Involvement of Non-Parental Caregivers in Obesity Prevention Interventions among 0–3-Year-Old Children: A Scoping Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Study Selection
2.4. Data Analysis
3. Results
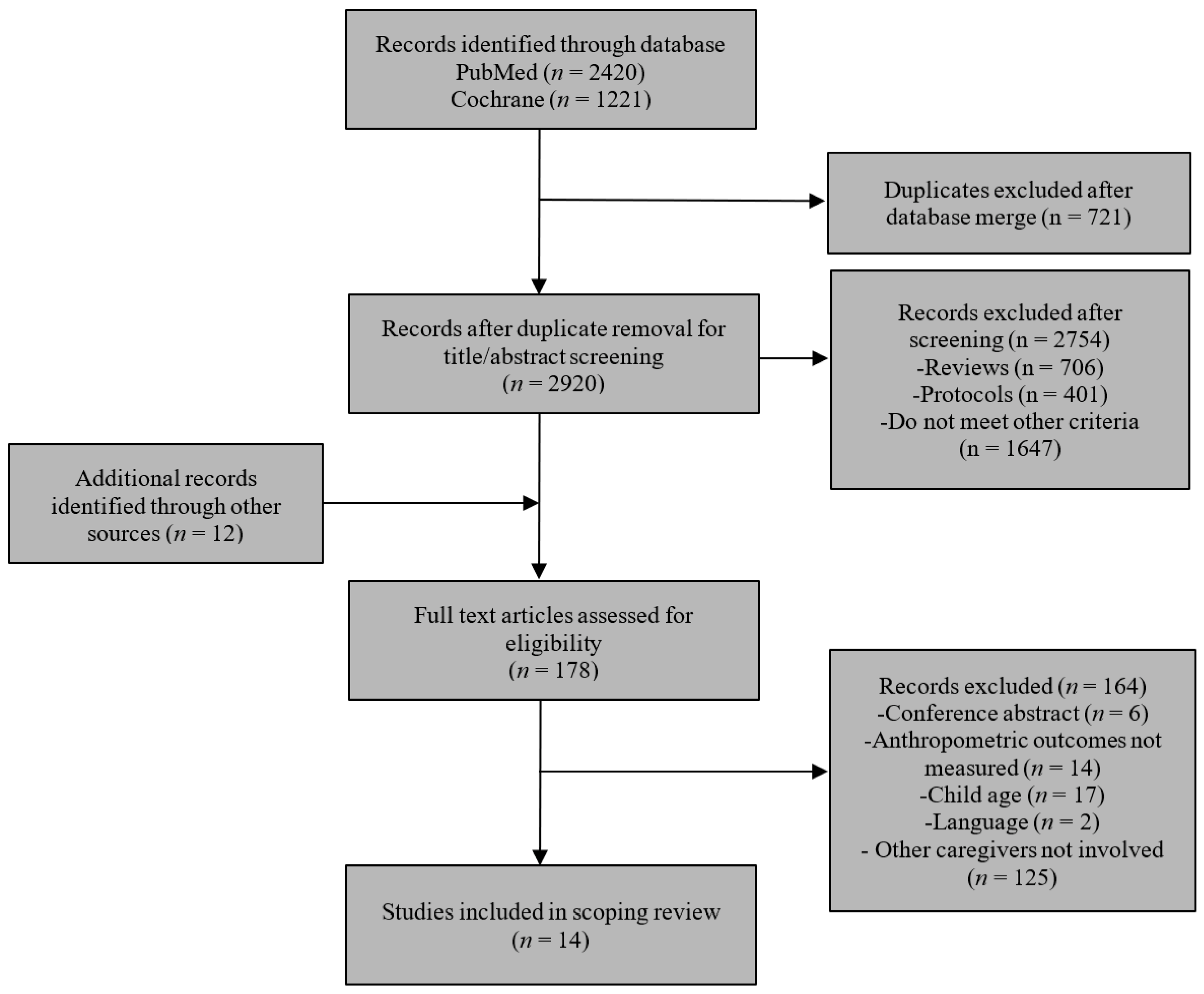
3.1. Study Selection
3.2. Study Characteristics
3.3. Description of the Intervention
3.3.1. Theoretical Framework
3.3.2. Intervention Duration
3.3.3. Sample Characteristics
3.4. Intervention Characteristics and Non-Parental Caregivers’ Description and Role in the Intervention
3.4.1. Interventions That Included Non-Parental Caregivers Post-Hoc
3.4.2. Interventions That Purposely Included Non-Parental Caregivers
3.5. Intervention Settings
3.6. Intervention Activities
3.7. Intervention Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Geserick, M.; Vogel, M.; Gausche, R.; Lipek, T.; Spielau, U.; Keller, E.; Pfaffle, R.; Kiess, W.; Korner, A. Acceleration of BMI in Early Childhood and Risk of Sustained Obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- United Nations Children’s Fund (UNICEF); World Health Organization; International Bank for Reconstruction and Development/The World Bank. Levels and Trends in Child Malnutrition: UNICEF/WHO/The World Bank Group Child Malnutrition Estimates: Key Findings of the 3030 Edition; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 2018, 141, e20173459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sonntag, D. Why Early Prevention of Childhood Obesity Is More Than a Medical Concern: A Health Economic Approach. Ann. Nutr. Metab. 2017, 70, 175–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trasande, L.; Elbel, B. The economic burden placed on healthcare systems by childhood obesity. Expert Rev. Pharm. Outcomes Res. 2012, 12, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.L.; Halvorson, E.E.; Cohen, G.M.; Lazorick, S.; Skelton, J.A. Addressing Childhood Obesity: Opportunities for Prevention. Pediatr. Clin. N. Am. 2015, 62, 1241–1261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mameli, C.; Mazzantini, S.; Zuccotti, G.V. Nutrition in the First 1000 Days: The Origin of Childhood Obesity. Int. J. Environ. Res. Public Health 2016, 13, 838. [Google Scholar] [CrossRef] [Green Version]
- Brown, T.; Moore, T.H.; Hooper, L.; Gao, Y.; Zayegh, A.; Ijaz, S.; Elwenspoek, M.; Foxen, S.C.; Magee, L.; O’Malley, C.; et al. Interventions for preventing obesity in children. Cochrane Database Syst. Rev. 2019, 2019, CD001871. [Google Scholar] [CrossRef] [Green Version]
- Diaz-Rodriguez, M.; Perez-Munoz, C.; Lendinez-de la Cruz, J.M.; Fernandez-Gutierrez, M.; Bas-Sarmiento, P.; Ferriz-Mas, B.C. Effectiveness of a Multifactorial Intervention in the First 1000 Days of Life to Prevent Obesity and Overweight in Childhood: Study Protocol. Int. J. Environ. Res. Public Health 2020, 17, 2239. [Google Scholar] [CrossRef] [Green Version]
- Hennessy, M.; Heary, C.; Laws, R.; Van Rhoon, L.; Toomey, E.; Wolstenholme, H.; Byrne, M. Health professional-delivered obesity prevention interventions during the first 1000 days: A systematic review of external validity reporting. HRB Open Res. 2019, 2, 14. [Google Scholar] [CrossRef]
- Savage, J.S.; Hohman, E.E.; Marini, M.E.; Shelly, A.; Paul, I.M.; Birch, L.L. INSIGHT responsive parenting intervention and infant feeding practices: Randomized clinical trial. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 64. [Google Scholar] [CrossRef] [Green Version]
- Blake-Lamb, T.L.; Locks, L.M.; Perkins, M.E.; Woo Baidal, J.A.; Cheng, E.R.; Taveras, E.M. Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review. Am. J. Prev. Med. 2016, 50, 780–789. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Booth, A.E. Immigration and the Family: Research and Policy on U.S. Immigrants; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 1997. [Google Scholar]
- Wang, S.; Guendelman, S.; Harley, K.; Eskenazi, B. When Fathers are Perceived to Share in the Maternal Decision to Breastfeed: Outcomes from the Infant Feeding Practices Study II. Matern. Child Health J. 2018, 22, 1676–1684. [Google Scholar] [CrossRef] [PubMed]
- Cheng, E.R.; Taveras, E.M.; Hawkins, S.S. Paternal Acculturation and Maternal Health Behaviors: Influence of Father’s Ethnicity and Place of Birth. J. Women’s Health 2018, 27, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Pulgaron, E.R.; Patino-Fernandez, A.M.; Sanchez, J.; Carrillo, A.; Delamater, A.M. Hispanic children and the obesity epidemic: Exploring the role of abuelas. Fam. Syst. Health 2013, 31, 274–279. [Google Scholar] [CrossRef] [Green Version]
- Morgan, E.H.; Schoonees, A.; Sriram, U.; Faure, M.; Seguin-Fowler, R.A. Caregiver involvement in interventions for improving children’s dietary intake and physical activity behaviors. Cochrane Database Syst. Rev. 2020, 2020, CD012547. [Google Scholar] [CrossRef] [Green Version]
- An, R.; Xiang, X.; Xu, N.; Shen, J. Influence of Grandparental Child Care on Childhood Obesity: A Systematic Review and Meta-Analysis. Child. Obes. 2020, 16, 141–153. [Google Scholar] [CrossRef] [Green Version]
- Eli, K.; Howell, K.; Fisher, P.A.; Nowicka, P. “A little on the heavy side”: A qualitative analysis of parents’ and grandparents’ perceptions of preschoolers’ body weights. BMJ Open 2014, 4, e006609. [Google Scholar] [CrossRef] [Green Version]
- Benjamin, S.E.; Rifas-Shiman, S.L.; Taveras, E.M.; Haines, J.; Finkelstein, J.; Kleinman, K.; Gillman, M.W. Early Child Care and Adiposity at Ages 1 and 3 Years. Pediatrics 2009, 124, 555–562. [Google Scholar] [CrossRef] [Green Version]
- Gubbels, J.S.; Kremers, S.P.J.; Stafleu, A.; Dagnelie, P.C.; de Vries, N.K.; van Buuren, S.; Thijs, C. Child-care use and the association with body mass index and overweight in children from 7 months to 2 years of age. Int. J. Obes. 2010, 34, 1480–1486. [Google Scholar] [CrossRef] [Green Version]
- Pearce, A.; Li, L.; Abbas, J.; Ferguson, B.; Graham, H.; Law, C.; Millennium Cohort Study Child Health Group. Is childcare associated with the risk of overweight and obesity in the early years? Findings from the UK Millennium Cohort Study. Int. J. Obes. 2010, 34, 1160–1168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costa, S.; Adams, J.; Gonzalez-Nahm, S.; Benjamin Neelon, S.E. Childcare in Infancy and Later Obesity: A Narrative Review of Longitudinal Studies. Curr. Pediatr. Rep. 2017, 5, 118–131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLean, N.; Griffin, S.; Toney, K.; Hardeman, W. Family involvement in weight control, weight maintenance and weight-loss interventions: A systematic review of randomised trials. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 987–1005. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, M. School-based interventions for childhood and adolescent obesity. Obes. Rev. 2006, 7, 261–269. [Google Scholar] [CrossRef]
- Neelon, S.E.B.; Ostbye, T.; Bennett, G.G.; Kravitz, R.M.; Clancy, S.M.; Stroo, M.; Iversen, E.; Hoyo, C. Cohort profile for the Nurture Observational Study examining associations of multiple caregivers on infant growth in the Southeastern USA. BMJ Open 2017, 7, e013939. [Google Scholar] [CrossRef] [Green Version]
- Perrin, E.M.; Rothman, R.L.; Sanders, L.M.; Skinner, A.C.; Eden, S.K.; Shintani, A.; Throop, E.M.; Yin, H.S. Racial and ethnic differences associated with feeding- and activity-related behaviors in infants. Pediatrics 2014, 133, e857–e867. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Daudt, H.M.; van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef] [Green Version]
- Grummon, A.H.; Cabana, M.D.; Hecht, A.A.; Alkon, A.; McCulloch, C.E.; Brindis, C.D.; Patel, A.I. Effects of a Multi-Pronged Beverage Intervention on Young Children’s Beverage Intake and Weight: A Cluster-Randomized Pilot Study. Public Health Nutr. 2019, 22, 2856–2867. [Google Scholar] [CrossRef] [Green Version]
- Tomayko, E.J.; Prince, R.J.; Cronin, K.A.; Adams, A.K. The Healthy Children, Strong Families intervention promotes improvements in nutrition, activity and body weight in American Indian families with young children. Public Health Nutr. 2016, 19, 2850–2859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wasser, H.M.; Thompson, A.L.; Suchindran, C.M.; Goldman, B.D.; Hodges, E.A.; Heinig, M.J.; Bentley, M.E. Home-based intervention for non-Hispanic black families finds no significant difference in infant size or growth: Results from the Mothers & Others randomized controlled trial. BMC Pediatr. 2020, 20, 385. [Google Scholar] [CrossRef]
- Jastreboff, A.M.; Chaplin, T.M.; Finnie, S.; Savoye, M.; Stults-Kolehmainen, M.; Silverman, W.K.; Sinha, R. Preventing Childhood Obesity Through a Mindfulness-Based Parent Stress Intervention: A Randomized Pilot Study. J. Pediatr. 2018, 202, 136–142.e1. [Google Scholar] [CrossRef] [PubMed]
- Tomayko, E.J.; Prince, R.J.; Cronin, K.A.; Kim, K.; Parker, T.; Adams, A.K. The Healthy Children, Strong Families 2 (HCSF2) Randomized Controlled Trial Improved Healthy Behaviors in American Indian Families with Young Children. Curr. Dev. Nutr. 2019, 3, 53–62. [Google Scholar] [CrossRef]
- Stookey, J.D.; Evans, J.; Chan, C.; Tao-Lew, L.; Arana, T.; Arthur, S. Healthy apple program to support child care centers to alter nutrition and physical activity practices and improve child weight: A cluster randomized trial. BMC Public Health 2017, 17, 965. [Google Scholar] [CrossRef] [Green Version]
- Haines, J.; Rifas-Shiman, S.L.; Gross, D.; McDonald, J.; Kleinman, K.; Gillman, M.W. Randomized trial of an obesity prevention intervention that embeds weight-related messages within a general parenting program. Obesity 2015, 24, 191–199. [Google Scholar] [CrossRef]
- Ward, D.S.; Vaughn, A.E.; Burney, R.V.; Hales, D.; Benjamin-Neelon, S.E.; Tovar, A.; Ostbye, T. Keys to healthy family child care homes: Results from a cluster randomized trial. Prev. Med. 2020, 132, 105974. [Google Scholar] [CrossRef]
- Natale, R.A.; Lopez-Mitnik, G.; Uhlhorn, S.B.; Asfour, L.; Messiah, S.E. Effect of a Child Care Center-Based Obesity Prevention Program on Body Mass Index and Nutrition Practices Among Preschool-Aged Children. Health Promot. Pract. 2012, 15, 695–705. [Google Scholar] [CrossRef]
- Natale, R.A.; Messiah, S.E.; Mitnik, G.; Asfour, L.; Englebert, N.E.; Arheart, K.L. Obesity Prevention Program in Childcare Centers: Two-Year Follow-Up. Am. J. Health Promot. 2017, 31, 502–510. [Google Scholar] [CrossRef]
- Hammersley, M.L.; Okely, A.D.; Batterham, M.J.; Jones, R.A. An Internet-Based Childhood Obesity Prevention Program (Time2bHealthy) for Parents of Preschool-Aged Children: Randomized Controlled Trial. J. Med. Internet Res. 2019, 21, e11964. [Google Scholar] [CrossRef] [Green Version]
- Yoong, S.L.; Grady, A.; Wiggers, J.H.; Stacey, F.G.; Rissel, C.; Flood, V.; Finch, M.; Wyse, R.; Sutherland, R.; Salajan, D.; et al. Child-level evaluation of a web-based intervention to improve dietary guideline implementation in childcare centers: A cluster-randomized controlled trial. Am. J. Clin. Nutr. 2020, 111, 854–863. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, G.; Demirli Caylan, N.; Karacan, C.D. An intervention to preschool children for reducing screen time: A randomized controlled trial. Child Care Health Dev. 2015, 41, 443–449. [Google Scholar] [CrossRef] [PubMed]
- van de Kolk, I.; Gerards, S.; Harms, L.S.E.; Kremers, S.P.J.; Gubbels, J.S. The Effects of a Comprehensive, Integrated Obesity Prevention Intervention Approach (SuperFIT) on Children’s Physical Activity, Sedentary Behavior, and BMI Z-Score. Int. J. Environ. Res. Public Health 2019, 16, 5016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McLeish, J.; Redshaw, M. Mothers’ accounts of the impact on emotional wellbeing of organised peer support in pregnancy and early parenthood: A qualitative study. BMC Pregnancy Childbirth 2017, 17, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanchez-Flack, J.C.; Herman, A.; Buscemi, J.; Kong, A.; Bains, A.; Fitzgibbon, M.L. A systematic review of the implementation of obesity prevention interventions in early childcare and education settings using the RE-AIM framework. Transl. Behav. Med. 2020, 10, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Yoong, S.L.; Lum, M.; Jones, J.; Kerr, E.; Falkiner, M.; Delaney, T.; McCrabb, S.; Chai, L.K.; Seward, K.; Grady, A. A systematic review of interventions to improve the dietary intake, physical activity and weight status of children attending family day care services. Public Health Nutr. 2020, 23, 2211–2220. [Google Scholar] [CrossRef]
- Wang, Y.; Cai, L.; Wu, Y.; Wilson, R.F.; Weston, C.; Fawole, O.; Bleich, S.N.; Cheskin, L.J.; Showell, N.N.; Lau, B.D.; et al. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obes. Rev. 2015, 16, 547–565. [Google Scholar] [CrossRef]
- Tomayko, E.J.; Mosso, K.L.; Cronin, K.A.; Carmichael, L.; Kim, K.; Parker, T.; Yaroch, A.L.; Adams, A.K. Household food insecurity and dietary patterns in rural and urban American Indian families with young children. BMC Public Health 2017, 17, 611. [Google Scholar] [CrossRef]
- Grossman, D.C.; Bibbins-Domingo, K.; Curry, S.J.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W., Jr.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 317, 2417–2426. [Google Scholar] [CrossRef]
- Paul, I.M.; Savage, J.S.; Anzman-Frasca, S.; Marini, M.E.; Beiler, J.S.; Hess, L.B.; Loken, E.; Birch, L.L. Effect of a Responsive Parenting Educational Intervention on Childhood Weight Outcomes at 3 Years of Age the INSIGHT Randomized Clinical Trial. JAMA 2018, 320, 461–468. [Google Scholar] [CrossRef] [Green Version]
- Daniels, L.A.; Mallan, K.M.; Battistutta, D.; Nicholson, J.M.; Perry, R.; Magarey, A. Evaluation of an intervention to promote protective infant feeding practices to prevent childhood obesity: Outcomes of the NOURISH RCT at 14 months of age and 6 months post the first of two intervention modules. Int. J. Obes. 2012, 36, 1292–1298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weihrauch-Bluher, S.; Wiegand, S. Risk Factors and Implications of Childhood Obesity. Curr. Obes. Rep. 2018, 7, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Roberto, C.A.; Swinburn, B.; Hawkes, C.; Huang, T.T.; Costa, S.A.; Ashe, M.; Zwicker, L.; Cawley, J.H.; Brownell, K.D. Patchy progress on obesity prevention: Emerging examples, entrenched barriers, and new thinking. Lancet 2015, 385, 2400–2409. [Google Scholar] [CrossRef]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [Green Version]
- Ward, D.S.; Welker, E.; Choate, A.; Henderson, K.E.; Lott, M.; Tovar, A.; Wilson, A.; Sallis, J.F. Strength of obesity prevention interventions in early care and education settings: A systematic review. Prev. Med. 2017, 95, S37–S52. [Google Scholar] [CrossRef]
- Zimmerman, E. Researching Health Together: Engaging Patients and Stakeholders, from Topic Identification to Policy Change; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2021. [Google Scholar]
- Cheney, A.M.; Nieri, T.; Ramirez Zarate, A.; Garcia, G.; Vaca, L.; Valencia, E.; Versteeg, C.; Molina, A.; Castillo, M.; Tovar, A. Grow well/Crecer bien: A protocol for research on infant feeding practices in low-income families. BMC Public Health 2020, 20, 1431. [Google Scholar] [CrossRef]
- Kid City USA. Early Childhood Education: When Do Kids Start Preschool? A Comprehensive Guide. Available online: https://kidcityusa.com/early-childhood-education/when-do-kids-start-preschool-a-comprehensive-guide (accessed on 3 November 2021).
| Component | Search String |
|---|---|
| Population | (infant) OR (child, preschool) OR (infant, newborn) AND (caregivers) OR (“non-parent caregivers”) OR (“non parental”) OR (sibling) OR (“sibling caregivers”) OR (grandparent) OR (“grandparent caregivers”) OR (family) OR (“family caregivers”) OR (caretakers) OR (“secondary caregivers”) OR (parents) OR (father) OR (mother) OR (“non-maternal caregivers”) OR (“non-parental caregivers”) |
| Intervention | (“nutrition intervention”) OR (“nutrition education”) OR (“obesity interventions”) OR (“nutritional intervention”) OR (“obesity education”) OR (“obesity prevention education”) OR (“obesity prevention”) OR (“infant nutrition education”) OR (“infant feeding”) OR (“parent feeding practices”)) OR (“parental feeding practices”) OR (child nutrition sciences) OR (infant nutritional physiological phenomena) OR (health education) |
| Outcome | (obesity) OR (“infant growth”) OR (pediatric obesity) OR (nutritional status) |
| Authors | Country | Research Question | Study Design | Sample Size | Sample Design | Infant Age |
|---|---|---|---|---|---|---|
| Natale et al. (2014) | U.S. | Is an obesity prevention intervention conducted in CCs effective in improving children’s diet, PA and weight? | RCT | 307 adult—child dyads, teachers in 8 CCs | CCs that served low-income, ethnically diverse families, and the center teachers. | 2–5 years |
| Yilmaz et al. (2015) | Turkey | Does an intervention applied at the health maintenance visit reduce screen time, meals eaten in front of television, child’s aggressive behaviors and improve BMI z-score? | RCT | 363 adult–child dyads | Parents who brought their children to the well-childcare visits in a hospital. No inclusion or exclusion criteria were stated in the paper. | 2–6 years |
| Tomayko et al. (2016) | U.S. | Is an obesity prevention toolkit more effective when delivered in-home vs. mailed to impact child and adult weight status, nutrition and PA behaviors, and self-efficacy? | RCT | 150 adult–child dyads | Children 2–5 years old who lived with one primary caregiver; without major physical or behavioral conditions. | 2–5 years |
| Haines et al. (2016) | U.S. | Does an obesity prevention intervention, embedded within a parenting program, result in smaller increases in children’s BMI and improves weight-related behaviors? | RCT | 112 adult–child dyads | Excluded parents unable to respond to interviews in English or Spanish, and children with severe health conditions. | 2–5 years |
| Stookey et al. (2017) | U.S. | Does the incorporation of Happy Apple Program into routine public health nursing services improve the nutrition and PA best practices in childcare, child BMI percentile and z-score? | Cluster RCT | 43 CCs; 791–945 children annually | CCs that participated in CCHP nutrition screenings in 2011–2012 except those with funding from Head Start, the school or community college district. | 2–5 years |
| Natale et al. (2017) | U.S. | Does an obesity prevention intervention conducted in childcare with ethnically diverse children improve child weight and diet? | RCT | 1211 children in 28 CC | 28 CCs that served low-income, ethnically diverse families, and teachers. | 2–5 years |
| Tomayko et al. (2019) | U.S. | Does a healthy lifestyle promotion/obesity prevention program improve health behaviors, and weight status in AI children? | RCT | 450 adult–child dyads | Adults with a dependent child from 4 tribal reservations and 1 urban site; with a cell phone; they were not required to be AI, and the adult did not have to be the biological parent of the child. | 2–5 years |
| Jastreboff et al. (2018) | U.S. | Does a novel mindfulness-based parent stress intervention decrease risk of early childhood obesity in low-income families? | Cluster RCT | 42 adult–child dyads | Low-income parents, with a child between 2–5 years-old, with high levels of perceived stress. | 2–5 years |
| Hammersley et al. (2019) | Australia | Does a parent-focused, internet-based lifestyle program aimed to overweight children or at risk to becoming overweight, improve child BMI, obesity-related behaviors, parent modeling and self-efficacy? | RCT | 86 adult–child dyads | Children were at or above the WHO fiftieth percentile for BMI for their age and sex; they were excluded if they had a medical condition that affected weight. | 2–5 years |
| Grummon et al., 2019) | U.S. | Does a multi-pronged pilot intervention promoting healthier beverage consumption improve children’s beverage consumption and weight status? | Cluster RCT | 154 adult–child dyads and staff from 4 CCs | Licensed CCs that participated in CACFP and served English or Spanish-speaking families. | 2–5 years |
| Van de Kolk et al. (2019) | The Netherlands | Does a comprehensive intervention embed in ECE improve child PA, sedentary behavior, and BMI z-score? | Quasi-experimental | 191 parent–child dyads from 21 preschools | Preschools in neighborhoods with low SES were eligible, with Dutch speaking parents. | 2–4 years |
| Wasser et al. (2020) | U.S. | Does a home-based intervention for NHB women and their study partners improve infant size and growth? | RCT | 430 women their study partner and child | NBH, pregnant women, who spoke English, between 18 and 39 years, with a singleton pregnancy. | 0–12 months |
| Yoong et al. (2020) | Australia | Does a web-based menu-planning tool program that implements dietary guidelines in CCs improve children’s diet, BMI z scores and child health-related quality of life? | Cluster RCT | 483 children in 35 CCs | CCs were responsible of the menu planning decisions with a menu planner, provided at least 1 meal and 2 snacks to children. | 2–6 years |
| Ward et al. (2020) | U.S. | Does a FCCH-based intervention improve children’s diet and PA? | Cluster RCT | 496 children in 166 FCCH | Convenience sample of FCCHs, that provided at least one meal and one snack. | 1.5–4 years |
| Authors/Intervention Name | Framework or Theoretical Model | Intervention | Sample Characteristics | Main Results |
|---|---|---|---|---|
| Natale et al. (2014) Healthy Inside—Healthy Outside (HI-HO) | SEM | 6-month, culturally appropriate intervention that implemented a nutrition and PA curriculum. CCs teachers received two trainings about healthy menus, and child nutrition; parents received information about nutrition and PA, and at home activities once a month by a registered dietitian; the centers incorporated policies. | Majority of families identified as Hispanic, and 35% were Spanish-speaking. Providers were also ethnically diverse. | No significant changes in PA, weight z-score, height z-score; however, BMI z-score was negatively correlated with their participation in home activities, and 97% of the children with normal weight remained with normal weight. Children in the intervention consumed more F/V, 1% milk, and less juice and junk food. |
| Yilmaz et al. (2015) Name was not specified | SCT | Conducted by health care practitioners during maintenance visits in a hospital; non-parental caregivers received home visits. Consisted of four intervention components, with a total duration of 6 weeks. Included printed materials, interactive CDs, and a counseling call, which addressed consequences of increased screen time, and alternatives to watching TV. | Ethnicity and race were not presented in the results. Majority of families had an annual income between $10,000–20,000. | In the intervention group vs. control, there was a significant reduction in meals consumed in front of a screen, screen time of children, parents, and non-parental caregivers, and ins aggressive behaviors. There were no significant differences in BMI z-scores. |
| Tomayko et al. (2016) Healthy Children, Strong Families (HCSF) | CBPR | A two-year, family-based intervention, that included a healthy lifestyle toolkit delivered by in-home mentoring or by mail (control). Designed with AI community input. The 1st year included monthly home visits (60 min) by community mentors. Lessons targeted lifestyle behavioral changes: F/V, sweetened drinks, sweets intake, PA, and TV viewing. The 2nd year included newsletters and group meetings. | More than 90% of the participants were AI. Most families (75.9%) received WIC benefits. | No significant effect of the toolkit delivery method was found. When control and intervention groups were combined, there was a significant decrease in child BMI percentile and TV use, and an increase in F/V intake and adult-self efficacy. No change in adult BMI was observed. |
| Haines et al. (2016) Parents and TOTS Together | Social contextual framework | Family-based intervention, adapted from the Chicago Parent Program. Consisted of 9 weekly group sessions, 2 h each, delivered by trained facilitators, at a community health center. Included information about parental roles in promoting healthy nutrition, PA, and weight related behaviors. Parents were given educational materials to share with other caregivers. | Children were primarily Hispanic (59%) or Black/African American (22%). Majority of participants (87%) had annual household incomes at or be ≤$50,000. | No significant differences in BMI. Parents in the intervention vs. control decreased restrictive feeding practices relative. Similar changes in children’s weight-related behaviors were observed in the intervention and control parents. |
| Stookey et al. (2017) Healthy Apple Program (HAP) | Not reported | Consisted of the integration of HAP into CCHP. Delivered by CCHP public health nurses or health workers in CCs. The HAP portion adapted resources from the University of North Carolina Nutrition and Physical Activity Self-Assessment for Child Care program and provided CCs providers with PA and nutrition resources. Each CC received 16 h of training and support. | Providers at CCs that serve low-income children. Race-ethnic data were not available. | In the HAP + CCHP program, there was a significant increase in the proportion of children exposed to nutrition and PA best practices, and a significant reduction in child BMI. |
| Natale et al. (2017) Healthy Caregivers—Healthy Children (HC2) | SCT | 12-month, CC-based, culturally sensitive obesity prevention, intervention aimed to low income, diverse children. Curriculums addressed nutrition and PA. The policy curriculum included the implementation of policies. The parent/teacher curriculum included joint bimonthly meetings and additional trainings. The child curriculum included weekly lessons and support for teachers from curriculum specialists. | Majority of families identified as Hispanic or African American and were Spanish-speaking. Providers were also ethnically diverse. | Children in intervention vs. control had a lesser increase of BMI percentile. No significant changes in F/V and unhealthy food consumption. |
| Tomayko et al. (2019) Healthy Children, Strong Families 2 (HCSF2) | CBPR | Home-delivered, aimed to improve health behaviors. For a year, monthly toolkits were sent to families, with information and supportive items (measuring cups, games). Social media consisted of 2 weekly text messages and a Facebook group. | Majority of participants (>84.9%) were AI/AN. All families, reported income <$20,000/year. | Significant improvements in adult and child diet patterns, adult F/V intake, adult PA and self-efficacy for health behavior, home nutrition environment. No significant changes in adult BMI or child BMI z-score, child PA, adult stress, adult/child sleep, and screen time. |
| Jastreboff et al. (2018) Name was not specified | Not reported | Behavioral intervention delivered by a therapist trained in mindfulness and cognitive behavior therapy. Consisted of 8 weekly group sessions with other parents and included nutrition and PA counseling, goal setting, stress reduction techniques, and mindful eating. | Majority of parents (71%) and children (63%) were low-income were non-white (63%). | In the control group, there was a significant increase in child BMI-percentile. Intervention vs. control participants significantly improved parental emotional eating ratings. No significant differences in PA. |
| Hammersley et al. (2019) Time2bHealthy | SCT | Web-based intervention, consisted of 6 modules (introduction, nutrition, PA, screen time, sleep) delivered for 11 weeks. Each module included reading materials, videos, etc. Dietitian provided feedback to improve their goals. Participants could join a Facebook group. | 3.5% of the children in the study were Australian-Aboriginal. | No significant differences in the BMI, PA, screen time, or sleep outcomes. Intervention vs. control group showed a reduced intake of discretionary food, and parents improved self-efficacy and child feeding pressure to eat. |
| Grummon et al. (2019) Name was not specified | SEM | Multi-level,12- week intervention aimed to improve beverage intake. Delivered via CC by research assistants and childcare teachers. Targeted children, parents, and CC staff. Included environmental changes, implementation of rules and policies, and educational activities for parents. Children participated in activities at childcare. | Predominantly Hispanic/Latino and low-income, with two-thirds of parents reporting annual household income of $30,000 or less. | Children reduced their consumption of less-healthy beverages and increased their consumption of healthier beverages. Children’s likelihood of being overweight decreased by 3 percentage points. |
| Van de Kolk et al. (2019) SuperFIT | SEM and systems theory | 12-mo implementation intervention to connect strategies between settings. Delivered by health promotion experts. The preschool component targeted the sociocultural environment, such as PA and nutrition practices of teachers and physical environment. The family component addressed the sociocultural, political, and economic environment. The community component aimed to increase connections between organizations involved in PA and nutrition. Children could participate in the preschool and family components (full intervention) or in the preschool component (partial intervention). | Childcare in low-income neighborhoods, families, caregivers, and teachers. Ethnicity/race information was not presented. | No significant changes in BMI z-score in overall PA levels. Sedentary behavior decreased more in the full intervention group. |
| Wasser et al. (2020) Mothers & Others | Not reported | Home-based, responsive feeding intervention delivered by trained peer educators. Consisted of 8 visits during pregnancy and after birth, an information toolkit, and four newsletters. Included information about breastfeeding, responsive feeding style, complementary feeding, TV/media, and infant sleep. Women selected a study partner to participate, and they received their own set of materials. | NHB mothers, the majority were low income. Data about partners were not presented. | No significant differences in infant growth. |
| Yoong et al. (2020) feedAustralia | Theoretical Domains Framework | Web-based, 12-month intervention designed to address barriers to guideline implementation. It included the use of a web-based menu-planning program, educational resources reminder to increase compliance), training, and support by health promotion officer). | CCs from different economic backgrounds. Ethnicity/race was not presented. | In the intervention group vs. control, there was a significant increase in mean child consumption of fruit and dairy and a reduction in consumption of discretionary foods. No significant differences were observed in diet quality, BMI z-scores, or child health-related quality of life. |
| Ward et al. (2020) Keys to a Healthy Family Child Care Homes | SCT and SDT | 9-month intervention to improve children’s diet and PA. Delivered by health coaches through a workshop, a home visit, and telephone calls/emails. It addressed the children intrapersonal and interpersonal relations, and FCCH organizational level. The intervention included three modules (3 months each) regarding FCCH provider health, FCCH environment and FCCH business practice. | 63.3% of the children and 74.1% of providers participating were African American. Half the providers had an associated degree or college credit. | Children in the intervention group significantly improved their diet quality, no changes were observed in BMI, BMI percentile and PA. Providers improved their diet quality and some components of the FCCH environment. |
| Authors/Intervention Name | Non-Parental Caregivers Included in the Intervention | Non-Parental Caregivers’ Characteristics | |||
|---|---|---|---|---|---|
| Other Family Members | Childcare Staff | Other Non-Relatives | Others/Unspecified | ||
| Natale et al. (2014) Healthy Inside—Healthy Outside (HI-HO) | X | Intervention was developed to include CC teachers in childcare centers with low-income, mainly Latino children. | |||
| Yilmaz et al. (2015) Name was not specified | X | Unspecified | |||
| Tomayko et al. (2016) Healthy Children, Strong Families (HCSF) | X | X | Intervention was developed to include any primary caregiver that lived with the child at home: 85% of the participating caregivers were the mother of the child, 2% were the father and 12.7% were the grandparent/other. | ||
| Haines et al. (2016) Parents and TOTS Together | X | X | Intervention was developed to include parents as the primary participants, but other adults participated: 92.9% were the mothers of the children, 5.4% were the fathers, and 1.8% were stepmother/other. | ||
| Stookey et al. (2017) Healthy Apple Program | X | Intervention was developed to include childcare providers. Unspecified providers’ characteristics | |||
| Natale et al. (2017) Healthy Caregivers—Healthy Children (HC2) | X | Intervention was developed to include CC teachers in childcare centers with low-income, mainly Latino children. | |||
| Tomayko et al. (2019) Healthy Children, Strong Families 2 | X | Intervention was developed to include any adult primary caregiver and did not have to be the biological parent of the child. Adults in the intervention were on average 31.4 ± 7.8 years old, and they were mostly women (94.7%). Information about the relationship between the adults and the children was not provided. | |||
| Jastreboff et al. (2018) Name was not specified | X | Intervention was developed for parents as the primary participants, but other adults participated: 95% (n = 59) were biological mothers, one was the biological father, one was an adoptive mother, and one was a grandmother. | |||
| Hammersley et al. (2019) Time2bHealthy | X | X | Intervention was developed for parents as the primary participants, but other adults participated: 93% of the adults were the children’s mother, 5% were the father, and 2% were other. | ||
| Grummon et al. (2019) Name was not specified | X | Intervention was developed to include childcare providers. Unspecified providers’ characteristics | |||
| Van de Kolk et al. (2019) SuperFIT | X | Intervention was developed to include childcare providers. Unspecified providers’ characteristics | |||
| Wasser et al. (2020) Mothers & Others | X | X | X | Intervention included a study partner selected by the mother. Approximately, half of the study partners (54.6%) were the infant’s father, 27.5% were the infant’s grandmother, 11.5% were another type of relative (infant’s aunt, cousin, grandfather, sister or unspecified), and 6.4% were not non-relatives (mother’s roommate, infant’s godmother, or unspecified). | |
| Yoong et al. (2020) feedAustralia | X | Intervention was developed to include childcare providers. Unspecified providers’ characteristics | |||
| Ward et al. (2020) Keys to a Healthy Family Child Care Homes | X | Intervention was developed to include providers in FCCH. Most of them were female, African American (74.1%). | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramirez, A.; Tovar, A.; Garcia, G.; Nieri, T.; Hernandez, S.; Sastre, M.; Cheney, A.M. Involvement of Non-Parental Caregivers in Obesity Prevention Interventions among 0–3-Year-Old Children: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 4910. https://doi.org/10.3390/ijerph19084910
Ramirez A, Tovar A, Garcia G, Nieri T, Hernandez S, Sastre M, Cheney AM. Involvement of Non-Parental Caregivers in Obesity Prevention Interventions among 0–3-Year-Old Children: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(8):4910. https://doi.org/10.3390/ijerph19084910
Chicago/Turabian StyleRamirez, Andrea, Alison Tovar, Gretel Garcia, Tanya Nieri, Stephanie Hernandez, Myrna Sastre, and Ann M. Cheney. 2022. "Involvement of Non-Parental Caregivers in Obesity Prevention Interventions among 0–3-Year-Old Children: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 8: 4910. https://doi.org/10.3390/ijerph19084910
APA StyleRamirez, A., Tovar, A., Garcia, G., Nieri, T., Hernandez, S., Sastre, M., & Cheney, A. M. (2022). Involvement of Non-Parental Caregivers in Obesity Prevention Interventions among 0–3-Year-Old Children: A Scoping Review. International Journal of Environmental Research and Public Health, 19(8), 4910. https://doi.org/10.3390/ijerph19084910






