Quantitative Methods to Detect Suicide and Self-Harm Clusters: A Systematic Review
Abstract
1. Introduction
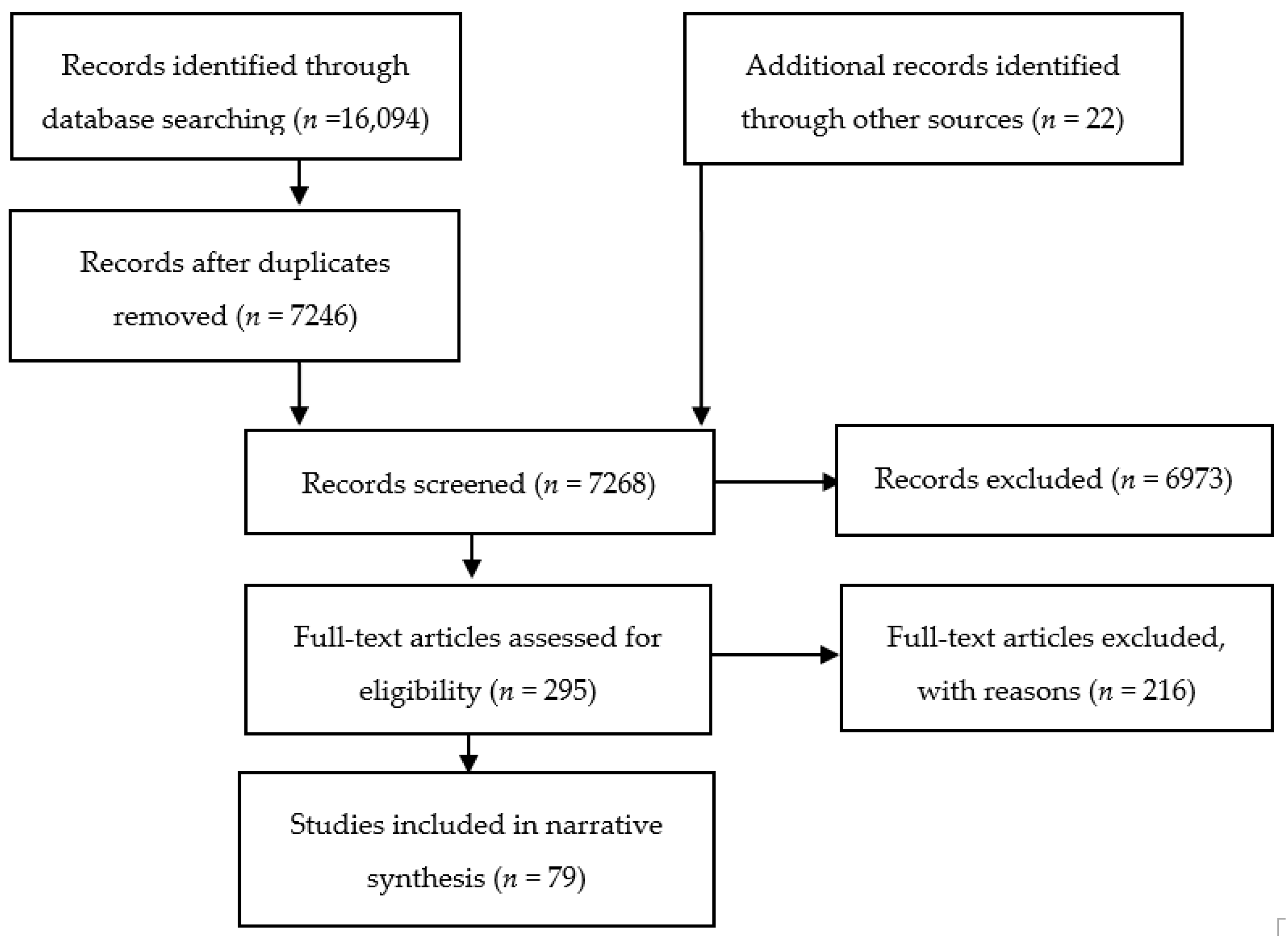
2. Materials and Methods
3. Results
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Suicide Prevention and Considerations for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Carroll, P.W.; Mercy, J.A.; Steward, J.A. CDC recommendations for a community plan for the prevention and containment of suicide clusters. MMWR Supp. 1988, 37, 1–12. [Google Scholar]
- Niedzwiedz, C.; Haw, C.; Hawton, K.; Platt, S. The definition and epidemiology of clusters of suicidal behavior: A systematic review. Suicide Life Threat Behav. 2014, 44, 569–581. [Google Scholar] [CrossRef] [PubMed]
- Bohanna, I. Suicide “contagion”: What we know and what we need to find out. Can. Med. Assoc. J. 2013, 185, 861–862. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hazell, P. Adolescent suicide clusters: Evidence, mechanisms, and prevention. Aust. N. Z. J. Psychiatry 1993, 27, 653–665. [Google Scholar] [CrossRef]
- Gould, M.S.; Wallenstein, S.; Kleinman, M. Time-space clustering of teenage suicide. Am. J. Epidemiol. 1990, 131, 71–78. [Google Scholar] [CrossRef]
- Gould, M.; Wallenstein, S.; Kleinman, N. A Study of Time-Space Clustering of Suicide: Final Report; Centers for Disease Control and Prevention (CDC): Atlanta, GA, USA, 1987.
- Gould, M.S.; Wallenstein, S.; Kleinman, M.H.; O’Carroll, P.; Mercy, J. Suicide clusters: An examination of age-specific effects. Am. J. Public Health 1990, 80, 211–212. [Google Scholar] [CrossRef]
- Larkin, G.; Beautrais, A. Geospatial Mapping of Suicide Clusters; Te Pou o Te Whakaaro Nui: Auckland, New Zealand, 2012. [Google Scholar]
- Biddle, L.; Donovan, J.; Hawton, K.; Kapur, N.; Gunnell, D. Suicide and the internet. BMJ 2008, 336, 800–802. [Google Scholar] [CrossRef] [PubMed]
- Haw, C.; Hawton, K.; Niedzwiedz, C.; Platt, S. Suicide clusters: A review of risk factors and mechanisms. Suicide Life Threat Behav. 2013, 43, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Joiner, T.E., Jr. The clustering and contagion of suicide. Curr. Dir. Psychol. Sci. 1999, 8, 89–92. [Google Scholar] [CrossRef]
- Cox, G.R.; Owens, C.; Robinson, J.; Nicholas, A.; Lockley, A.; Williamson, M.; Cheung, Y.T.D.; Pirkis, J. Interventions to reduce suicides at suicide hotspots: A systematic review. BMC Public Health 2013, 13, 214. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; Chang, S.S.; Yip, P. Individual-, household-and neighbourhood-level characteristics associated with life satisfaction: A multilevel analysis of a population-based sample from Hong Kong. Urban Stud. 2017, 54, 3700–3717. [Google Scholar] [CrossRef]
- Hanssens, L. ‘Echo Clusters’-Are they a Unique Phenomenon of Indigenous Attempted and Completed Suicide? Aborig. Isl. Health Work J. 2010, 34, 17–26. [Google Scholar] [CrossRef]
- Hanssens, L. Suicide Echo Clusters: Are they Socially Determined, and the Result of a Pre-existing Vulnerability in Indigenous Communities in the Northern Territory? Aborig. Isl. Health Work J. 2011, 35, 14. [Google Scholar]
- Jones, P.; Gunnell, D.; Platt, S.; Scourfield, J.; Lloyd, K.; Huxley, P.; John, A.; Kamran, B.; Wells, C.; Dennis, M. Identifying probable suicide clusters in Wales using national mortality data. PLoS ONE 2013, 8, e71713. [Google Scholar] [CrossRef] [PubMed]
- Bando, D.H.; Moreira, R.S.; Pereira, J.C.; Barrozo, L.V. Spatial clusters of suicide in the municipality of Sao Paulo 1996–2005: An ecological study. BMC Psychiatry 2012, 12, 124. [Google Scholar] [CrossRef]
- Larkin, G.; Beautrais, A.L.; Xu, H. Geospatial mapping of suicide clusters in Cantebury New Zealand. Inj. Prev. 2010, 16 (Suppl. 1), A258. [Google Scholar] [CrossRef]
- Mclafferty, S. Disease cluster detection methods: Recent developments and public health implications. Ann. GIS 2015, 21, 127–133. [Google Scholar] [CrossRef]
- Kulldorff, M. A spatial scan statistic. Commun. Stat.-Theory Methods 1997, 26, 1481–1496. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Bando, D.H.; Brunoni, A.R.; Bensenor, I.M.; Lotufo, P.A. Suicide rates and income in Sao Paulo and Brazil: A temporal and spatial epidemiologic analysis from 1996 to 2008. BMC Psychiatry 2012, 12, 127. [Google Scholar] [CrossRef]
- Hill, N.T.; Spittal, M.J.; Pirkis, J.; Torok, M.; Robinson, J. Risk factors associated with suicide clusters in Australian youth: Identifying who is at risk and the mechanisms associated with cluster membership. EClinicalMedicine 2020, 29, 100631. [Google Scholar] [CrossRef] [PubMed]
- Carcach, C. A spatio-temporal analysis of suicide in El Salvador. BMC Public Health 2017, 17, 339. [Google Scholar] [CrossRef]
- Ngui, A.N.; Apparicio, P.; Moltchanova, E.; Vasiliadis, H.M. Spatial analysis of suicide mortality in Québec: Spatial clustering and area factor correlates. Psychiatry Res. 2014, 220, 20–30. [Google Scholar] [CrossRef]
- Cheung, Y.T.D.; Spittal, M.J.; Williamson, M.K.; Tung, S.J.; Pirkis, J. Application of scan statistics to detect suicide clusters in Australia. PLoS ONE 2013, 8, e54168. [Google Scholar] [CrossRef] [PubMed]
- Exeter, D.J.; Boyle, P.J. Does young adult suicide cluster geographically in Scotland? J. Epidemiol. Community Health 2007, 61, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.M.; Woodside, J.M.; Johnson, A.; Pollack, J.M. Spatial patterns and neighborhood characteristics of overall suicide clusters in Florida from 2001 to 2010. Am. J. Prev. Med. 2017, 52, e1–e7. [Google Scholar] [CrossRef]
- Robinson, J.; Too, L.S.; Pirkis, J.; Spittal, M.J. Spatial suicide clusters in Australia between 2010 and 2012: A comparison of cluster and non-cluster among young people and adults. BMC Psychiatry 2016, 16, 417. [Google Scholar] [CrossRef]
- Núñez-González, S.; Lara-Vinueza, A.G.; Gault, C.; Delgado-Ron, J.A. Trends and spatial patterns of suicide among adolescent in Ecuador, 1997–2016. Clin. Pract. Epidemiol. Ment. Health 2018, 14, 283. [Google Scholar] [CrossRef] [PubMed]
- Sy, K.T.L.; Shaman, J.; Kandula, S.; Pei, S.; Gould, M.S.; Keyes, K.M. Spatiotemporal clustering of suicides in the US from 1999 to 2016: A spatial epidemiological approach. Soc. Psychiatry Psychiatr. Epidemiol. 2019, 54, 1471–1482. [Google Scholar] [CrossRef] [PubMed]
- Milner, A.; Too, L.S.; Spittal, M.J. Cluster Suicides among Unemployed Persons in Australia Over the Period 2001–2013. Soc. Indic. Res. 2018, 137, 189–201. [Google Scholar] [CrossRef]
- Gibbons, R.D.; Clark, D.C.; Fawcett, J. A statistical method for evaluating suicide clusters and implementing cluster surveillance. Am. J. Epidemiol. 1990, 132 (Suppl. 1), S183–S191. [Google Scholar] [CrossRef] [PubMed]
- Kirch, M.R.; Lester, D. Suicide from the Golden Gate Bridge: Do they cluster over time? Psychol. Rep. 1986, 59, 1314. [Google Scholar] [CrossRef] [PubMed]
- Cox, B.; Skegg, K. Contagious suicide in prisons and police cells. J. Epidemiol. Community Health 1993, 47, 69–72. [Google Scholar] [CrossRef]
- Fontanella, C.A.; Saman, D.M.; Campo, J.V.; Hiance-Steelesmith, D.L.; Bridge, J.A.; Sweeney, H.A.; Root, E.D. Mapping suicide mortality in Ohio: A spatial epidemiological analysis of suicide clusters and area level correlates. Prev. Med. 2018, 106, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Hu, W.; Page, A.; Tong, S. Spatial clusters of suicide in Australia. BMC Psychiatry 2012, 12, 86. [Google Scholar] [CrossRef]
- Qi, X.; Tong, S.; Hu, W. Spatial distribution of suicide in Queensland, Australia. BMC Psychiatry 2010, 10, 106. [Google Scholar] [CrossRef] [PubMed]
- Strauss, M.J.; Klimek, P.; Sonneck, G.; Niederkrotenthaler, T. Suicides on the Austrian railway network: Hotspot analysis and effect of proximity to psychiatric institutions. R. Soc. Open Sci. 2017, 4, 160711. [Google Scholar] [CrossRef] [PubMed]
- Tomita, M.; Kubota, T.; Ishioka, F. Spatial Clustering Properties in the Temporal Variation of Suicide Rates/Numbers among Japanese Citizens: A Comprehensive Comparison and Discussion. PLoS ONE 2015, 10, e0127358. [Google Scholar] [CrossRef] [PubMed]
- Too, L.S.; Pirkis, J.; Milner, A.; Bugeja, L.; Spittal, M.J. Railway suicide clusters: How common are they and what predicts them? Inj. Prev. 2017, 23, 328–333. [Google Scholar] [CrossRef] [PubMed]
- Too, L.; Pirkis, J.; Milner, A.; Spittal, M. Clusters of suicides and suicide attempts: Detection, proximity, and correlates. Epidemiol. Psychiatr. Sci. 2017, 26, 491–500. [Google Scholar] [CrossRef]
- Sugg, M.M.; Woolard, S.; Lawrimore, M.; Michael, K.D.; Runkle, J.D. Spatial Clustering of Suicides and Neighborhood Determinants in North Carolina, 2000 to 2017. Appl. Spat. Anal. Policy. 2021, 14, 395–413. [Google Scholar] [CrossRef]
- Lai, C.; Law, Y.W.; Shum, A.K.; Ip, F.W.; Yip, P.S. A community-based response to a suicide cluster: A Hong Kong experience. Crisis 2020, 41, 163–171. [Google Scholar] [CrossRef]
- Too, L.S.; Spittal, M.J. Suicide Clusters among Top 10 High-Risk Occupations: A Study From 2001 to 2016 in Australia. J. Nerv. Ment. Dis. 2020, 208, 942–946. [Google Scholar] [CrossRef]
- Hill, N.T.; Too, L.S.; Spittal, M.J.; Robinson, J. Understanding the characteristics and mechanisms underlying suicide clusters in Australian youth: A comparison of cluster detection methods. Epidemiol. Psychiatr. Sci. 2020, 29, e151. [Google Scholar] [CrossRef]
- Yamaoka, K.; Suzuki, M.; Inoue, M.; Ishikawa, H.; Tango, T. Spatial clustering of suicide mortality and associated community characteristics in Kanagawa prefecture, Japan, 2011–2017. BMC Psychiatry 2020, 20, 74. [Google Scholar] [CrossRef]
- Hsu, C.Y.; Chang, S.S.; Lee, E.S.; Yip, P.S. Geography of suicide in Hong Kong: Spatial patterning, and socioeconomic correlates and inequalities. Soc. Sci. Med. 2015, 130, 190–203. [Google Scholar] [CrossRef]
- Yoshioka, E.; Hanley, S.J.; Sato, Y.; Saijo, Y. Geography of suicide in Japan: Spatial patterning and rural–urban differences. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 731–7466. [Google Scholar] [CrossRef]
- Vaz, E.; Shaker, R.R.; Cusimano, M.D. A geographical exploration of environmental and land use characteristics of suicide in the greater Toronto area. Psychiatry Res. 2020, 1, 112790. [Google Scholar] [CrossRef]
- Pérez-Costillas, L.; Blasco-Fontecilla, H.; Benítez, N.; Comino, R.; Antón, J.M.; Ramos-Medina, V.; López, A.; Palomo, J.L.; Madrigal, L.; Alcalde, J.; et al. Space–time suicide clustering in the community of Antequera (Spain). Rev. Psiquiatr. Salud Men. 2015, 8, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Kassem, A.M.; Carter, K.K.; Johnson, C.J.; Hahn, C.G. Peer Reviewed: Spatial Clustering of Suicide and Associated Community Characteristics, Idaho, 2010–2014. Prev. Chronic Dis. 2019, 16, E37. [Google Scholar] [CrossRef]
- Takahashi, K.; Yokoyama, T.; Tango, T. FleXScan v3. 1: Software for the Flexible Scan Statistic; National Institute of Public Health: Tokyo, Japan, 2010. [Google Scholar]
- Lersch, K.M. Exploring the geography of suicide threats and suicide attempts: An application of Risk Terrain Modeling. Soc. Sci. Med. 2020, 249, 112860. [Google Scholar] [CrossRef] [PubMed]
- Ceccato, V.; Uittenbogaard, A. Suicides in commuting railway systems: The case of Stockholm county, Sweden. J. Affect. Disord. 2016, 198, 206–2157. [Google Scholar] [CrossRef] [PubMed]
- Tidemalm, D.; Runeson, B.; Waern, M.; Frisell, T.; Carlström, E.; Lichtenstein, P.; Långström, N. Familial clustering of suicide risk: A total population study of 11.4 million individuals. Psychol. Med. 2011, 41, 2527–2534. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, A.D.; Guimarães, L.M.L.; De Carvalho, Y.F.; Viana, L.D.C.; Alves, G.L.; Lima, A.C.R.; Santos, M.B.; Góes, M.A.D.O.; De Araújo, K.C.G.M. Spatial analysis and temporal trends of suicide mortality in Sergipe, Brazil, 2000–2015. Trends Psychiatry Psychother. 2018, 40, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Bando, D.H.; Barrozo, L.V.; Volpe, F.M. Geographical clusters and social risk factors for suicide in the city of São Paulo, 2006–2015: An ecologic study. Int. J. Soc. Psychiatry 2020, 66, 460–468. [Google Scholar] [CrossRef]
- Beringuel, B.M.; de Barros Canuto, I.M.; Silva, A.P.; do Bonfim, C.V. Epidemiology and Spatiotemporal Clustering of Suicides in the State of Pernambuco (1999–2018). Trends Psychol. 2021, 29, 123–138. [Google Scholar] [CrossRef]
- Guo, Y.; Chau, P.P.; Chang, Q.; Woo, J.; Wong, M.; Yip, P.S. The geography of suicide in older adults in Hong Kong: An ecological study. Int. J. Geriatr. Psychiatry 2020, 35, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Santos, E.G.; Barbosa, I.R.; Severo, A.K. Space-time analysis of mortality by suicide in the State of Rio Grande do Norte, Brazil, in the period from 2000 to 2015. Cien Saude Colet. 2020, 25, 633–643. [Google Scholar] [CrossRef] [PubMed]
- Reser, J.P. Australian Aboriginal suicide deaths in custody: Cultural context and cluster evidence. Aust. Psychol. 1989, 24, 325–342. [Google Scholar] [CrossRef]
- Lazzarini, T.A.; Gonçalves, C.C.M.; Benites, W.M.; Silva LFd Tsuha, D.H.; Ko, A.I.; Rohrbaugh, R.; Andrews, J.R.; Croda, J. Suicide in Brazilian indigenous communities: Clustering of cases in children and adolescents by household. Rev. Saúde Públ. 2018, 52, 56. [Google Scholar] [CrossRef]
- Austin, A.E.; van den Heuvel, C.; Byard, R.W. Cluster hanging suicides in the young in South Australia. J. Forensic Sci. 2011, 56, 1528–1530. [Google Scholar] [CrossRef]
- Mackenzie, D.W.; Lester, D.; Manson, R.; Yeh, C. Do suicides from the Golden Gate Bridge cluster? Psychol. Rep. 2016, 118, 70–73. [Google Scholar] [CrossRef] [PubMed]
- Torok, M.; Konings, P.; Batterham, P.J.; Christensen, H. Spatial clustering of fatal, and non-fatal, suicide in new South Wales, Australia: Implications for evidence-based prevention. BMC Psychiatry 2017, 17, 339. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.S.; Petrie, K.; Kleinman, M.H.; Wallenstein, S. Clustering of attempted suicide: New Zealand national data. Int. J. Epidemiol. 1994, 23, 1185–1189. [Google Scholar] [CrossRef]
- Leung, M.; Chow, C.B.; Ip, P.; Yip, S. Pure spatial and space-time clusters of self-harm in Kwai Tsing 2004 to 2012. Spat Spatiotemporal Epidemiol. 2018, 27, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Karami, M.; Yazdi–Ravandi, S.; Ghaleiha, A.; Olfatifar, M. Comparison of the clusters and non-clusters areas of attempted suicide cases in Hamadan Province, western Iran: Findings from a pilot study (2016–2017). J. Res. Health Sci. 2018, 18, e00425. [Google Scholar] [CrossRef]
- Smeeton, N.; Wilkinson, G. The identification of clustering in parasuicide. Br. J. Psychiatry 1988, 153, 218–221. [Google Scholar] [CrossRef]
- Mittendorfer-Rutz, E.; Rasmussen, F.; Wasserman, D. Familial clustering of suicidal behaviour and psychopathology in young suicide attempters. Soc. Psychiatry Psychiatr. Epidemiol. 2008, 43, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Pisinger, V.S.; Hawton, K.; Tolstrup, J.S. School-and class-level variation in self-harm, suicide ideation and suicide attempts in Danish high schools. Scand. J. Public Health 2019, 47, 146–156. [Google Scholar] [CrossRef] [PubMed]
- Goodman, M.L.; Puffer, E.S.; Keiser, P.H.; Gitari, S. Suicide clusters among young Kenyan men. Health Psychol. 2020, 25, 1004–1013. [Google Scholar] [CrossRef] [PubMed]
- Queinec, R.; Benjamin, C.; Beitz, C.; Lagarde, E.; Encrenaz, G. Suicide contagion in France: An epidemiologic study. Inj. Prev. 2010, 16 (Suppl. 1), A241. [Google Scholar] [CrossRef]
- Jonas, K. Modelling and suicide: A test of the Werther effect. Br. J. Soc. Psychol. 1992, 31, 295–306. [Google Scholar] [CrossRef]
- Sinyor, M.; Williams, M.; Tran, U.S.; Schaffer, A.; Kurdyak, P.; Pirkis, J.; Niederkrotenthaler, T. Suicides in Young People in Ontario Following the Release of “13 Reasons Why”. Can. J. Psychiatry 2019, 64, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Niederkrotenthaler, T.; Stack, S.; Till, B.; Sinyor, M.; Pirkis, J.; Garcia, D.; Rockett, I.R.H.; Tran, U.S. Association of increased youth suicides in the United States with the release of 13 Reasons Why. JAMA Psychiatry 2019, 76, 933–940. [Google Scholar] [CrossRef]
- Whitley, R.; Fink, D.S.; Santaella-Tenorio, J.; Keyes, K.M. Suicide mortality in Canada after the death of Robin Williams, in the context of high-fidelity to suicide reporting guidelines in the Canadian media. Can. J. Psychiatry 2019, 64, 805–812. [Google Scholar] [CrossRef] [PubMed]
- Fink, D.S.; Santaella-Tenorio, J.; Keyes, K.M. Increase in suicides the months after the death of Robin Williams in the US. PLoS ONE 2018, 13, e0191405. [Google Scholar] [CrossRef] [PubMed]
- Pirkis, J.; Currier, D.; Too, L.S.; Bryant, M.; Bartlett, S.; Sinyor, M.; Spittal, M.J. Suicides in Australia following media reports of the death of Robin Williams. Aust. N. Z. J. Psychiatry 2020, 54, 99–104. [Google Scholar] [CrossRef]
- Sinyor, M.; Tran, U.S.; Garcia, D.; Till, B.; Voracek, M.; Niederkrotenthaler, T. Suicide mortality in the United States following the suicides of Kate Spade and Anthony Bourdain. 2020. Aust. N. Z. J. Psychiatry 2021, 55, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Bridge, J.A.; Greenhouse, J.B.; Ruch, D.; Stevens, J.; Ackerman, J.; Sheftall, A.H.; Horowitz, L.M.; Kelleher, K.J.; Campo, J.V. Association between the release of netflix’s 13 Reasons Why and suicide rates in the United States: An interrupted time series analysis. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 236–243. [Google Scholar] [CrossRef] [PubMed]
- Romer, D. Reanalysis of the Bridge et al. study of suicide following release of 13 Reasons Why. PLoS ONE 2020, 15, e0227545. [Google Scholar] [CrossRef]
- Jang, S.A.; Sung, J.M.; Park, J.Y.; Jeon, W.T. Copycat suicide induced by entertainment celebrity suicides in South Korea. Psychiatry Investig. 2016, 13, 74. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Tsai, P.C.; Chen, P.H.; Fan, C.C.; Hung, G.C.L.; Cheng, A.T. Effect of media reporting of the suicide of a singer in Taiwan: The case of Ivy Li. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.P.; Carstensen, L.L. Clustering of teenage suicides after television news stories about suicide. N. Engl. J. Med. 1986, 315, 685–689. [Google Scholar] [CrossRef] [PubMed]
- Ladwig, K.H.; Kunrath, S.; Lukaschek, K.; Baumert, J. The railway suicide death of a famous German football player: Impact on the subsequent frequency of railway suicide acts in Germany. J. Affect. Disord. 2012, 136, 194–198. [Google Scholar] [CrossRef]
- Cheng, Q.; Chen, F.; Yip, P.S. The Foxconn suicides and their media prominence: Is the Werther Effect applicable in China? BMC Public Health 2011, 11, 841. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y. Media Coverage of Adolescent and Celebrity Suicides and Imitation Suicides among Adolescents. J. Broadcast. Electron. Media 2019, 63, 130–143. [Google Scholar] [CrossRef]
- Koburger, N.; Mergl, R.; Rummel-Kluge, C.; Ibelshäuser, A.; Meise, U.; Postuvan, V.; Roskar, S.; Székely, A.; Tóth, M.D.; Van der Feltz-Cornelis, C.; et al. Celebrity suicide on the railway network: Can one case trigger international effects? J. Affect. Disord. 2015, 85, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Etzersdorfer, E.; Sonneck, G.; Nagel-Kuess, S. Newspaper reports and suicide. N. Engl. J. Med. 1992. [Google Scholar] [CrossRef]
- Too, L.S.; Pirkis, J.; Milner, A.; Robinson, J.; Spittal, M.J. Clusters of suicidal events among young people: Do clusters from one time period predict later clusters? Suicide Life Threat Behav. 2019, 49, 561–571. [Google Scholar] [CrossRef]
- Lawson, A.B.; Kleinman, K. Spatial and Syndromic Surveillance for Public Health; John Wiley & Sons: Hoboken, NJ, USA, 2005. [Google Scholar]
- Maurya, S.P.; Ohri, A.; Mishra, S. (Eds.) Open-Source GIS: A Review. In Proceedings of the National Conference on Open-Source GIS: Opportunities and Challenges, Varanasi, India, 9–10 October 2015. [Google Scholar]
- Nsubuga, P.; White, M.E.; Thacker, S.B.; Anderson, M.A.; Blount, S.B.; Broome, C.V.; Chiller, T.M.; Espitia, V.; Imtiaz, R.; Sosin, D.; et al. Public Health Surveillance: A Tool for Targeting and Monitoring Interventions. In Disease Control Priorities in Developing Countries, 2nd ed.; Jamison, D.T., Breman, J.G., Measham, A.R., Alleyne, G., Claeson, M., Evans, D.B., Jha, P., Mills, A., Musgrove, P., Eds.; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA; Oxford University Press: New York, NY, USA, 2006; Chapter 53; pp. 99–1015. ISBN -10 0-8213-6179-1. [Google Scholar]
- Cromley, E.K.; McLafferty, S.L. GIS and Public Health; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Ishioka, F.; Kurihara, K. (Eds.) Evaluation of Hotspot Detection Method Based on Echelon Structure. In Proceedings of the 59th ISI World Statistics Congress, Hong Kong, China, 25–30 August 2013; p. 5366. [Google Scholar]
- Tango, T.; Takahashi, K. A flexibly shaped spatial scan statistic for detecting clusters. Int. J. Health Geogr. 2005, 4, 11. [Google Scholar] [CrossRef]
- Patil, G.P.; Taillie, C. Upper-level set scan statistic for detecting arbitrarily shaped hotspots. Environ. Ecol. Stat. 2004, 11, 183–197. [Google Scholar] [CrossRef]
- Kurihara, K. Hotspots Detection for Cellular Surface Data. Bull. Int. Stat. Inst. 2003, 54, 115–116. [Google Scholar]
- Tango, T.; Takahashi, K. A flexible spatial scan statistic with a restricted likelihood ratio for detecting disease clusters. Stat. Med. 2012, 31, 4207–4218. [Google Scholar] [CrossRef]
- Myers, W.; Patil, G.P.; Joly, K. Echelon approach to areas of concern in synoptic regional monitoring. Environ. Ecol. Stat. 1997, 4, 131–152. [Google Scholar] [CrossRef]
- Kurihara, K.; Ishioka, F.; Kajinishi, S. Spatial and temporal clustering based on the echelon scan technique and software analysis. JJSD 2020, 3, 313–332. [Google Scholar] [CrossRef]
- Terrell, C. Predictions in Time Series Using Regression Models; Scientific e-Resources: New Delhi, India, 2019. [Google Scholar]
- Värnik, P.; Sisask, M.; Värnik, A.; Laido, Z.; Meise, U.; Ibelshäuser, A.; Van Audenhove, C.; Reynders, A.; Kocalevent, R.D.; Kopp, M.; et al. Suicide registration in eight European countries: A qualitative analysis of procedures and practices. Forensic Sci. Int. 2010, 202, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Baran, A.; Gerstner, R.; Ueda, M.; Gmitrowicz, A. Implementing real-time data suicide surveillance systems. Crisis 2021, 42, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Kulldorff, M. Prospective time periodic geographical disease surveillance using a scan statistic. J. R. Stat. Soc. Ser. A 2001, 164, 61–72. [Google Scholar] [CrossRef]
| Number of Studies | 51 | ||||||||||||
| Level of data used in the study | Location | City | State | Regional | National | ||||||||
| 2 | 2 | 6 | 18 | 23 | |||||||||
| Type of analysis (Studies that performed multiple statistical analyses are counted twice.) | Nearest Neighbour Statistic | Kernel density estimator | Spherical Trigonometry | Descriptive network analysis | Knox procedure | Ripleys k function | Chi-square | Fishers Exact Test | Morans I | Bayesian hierarchical model | Anderson Darling | Regression model | Poisson model |
| 1 | 2 | 1 | 1 | 1 | 1 | 5 | 1 | 4 | 6 | 1 | 10 | 28 | |
| Geospatial analysis conducted | No | Yes | |||||||||||
| 13 | 38 | ||||||||||||
| Clusters detected | No | Yes | |||||||||||
| 3 | 48 | ||||||||||||
| Addressed analysed | Not specified | Location of death | Residence | ||||||||||
| 4 | 13 | 34 | |||||||||||
| SaTScan spatial applied | Not specified | No | Yes | ||||||||||
| 7 | 24 | 20 | |||||||||||
| Number of clusters reported | Not specified | 20+ | 1–20 | No clusters detected | |||||||||
| 7 | 3 | 28 | 3 | ||||||||||
| Number of Studies | 8 | |||||||
| Level Of Data Used in the Study | National | National | Regional | City | Regional | City | National | County |
| Location of studies | Sweden | New Zealand | New South Wales, Australia | Edinburgh, Scotland | Kwai Tsing, Hong Kong | Hamadan, Iran | Denmark | Meru, Kenya |
| Aggregated data used | No | No | Yes | No | Yes | No | Yes | No |
| Type of statistical analysis conducted | Logistical regression | SaTScan and Knox Procedure | SaTScan, Hotspot analysis (Getis-Ord Gi*) and ArcGIS for mapping | A scan interval test proposed by Naus, 1966 | Chi square and SaTScan | Logistic regression and Chi-square, SaTScan and Monte Carlo simulation | Multi-level regressions and log likelihood ratio tests | Multiple logistic regression |
| Geospatial analysis conducted | No | Yes | Yes | No | Yes | Yes | No | No |
| Clusters detected | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Number of clusters reported | Not specified | Not specified | Twenty-five spatial cluster regions identified | 1 cluster | Four spatial clusters, one spatiotemporal cluster | 2 clusters | N/A | Not specified |
| Number of Studies | 19 | |||
| Level of data used in the study | Continental | National | Regional | Provincial |
| 1 | 13 | 4 | 1 | |
| Type of analysis conducted (Studies that performed multiple statistical analyses are counted twice.) | Poisson model | Regression analysis | Non-parametric tests, i.e., Mann–Whitney U test, Kolmogorov-Smirnov test | Time-series models, e.g., SARIMA |
| 4 | 8 | 3 | 11 | |
| Geospatial analysis conducted | Yes | No | ||
| 0 | 19 | |||
| Mass cluster(s) detected | Yes | No | ||
| 17 | 2 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benson, R.; Rigby, J.; Brunsdon, C.; Cully, G.; Too, L.S.; Arensman, E. Quantitative Methods to Detect Suicide and Self-Harm Clusters: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5313. https://doi.org/10.3390/ijerph19095313
Benson R, Rigby J, Brunsdon C, Cully G, Too LS, Arensman E. Quantitative Methods to Detect Suicide and Self-Harm Clusters: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(9):5313. https://doi.org/10.3390/ijerph19095313
Chicago/Turabian StyleBenson, Ruth, Jan Rigby, Christopher Brunsdon, Grace Cully, Lay San Too, and Ella Arensman. 2022. "Quantitative Methods to Detect Suicide and Self-Harm Clusters: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 9: 5313. https://doi.org/10.3390/ijerph19095313
APA StyleBenson, R., Rigby, J., Brunsdon, C., Cully, G., Too, L. S., & Arensman, E. (2022). Quantitative Methods to Detect Suicide and Self-Harm Clusters: A Systematic Review. International Journal of Environmental Research and Public Health, 19(9), 5313. https://doi.org/10.3390/ijerph19095313






