Use of Health Services and Rehabilitation before and after the Beginning of Long-Term Sickness Absence—Comparing the Use by Employment and Disability Pension Transition after the Sickness Absence in Finland
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Long-Term Sickness Absence (LTSA) and Disability Pension
2.3. The Follow-Up Setting
2.4. Grouping Based on Employment and Disability Pension Transition after an LTSA
2.5. Data on Outpatient and Inpatient Health Care and Rehabilitation
2.6. Covariates
2.7. Statistical Methods
3. Results
3.1. Characteristics of the LTSA Groups
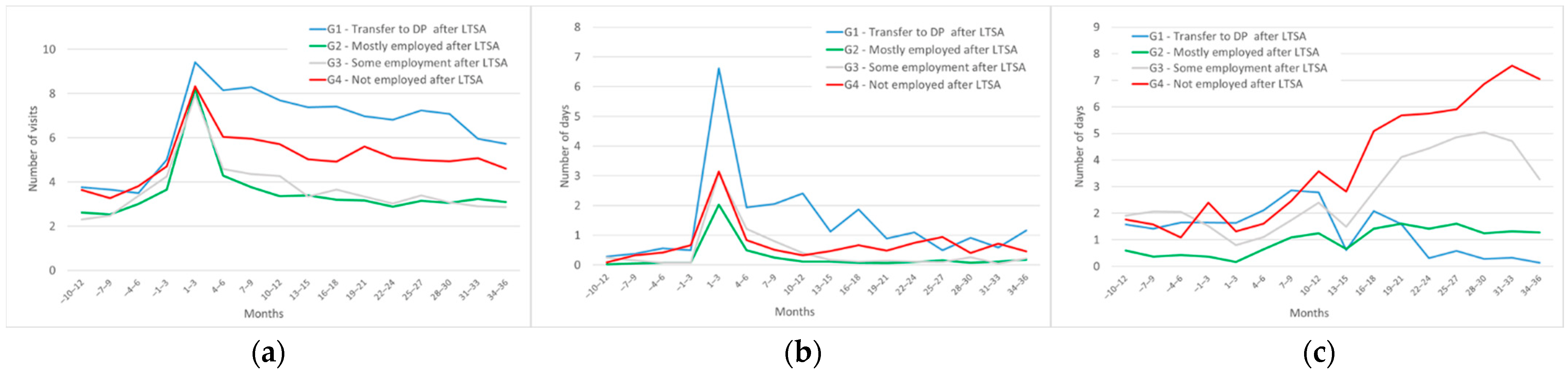
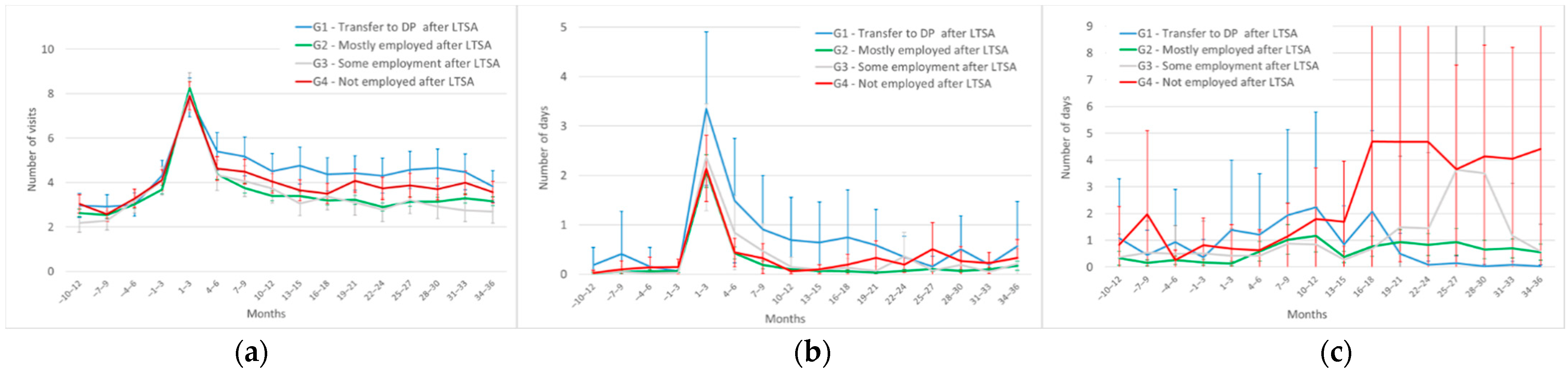
3.2. Unadjusted Averages for Outpatient Health Care, Inpatient Care and Rehabilitation Use
3.3. The Association of LTSA Groups with Service Use after the Start of the LTSA Spell
4. Discussion
4.1. Outpatient and Inpatient Health Care
4.2. Rehabilitation
4.3. Strengths and Limitations
4.4. Practical Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- OECD. Sickness, Disability and Work: Breaking the Barriers—A Synthesis of Findings across OECD Countries; OECD: Paris, France, 2010. [Google Scholar]
- OECD. Public Spending on Incapacity. 2020. Available online: https://data.oecd.org/socialexp/public-spending-on-incapacity.htm#indicator-chart (accessed on 1 July 2021).
- Kivimäki, M.; Ferrie, J.; Hagberg, J.; Head, J.; Westerlund, H.; Vahtera, J. Alexanderson. Diagnosis-specific sick leave as a risk marker for disability pension in a Swedish population. J. Epidemiol. Community Health 2007, 61, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Alexanderson, K.; Kivimäki, M.; Ferrie, J.E.; Westerlund, H.; Vahtera, J.; Singh-Manoux, A.; Melchior, M.; Zins, M.; Goldberg, M.; Head, J. Diagnosis-specific sick leave as a long-term predictor of disability pension: A 13-year follow-up of the GAZEL cohort study. J. Epidemiol. Community Health 2012, 66, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Salonen, L.; Blomgren, J.; Laaksonen, M.; Niemelä, M. Sickness absence as a predictor of disability retirement in different occupational classes: A register-based study of a working-age cohort in Finland in 2007–2014. BMJ Open 2018, 8, e020491. [Google Scholar] [CrossRef] [PubMed]
- Mittendorfer-Rutz, E.; Härkänen, T.; Tiihonen, J.; Haukka, J. Association of Socio-Demographic Factors, Sick-Leave and Health Care Patterns with the Risk of Being Granted a Disability Pension among Psychiatric Outpatients with Depression. PLoS ONE 2014, 9, e99869. [Google Scholar] [CrossRef]
- Perhoniemi, R.; Blomgren, J. Frequent attenders of three outpatient health care schemes in Finland: Characteristics and association with long-term sickness absences, 2016–2018. BMC Public Health 2021, 21, 870. [Google Scholar] [CrossRef]
- Laaksonen, M.; Mastekaasa, A.; Martikainen, P.; Rahkonen, O.; Piha, K.; Lahelma, E. Gender differences in sickness absence—The contribution of occupation and workplace. Scand. J. Work Environ. Health 2010, 36, 394–403. [Google Scholar] [CrossRef] [PubMed]
- Löve, J.; Hensing, G.; Holmgren, K.; Torén, K. Explaining the social gradient in sickness absence: A study of a general working population in Sweden. BMC Public Health 2013, 13, 545. [Google Scholar] [CrossRef]
- Beemsterboer, W.; Stewart, R.; Groothoff, J.; Nijhuis, F. A literature review on sick leave determinants (1984–2004). Int. J. Occup. Med. Environ. Health 2009, 22, 169–179. [Google Scholar] [CrossRef]
- Blomgren, J.; Jäppinen, S. Incidence and Length of Sickness Absence among Hierarchical Occupational Classes and Non-Wage-Earners: A Register Study of 1.6 Million Finns. Int. J. Environ. Res. Public. Health 2021, 18, 501. [Google Scholar] [CrossRef]
- Bergh, H.; Baigia, A.; Månsson, J.; Mattsson, B.; Marklund, B. Predictive factors for long-term sick leave and disability pension among frequent and normal attenders in primary health care over 5 years. Public Health 2007, 121, 25–33. [Google Scholar] [CrossRef]
- Foster, A.; Jordan, K.; Croft, P. Is frequent attendance in primary care disease-specific? Fam. Pract. 2006, 23, 444–452. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Karlsson, H.; Lehtinen, V.; Joukamaa, M. Frequent attenders of Finnish public primary health care: Sociodemographic characteristics and physical morbidity. Fam. Pract. 1994, 11, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Pymont, C.; Butterworth, P. Longitudinal cohort study describing persistent frequent attenders in Australian primary healthcare. BMJ Open 2015, 5, e008975. [Google Scholar] [CrossRef]
- Sumanen, H.; Harkko, J.; Piha, K.; Pietiläinen, O.; Rahkonen, O.; Kouvonen, A. Association between socioeconomic position and occupational health service use trajectories among young municipal employees in Finland. BMJ Open 2019, 9, e028742. [Google Scholar] [CrossRef] [PubMed]
- Vedsted, P.; Olesen, F. Social environment and frequent attendance in Danish general practice. Br. J. Gen. Pract. 2005, 55, 510–515. [Google Scholar] [PubMed]
- Ropponen, A.; Gémes, K.; Frumento, P.; Almondo, G.; Bottai, M.; Friberg, E.; Alexanderson, K. Predicting the duration of sickness absence spells due to back pain: A population-based study from Sweden. Occup. Environ. Med. 2020, 77, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Reho, T.; Atkins, S.; Talola, N.; Sumanen, M.; Viljamaa, M.; Uitti, J. Occasional and persistent frequent attenders and sickness absences in occupational health primary care: A longitudinal study in Finland. BMJ Open 2019, 9, e024980. [Google Scholar] [CrossRef]
- Harkko, J.; Sumanen, H.; Pietiläinen, O.; Piha, K.; Mänty, M.; Lallukka, T.; Rahkonen, O.; Kouvonen, A. Socioeconomic Differences in Occupational Health Service Use and Sickness Absence Due to Mental Disorders: A Register-Based Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, e2064. [Google Scholar] [CrossRef] [PubMed]
- Al-Windi, A.; Elmfeldt, D.; Svärdsudd, K. The influence of sociodemographic characteristics on health care use in a Swedish municipality. Upps. J. Med. Sci. 2004, 109, 33–42. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jyväsjärvi, S.; Keinänen-Kiukaanniemi, S.; Väisänen, E.; Larivaara, P.; Kivelä, S. Frequent attenders in a Finnish health centre: Morbidity and reasons for encounter. Scand. J. Prim. Health Care 1998, 16, 141–148. [Google Scholar] [PubMed]
- Norlund, A.; Ropponen, A.; Alexanderson, K. Multidisciplinary interventions: Review of studies of return to work after rehabilitation for low back pain. J. Rehabil. Med. 2009, 41, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Leinonen, T.; Viikari-Juntura, E.; Husgafvel-Pursiainen, K.; Juvonen-Posti, P.; Laaksonen, M.; Solovieva, S. The effectiveness of vocational rehabilitation on work participation: A propensity score matched analysis using nationwide register data. Scand. J. Work Environ. Health. 2019, 45, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Waddell, G.; Burton, K.; Kendall, N. Vocational Rehabilitation: What Works, for Whom, and When? TSO: London, UK. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/209474/hwwb-vocational-rehabilitation.pdf (accessed on 14 January 2020).
- Gould, R.; Laaksonen, M.; Kivekäs, J.; Ropponen, T.; Kettunen, S.; Hannu, T.; Käppi, I.; Ripatti, P.; Rokkanen, T.; Turtiainen, S. Työkyvyttömyyseläkettä Edeltävät Vaiheet: Asiakirja-Aineistoon Perustuva Tutkimus [Phases Preceding Disability Pension—A Study of Documentation]; Raportteja 6/2014; Eläketurvakeskus: Helsinki, Finland, 2014; (In Finnish, with English Abstract). [Google Scholar]
- Laaksonen, M.; Blomgren, J.; Gould, R. Työkyvyttömyyseläkkeelle siirtyneiden sairauspäiväraha-, kuntoutus- ja työttömyyshistoria. Rekisteripohjainen Tarkastelu [Sickness Absence, Rehabilitation and Unemployment History of Disability Retirees—A Register Study]; Eläketurvakeskuksen raportteja 5/2014; Eläketurvakeskus: Helsinki, Finland, 2014; (In Finnish, with English Abstract). [Google Scholar]
- Gould, R.; Nyman, H. Työkyvyttömyyseläkepäätökset 2000–2011 [Disability Pension Decisions 2000–2011]; Eläketurvakeskuksen Keskustelualoitteita 3/2012; Eläketurvakeskus: Helsinki, Finland, 2012; (In Finnish, with English Abstract). [Google Scholar]
- Juopperi, J.; Lampi, J. Työllisyys Ja Kuntoutus Ennen Työkyvyttömyyseläkepäätöstä [Employent and Rehabilitation before Disability Pension Decision]; Eläketurvakeskuksen Keskustelualoitteita 01/2012; Eläketurvakeskus: Helsinki, Finland, 2012; (In Finnish, with English Abstract). [Google Scholar]
- Perhoniemi, R.; Blomgren, J. Outpatient health care use before and during a long-term sickness absence spell—A register-based follow-up study comparing health care use by the length of sickness absence and transition to disability pension in Finland. BMJ Open 2022, 12, e053948. [Google Scholar] [CrossRef] [PubMed]
- Laaksonen, M.; Rantala, J.; Liukko, J.; Polvinen, A.; Varis, J.; Kesälä, M.; Kuivalainen, S. Individual-and company level determinants of vocational rehabilitation: A multilevel study. Eur. J. Public Health 2019, 29 (Suppl. S4), 498–499. [Google Scholar] [CrossRef]
- Madsen, A. Return to work after first incidence of long-term sickness absence: A 10-year prospective follow-up study identifying labour-market trajectories using sequence analysis. Scand. J. Public Health 2020, 48, 134–143. [Google Scholar] [CrossRef]
- Højsted, J.; Albanb, A.; Hagildc, K.; Eriksens, J. Use of health care system by chronic pain patients who applied for disability pensions. Pain 1999, 82, 275–282. [Google Scholar] [CrossRef]
- Eden, L.; Ejlertsson, G.; Leden, I. Health and health care use among early retirement pensioners with musculoskeletal disorders. Scand. J. Prim. Health Care 1995, 13, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Wallman, T.; Burell, G.; Kullman, S.; Svärdsudd, K. Health care use before and after retirement due to illness. A 13-year population-based follow-up study of prematurely retired men and referents from the general population. Scand. J. Prim. Health Care 2004, 22, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Blomgren, J.; Jäppinen, S. Sosiaali- Ja Terveyspalveluiden Ja Etuuksien Käyttö Oulussa 2013–2018. Tutkimushankkeen Aineiston Yleiskuvaus [Social and Health Care Services and Social Security Benefits in Oulu in 2013–2018; Basic Description of Data]; Kela Working Papers 154/2020; Kela: Helsinki, Finland, 2020; (In Finnish, with English Abstract). [Google Scholar]
- Gjesdal, S.; Bratberg, E. Diagnosis and duration of sickness absence as predictors for disability ension: Results from a three-year, multi-register based and prospective study. Scand. J. Public Health 2003, 31, 246–254. [Google Scholar] [CrossRef]
- Gissler, M.; Haukka, J. Finnish health and social welfare registers in epidemiological research. Nor. Epidemiologi. 2004, 14, 113–120. [Google Scholar]
- Hujanen, T.; Mikkola, H. Työterveyshuollon kustannuskehitys [Cost development of occupational health services]. Suom. Laakaril. 2016, 71, 1537–1540, (In Finnish, with English Abstract). [Google Scholar]
- Räsänen, K.; Heikkinen, J.; Myllykangas, M. Työterveyshuollon sairaanhoitopalvelujen käyttö vaihtelee tarjonnan mukaan [Supply and use of consultation services in occupational health units in the nine biggest cities in Finland]. Suom. Laakaril. 2014, 69, 1325–1330, (In Finnish, with English Summary). [Google Scholar]
- Statistics Finland. Sosioekonominen Asema 1989 [Classification of Socioeconomic Groups 1989]. Available online: https://www.stat.fi/meta/luokitukset/sosioekon_asema/001-1989/index.html (accessed on 1 March 2020).
- Saastamoinen, L.; Aaltonen, K.; Maljanen, T.; Tuominen, U.; Martikainen, J. Health registers as a source of data for research and policy making. Dosis 2012, 28, 199–205. [Google Scholar]
- World Health Organization (WHO). International Statistical Classification of Diseases and Related Health Problems, 10th Revision; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Cameron, A.; Trivedi, P. Microeconometrics Using Stata, Revised Edition; Stata Press: College Station, TX, USA, 2010. [Google Scholar]
- StataCorp. Stata Statistical Software: Release 14, StataCorp LP: College Station, TX, USA, 2015.
- Keskimäki, I.; Tynkkynen, L.; Reissell, E.; Koivusalo, M.; Syrjä, V.; Vuorenkoski, L.; Rechel, B.; Karanikolos, M. Finland: Health system review. Health Syst. Transition 2019, 21, 1–166. [Google Scholar]
- Blomgren, J.; Virta, L. Socioeconomic differences in use of public, occupational and private health care: A register-linkage study of a working-age population in Finland. PLoS ONE 2020, 15, e0231792. [Google Scholar] [CrossRef]
- Regidor, E.; Martınez, D.; Calle, M.; Astasio, P.; Ortega, P.; Domınguez, V. Socioeconomic patterns in the use of public and private health services and equity in health care. BMC Health Serv. Res. 2008, 8, 183. [Google Scholar] [CrossRef] [PubMed]
- Van Doorslaer, E.; Masseria, C.; Koolman, X. Inequalities in access to medical care by income in developed countries. CMAJ 2006, 174, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Øverland, S.; Glozier, N.; Henderson, M.; Mæland, J.; Hotopf, J.; Mykletun, A. Health status before, during and after disability pension award: The Hordaland Health Study (HUSK). Occup. Environ. Med. 2008, 65, 769–773. [Google Scholar] [CrossRef] [PubMed]
- Perhoniemi, R.; Tuulio-Henriksson, A.; Blomgren, J.; Laaksonen, M. Consumption of psychotropic drugs among disability pension applicants with mental disorders: Comparing awarded and rejected applicants in Finland. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Laaksonen, M.; Metsä-Simola, N.; Martikainen, P.; Pietiläinen, O.; Rahkonen, O.; Gould, R.; Partonen, T.; Lahelma, E. Trajectories of mental health before and after old-age and disability retirement: A register-based study on purchases of psychotropic drugs. Scand. J. Work Environ. Health 2012, 38, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Perhoniemi, R.; Blomgren, J.; Laaksonen, M. Determinants of disability pension applications and awarded disability pensions in Finland, 2009 and 2014. Scand. J. Public Health 2020, 48, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Perhoniemi, R.; Blomgren, J.; Laaksonen, M. Sources of income following a rejected disability pension application: A sequence analysis study. Disabil. Rehabil. 2020, 42, 2161–2169. [Google Scholar] [CrossRef] [PubMed]
- Cockerham, W. Social Causes of Health and Disease, 2nd ed.; Polity Press: Cambridge, UK, 2007. [Google Scholar]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Härkäpää, K.; Järvikoski, A.; Gould, R. Motivational orientation of people participating in vocational rehabilitation. J. Occup. Rehabil. 2014, 24, 658–669. [Google Scholar] [CrossRef] [PubMed]
- Gould, R.; Härkäpää, K.; Järvikoski, A. Too Late? The Timing of Vocational Rehabilitation. Int. J. Rehabil. Res. 2009, 32, S64. [Google Scholar]
- Ministry of Social Affairs and Health. Press Release 253/2021. Available online: https://valtioneuvosto.fi/en/-//1271139/progress-made-in-seven-day-cap-on-waiting-times-for-access-to-care (accessed on 2 January 2022).
- Finnish National Board on Research Integrity TENK. The Ethical Principles of Research with Human Participants and Ethical Review in the Human Sciences in Finland; Tutkimuseettisen Neuvottelukunnan Julkaisuja 3/2019; Finnish National Board on Research Integrity: Helsinki, Finland, 2019. [Google Scholar]
| All | Group 1—Transfer to DP after LTSA | Group 2—Mostly Employed after LTSA | Group 3—Some Employment after LTSA | Group 4—Not Employed after LTSA | |
|---|---|---|---|---|---|
| N = 2427 | N = 189 | N = 1639 | N = 169 | N = 430 | |
| % | % | % | % | % | |
| Sex | |||||
| Male | 42.3 | 50.8 | 40.4 | 43.8 | 45.1 |
| Female | 57.7 | 49.2 | 59.6 | 56.2 | 54.9 |
| Age group | |||||
| 18–30 | 20.2 | 2.1 | 16.8 | 39.6 | 33.3 |
| 31–40 | 24.2 | 4.2 | 27.0 | 21.9 | 23.3 |
| 41–50 | 27.0 | 17.5 | 30.1 | 17.8 | 23.3 |
| 51–58 | 28.6 | 76.2 | 26.1 | 20.7 | 20.2 |
| Marital status | |||||
| Married | 46.2 | 44.4 | 51.9 | 37.9 | 28.8 |
| Unmarried | 36.6 | 28.6 | 32.5 | 49.7 | 50.9 |
| Divorced/separated/ widowed | 17.1 | 27.0 | 15.7 | 12.4 | 20.2 |
| Occupational class | |||||
| Upper non-manual employee | 15.6 | 7.9 | 19.8 | 10.7 | 5.1 |
| Lower non-manual employee | 34.2 | 23.3 | 41.5 | 28.4 | 13.7 |
| Manual worker | 22.9 | 24.3 | 24.8 | 24.3 | 14.7 |
| Entrepreneur | 5.3 | 5.8 | 5.1 | 4.7 | 6.1 |
| Other | 21.9 | 38.6 | 8.9 | 32.0 | 60.5 |
| Labour market status at the start of LTSA | |||||
| Employed | 77.3 | 61.4 | 91.7 | 66.3 | 33.3 |
| Unemployed | 17.2 | 33.9 | 6.4 | 21.3 | 49.3 |
| Other | 5.6 | 4.8 | 17.9 | 12.4 | 17.4 |
| Chronic or severe diseases | |||||
| No diseases | 72.4 | 44.4 | 75.4 | 75.7 | 72.1 |
| One disease | 19.3 | 33.9 | 17.9 | 18.9 | 18.4 |
| Multiple diseases | 8.3 | 21.7 | 6.8 | 5.3 | 9.5 |
| LTSA length | |||||
| Under 2 months | 31.1 | 2.1 | 38.6 | 31.4 | 15.1 |
| Two months to 11 months | 48.5 | 28.6 | 53.8 | 53.3 | 34.9 |
| Maximum length (one year) | 20.4 | 69.3 | 7.6 | 15.4 | 50.0 |
| LTSA diagnosis group | |||||
| Mental LTSA | 20.8 | 14.3 | 15.8 | 26.6 | 40.2 |
| Musculoskeletal LTSA | 26.6 | 32.3 | 27.7 | 23.1 | 21.2 |
| Other diagnosis LTSA | 52.7 | 54.4 | 56.5 | 50.3 | 38.6 |
| All | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| M1 | M2 | M3 | ||||
|---|---|---|---|---|---|---|
| Predicted Means | 95% CI | Predicted Means | 95% CI | Predicted Means | 95% CI | |
| The Expected Number of Outpatient Health Care Visits | ||||||
| G1—Transfer to DP after an LTSA | 7.56 | 6.75–8.36 | 7.43 | 6.62–8.23 | 4.87 | 4.36–5.38 |
| G2—Mostly employed after an LTSA | 3.65 | 3.51–3.79 | 3.66 | 3.51–3.81 | 3.79 | 3.65–3.94 |
| G3—Some employment after an LTSA | 3.96 | 3.49–4.43 | 3.94 | 3.47–4.40 | 3.69 | 3.28–4.10 |
| G4—Not employed after an LTSA | 5.57 | 5.18–5.97 | 5.51 | 5.06–5.96 | 4.22 | 3.89–4.55 |
| The Expected Number of Days in Inpatient Care | ||||||
| G1—Transfer to DP after an LTSA | 1.95 | 1.47–2.43 | 1.79 | 1.34–2.23 | 0.84 | 0.62–1.06 |
| G2—Mostly employed after an LTSA | 0.31 | 0.28–0.35 | 0.32 | 0.28–0.36 | 0.29 | 0.26–0.33 |
| G3—Some employment after an LTSA | 0.52 | 0.36–0.68 | 0.49 | 0.34–0.63 | 0.40 | 0.28–0.52 |
| G4—Not employed after an LTSA | 0.77 | 0.63–0.90 | 0.62 | 0.50–0.75 | 0.42 | 0.33–0.51 |
| The Expected Number of Days in Rehabilitation | ||||||
| G1—Transfer to DP after an LTSA | 1.59 | 0.46–2.73 | 1.08 | 0.30–1.87 | 0.40 | 0.12–0.68 |
| G2—Mostly employed after an LTSA | 1.11 | 0.86–1.36 | 1.06 | 0.82–1.30 | 0.76 | 0.60–0.93 |
| G3—Some employment after an LTSA | 2.72 | 0.82–4.63 | 2.41 | 0.65–4.17 | 1.29 | 0.37–2.21 |
| G4—Not employed after an LTSA | 4.42 | 2.42–6.40 | 4.08 | 2.21–5.59 | 2.22 | 1.28–3.16 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perhoniemi, R.; Blomgren, J. Use of Health Services and Rehabilitation before and after the Beginning of Long-Term Sickness Absence—Comparing the Use by Employment and Disability Pension Transition after the Sickness Absence in Finland. Int. J. Environ. Res. Public Health 2022, 19, 4990. https://doi.org/10.3390/ijerph19094990
Perhoniemi R, Blomgren J. Use of Health Services and Rehabilitation before and after the Beginning of Long-Term Sickness Absence—Comparing the Use by Employment and Disability Pension Transition after the Sickness Absence in Finland. International Journal of Environmental Research and Public Health. 2022; 19(9):4990. https://doi.org/10.3390/ijerph19094990
Chicago/Turabian StylePerhoniemi, Riku, and Jenni Blomgren. 2022. "Use of Health Services and Rehabilitation before and after the Beginning of Long-Term Sickness Absence—Comparing the Use by Employment and Disability Pension Transition after the Sickness Absence in Finland" International Journal of Environmental Research and Public Health 19, no. 9: 4990. https://doi.org/10.3390/ijerph19094990
APA StylePerhoniemi, R., & Blomgren, J. (2022). Use of Health Services and Rehabilitation before and after the Beginning of Long-Term Sickness Absence—Comparing the Use by Employment and Disability Pension Transition after the Sickness Absence in Finland. International Journal of Environmental Research and Public Health, 19(9), 4990. https://doi.org/10.3390/ijerph19094990






