The Development of ICT-Based Exercise Rehabilitation Service Contents for Patients with Musculoskeletal Disorders and Stroke
Abstract
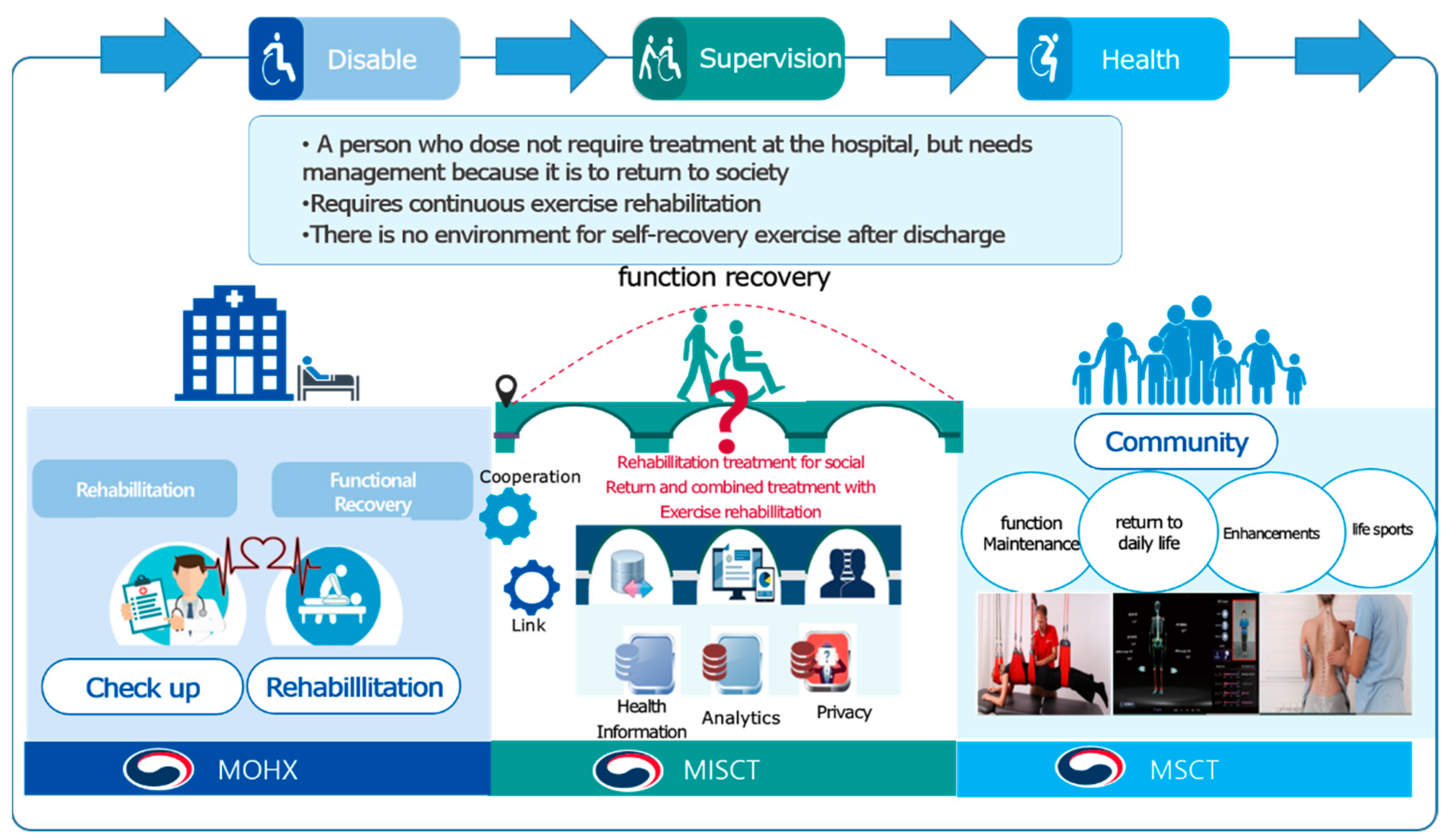
:1. Introduction
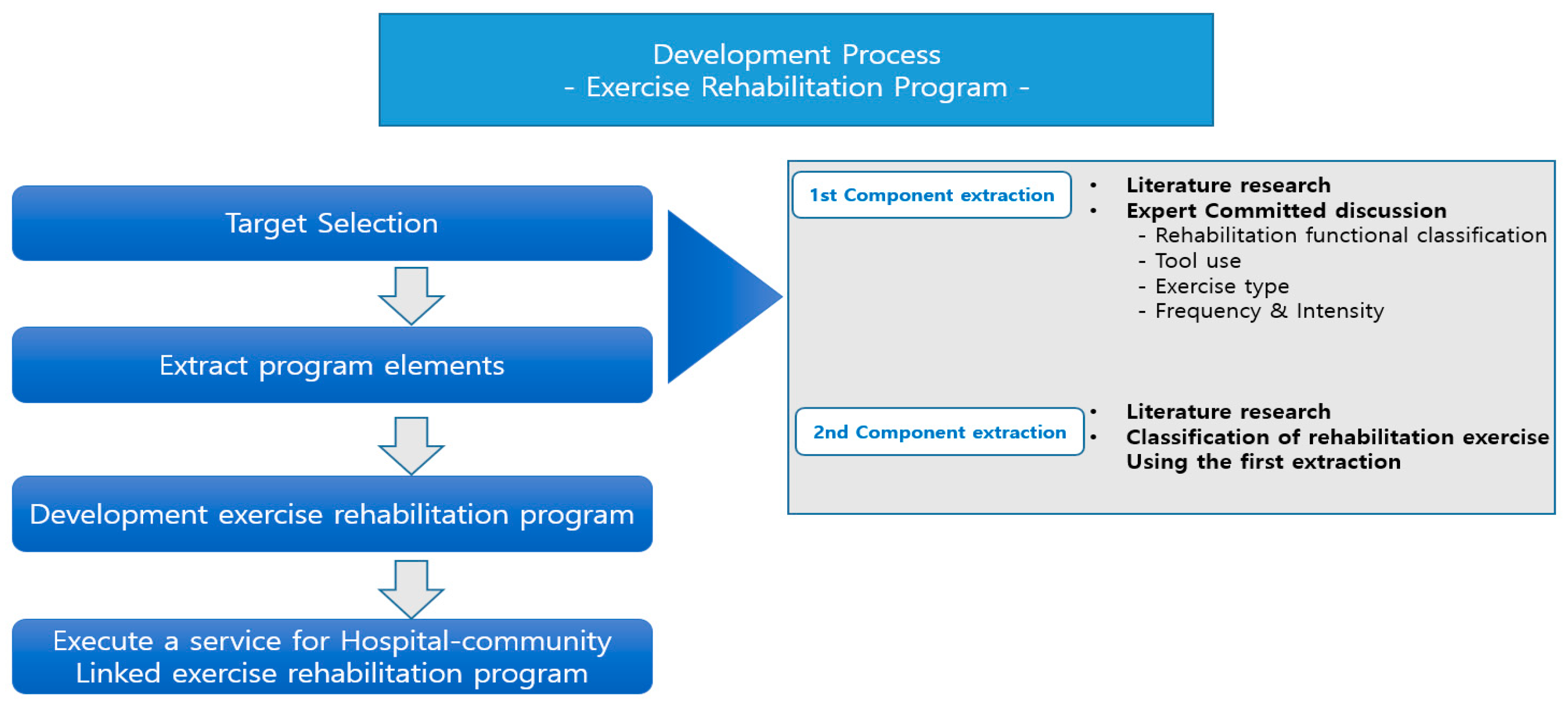
2. Materials and Methods
2.1. Intervention Design and Participants
2.2. Process
2.3. Theoretical Approach
3. Results
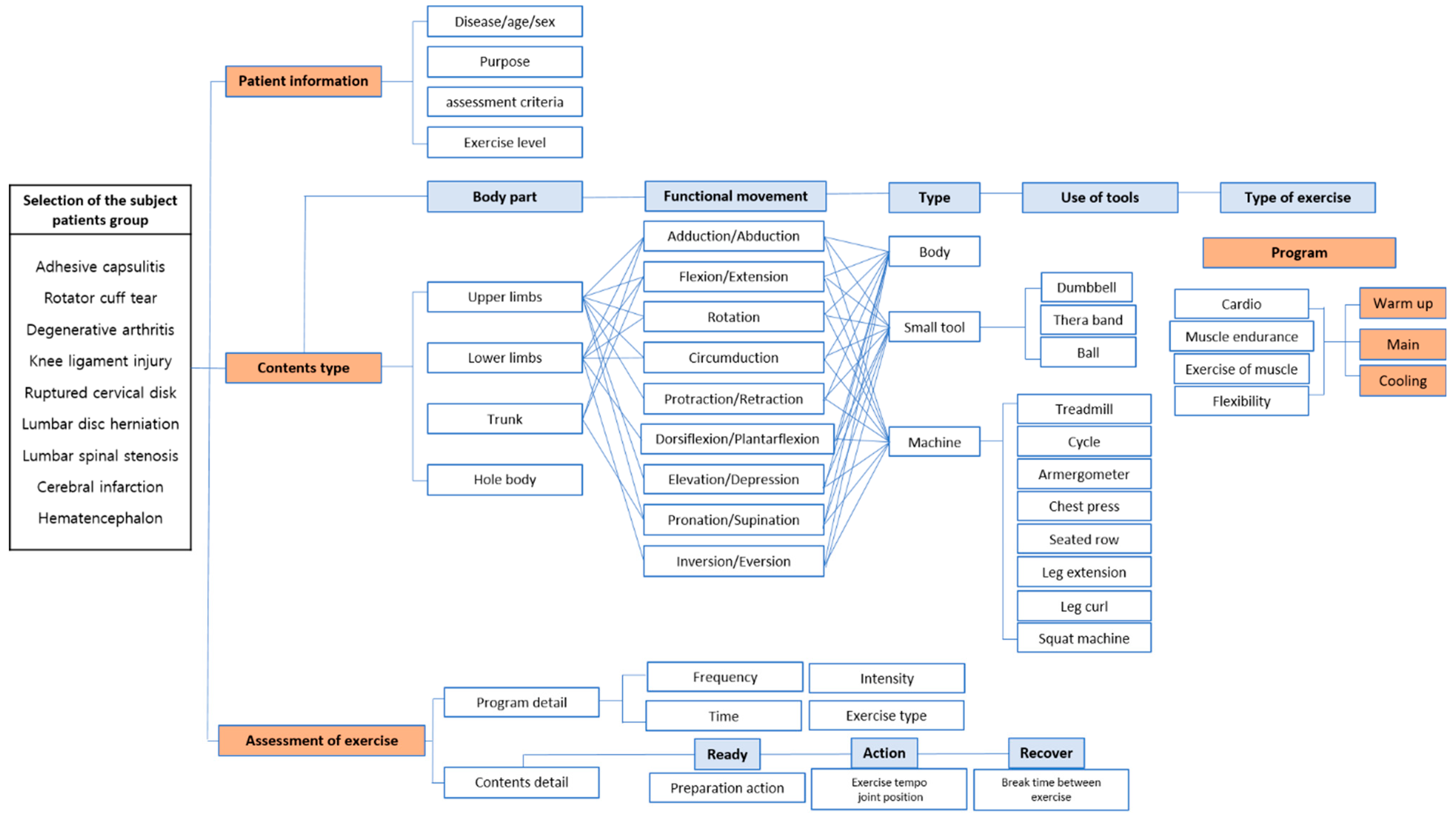
3.1. First Components Selection of the Exercise Rehabilitation Service
- (1)
- Selection of the subject patients group
- (2)
- Functional movement classification
- (3)
- Use of tools
- (4)
- Type of exercise
- (5)
- Frequency and intensity
3.2. Second Components Selection of the Exercise Rehabilitation Service
3.3. Differentiation of Exercise Rehabilitation Service Composition—1: N Movement Classification
3.4. Monitoring Plan
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Healhcare Bigdata Hub. Total Cost of Medical Care by Disease in South Korea, 2020. Available online: http://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do (accessed on 15 December 2021).
- World Health Organization. Musculoskeletal Conditions, 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 15 December 2021).
- Hendi, O.M.; Abdulaziz, A.A.; Althaqafi, A.M.; Hindi, A.M.; Khan, S.A.; Atalla, A.A. Prevalence of musculoskeletal disorders and its correlation to physical activity among health specialty students. Int. J. Prev. Med. 2019, 10, 48. [Google Scholar] [CrossRef] [PubMed]
- Cieza, A.; Causey, K.; Kamenov, K.; Hanson, S.W.; Chatterji, S.; Vos, T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 2006–2017. [Google Scholar] [CrossRef]
- Health Insurance Review and Assessment Service. The Current Status of Musculoskeletal Disorders, 2020. Available online: https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA020041000100&brdScnBltNo=4&brdBltNo=10167 (accessed on 15 December 2021).
- Kuriakose, D.; Xiao, Z. Pathophysiology and Treatment of Stroke: Present Status and Future Perspectives. Int. J. Mol. Sci. 2020, 21, 7609. [Google Scholar] [CrossRef] [PubMed]
- Korean Statistical Information Service. Number of Stroke Patients. Seoul: Stastics Korea, 2019. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=411&tblId=DT_41104_222&conn_path=I2 (accessed on 15 December 2021).
- Demir, S.; Dulgeroglu, D.; Cakci, A. Effects of dynamic lumbar stabilization exercises following lumbar microdiscectomy on pain, mobility and return to work. Randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2014, 50, 627–640. [Google Scholar] [PubMed]
- Bohannon, R. Muscle strength and muscle training after stroke. Acta Derm. Venereol. 2007, 39, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahn, M.S.; Park, J.H. A study on the problems and improvement of long-term care insurance for the elderly. J. Korea Contents Assoc. 2019, 19, 525–534. [Google Scholar]
- Gheno, R.; Cepparo, J.M.; Rosca, C.E.; Cotten, A. Musculoskeletal Disorders in the Elderly. J. Clin. Imaging Sci. 2012, 2, 39. [Google Scholar] [CrossRef]
- Brech, G.C.; Andrusaitis, S.F.; Vitale, G.F.; Greve, J.M.D.A. Correlation of disability and pain with postural balance among women with chronic low back pain. Clinics 2012, 67, 959–962. [Google Scholar] [CrossRef]
- Ciolac, E.G.; Rodrigues-Da-Silva, J.M. Resistance Training as a Tool for Preventing and Treating Musculoskeletal Disorders. Sports Med. 2016, 46, 1239–1248. [Google Scholar] [CrossRef]
- Rodrigues, E.V.; Gomes, A.R.S.; Tanhoffer, A.I.P.; Leite, N. Effects of exercise on pain of musculoskeletal disorders: A systematic review. Acta Ortopédica Bras. 2014, 22, 334–338. [Google Scholar] [CrossRef] [Green Version]
- An, M.; Shaughnessy, M. The Effects of Exercise-Based Rehabilitation on Balance and Gait for Stroke Patients: A Systematic Review. J. Neurosci. Nurs. 2011, 43, 298–307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ada, L.; Dorsch, S.; Canning, C.G. Strengthening interventions increase strength and improve activity after stroke: A systematic review. Aust. J. Physiother. 2006, 52, 241–248. [Google Scholar] [CrossRef] [Green Version]
- Pang, M.Y.; Charlesworth, S.A.; Lau, R.W.; Chung, R.C. Using Aerobic Exercise to Improve Health Outcomes and Quality of Life in Stroke: Evidence-Based Exercise Prescription Recommendations. Cerebrovasc. Dis. 2013, 35, 7–22. [Google Scholar] [CrossRef]
- Oosterhuis, T.; Costa, L.O.P.; Maher, C.; de Vet, H.C.W.; van Tulder, M.W.; Ostelo, R.W.J.G. Rehabilitation after lumbar disc surgery. Cochrane Database Syst. Rev. 2014, 2014, CD003007. [Google Scholar] [CrossRef] [Green Version]
- Selves, C.; Stoquart, G.; Lejeune, T. Gait rehabilitation after stroke: Review of the evidence of predictors, clinical outcomes and timing for interventions. Acta Neurol. Belg. 2020, 120, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Japanese Association of Occupational Therapy. Occupational Therapy Guidelines. Available online: https://www.jaot.or.jp/files/page/wp-content/uploads/2019/02/OTguideline-2018.pdf (accessed on 15 December 2021).
- Nijstad, B.A.; Paulus, P.B. Group Creativity: Common Themes and Future Directions. In Group Creativity: Innovation Through Collaboration New York; Paulus, P.B., Ed.; Oxford University Press: Oxford, UK, 2003; ISBN 978-019-514-730-8. [Google Scholar]
- Oh, A.; So, W.-Y. Assessing the Needs of People with Disabilities for Physical Activities and Sports in South Korea. Healthcare 2022, 10, 265. [Google Scholar] [CrossRef]
- Bolognini, N.; Pascual-Leone, A.; Fregni, F. Using non-invasive brain stimulation to augment motor training-induced plasticity. J. Neuroeng. Rehabil. 2009, 6, 8. [Google Scholar] [CrossRef] [Green Version]
- Zenko, Z.; Ekkekakis, P. Knowledge of Exercise Prescription Guidelines Among Certified Exercise Professionals. J. Strength Cond. Res. 2015, 29, 1422–1432. [Google Scholar] [CrossRef] [PubMed]
- National Academy of Sports Medicine. Essentials of Corrective Exercise Training; Jones & Bartlett Learning: Burlington, MA, USA, 2013. [Google Scholar]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 11th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2021. [Google Scholar]
- Neumann, D. Kinesiology of the Musculoskeletal System, 3rd ed.; C.V. Mosby: Missouri, MD, USA, 2016. [Google Scholar]
- Saunders, D.H.; Greig, C.A.; Mead, G.E. Physical activity and exercise after stroke: Review of multiple meaningful benefits. Stroke 2014, 45, 3742–3747. [Google Scholar] [CrossRef] [Green Version]
- Kisner, C.; Colby, L.A. Therapeutic Exercise: Foundations and Techniques, 6th ed.; F.A. Davis Company: Philadelphia, PA, USA, 2014. [Google Scholar]
- Delavier, F. Strength Training Anatomy, 3rd ed.; Human Kinetics: Champaign, IL, USA, 2010. [Google Scholar]
- Siler, B. The Pilates Body; Harmony Books: New York, NY, USA, 2000. [Google Scholar]
- Belden, J.; Mansoor, M.M.; Hellum, A.; Rahman, S.R.; Meyer, A.; Pease, C.; Pacheco, J.; Koziol, S.; Truscott, T.T. How vision governs the collective behaviour of dense cycling pelotons. J. R. Soc. Interface 2019, 16, 20190197. [Google Scholar] [CrossRef] [Green Version]
- Park, H.S.; Lee, G.A.; Seo, B.-K.; Billinghurst, M. User experience design for a smart-mirror-based personalized training system. Multimed. Tools Appl. 2021, 80, 31159–31181. [Google Scholar] [CrossRef]
- Orlova, Y.A.; Dmitriev, A.S.; Donsckaia, A.R.; Noskin, V.V.; Sibirny, N.D. Development of an approach and software tools to distance the rehabilitation process for adaptation to home use. J. Phys. Conf. Ser. 2021, 2060, 012024. [Google Scholar] [CrossRef]
- Ministry of Culture. Sports and Difficulty, 2020. Available online: https://nfa.kspo.or.kr/front/main/main.do (accessed on 28 December 2021).
- Park, S.; Lee, Y. An Analysis on the Physical Activity Promoting Effect of National Fitness Award Program. J. Korean Soc. Sport Policy 2019, 17, 53–62. [Google Scholar] [CrossRef]
- Jeon, W.J.; Lim, S.W.; Lee, W.H. The Problem and Future Challenges of “National Fitness Award 100” Base Center Managing System. Korean J. Phys. Educ. 2015, 54, 113–126. [Google Scholar]
- Shin, H.I.; Lee, J.E. Development of Standards and Certification Criteria for Early Intensive Rehabilitation Treatment, Policy Activation Plan; Ministry of Health and Welfare: Seoul, Korea, 2014.
- Sheehan, K.J.; Fitzgerald, L.; Lambe, K.; Martin, F.C.; Lamb, S.E.; Sackley, C. Effectiveness of community-based rehabilitation interventions incorporating outdoor mobility on ambulatory ability and falls-related self-efficacy after hip fracture: A systematic review and meta-analysis. Arch. Osteoporos. 2021, 16, 99. [Google Scholar] [CrossRef]
- Kim, J.M.; Moon, H.J.; Shin, B.W.; Lee, D.Y.; Hong, J.H.; Kim, J.S.; Yu, J.H. The effect of lower extremity exercise on gait, balance and proprioceptive sensation with or without AR. Int. J. Psychosoc. Rehabil. 2020, 24, 1651–1660. [Google Scholar]
- Palazzo, C.; Nguyen, C.; Lefevre-Colau, M.-M.; Rannou, F.; Poiraudeau, S. Risk factors and burden of osteoarthritis. Ann. Phys. Rehabil. Med. 2016, 59, 134–138. [Google Scholar] [CrossRef]

| Name | Specialists Classification | Institution | Career/ Year | Name | Specialists Classification | Institution | Career/ Year |
|---|---|---|---|---|---|---|---|
| S1 | Medical Specialists | Doctor | 10 | S21 | Exercise Rehabilitation Specialists | Researcher | 5 |
| S2 | 16 | S22 | 9 | ||||
| S3 | 7 | S23 | 6 | ||||
| S4 | 5 | S24 | 8 | ||||
| S5 | 8 | S25 | 8 | ||||
| S6 | 7 | S26 | Exercise Specialist | 7 | |||
| S7 | Physical Therapist | 21 | S27 | 9 | |||
| S8 | 16 | S28 | 10 | ||||
| S9 | 8 | S29 | 6 | ||||
| S10 | 9 | S30 | 12 | ||||
| S11 | 7 | S31 | 5 | ||||
| S12 | 11 | S32 | 8 | ||||
| S13 | 6 | S33 | ICT Development Specialist | Electronics and Telecommunications Research Institute | 8 | ||
| S14 | Exercise Rehabilitation Specialists | Professor | 7 | S34 | 10 | ||
| S15 | 7 | S35 | 7 | ||||
| S16 | 14 | S36 | 6 | ||||
| S17 | 11 | S37 | 16 | ||||
| S18 | 12 | S38 | 14 | ||||
| S19 | 6 | S39 | 9 | ||||
| S20 | 8 | S40 | 12 |
| Plane | Joint Movements |
|---|---|
| Sagittal plane | Flexion/Extension |
| Frontal plane | Abduction/Adduction |
| Lateral Flexion | |
| Inversion/Eversion | |
| Transverse plane | Lateral Rotation/External Rotation |
| Spinal Rotation | |
| Horizontal Adduction/Horizontal Abduction | |
| Combined joint movement | Protraction/Retraction |
| Dorsiflexion/Plantar flexion | |
| Elevation/Depression | |
| Pronation/Supination | |
| Circumduction |
| Category | Theme Cluster | Theme | |
|---|---|---|---|
| Selection of the subject patients group | Adhesive capsulitis | Shoulder Joint | Upper Limbs |
| Rotator cuff tear | |||
| Degenerative arthritis | Knee Joint | Low Limbs | |
| Knee ligament injury | |||
| Ruptured cervical disk | Cervical | Trunk | |
| Lumbar disc herniation | Lumbar | ||
| Lumbar spinal stenosis | |||
| Cerebral infarction | Brain-Blood Vessel | Whole Body | |
| Hematencephalon | |||
| Functional movement classification | Adduction/Abduction | Adduction/Abduction | |
| Horizontal Adduction/Horizontal Abduction | |||
| Flexion/Extension | Flexion/Extension | ||
| Lateral Flexion | |||
| Rotation | Lateral Rotation/External Rotation | ||
| Spinal Rotation | |||
| Circumduction | Circumduction | ||
| Protraction/Retraction | Protraction/Retraction | ||
| Dorsiflexion/Plantarflexion | Dorsiflexion/Plantarflexion | ||
| Elevation/Depression | Elevation/Depression | ||
| Pronation/Supination | Pronation/Supination | ||
| Inversion/Eversion | Inversion/Eversion | ||
| Use of tools | Small Tool | Chair, Dumbbell, Thera band, Ball, Step Box | |
| Machine | Treadmill, Cycle, Arm Ergometer, Chest Press, Seated Row, Butterfly, Leg Press, Leg Extension, Leg Curl, Squat Machine, Sit Up, Back Extension | ||
| Type of exercise | Health-related physical fitness elements | Cardiopulmonary Endurance, Muscle Endurance, Flexibility | |
| Skill-related physical fitness elements | Agility, Coordination, Balance | ||
| Muscular Strength | ||||||
|---|---|---|---|---|---|---|
| Body Part | Category | Standard Exercise (1) | Category | Exercise Variations (N) | ||
| Upper Limbs | Picture |  | Picture |  |  |  |
| Name | Shoulder flexion (seated chair, one arm) | Shoulder flexion (using dumbbell, one arm) | Shoulder flexion (using band, one arm) | |||
| Equipment | Chair | Dumbbells | Band | |||
| Frequency | 2–3 days/week | 2–3 days/week | 2–3 days/week | |||
| Intensity | 40–60% of MVC | 40–60% of MVC | 40–60% of MVC | |||
| Volume | Repetitions: 10 | Repetitions: 10 | Repetitions: 10 | |||
| Sets: 3–4 | Sets: 3–4 | Sets: 3–4 | ||||
| Pattern: 1 min | Pattern: 1 min | Pattern: 1 min | ||||
| Picture |  |  | ||||
| Name | Shoulder flexion (standing, one arm) | Name | Shoulder flexion (prone position, one arm) | Shoulder flexion (prone position, using dumbbell, one arm) | ||
| Use of tools | None | Use of tools | None | Dumbbells | ||
| Frequency | 2–3 days/week | Frequency | 2–3 days/week | 2–3 days/week | ||
| Intensity | 40–60% of MVC | Intensity | 40–60% of MVC | 40–60% of MVC | ||
| Volume | Repetitions: 10 | Volume | Repetitions: 10 | Repetitions: 10 | ||
| Sets: 3–4 | Sets: 3–4 | Sets: 3–4 | ||||
| Pattern *: 1 min | Pattern: 1 min | Pattern: 1 min | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Song, J.; Kim, D.; Park, J. The Development of ICT-Based Exercise Rehabilitation Service Contents for Patients with Musculoskeletal Disorders and Stroke. Int. J. Environ. Res. Public Health 2022, 19, 5022. https://doi.org/10.3390/ijerph19095022
Kim J, Song J, Kim D, Park J. The Development of ICT-Based Exercise Rehabilitation Service Contents for Patients with Musculoskeletal Disorders and Stroke. International Journal of Environmental Research and Public Health. 2022; 19(9):5022. https://doi.org/10.3390/ijerph19095022
Chicago/Turabian StyleKim, Jiyoun, Jiyeon Song, Donguk Kim, and Jinho Park. 2022. "The Development of ICT-Based Exercise Rehabilitation Service Contents for Patients with Musculoskeletal Disorders and Stroke" International Journal of Environmental Research and Public Health 19, no. 9: 5022. https://doi.org/10.3390/ijerph19095022
APA StyleKim, J., Song, J., Kim, D., & Park, J. (2022). The Development of ICT-Based Exercise Rehabilitation Service Contents for Patients with Musculoskeletal Disorders and Stroke. International Journal of Environmental Research and Public Health, 19(9), 5022. https://doi.org/10.3390/ijerph19095022







