---|---|
| Age | ||
| <50 years | 43 | 39.4 |
| >50 years | 66 | 60.6 |
| Marital status | ||
| Single | 25 | 23.0 |
| Married | 70 | 64.2 |
| Divorced | 12 | 11.0 |
| Widowed | 2 | 1.8 |
| Educational level | ||
| Primary | 12 | 11.0 |
| Secondary | 13 | 11.9 |
| Other non-university | 31 | 28.5 |
| University | 53 | 48.6 |
| Occupation | ||
| Home-keeper | 16 | 14.7 |
| Employed | 78 | 71.6 |
| Unemployed | 7 | 6.4 |
| Retired | 8 | 7.3 |
| Number of children | ||
| 0 | 27 | 24.8 |
| 1 | 24 | 22.0 |
| 2 | 52 | 47.7 |
| >2 | 6 | 5.5 |
| Breast cancer stage | ||
| 0 | 3 | 2.8 |
| I | 19 | 17.4 |
| II | 52 | 47.7 |
| III | 33 | 30.8 |
| IV | 2 | 1.8 |
| Axillary dissection | ||
| No | 39 | 35.8 |
| Yes | 70 | 64.2 |
| Time since diagnosis (years) | ||
| <2 | 31 | 28.5 |
| 2–5 | 36 | 33.0 |
| >5 | 38.5 | 38.5 |
| Variables | General Health (Total Score) | 1 (SS) | 2 (A&I) | 3 (SDY) | 4 (MA) | 5 (PA) | 6 (NA) | 7 (SWL) |
|---|---|---|---|---|---|---|---|---|
| 1 Somatic symptoms (SS) | 0.76 * | |||||||
| 2 Anxiety and insomnia (A&I) | 0.88 * | 0.56 * | ||||||
| 3 Social dysfunction (SDY) | 0.77 * | 0.47 * | 0.61 * | |||||
| 4 Major depression (MA) | 0.75 * | 0.35 * | 0.55 * | 0.47 * | ||||
| 5 Positive affect (PA) | −0.55 * | −0.30 * | −0.46 * | −0.43 * | −0.56 * | |||
| 6 Negative affect (NA) | 0.65 * | 0.36 * | 0.59 * | 0.54 * | 0.56 * | −0.35 * | ||
| 7 Satisfaction with life (SWL) | −0.28 * | −0.15 | −0.23 ** | −0.20 ** | −0.38* | 0.40 * | −0.20 ** | |
| 8 Resilience | −0.37 * | −0.19 ** | −0.33 * | −0.35 * | −0.40 * | 0.54 * | −0.52 * | 0.12 |
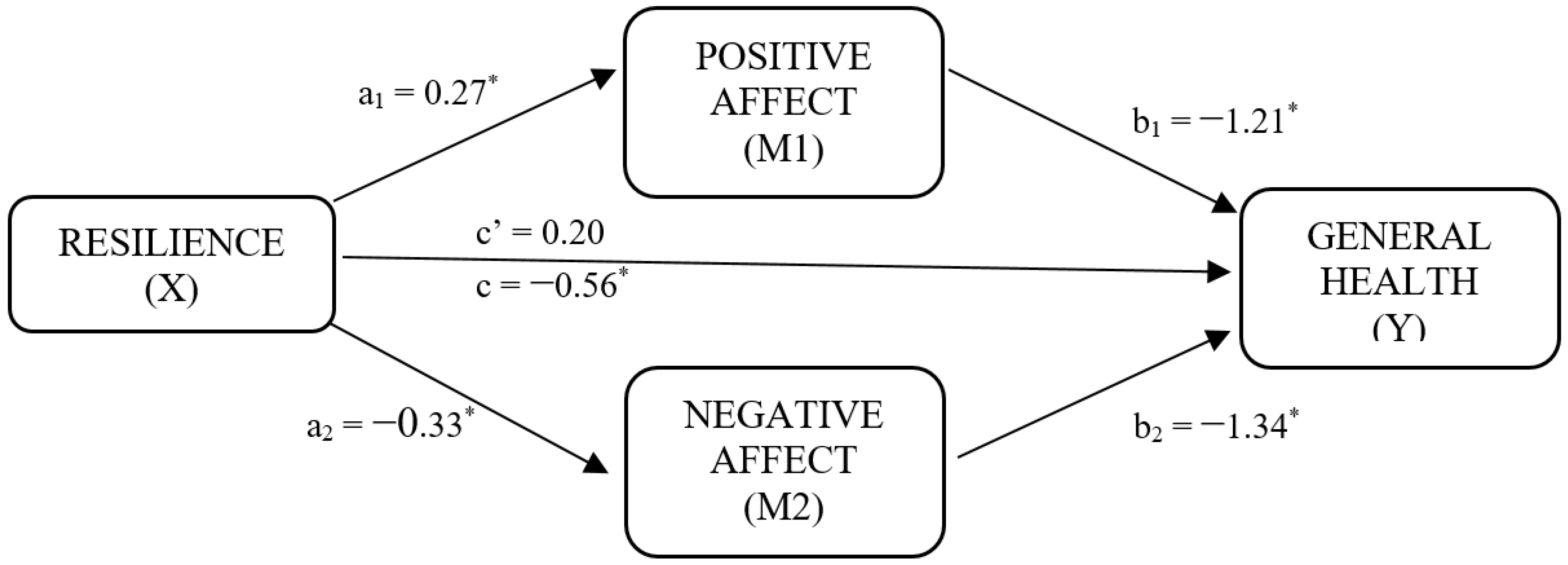
| Model Summary | R2 | MSE | F | df1 | df2 | p | |
| Total effect model | 0.17 | 187.28 | 10.60 | 2 | 106 | <0.001 | |
| Positive affect on resilience | 0.29 | 18.97 | 22.41 | 2 | 106 | <0.001 | |
| Negative affect on resilience | 0.30 | 2929 | 23.11 | 2 | 106 | <0.001 | |
| General health on resilience | 0.55 | 102.16 | 32.30 | 4 | 104 | <0.001 | |
| Direct effects | Path | Coef. | SE | T | 95% CI | ||
| p | BootLL | BootUL | |||||
| Positive affect on resilience | a1 | 0.27 | 0.04 | 6.59 | <0.001 | 0.19 | 0.34 |
| Negative affect on resilience | a2 | −0.33 | 0.05 | −6.51 | <0.001 | −0.43 | −0.23 |
| Positive affect on general health | b1 | −1.21 | 0.22 | −5.39 | <0.001 | −1.65 | −0.76 |
| Negative affect on general health | b2 | −1.32 | 0.17 | 7.42 | <0.001 | 0.97 | 1.68 |
| Resilience on general health | c’ | 0.20 | 0.12 | 1.60 | 0.11 | −0.05 | 0.44 |
| Total effect of resilience on general health | c | −0.56 | 0.13 | −4.45 | <0.001 | −0.81 | −0.31 |
| Indirect effects | Path | Effect | BootSE | BootLL | BootUL | ||
| Total | −0.75 | 0.13 | −1.02 | −0.52 | |||
| Resilience -> Positive affect -> General Health | a1b1 | −0.32 | 0.07 | −0.48 | −0.19 | ||
| Resilience -> Negative affect -> General health | a2b2 | −0.44 | 0.10 | −0.64 | −0.27 | ||
| C1 | 0.12 | 0.11 | −0.10 | 0.34 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerezo, M.V.; Álvarez-Olmo, A.; Rueda, P. General Health and Resilience of Breast Cancer Patients: The Mediator Role of Affective Well-Being. Int. J. Environ. Res. Public Health 2022, 19, 5398. https://doi.org/10.3390/ijerph19095398
Cerezo MV, Álvarez-Olmo A, Rueda P. General Health and Resilience of Breast Cancer Patients: The Mediator Role of Affective Well-Being. International Journal of Environmental Research and Public Health. 2022; 19(9):5398. https://doi.org/10.3390/ijerph19095398
Chicago/Turabian StyleCerezo, M. Victoria, Ana Álvarez-Olmo, and Pilar Rueda. 2022. "General Health and Resilience of Breast Cancer Patients: The Mediator Role of Affective Well-Being" International Journal of Environmental Research and Public Health 19, no. 9: 5398. https://doi.org/10.3390/ijerph19095398
APA StyleCerezo, M. V., Álvarez-Olmo, A., & Rueda, P. (2022). General Health and Resilience of Breast Cancer Patients: The Mediator Role of Affective Well-Being. International Journal of Environmental Research and Public Health, 19(9), 5398. https://doi.org/10.3390/ijerph19095398







