Association between Healthy Eating Index and Mental Health in Middle-Aged Adults Based on Household Size in Korea
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. General Measurements
2.3. Mental Health Behavior Measures
2.3.1. Subjective Health Status
2.3.2. Stress Perception
2.3.3. Depression
2.3.4. Health-Related Quality of Life
2.4. Dietary Intake Measures
2.4.1. Dietary Intake
2.4.2. KHEI
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of Participants
3.2. Mental Health-Related Outcomes of Participants
3.3. Daily Nutrient Intake of Participants
3.4. KHEI of Participants
3.5. Relationship between Household Size and Mental Health-Related Outcomes
3.6. Relationship between KHEI and Mental Health-Related Outcomes
4. Discussion
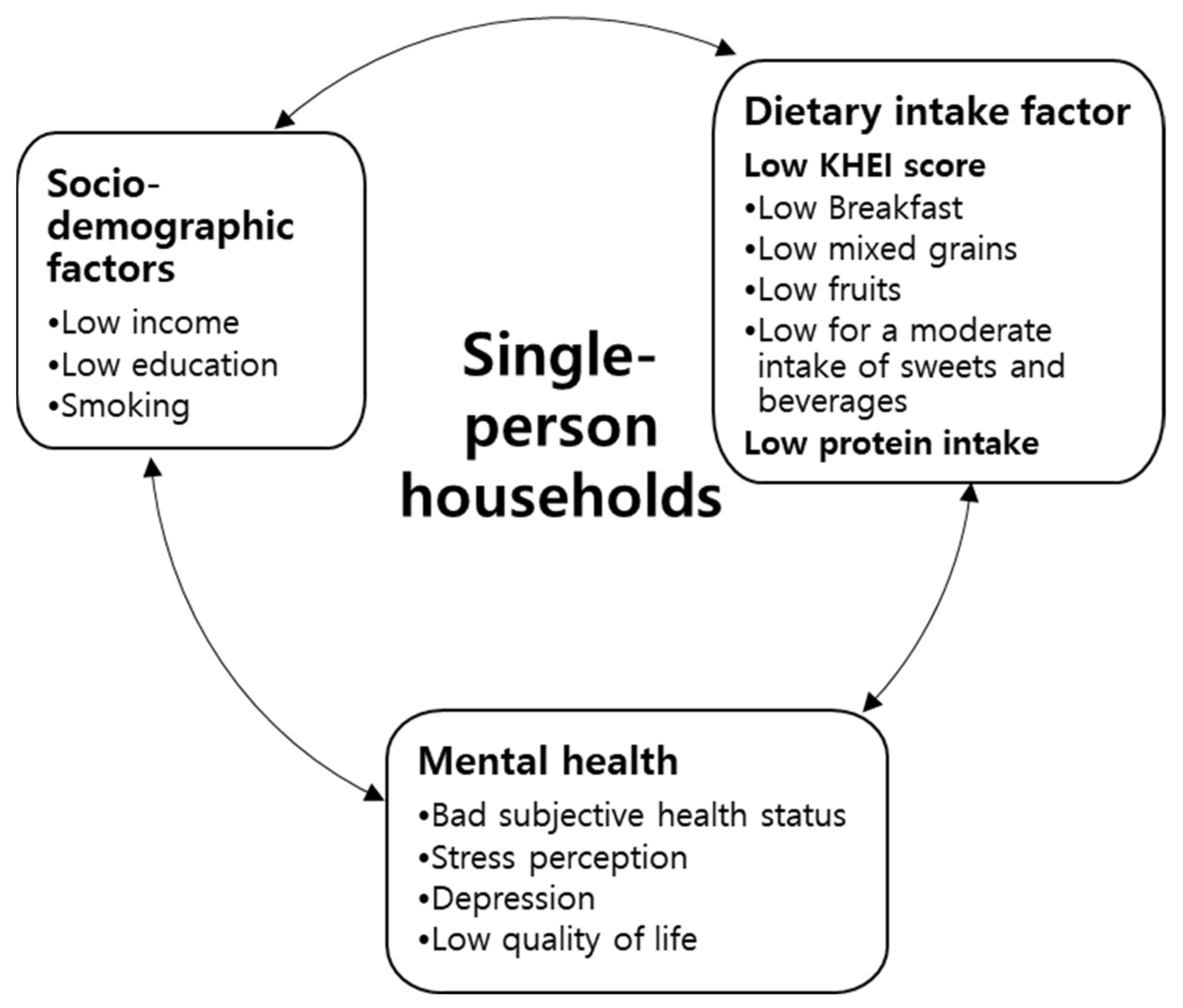
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Patterson, R.E.; Haines, P.S.; Popkin, B.M. Diet quality index: Capturing a multidimensional behavior. J. Am. Diet. Assoc. 1994, 94, 57–64. [Google Scholar] [CrossRef]
- Kennedy, E.T.; Ohls, J.; Carlson, S.; Fleming, K. The healthy eating index: Design and applications. J. Am. Diet. Assoc. 1995, 95, 1103–1108. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Vassilakou, T.; Lipworth, L.; Trichopoulos, D. Diet and overall survival in elderly people. BMJ 1995, 311, 1457–1460. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yook, S.M.; Park, S.; Moon, H.K.; Kim, K.; Shim, J.E.; Hwang, J.Y. Development of Korean Healthy Eating Index for adults using the Korea National Health and Nutrition Examination Survey data. J. Nutr. Health 2015, 48, 419–428. [Google Scholar] [CrossRef] [Green Version]
- Hanna, K.L.; Collins, P.F. Relationship between Living Alone and Food and Nutrient Intake. Nutr. Rev. 2015, 73, 594–611. [Google Scholar] [CrossRef] [Green Version]
- Korean Statistical Information Service (KOSIS). Available online: http://kosis.kr/statisticsList/statisticsList_01List.jsp?vwcd=MT_ZTITLE&4arentId=A#SubCont (accessed on 21 January 2022).
- Oh, Y.J. Considering single households for new health vulnerable groups. Korea Health Promot. Inst. 2017, 4, 1–8. [Google Scholar]
- Jung, K.H.; Nam, S.H.; Jung, E.J.; Lee, J.H.; Lee, Y.K.; Kim, J.S. Policy Implications of Changes in Family Structure: Focused on the Increase of Single Households in Korea; Korea Institute for Health and Social Affairs: Sejong, Korea, 2012. [Google Scholar]
- Byun, M. Single person household and urban policy in seoul. Korean J. Cult. Soc. Issues 2015, 21, 551–573. [Google Scholar] [CrossRef]
- Kim, H.Y. Floating families in Korea: Focusing on oneperson households. Korean Soc. 2014, 15, 255–292. [Google Scholar]
- Han, S.M.; Lee, S.J. Quality of life of youth living alone: With the focus of social capital influence. J. Law Public Policy 2018, 12, 60–85. [Google Scholar]
- Song, H.J.; Park, S.; Kwon, J.W. Quality of life of middle-aged adults in single households in South Korea. Qual. Life Res. 2018, 27, 2117–2125. [Google Scholar] [CrossRef]
- Kang, E.N.; Lee, M.H. Single-person household in South Korea and their policy implications. Minist. Health Welf. Forum 2016, 234, 47–56. [Google Scholar]
- Henning-Smith, C.; Gonzales, G. The relationship between living alone and self-rated health varies by age: Evidence from the National Health Interview Survey. J. Appl. Gerontol. 2020, 39, 971–980. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Organization Quality of life (WHOQOL). 1998. Available online: https://www.who.int/publications/i/item/WHO-HIS-his-Rev.2012.03 (accessed on 22 January 2022).
- Kauppinen, T.M.; Martelin, T.; Hannikainen-Ingman, K.; Virtala, E. Yksin Asuvien Hyvinvointi. Mitä Tällä Hetkellä Tiedetään? [Well-Being of People Living Alone. What Do We Know at the Moment?]; Finnish Institute for Health and Welfare: Helsinki, Finland, 2014; Volume 27. [Google Scholar]
- Lindström, M.; Rosvall, M. Marital status and 5-year mortality: A populationbased prospective cohort study. Public Health 2019, 170, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.E. The effects of a chronic disease/disability and stress from health on depressive symptoms among one-person households: A focus on the moderating effect of social support. Fam. Environ. Res. 2019, 57, 201–211. [Google Scholar] [CrossRef] [Green Version]
- Tamminen, N.; Kettunen, T.; Martelin, T.; Reinikainen, J.; Solin, P. Living alone and positive mental health: A systematic review. Syst. Rev. 2019, 8, 134–141. [Google Scholar] [CrossRef]
- Rossa-Roccor, V.; Richardson, C.G.; Murphy, R.A.; Gadermann, A.M. The association between diet and mental health and wellbeing in young adults within a biopsychosocial framework. PLoS ONE 2021, 16, e0252358. [Google Scholar]
- Pasanen, T.P.; Tamminen, N.; Martelin, T.; Mankinen, K.; Solin, P. Profiles of subjective health among people living alone: A latent class analysis. BMC Public Health 2021, 21, 1335. [Google Scholar] [CrossRef]
- Ishikawa, M.; Yokomichi, H.; Yokoyama, T. Difference and Variance in Nutrient Intake by Age for Older Adults Living Alone in Japan: Comparison of Dietary Reference Intakes for the Japanese Population. Nutrients 2021, 13, 1431. [Google Scholar] [CrossRef]
- Fukuda, Y.; Ishikawa, M.; Yokoyama, T.; Hayashi, T.; Nakaya, T.; Takemi, Y.; Kusama, K.; Yoshiike, N.; Nozue, M.; Yoshiba, K.; et al. Physical and Social Determinants of Dietary Variety among Older Adults Living Alone In Japan: Determinants of Dietary Variety in Elderly. Geriatr. Gerontol. Int. 2017, 17, 2232–2238. [Google Scholar] [CrossRef]
- Głąbska, D.; Guzek, D.; Groele, B.; Gutkowska, K. Fruit and vegetable intake and mental health in adults: A systematic review. Nutrients 2020, 12, 115. [Google Scholar] [CrossRef] [Green Version]
- Kuczmarski, M.F.; Sees, A.C.; Hotchkiss, L.; Cotugna, N.; Evans, M.K.; Zonderman, A.B. Higher Healthy Eating Index-2005 scores associated with reduced symptoms of depression in an urban population: Findings from the Healthy Aging in Neighborhoods of Diversity Across the Life Span (HANDLS) study. J. Am. Diet. Assoc. 2010, 110, 383–389. [Google Scholar] [CrossRef] [Green Version]
- Wang, K.; Zhao, Y.; Nie, J.; Xu, H.; Yu, C.; Wang, S. Higher HEI-2015 Score Is Associated with Reduced Risk of Depression: Result from NHANES 2005–2016. Nutrients 2021, 13, 348. [Google Scholar] [CrossRef] [PubMed]
- Bae, Y.J.; Yu, K.W.; Lee, K.H.; Jang, K.-II. Association of the Healthy Eating Index with Metabolic Abnormalities among Middle-Aged Adults Living in Single-Person Households in Korea. Nutrients 2021, 13, 3937. [Google Scholar] [CrossRef] [PubMed]
- Rahmani, J.; Milajerdi, A.; Dorosty-Motlagh, A. Association of the Alternative Healthy Eating Index (AHEI-2010) with depression, stress and anxiety among Iranian military personnel. BMJ Military Health 2018, 164, 87–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoon, Y.S.; Oh, S.W. Relationship between psychological distress and the adherence to the Korean healthy eating index (KHEI): The Korea National Health and Nutrition Examination Survey (KNHANES) 2013 and 2015. Nutr. Res. Pract. 2021, 15, 516–527. [Google Scholar] [CrossRef] [PubMed]
- Kweon, Y.; Kim, M.J.; Jang, Y.; Kim, K.; Kim, S.; Choi, C.; Chun, Y.H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [Green Version]
- Willett, W. Nutritional Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. In International Obesity Task Force; World Health Organization: Brussels, Belgium, 2000. [Google Scholar]
- Lee, E.J.; Kim, J.M. Association between depression and eating behavior factors in Korean adults: The Korea National Health and Nutrition Examination Survey 2018. J. Nutr. Health 2021, 54, 152–164. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- EuroQol Group. EuroQol: A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- National Rural Resources Development Institute. Korean Food Composition Table, 8th ed.; Rural Development Administration: Suwon, Korea, 2011; ISBN 978-89-363-1289-3.
- Kwon, J.S. Influencing factors on health-related quality of life in middle and old adult one-person households. J. Converg. Inf. Technol. 2019, 5, 153–167. [Google Scholar]
- Tan, Z.; Shi, F.; Zhang, H.; Li, N.; Xu, Y.; Liang, Y. Household income, income inequality, and health-related quality of life measured by the EQ-5D in Shaanxi, China: A cross sectional study. Int. J. Equity Health 2018, 17, 32. [Google Scholar] [CrossRef] [PubMed]
- Ko, A.R.; Jeong, K.H.; Shin, B.K. A longitudinal study on the effects of socioeconomic deprivations on depression of middle-aged single-person household—A focus on the comparison between single-person and multi-person households. Korean J. Family Soc. Work 2018, 59, 55–79. [Google Scholar]
- Lee, S. The integrated approach of the social and psychological factors affecting suicidal ideation. Democr. Soc. Policy Stud. 2016, 30, 104–139. [Google Scholar]
- Park, B. The path analysis for mutual relationship of stress and depression that affect the suicidality: Comparison of sex and age group. Health Soc. Welf Rev. 2012, 32, 485–521. [Google Scholar]
- Kang, Y.; Kang, S.; Kim, K.J.; Ko, H.; Shin, J.; Song, Y.M. The association between family mealtime and depression in elderly Koreans. Korean J. Fam. Med. 2018, 39, 340. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.H.; Kim, J.M. Relationship between Eating Behavior and Healthy Eating Competency of Single-Person and Multi-Person Households by Age Group. Korean J. Community Nutr. 2021, 26, 337–349. [Google Scholar] [CrossRef]
- Kang, N.Y.; Jung, B.M. Analysis of the Difference in Nutrients Intake, Dietary Behaviors and Food Intake Frequency of Single- and Non Single-Person Households—The Korea National Health and Nutrition Examination Survey (KNHANES), 2014–2016. Korean J. Community Nutr. 2019, 24, 1–17. [Google Scholar] [CrossRef]
- Kim, H.J.; Kwon, S.Y.; Hong, S.Y.; Lee, S.E. Health behaviors influencing depressive symptoms in older Koreans living alone: Secondary data analysis of the 2014 Korean longitudinal study of aging. BMC Geriatr. 2018, 18, 186. [Google Scholar] [CrossRef]
- Hu, X.Y.; Chen, Q.; Peng, X.D.; Zhang, X.M.; Huang, C.Q. Living arrangements and risk for late life depression: A meta-analysis of published literature. Int. J. Psychiatry Med. 2012, 43, 19–34. [Google Scholar]
- Lee, S.J.; Lee, S.M. Association of Dietary Quality with Subjective Health-Related Perception and Chronic Diseases According to Age Segmentation of Korean Elderly. Korean J. Community Nutr. 2021, 26, 363–381. [Google Scholar] [CrossRef]
- Miki, T.; Eguchi, M.; Kurotani, K.; Kochi, T.; Kuwahara, K.; Ito, R.; Kimura, Y.; Tsuruoka, H.; Akter, S.; Kashino, I.; et al. Dietary fiber intake and depressive symptoms in Japanese employees: The Furukawa Nutrition and Health Study. Nutrition 2016, 32, 584–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMartin, S.E.; Jacka, F.N.; Colman, I. The association between fruit and vegetable consumption and mental health disorders: Evidence from five waves of a national survey of Canadians. Prev. Med. 2013, 56, 225–230. [Google Scholar] [CrossRef]
- Jacka, F.N.; Mykletun, A.; Berk, M.; Bjelland, I.; Tell, G.S. The association between habitual diet quality and the common mental disorders in community dwelling adults: The Hordaland Health study. Psychosom. Med. 2011, 73, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Jacka, F.N.; Pasco, J.A.; Mykletun, A.; Williams, L.J.; Hodge, A.M.; O’Reilly, S.L.; Nicholson, G.C.; Kotowicz, M.A.; Berk, M. Association of Western and traditional diets with depression and anxiety in women. Am. J. Psychiatry 2010, 167, 305–311. [Google Scholar] [CrossRef] [Green Version]
- Opie, R.S.; Itsiopoulos, C.; Parletta, N.; Sanchez-Villegas, A.; Akbaraly, T.N.; Ruusunen, A.; Jacka, F.N. Dietary recommendations for the prevention of depression. International Journal on Nutrition. Diet. Nerv. Syst. 2016, 20, 161–171. [Google Scholar]
- Li, Y.; Lv, M.R.; Wei, U.J.; Sun, L.; Zhang, J.X.; Zhang, H.G.; Li, B. Dietary patterns and depression risk: A meta-analysis. Psychiatry Res. 2017, 253, 373–382. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Men (n = 1334) | Women (n = 2185) | |||||
|---|---|---|---|---|---|---|---|
| Single-Person (n = 114) | Multi-Person (n = 1220) | p-Value 3 | Single-Person (n = 144) | Multi-Person (n = 2041) | p-Value | ||
| Age (yrs) | 49.19 ± 0.54 1 | 49.59 ± 0.18 | 0.484 | 51.11 ± 0.61 | 49.65 ± 0.16 | 0.021 | |
| Education | ≤Elementary | 8 (6.22) 2 | 55 (4.96) | 0.337 | 25 (15.50) | 151 (7.05) | <0.001 |
| ≤Middle school | 15 (10.81) | 99 (7.19) | 20 (14.69) | 191 (9.64) | |||
| ≥High school | 91 (82.97) | 1066 (87.86) | 99 (69.81) | 1699 (83.31) | |||
| Household income | Low | 22 (19.74) | 76 (6.79) | 0.001 | 36 (26.53) | 144 (7.46) | <0.0001 |
| Middle–low | 26 (20.47) | 243 (19.76) | 50 (33.21) | 422 (20.32) | |||
| Middle–high | 24 (24.70) | 388 (19.76) | 28 (18.51) | 655 (32.68) | |||
| High | 42 (35.10) | 511 (41.68) | 30 (21.76) | 819 (39.54) | |||
| Marrital status | Single | 90 (80.24) | 104 (9.44) | <0.0001 | 106 (73.00) | 212 (10.68) | <0.0001 |
| Married | 24 (19.76) | 1116 (90.56) | 38 (27.00) | 1829 (89.32) | |||
| Alcohol intake | No | 38 (31.43) | 335 (28.22) | 0.491 | 83 (57.51) | 1096 (52.47) | 0.304 |
| Yes | 76 (68.57) | 885 (71.78) | 61 (42.49) | 945 (47.54) | |||
| Smoking status | No | 45 (39.13) | 748 (61.84) | <0.0001 | 125 (84.97) | 1946 (94.81) | <0.0001 |
| Yes | 69 (60.87) | 472 (38.16) | 19 (15.03) | 95 (5.19) | |||
| Physical activity | No | 63 (55.67) | 692 (55.16) | 0.929 | 89 (58.03) | 1156 (54.99) | 0.518 |
| Yes | 51 (44.33) | 528 (44.84) | 55 (41.97) | 885 (45.01) | |||
| Body mass index (kg/m2) | 24.30 ± 0.39 | 24.76 ± 0.10 | 0.256 | 23.96 ± 0.33 | 23.50 ± 0.09 | 0.177 | |
| Underweight (BMI < 18.5 kg/m2) | 2 (2.41) | 24 (2.20) | 0.061 | 4 (2.93) | 74 (3.44) | 0.349 | |
| Normal (18.5 ≤ BMI < 23 kg/m2) | 32 (29.36) | 324 (26.59) | 59 (39.48) | 950 (46.96) | |||
| Overweight (23.0 ≤ BMI < 25 kg/m2) | 39 (36.93) | 316 (25.85) | 41 (27.09) | 436 (21.47) | |||
| Obesity (BMI ≥ 25 kg/m2) | 41 (31.30) | 556 (45.36) | 40 (30.50) | 581 (28.13) | |||
| Variables | Men (n = 1334) | Women (n = 2185) | ||||
|---|---|---|---|---|---|---|
| Single-Person (n = 114) | Multi-Person (n = 1220) | p-Value 3 | Single-Person (n = 144) | Multi-Person (n = 2041) | p-Value | |
| Subjective health status | 2.98 ± 0.09 1 | 3.23 ± 0.02 | 0.015 | 2.84 ± 0.08 | 3.15 ± 0.02 | <0.001 |
| Good | 86 (75.02) 2 | 1052 (86.95) | <0.001 | 402 (69.95) | 1693 (83.18) | <0.001 |
| Poor | 28 (24.98) | 168 (13.05) | 42 (30.05) | 348 (16.82) | ||
| Stress perception | 2.16 ± 0.07 | 2.18 ± 0.02 | 0.813 | 2.26 ± 0.07 | 2.16 ± 0.02 | 0.160 |
| No | 85 (74.49) | 896 (73.51) | 0.845 | 99 (68.17) | 1528 (75.59) | 0.086 |
| Yes | 29 (25.51) | 324 (26.49) | 45 (31.83) | 513 (24.41) | ||
| PHQ-9 index | 3.28 ± 0.52 | 1.70 ± 0.10 | 0.004 | 3.82 ± 0.43 | 2.29 ± 0.08 | <0.001 |
| Normal | 102 (87.41) | 1194 (97.75) | <0.0001 | 128 (89.44) | 1963 (96.35) | <0.0001 |
| Depression | 12 (12.59) | 26 (2.25) | 16 (10.56) | 78 (3.65) | ||
| EQ-5D index | 0.95 ± 0.01 | 0.97 ± 0.00 | 0.011 | 0.93 ± 0.01 | 0.96 ± 0.00 | 0.003 |
| Variables | Men (n = 1334) | Women (n = 2185) | ||||
|---|---|---|---|---|---|---|
| Single-Person (n = 114) | Multi-Person (n = 1220) | p-Value 2 | Single-Person (n = 144) | Multi-Person (n = 2041) | p-Value | |
| Total energy (kcal) | 2229.77 ± 85.43 1 | 2310.44 ± 22.15 | 0.370 | 1728.32 ± 57.46 | 1672.62 ± 15.34 | 0.349 |
| % energy of carbohydrate | 63.68 ± 1.33 | 63.52 ± 0.35 | 0.909 | 65.78 ± 0.90 | 65.39 ± 0.28 | 0.682 |
| % energy of protein | 16.43 ± 0.64 | 15.74 ± 0.14 | 0.301 | 14.39 ± 0.35 | 14.78 ± 0.11 | 0.287 |
| % energy of fat | 19.89 ± 0.92 | 20.73 ± 0.29 | 0.387 | 19.84 ± 0.74 | 19.82 ± 0.23 | 0.985 |
| Protein (g/1000 kcal) | 36.45 ± 1.46 | 35.83 ± 0.30 | 0.683 | 34.39 ± 0.78 | 36.19 ± 0.27 | 0.031 |
| Fat (g/1000 kcal) | 19.84 ± 0.93 | 21.10 ± 0.29 | 0.196 | 21.16 ± 0.79 | 21.62 ± 0.26 | 0.583 |
| Carbohydrate (g/1000 kcal) | 143.52 ± 4.19 | 147.44 ± 1.12 | 0.376 | 160.02 ± 2.91 | 161.01 ± 0.74 | 0.742 |
| Total dietary fiber (g/1000 kcal) | 11.41 ± 0.56 | 12.35 ± 0.16 | 0.108 | 15.50 ± 0.60 | 15.36 ± 0.18 | 0.822 |
| Calcium (mg/1000 kcal) | 263.72 ± 16.78 | 263.81 ± 4.09 | 0.996 | 304.46 ± 13.69 | 294.96 ± 3.83 | 0.498 |
| Phosphorus (mg/1000 kcal) | 533.12 ± 17.23 | 537.19 ± 4.17 | 0.817 | 564.65 ± 12.94 | 575.83 ± 3.86 | 0.406 |
| Iron (mg/1000 kcal) | 5.99 ± 0.26 | 6.10 ± 0.08 | 0.673 | 6.58 ± 0.26 | 6.62 ± 0.07 | 0.889 |
| Sodium (mg/1000 kcal) | 1815.70 ± 72.32 | 1811.50 ± 23.61 | 0.956 | 1717.69 ± 66.31 | 1748.98 ± 21.89 | 0.646 |
| Potassium (mg/1000 kcal) | 1381.32 ± 46.01 | 1418.15 ± 16.32 | 0.430 | 1675.20 ± 55.36 | 1659.88 ± 14.44 | 0.785 |
| Vitamin A(ugRAE/1000 kcal) | 189.45 ± 17.20 | 190.00 ± 7.63 | 0.977 | 251.51 ± 18.61 | 213.86 ± 4.21 | 0.042 |
| Thiamin (mg/1000 kcal) | 0.70 ± 0.04 | 0.69 ± 0.01 | 0.900 | 0.70 ± 0.03 | 0.69 ± 0.01 | 0.903 |
| Riboflavin (mg/1000 kcal) | 0.76 ± 0.04 | 0.79 ± 0.01 | 0.377 | 0.88 ± 0.03 | 0.86 ± 0.01 | 0.524 |
| Niacin (mg/1000 kcal) | 6.54 ± 0.27 | 6.84 ± 0.08 | 0.285 | 6.89 ± 0.24 | 7.24 ± 0.07 | 0.157 |
| Vitamin C (mg/1000 kcal) | 26.89 ± 5.01 | 30.27 ± 1.11 | 0.510 | 37.58 ± 3.87 | 40.26 ± 1.18 | 0.511 |
| Variables | Men (n = 1334) | Women (n = 2185) | ||||
|---|---|---|---|---|---|---|
| Single-Person (n = 114) | Multi-Person (n = 1220) | p-Value 2 | Single-Person (n = 144) | Multi-Person (n = 2041) | p-Value | |
| Total KHEI score (0–100) | 57.74 ± 1.28 1 | 63.68 ± 0.43 | <0.0001 | 65.99 ± 1.25 | 66.53 ± 0.37 | 0.681 |
| Component of KHEI score | ||||||
| Adequacy | ||||||
| Breakfast (0–10) | 5.52 ± 0.47 | 7.55 ± 0.13 | <0.0001 | 6.86 ± 0.38 | 7.51 ± 0.10 | 0.100 |
| Mixed grains (0–5) | 0.93 ± 0.18 | 2.06 ± 0.07 | <0.0001 | 1.97 ± 0.21 | 2.11 ± 0.05 | 0.519 |
| Total fruits (0–5) | 1.28 ± 0.20 | 1.91 ± 0.07 | 0.003 | 2.85 ± 0.21 | 2.88 ± 0.06 | 0.868 |
| Fresh fruits (0–5) | 1.28 ± 0.21 | 2.21 ± 0.07 | <0.0001 | 3.06 ± 0.21 | 3.12 ± 0.07 | 0.765 |
| Total vegetable (0–5) | 3.94 ± 0.14 | 3.91 ± 0.04 | 0.816 | 3.47 ± 0.14 | 3.38 ± 0.03 | 0.565 |
| Vegetable, excluding kimchi and pickles (0–5) | 3.53 ± 0.15 | 3.44 ± 0.05 | 0.551 | 3.31 ± 0.14 | 3.14 ± 0.04 | 0.235 |
| Meat, fish, eggs, and legumes (0–10) | 7.09 ± 0.35 | 7.42 ± 0.09 | 0.373 | 6.86 ± 0.30 | 6.86 ± 0.09 | 0.986 |
| Milk and dairy (0–10) | 2.95 ± 0.44 | 3.03 ± 0.14 | 0.873 | 3.83 ± 0.40 | 3.41 ± 0.12 | 0.298 |
| Moderation | ||||||
| Sodium (0–10) | 5.77 ± 0.32 | 5.52 ± 0.11 | 0.457 | 7.44 ± 0.29 | 7.71 ± 0.07 | 0.356 |
| Saturated fatty acid (0–10) | 7.34 ± 0.41 | 7.55 ± 0.12 | 0.629 | 7.80 ± 0.30 | 7.69 ± 0.10 | 0.738 |
| Sweets and beverages (0–10) | 8.67 ± 0.29 | 9.26 ± 0.07 | 0.049 | 9.28 ± 0.18 | 9.28 ± 0.05 | 0.999 |
| Balance | ||||||
| Carbohydrate (0–5) | 2.55 ± 0.21 | 2.83 ± 0.07 | 0.222 | 2.70 ± 0.18 | 2.66 ± 0.06 | 0.796 |
| Fat (0–5) | 3.61 ± 0.17 | 3.69 ± 0.06 | 0.653 | 3.49 ± 0.18 | 3.55 ± 0.05 | 0.778 |
| Total energy (0–5) | 3.28 ± 0.22 | 3.31 ± 0.07 | 0.900 | 3.07 ± 0.20 | 3.22 ± 0.05 | 0.440 |
| Variables | Men (n = 1334) | Women (n = 2185) | |||||
|---|---|---|---|---|---|---|---|
| Single-Person (n = 114) | Multi-Person (n = 1220) | p-Value | Single-Person (n = 144) | Multi-Person (n = 2041) | p-Value | ||
| Subjective health status (poor) | Model 1 2 | 2.2 (1.4–3.6) 1 | 1.0 (ref.) | 0.001 | 2.1 (1.4–3.2) | 1.0 (ref.) | <0.001 |
| Model 2 3 | 1.4 (0.8–2.5) | 1.0 (ref.) | 0.250 | 1.5 (0.9–2.4) | 1.0 (ref.) | 0.137 | |
| Stress perception (yes) | Model 1 | 1.0 (0.6–1.6) | 1.0 (ref.) | 0.847 | 1.4 (0.9–2.2) | 1.0 (ref.) | 0.088 |
| Model 2 | 1.0 (0.5–1.8) | 1.0 (ref.) | 0.905 | 1.1 (0.7–1.7) | 1.0 (ref.) | 0.816 | |
| Depression | Model 1 | 6.3 (2.7–14.3) | 1.0 (ref.) | <0.0001 | 3.1 (1.7–5.6) | 1.0 (ref.) | <0.001 |
| Model 2 | 3.5 (1.2–10.1) | 1.0 (ref.) | 0.018 | 1.1 (0.6–2.0) | 1.0 (ref.) | 0.852 |
| Variables | Single-Person (n 114) | Multi-Person (n = 1220) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Tertile of KHEI | Tertile of KHEI | ||||||||
| T1 (n = 38) | T2 (n = 38) | T3 (n = 38) | p for trend | T1 (n = 406) | T2 (n = 407) | T3 (n = 407) | p for Trend | ||
| Subjective health status (poor) | Model 1 2 | 1.4 (0.5–4.4) 1 | 0.8 (0.2–2.9) | 1.0 (ref.) | 0.638 | 1.5 (0.9–2.4) | 1.2 (0.8–2.0) | 1.0 (ref.) | 0.084 |
| Model 2 3 | 1.3 (0.4–4.5) | 0.5 (0.1–2.1) | 1.0 (ref.) | 0.860 | 1.4 (0.9–2.2) | 1.2 (0.8–1.9) | 1.0 (ref.) | 0.183 | |
| Stress perception (yes) | Model 1 | 1.3 (0.4–4.5) | 1.1 (0.3–4.1) | 1.0 (ref.) | 0.697 | 1.3 (1.0–1.9) | 1.1 (0.8–1.5) | 1.0 (ref.) | 0.084 |
| Model 2 | 1.2 (0.3–4.1) | 1.2 (0.3–4.7) | 1.0 (ref.) | 0.775 | 1.2 (0.9–1.7) | 1.1 (0.8–1.4) | 1.0 (ref.) | 0.263 | |
| Depression | Model 1 | 3.1 (0.6–17.0) | 0.9 (0.1–8.1) | 1.0 (ref.) | 0.255 | 2.7 (0.9–8.0) | 1.4 (0.4–4.4) | 1.0 (ref.) | 0.055 |
| Model 2 | 2.3 (0.4–14.2) | 0.7 (0.1–5.1) | 1.0 (ref.) | 0.418 | 1.8 (0.7–5.0) | 1.2 (0.4–3.8) | 1.0 (ref.) | 0.214 |
| Variables | Single-Person (n = 144) | Multi-Person (n = 2041) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Tertile of KHEI | Tertile of KHEI | ||||||||
| T1 (n = 48) | T2 (n = 48) | T3 (n = 48) | p for Trend | T1 (n = 680) | T2 (n = 681) | T3 (n = 680) | p for Trend | ||
| Subjective health status (poor) | Model 1 2 | 1.5 (0.6–3.6) 1 | 1.0 (0.4–2.7) | 1.0 (ref.) | 0.385 | 1.3 (0.9–1.8) | 0.9 (0.7–1.3) | 1.0 (ref.) | 0.192 |
| Model 2 3 | 1.2 (0.5–3.1) | 0.8 (0.3–2.4) | 1.0 (ref.) | 0.764 | 1.2 (0.8–1.7) | 0.9 (0.6–1.3) | 1.0 (ref.) | 0.340 | |
| Stress perception (yes) | Model 1 | 3.5 (1.3–9.0) * | 1.1 (0.4–3.1) | 1.0 (ref.) | 0.013 | 1.4 (1.0–1.8) * | 1.0 (0.7–1.3) | 1.0 (ref.) | 0.035 |
| Model 2 | 2.8 (1.0–7.5) * | 1.1 (0.4–3.3) | 1.0 (ref.) | 0.051 | 1.3 (0.9–1.6) | 0.9 (0.7–1.3) | 1.0 (ref.) | 0.182 | |
| Depression | Model 1 | 25.4 (3.2–203.8) ** | 7.2 (0.7–79.5) | 1.0 (ref.) | 0.002 | 2.2 (1.1–4.6) * | 1.7 (0.8–3.6) | 1.0 (ref.) | 0.027 |
| Model 2 | 28.3 (2.1–374.2) * | 5.2 (0.4–61.4) | 1.0 (ref.) | 0.007 | 1.9 (0.9–4.1) | 1.5 (0.7–3.4) | 1.0 (ref.) | 0.092 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-M.; Lee, E. Association between Healthy Eating Index and Mental Health in Middle-Aged Adults Based on Household Size in Korea. Int. J. Environ. Res. Public Health 2022, 19, 4692. https://doi.org/10.3390/ijerph19084692
Kim J-M, Lee E. Association between Healthy Eating Index and Mental Health in Middle-Aged Adults Based on Household Size in Korea. International Journal of Environmental Research and Public Health. 2022; 19(8):4692. https://doi.org/10.3390/ijerph19084692
Chicago/Turabian StyleKim, Ji-Myung, and EunJung Lee. 2022. "Association between Healthy Eating Index and Mental Health in Middle-Aged Adults Based on Household Size in Korea" International Journal of Environmental Research and Public Health 19, no. 8: 4692. https://doi.org/10.3390/ijerph19084692
APA StyleKim, J.-M., & Lee, E. (2022). Association between Healthy Eating Index and Mental Health in Middle-Aged Adults Based on Household Size in Korea. International Journal of Environmental Research and Public Health, 19(8), 4692. https://doi.org/10.3390/ijerph19084692






