Abstract
The youth mental health sector is persistently challenged by issues such as service fragmentation and inefficient resource allocation. Systems modelling and simulation, particularly utilizing participatory approaches, is offering promise in supporting evidence-informed decision making with limited resources by testing alternative strategies in safe virtual environments before implementing them in the real world. However, improved evaluation efforts are needed to understand the critical elements involved in and to improve methods for implementing participatory modelling for youth mental health system and service delivery. An evaluation protocol is described to evaluate the feasibility, value, impact, and sustainability of participatory systems modelling in delivering advanced decision support capabilities for youth mental health. This study applies a comprehensive multi-scale evaluation framework, drawing on participatory action research principles as well as formative, summative, process, and outcome evaluation techniques. Novel data collection procedures are presented, including online surveys that incorporate gamification to enable social network analysis and patient journey mapping. The evaluation approach also explores the experiences of diverse stakeholders, including young people with lived (or living) experience of mental illness. Social and technical opportunities will be uncovered, as well as challenges implementing these interdisciplinary methods in complex settings to improve youth mental health policy, planning, and outcomes. This study protocol can also be adapted for broader international applications, disciplines, and contexts.
1. Introduction
Health systems internationally are under immense pressure to manage complex and compounding health challenges, often being met with policy resistance [1,2]. The introduction of new policies is often top-down and as such can be opposed by health service providers and consumers [3]. This is also true in mental health, which is currently one of the top public health concerns that affects all aspects of individual lives, as well as the health and wellbeing of families and whole communities [4,5,6]. In particular, young people are the most vulnerable, as mental disorders and substance misuse affect at least 1 in 4 young people by the time they reach 25 years of age and are the leading causes of disability and premature death in this age group globally [7]. Mental disorders and substance abuse that emerge during adolescence can persist into later adulthood, having lifelong implications [8,9].
Despite Australia being one of the first countries to develop and implement a national mental health plan in 1993 [10], its mental health system continues to be underdeveloped and over-stretched, faced with persistent challenges including but not limited to service fragmentation, late intervention, mental health treatment isolated from other physical and social needs, poor quality of care, and inefficient resource allocation [11,12,13]. This has led to attempts by the government to invest billions of dollars in mental health system reforms, programs, and services, which has achieved little impact in the population’s mental health outcomes [14]. Insufficient evaluations of such mental health system reforms, programs, and services contribute to an ongoing cycle of refunding and reactive acts of government without truly understanding which initiatives would yield the best returns on investment [15].
1.1. Supporting Strategic Decision Making with Participatory Systems Modelling
The deployment of systems models offers a valuable tool to support strategic decision making for some of the world’s most complex challenges, including the current global mental health crisis that is particularly exacerbated in young people. Systems models consider the complex causal inter-relationships that drive population mental health outcomes and can be used to simulate policies and initiatives to determine which combinations are likely to deliver the best outcomes and returns on investment in youth mental health [2]. In particular, system dynamics modelling is a well-established quantitative method long used in other sectors [16]. System dynamics modelling can also lend itself to a participatory approach whereby an interdisciplinary stakeholder group is actively engaged in mapping and contextualizing causal mechanisms driving complex system behaviors [17]. This process is commonly referred to as participatory systems modelling (PSM). The involvement of stakeholders in the model building process is particularly significant in mental health, as it offers the opportunity for the perspectives of community representatives from across the system—including young people with lived (or living) experience of mental illness—to contribute to the technical model development process [18]. This enables improved model credibility, utility, and a robust basis for policy and planning dialogues which can lead to organized, evidence-informed, and active advocacy [16].
Systems models also have the ability to incorporate local contextual factors [19,20]. Such factors include but are not limited to local service capacity, quality, and affordability that contribute to delays in service access, incentives and disincentives in the system, as well as other characteristics and locally specific contextual drivers of mental illness and suicidal behavior such as high youth unemployment, a lack of education and training opportunities, and intergenerational disadvantages [17,21,22].
1.2. The Need to Evaluate Participatory Systems Modelling Programs
Though PSM methods have been widely adopted across disciplines, including in the business and environmental sectors [16,17,23,24], they are only more recently being applied to support youth mental health systems planning and policy [17,25]. PSM in this area offers much promise in improving understanding and ownership of systems issues among the diverse stakeholders involved, providing an opportunity to explore the implications of alternate resource allocation strategies or policies, improving communication and coordination across the system, building consensus and collaborative action, and delivering transparency in decision making [26,27,28]. However, there is need for improved evaluation efforts in PSM programs to understand their value in different contexts [26].
Reflective evaluation practices that include feedback from system stakeholders enables an iterative process that investigates whether the participatory modelling program has achieved its aims. Such aims may include but are not limited to building stakeholder capacity in understanding the behavior of complex systems, forming connections between stakeholders from different parts of the system to improve coordination (and reduce fragmentation), fostering confidence in using the systems model, accountability to better inform decision making, as well as consensus for collaborative action to improve the system at the national, state, and local government levels [26].
A scoping review of participatory modelling evaluation frameworks is described elsewhere. This review provides a synthesis of the literature and presents a comprehensive multi-scale evaluation framework that can be applied to assess participatory modelling programs across diverse disciplines as well as across different modelling methods. The framework aims to assess four key outcomes: feasibility (i.e., is participatory modelling feasible?), value (i.e., what is the value of the participatory modelling process?), impact (i.e., what changed or was actioned as a result of the participatory modelling process?), and sustainability (i.e., are the changes and actions from the participatory modelling process sustained over time?). To our knowledge, this evaluation study protocol is the first of its kind, applying a novel evaluation framework and techniques in the context of PSM for youth mental health research.
1.3. Right Care, First Time, Where You Live Program
A team of multidisciplinary mental health researchers at The University of Sydney in Australia has been developing system dynamics models for youth mental health utilizing a participatory approach [17,18,19,25]. Right care, first time, where you live is a national multi-site health services research program (henceforth referred to as the Program) that will work with eight sites across Australia, delineated by local health regions in the Australian Capital Territory, New South Wales, Queensland, and Western Australia. As part of the Program, system dynamics models will be co-designed and implemented at each of the eight participating sites. A national Australian systems model will also be developed to ensure the expansion of the modelling infrastructure can be applied to youth mental health systems across the country through evidence-informed decision making in mental health policy and planning [29]. Blueprints describing the development of the technical systems models [30], the participatory modelling approach [31], as well as the overall protocol for the Program are provided elsewhere.
This research protocol describes the PSM evaluation of the Program. The feasibility and value of PSM to support decision making have previously been evaluated for population health issues including obesity prevention and diabetes in pregnancy [32]. However, important gaps in knowledge remain, such as evaluating the PSM approach for youth mental health policy and planning, system strengthening, and the inclusion of the perspectives of diverse stakeholders including young people with lived (or living) experience as well as their carers in the participatory (co-design) process. This evaluation study will contribute new knowledge by comprehensively analyzing how developing and implementing co-designed systems models can influence decision making, stakeholder engagement and learning, consensus, as well as collaboration to positively impact the youth mental health landscape.
1.4. Objectives
This study applies a comprehensive multi-scale evaluation framework designed for participatory modelling programs that is described elsewhere and aims to answer four research questions:
- Is it feasible to undertake an inclusive, transparent, participatory approach to develop highly technical and broadly scoped youth mental health systems models in a way that local stakeholders can understand (i.e., the structure, logic and assumptions of the systems model) and find credible?
- Does the co-designed systems model add value to decision making for youth mental health system strengthening or resource allocation?
- What has been impacted as a result of the PSM process (i.e., what changes or actions has the PSM process facilitated)?
- Have these impacts (changes or actions) been sustained over time to improve youth mental health outcomes?
The experiences arising from the application of PSM among diverse stakeholder groups will be explored, including but not limited to the following:
- Health organization administrators, including staff from funding agencies;
- Front-line health service professionals, including clinicians;
- Community representatives, including educators and young people with lived (or living) experience of mental illness.
2. Materials and Methods
The described evaluation study protocol was reviewed and approved by the Sydney Local Health District Human Research Ethics Committee (HREC; Protocol No X21-0151 and 2021/ETH00553) on 5 July 2021.
2.1. Study Design and Setting
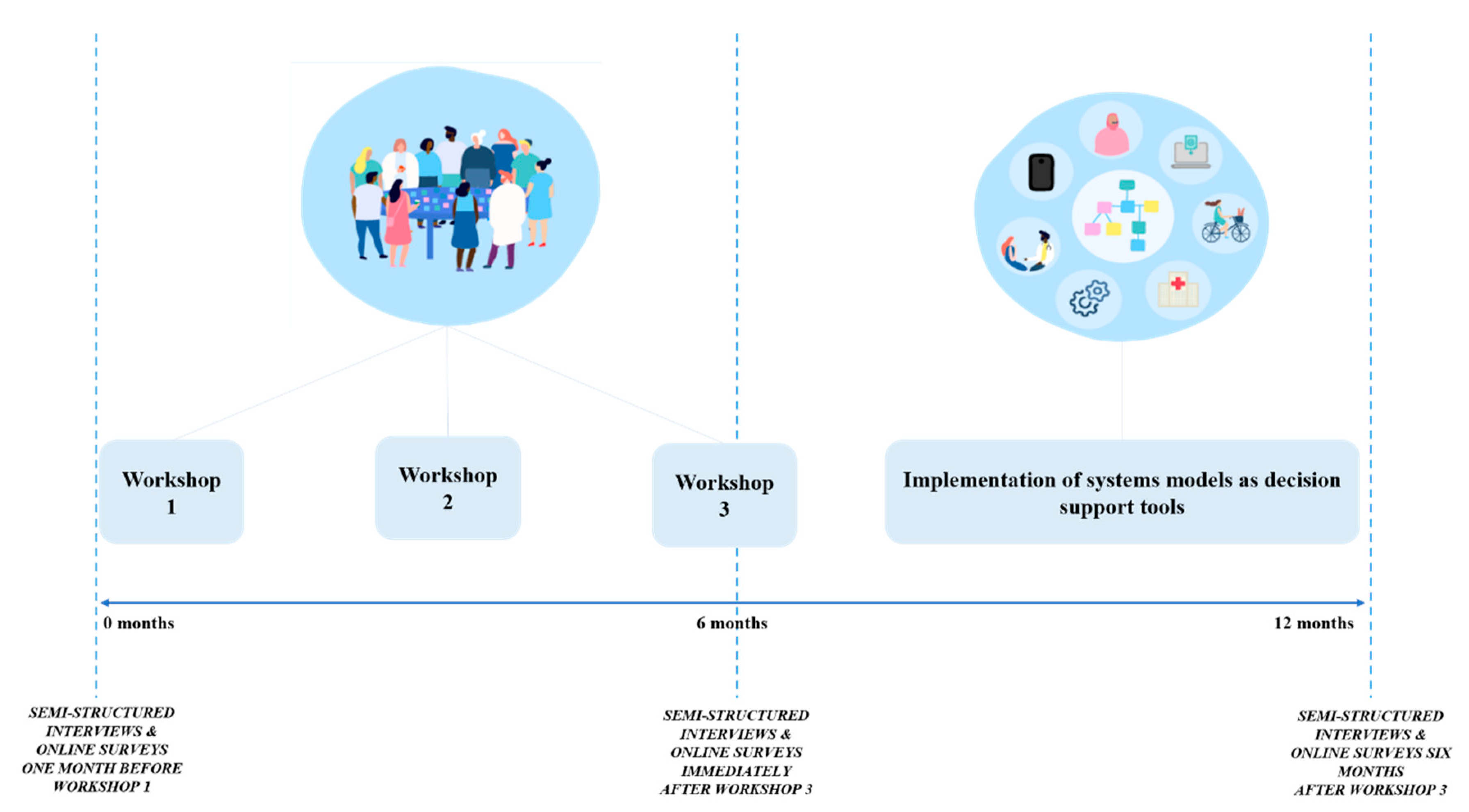
This protocol describes an evaluation study of the PSM process of the Program that applies a comprehensive multi-scale evaluation framework drawing on participatory action research (PAR) principles and methods described elsewhere. This evaluation study also adopts formative, summative, process, and outcome evaluation techniques. The PAR approach of action and reflection enables the flexibility to iterate the evaluation study throughout the Program, responding to different research contexts as needed for the eight participating sites [33]. A co-design process involving three PSM workshops with local stakeholders will be conducted at each participating site to develop eight local youth mental health systems models. The evaluation process will be aligned to the PSM workshops and will be conducted in two sites per year from 2022 to 2025. The evaluation approach, including the data collection procedures, are described below. Figure 1 summarizes the time points of evaluation at each site aligned to the PSM workshops.
Figure 1.
Evaluation time points aligned to the three PSM workshops. Evaluation will be conducted in two sites per year from 2022 to 2025 (total of eight sites).
2.2. Study Population
To best capture the Australian mental health context, the eight research sites will vary across urban, outer-urban, regional, and rural-remote locations and may include diverse cultural or socioeconomic subgroups [18]. Up to 55 participants will be included per site (8 sites in total, N ≈ 440 participants). The proposed sample size is based on the extensive experience of the research team in conducting PSM studies [2,18,32], and reflects the likely number of participants needed to capture diverse perspectives across the system and achieve the saturation of themes [34].
2.3. Inclusion and Exclusion Criteria
Diverse stakeholders from each local youth mental health and broader social systems will be invited to participate in the PSM workshops. Invited representatives will include but are not limited to young people with lived (or living) experience, supportive others (e.g., family members, carers, and close friends), health professionals, service managers, policy makers, local academics, educators (e.g., teachers), and administrators.
- Inclusion Criteria:
- Individuals (≥14 years), supportive others (e.g., carers), as well as professionals who work with young people or are involved in the local youth mental health and broader social systems;
- English proficiency;
- Capacity to give written informed consent and willingness to participate in the study.
2.4. Recruitment Procedure
The recruitment process for this study will be undertaken in collaboration with the primary partner organization at each of the participating sites with guidance from the research team. Active snowball sampling will be employed when appropriate to enable PAR, whereby the invited participants are empowered to contribute and identify any other stakeholders who should also be invited to participate. Throughout this process, a local chief investigator for each participating site will be identified to play a critical role in both recruiting key stakeholders as well as facilitating the engagement of local communities [35,36]. Eligible participants will be enrolled into the study after providing informed consent through a transparent communication process to ensure that all stakeholders can make their own decisions to participate [37]. The privacy of all participants will be emphasized, and all potential participants will be informed that their data will be non-identifiable and securely stored [38,39].
As populations from culturally and linguistically diverse backgrounds, including Aboriginal and Torres Strait Islander communities, may be invited to participate across the eight sites, recruitment will be conducted in an ethical and effective manner to ensure engagement in intercultural settings will be respectful, reflective, and reasoned [40,41,42]. Cultural competency in research is the ability to provide high-quality research that considers the culture and diversity of populations when developing ideas, conducting research, and exploring applicability of research findings [43].
2.5. Data Collection Procedures
A mixed methods approach will be adopted, as this strengthens the study design through the triangulation, cross-verification, and validation of evaluation data [44]. Data collection will occur via online surveys (which will incorporate patient journey mapping and social network analysis), semi-structured interviews, researcher observations and recordings from the PSM workshops, meetings with local stakeholders outside the PSM workshops, reflections and field notes made by the research team throughout the Program, and monitoring stakeholder use of the final systems model by configuring the model interface to collect user tracking data by page. Participants will be reimbursed for their time participating in online surveys and semi-structured interviews.
Table 1 summarizes the mixed method application of the comprehensive multi-scale evaluation framework. Table 1 was utilized when developing the interview and online survey questions to ensure that all evaluation criteria of the comprehensive multi-scale framework were incorporated into the data collection procedures. Data may also be compared across (e.g., rural vs. urban) and within (e.g., differing experiences across subgroups of participants) the participating sites to analyze how the feasibility, value, impact, and sustainability of PSM varies depending on the implementation context. Cross-site and subgroup analyses will likely lead to consideration of the impact of broader determinants that may affect participation in and outcomes of the PSM process [8,9,10,12].

Table 1.
Applying a comprehensive multi-scale evaluation framework to collect data utilizing a mixed-methods approach for the Program.
- Online Surveys
Surveys will be conducted with local stakeholders participating in the Program for each site at three time points. Quantitative and qualitative data will be collected (1) prior to commencement of the PSM workshop series (baseline), (2) on completion of the PSM workshop series and systems model development (first follow-up: around month 6), and (3) 6 months following the completion of the PSM workshop series (final follow-up: around month 12). The surveys, adapted from Freebairn et al. [34], have four main components: (1) questions to elicit perceptions regarding priorities for youth mental health system strengthening, (2) expectations and experiences of participating in the PSM process, (3) social network analysis, and (4) patient journey mapping.
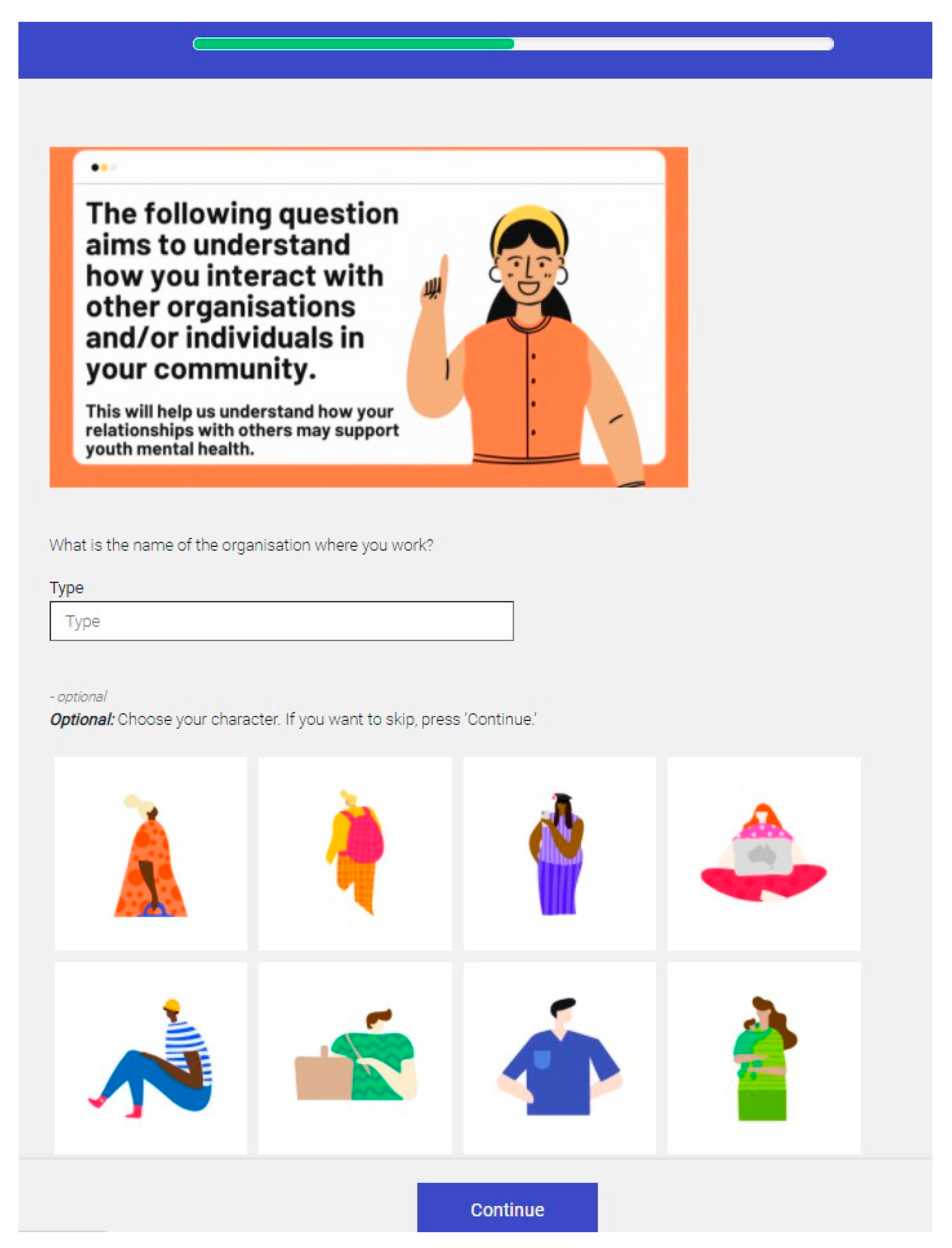
All local stakeholders invited to participate in the PSM workshops will be invited to complete online surveys. The survey questions have undergone cognitive testing to ensure they are relevant, logical, and easily understood by participants [45]. Specifically, the survey questions have been reviewed by the Brain and Mind Centre’s Youth Lived Experience Working Group to ensure that the questions are appropriate and suitable for young people with lived (or living) experience of mental illness. Numerous changes were made from the working group’s feedback, including rephrasing the questions to utilize strength-based language. Surveys will be administered through a secure online data collection tool, Cogniss, which is an online platform that has the ability to gamify survey components [46]. Gamification of online surveys has been acknowledged to improve participant engagement, reduce bias, and improve the quality of survey results [47]. The online surveys will incorporate game design elements such as avatars and badges to motivate respondents to complete activities. Gamification techniques such as competition with others will not be utilized to ensure that surveys remain non-identifiable. The process of prototyping, developing, and iterating the gamified activities through usability testing is described elsewhere [48]. Usability testing is distinct from cognitive testing, as the focus will be on the usability of the online survey (e.g., how well the gamified activities are received by a diverse sample to represent stakeholders that may attend the PSM workshops) [49].
Within the online surveys, two activities will be gamified, specifically social network analysis and patient journey mapping. Social network analysis is a methodology to quantitatively measure and visually analyze social relationships and how they change over time [50,51]. As online surveys will be configured so that questions can be personalized to the participant depending on how they have identified themselves (e.g., young person vs. professional), only the participants who have identified as working in a professional capacity in the youth mental health or broader social system will be asked to complete questions related to social networks, with the aim to measure if interdisciplinary collaboration has changed (i.e., improved or been made worse) as a result of the PSM process. The customization of survey questions to particular demographic groups ensures that the questions are relevant and minimizes respondent confusion or fatigue [52]. A preview of the gamified social network analysis activity is shown in Figure 2.
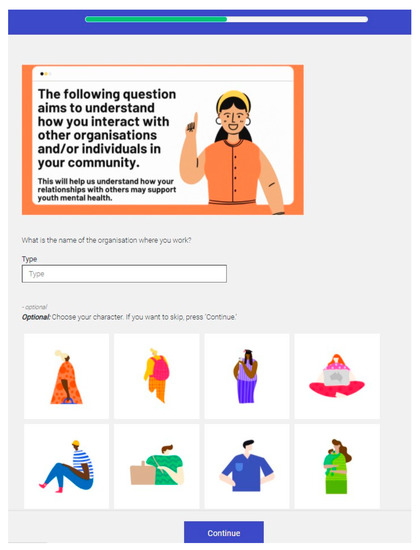
Figure 2.
Preview of the gamified social network analysis activity to measure if interdisciplinary collaboration has changed (i.e., improved or been made worse) as a result of the PSM process.
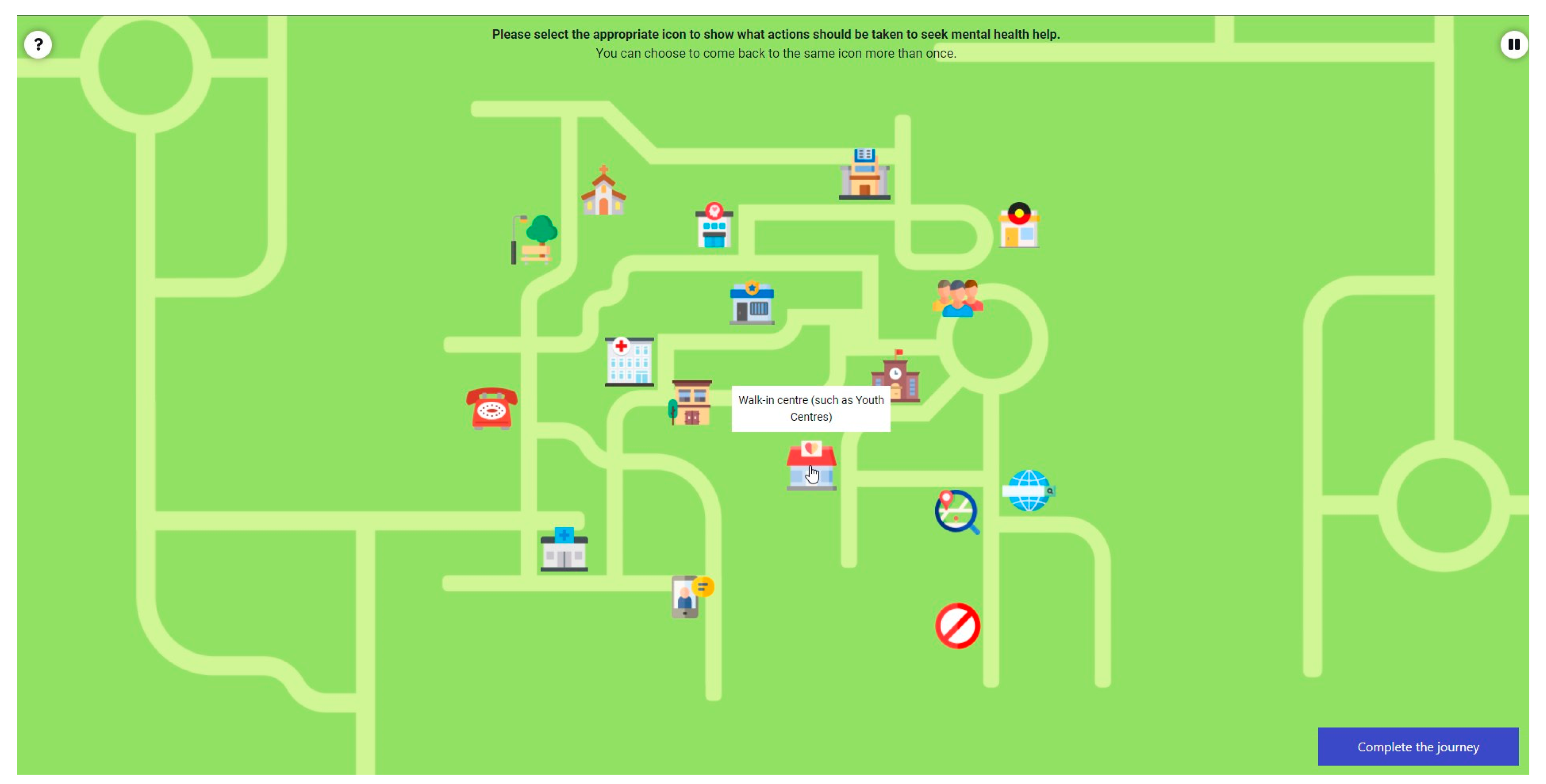
To understand how young people navigate the local youth mental health system at each participating site—and to uncover the potential strengths and challenges of the system—a patient journey mapping activity will be included within the online surveys. All participants will be presented with up to two vignettes that describe young people who are seeking mental health care. Using these two case studies, respondents will be asked to participate in a ‘complete the story’ activity and map out how a typical journey might look if the young person were to seek help and navigate their community’s youth mental health system. Participants can also optionally share their own personal experiences of navigating their community’s mental health system. Importantly, respondents will have the option to freely choose which story they would like to explore (i.e., fictional case study vs. personal experience). The patient journey mapping activity is followed by additional survey questions regarding the current gaps in the community’s mental health services, such as waiting times to make an appointment with the local youth mental health care service(s). The patient journey mapping activity will be included for both the baseline and follow-up surveys to understand if participants’ contributions to the PSM workshops led to any changes in perceived knowledge, beliefs, assumptions, or engagement behaviors with the local mental health system. Figure 3 shows a preview of the patient journey mapping activity.
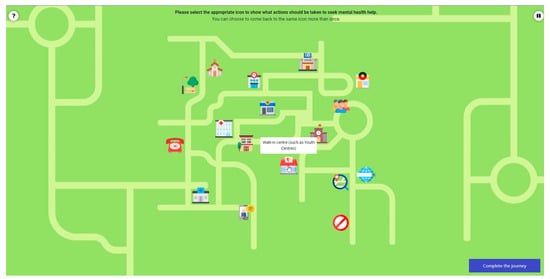
Figure 3.
Preview of the patient journey mapping activity. Respondents will explore a fictional case study or will share their own personal experiences of how young people seek help and navigate their community’s youth mental health system.
All participants will also be asked to complete a series of questions within the online surveys to rate the importance of youth mental health interventions. Through these questions, data will be analyzed to understand the similarities and differences among participants across the system before and after participating in the PSM workshops (e.g., measuring any convergence toward consensus) to specifically understand how the ratings of importance become more targeted and in line with what the final systems model is indicating are the best interventions options (i.e., measuring systems learning).
Box 1 provides example questions from the online survey. The complete baseline and follow-up online surveys have been provided as Supplementary Materials.
- Semi-Structured Interviews
Participants invited to the PSM workshops will be asked to participate in one-on-one interviews using questions adapted from Freebairn et al. [2] aligned to the time points for the online surveys (i.e., 1 month before the first PSM workshop, immediately after the last PSM workshop, and 6 months following the last PSM workshop). Interviews will take up to 1 h and conducted either face to face or via appropriate telecommunication tools (such as videoconferencing). Semi-structured interviews will be conducted to understand any detected change (or lack thereof) in participant perspectives regarding the current challenges and priorities of youth mental health services in their local communities, their experiences with and roles within their local community’s youth mental health and broader social systems, their previous experiences co-designing systems models, their experience of participating in this research Program, and their experience using (or their experience contributing to the development of) the systems model as a decision support tool in their community. Recruitment will continue until thematic saturation is achieved across the participant subgroups. Qualitative data collected from the interviews will be cross-verified with the quantitative data collected via the online surveys as a means to triangulate and validate data, forming a richer understanding of participants’ experience engaged in the PSM process. For example, questions regarding interdisciplinary collaboration probed during the interviews will be used to cross-check data from the online survey responses to conduct the social network analysis. An excerpt example of the semi-structured interview questions is provided in Box 2. The full baseline and follow-up semi-structured interview guides are provided as Supplementary Materials.
Box 1. Example questions from the online survey.
Topic: Expectations for the research Program
* Questions in this topic elicit understanding of the ‘Value’ category of the comprehensive multi-scale evaluation framework.
What do you hope will be the benefits of the systems model ‘what if’ tool for your community? Please select all that apply:
- ☐
- Improve the health and wellbeing of young people in my community
- ☐
- Assist in making better decisions to improve youth mental health treatments or programs
- ☐
- Address the current gaps in my community’s youth mental health system
- ○
- If this option is ticked: What do you think are the current gaps that exist in your community’s youth mental health system (e.g., cannot get an appointment because of long wait lists)?
- ☐
- Improve my understanding of the youth mental health system in my community
- ☐
- Better navigate the mental health services or organizations in my community (e.g., to find the right care, to make correct referrals to other services, etc)
- ☐
- Other:
Box 2. Example questions used during a semi-structured interview.
Topic: Current youth mental health system
* Questions in this topic elicit understanding of the ‘Change and Action (Impact)’ and ‘Sustainability’ categories of the comprehensive multi-scale evaluation framework.
- Based on your experience, what are the current challenges of youth mental health care in your community?
- What do you think is driving these challenges?
- What changes do you think are required to improve youth mental health care?
- Why do you think these changes have not yet been implemented?
2.6. Data Analysis Plan
Online survey analysis: Statistical analysis methods such as multilevel regression modelling will be used to assess the impact of time (baseline, first follow-up, and final follow-up) on the dependent variables, including participants’ attitudes regarding the feasibility of the PSM process, participants’ attitudes regarding the value of the PSM process, and changes in participants’ attitudes or actions (e.g., improved consensus of participants) due to the PSM process.
One-on-one interview analysis: A thematic analysis of qualitative data will be conducted to identify patterns or themes, guided by the approach described by Braun and Clarke [53,54]. An iterative process of descriptive coding and analytical memos will also be adopted to identify themes and categories [55]. Interview data will be coded and cross-checked by a senior researcher to assess interrater reliability, which will also be iteratively reviewed by senior members of the research team. Relevant computer software may be used, such as professional transcription tools (e.g., Rev Speech-to-Text), in addition to standard Microsoft packages including Excel and Word.
Social network analysis: Qualitative and quantitative data collected through online surveys and semi-structured interviews will be considered when conducting the social network analysis. Researcher observations, field notes, as well as Program outputs from the PSM process may also be used to further validate and contextualize the social network analysis. Visual analysis or mapping the identified social networks via algorithm-generated network diagrams will be completed using appropriate computer software packages such as Gephi [56]. Through this analysis, several ways to examine social connections can be considered, such as connectedness (number of connections one node—or actor that makes up the network—has to other nodes), reciprocity (level to which the connection is reciprocal), and propinquity (degree to which individuals have more ties with people geographically close to them) [57].
Patient journey mapping: Qualitative analysis will be conducted utilizing data collected from the gamified patient journey mapping exercise within the online survey. Data collected via researcher observations and field notes from the PSM process may also be used to further validate the data. Thematic analysis will be conducted to identify patterns or themes regarding whether participants’ contributions to the PSM process led to changes in perceived knowledge, beliefs, assumptions, or engagement behaviors with the local youth mental health system at each participating site.
Prioritizing interventions in the youth mental health system: Data will be analyzed to understand the similarities and differences among participants across the system before and after participating in the PSM process (e.g., assessing convergence between respondents), as well as to understand and measure any change in participants’ beliefs of the priority of importance and funding allocations of youth mental health interventions (e.g., convergence with insights from the systems model to indicate systems learning).
Prospective evaluation of impact using the systems models: The technical systems model that will be the final output of the PSM process will also provide analytic capacity. This will allow researchers and end users to simulate and track (and thus prospectively monitor and evaluate) both short- and long-term impacts, including but not limited to identifying unintended consequences through modelling as well as how suggested interventions of the systems model might impact outcomes such as death by suicide.
Analysis of other sources of data: In addition to cross-validating data collected from the online surveys and interviews, qualitative data collected via researcher observations and recordings from the PSM workshops, meetings with local stakeholders outside of the workshops, reflections, and field notes will be analyzed as part of the ongoing reflection cycle enabled by PAR. Specifically, researchers will work collaboratively with the local site to engage in ongoing planning, action (iteration), reflection, and observation throughout the evaluation process with the aim of improving the methods and outcomes of PSM.
2.7. Data Storage and Security
All data will be securely stored in accordance with The University of Sydney’s data management procedures [38,39]. The importance of data sovereignty is recognized when working with Aboriginal and Torres Strait Islander people [40,41]. Where relevant, a data governance framework will be established through a consultative process at an early stage to allow for sufficient time to work with the participating site and their respective Aboriginal governance councils.
3. Discussion
Evaluations are crucial for determining whether the postulated benefits of PSM are realized and to inform refinements to the process as needed throughout all stages of the Program [26,58,59]. This novel study is the first to apply a comprehensive multi-scale evaluation framework. The feasibility, value, impact (change or action), and sustainability that is achieved among the participants as a result of the PSM process for the Right care, first time, where you live Program will be assessed.
A novel mixed methods approach is described to evaluate the PSM component of the Program. This approach facilitates participant engagement at various levels by providing different mechanisms for participants to contribute. Specifically, a mixed methods approach creates the opportunity for participants to contribute their more in-depth experiences through a 60-min interview and conversely creates the opportunity for participants to contribute to a less onerous 15-min online survey [60]. As it is more difficult to elicit in-depth thinking within online surveys compared with semi-structured interviews (i.e., where researchers have the opportunity to probe), the online survey questions have been purposefully designed to encourage engagement as well as in-depth participant thinking through gamification.
The incorporations of gamification, patient journey mapping, and social network analysis as part of the evaluation process are novel features. Though gamification of online surveys has been conducted in many disciplines [47,61], it has not yet been considered in PSM evaluation to our knowledge. Aside from increasing participant engagement, the approach of gamifying survey questions has many benefits, such as increasing motivation and enjoyment to complete an activity [61]. This approach can also empower participants, particularly more vulnerable groups, to share their experiences in more detail, facilitated by visual, non-text cues as opposed to just presenting participants with traditional survey methods such as multi-response questions [62].
The patient journey mapping activity, which is widely conducted to help understand how patients interact with health services or the broader social system throughout their care journey [63], will yield data that can be analyzed to observe changes to how participants viewed the local youth mental health systems (e.g., challenges, strengths, priorities, etc.) before and after the PSM process. In addition, data from the patient journey mapping activity can inform the PSM process to facilitate discussion points around system challenges and address any discrepancies during the PSM workshops, as well as inform the design of the systems model (e.g., contextualizing it in the local system context) [64].
Social network analysis has not previously been applied to understand the changes in interdisciplinary collaboration among participants as a result of the PSM process, despite the general acceptance that PSM can promote knowledge exchange and facilitate interdisciplinary collaboration between participants [28,32]. Toward this end, a visual map of the social network will be developed at three time points to measure how local social networks changed over the PSM process.
A PAR approach allows for the evaluation processes to be embedded within program planning, iteration, reflection, and observation. PAR aims to improve equitable health and social practice, enable authentic participation and collaboration, and empower individuals to improve their knowledge to facilitate measurable change [65]. Embedding PAR throughout the Program creates a culture of equality when engaging with diverse stakeholders to ensure that the local systems model is developed collaboratively, therefore increasing stakeholders’ assurance of the credibility of the systems model. PAR can also facilitate stakeholder learning, ensuring insights from the final decision support tool can be easily understood by diverse subgroups. This study also incorporates evaluation processes ex ante (before), ex durante (during), and ex post (after) to ensure that reflective evaluation processes are considered throughout all phases of the Program to improve the PSM process in the current research study, as well as to provide researchers with a flexible blueprint for implementation and replication in diverse contexts [59].
4. Ethics and Dissemination
The described evaluation study protocol has been reviewed and approved by the Sydney Local Health District Human Research Ethics Committee (HREC; Protocol No. X21-0151 and 2021/ETH00553). Any modifications to the study protocol will only be implemented after HREC approval.
The results of this evaluation study will be published in peer-reviewed journals and policy documents and may be presented at both domestic and international scientific meetings. The results may also be communicated directly to the wider local community, such as through public presentations and podcasts. All dissemination of findings will only report aggregate, non-identifiable data.
5. Conclusions and Future Directions
An innovative evaluation study is described, in which the combination of PSM and novel evaluation tools using gamification will be deployed for the first time in the complex decision-making environment of youth mental health systems. The knowledge generated by this evaluation study will uncover the social and technical opportunities arising from PSM processes (e.g., measuring individual, group, and system changes to understand the value of adopting a participatory approach when developing systems models). The evaluation study will also provide insight into the challenges of implementing these interdisciplinary methods in complex settings to improve youth mental health policy, planning, and outcomes.
Though described in the context of a youth mental health PSM program in Australia, the comprehensive multi-scale evaluation framework can be applied internationally across diverse disciplines and modelling methods. Adopting such an evaluation approach will likely lead to local capacity building, thus improving the methods to explore and address complex systems challenges through stakeholder understanding, consensus building, and collaborative action, all of which underpin genuine individual and community empowerment.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ijerph19074015/s1. The full versions of the baseline and follow-up online surveys, as well as the interview guides are enclosed.
Author Contributions
G.Y.L. prepared the original draft of the manuscript and designed the study with academic oversight from L.F.; I.B.H., J.-A.O. and Y.J.C.S. substantially contributed to the conceptualization of the study, including acquisition of the research Program funding. S.C., A.S., K.L., S.J.H. and A.M.H. contributed to the review and editing of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was conducted under the Brain and Mind Centre’s Right care, first time, where you live Program, enabled by an AUD 12.8 million partnership with the BHP Foundation. The Program will develop infrastructure to support decisions relating to advanced mental health and guide investments and actions to foster the mental health and wellbeing of young people in their communities.
Institutional Review Board Statement
The described evaluation study protocol was reviewed and approved by the Sydney Local Health District Human Research Ethics Committee on 5 July 2021 (HREC; Protocol No. X21-0151 & 2021/ETH00553).
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors would like to thank the Youth Lived Experience Working Group at The University of Sydney’s Brain and Mind Centre (Jessica Cottle, Skye Choi, Alexis Hutcheon, Samuel J Hockey, Rachael Laidler, Tara Lindsay-Smith, Claudia Perry, Anith Mukherjee, Joshua New, and Annabel Ramsay) for their contributions in giving insightful feedback on the evaluation tools.
Conflicts of Interest
I.B.H. is the Co-Director of the Health and Policy at the Brain and Mind Centre (BMC) at The University of Sydney. The BMC operates an early intervention youth services at Camperdown under contract to headspace. He is the Chief Scientific Advisor to, and a 5% equity shareholder in, InnoWell Pty Ltd. InnoWell was formed by The University of Sydney (45% equity) and PwC (Australia, 45% equity) to deliver the AUD 30 million Australian government-funded Project Synergy (2017–20, a 3-year program for the transformation of mental health services) and to lead transformation of mental health services internationally through the use of innovative technologies. J.O. is both Head of Systems Modelling, Simulation & Data Science at The University of Sydney’s Brain and Mind Centre and Managing Director of Computer Simulation & Advanced Research Technologies (CSART). L.F. is currently employed part-time by the Brain and Mind Centre at The University of Sydney, ACT Health as Director of Knowledge Translation and Health Outcomes in the Epidemiology Section, and ACT Health and CSART as Director of Policy Applications & Translational Science. No other authors declare any conflict of interests. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Apostolopoulos, Y.; Lich, K.H.; Lemke, M.K. Complex Systems and Population Health; Oxford University Press, Incorporated: London, UK, 2020. [Google Scholar]
- Freebairn, L.; Atkinson, J.; Kelly, P.; McDonnell, G.; Rychetnik, L. Simulation modelling as a tool for knowledge mobilisation in health policy settings: A case study protocol. Health Res. Policy Syst. 2016, 14, 71. [Google Scholar] [CrossRef] [Green Version]
- Moth, R.; Greener, J.; Stoll, T. Crisis and resistance in mental health services in England. Crit. Radic. Soc. Work 2015, 3, 89–101. [Google Scholar] [CrossRef]
- Klaus, H.; Franz-Xaver, K.; Friedrich, L. Social Intervention; De Gruyter: Berlin, Germany; Boston, MA, USA, 2014. [Google Scholar] [CrossRef]
- Kohrt, B.A.; Asher, L.; Bhardwaj, A.; Fazel, M.; Jordans, M.J.; Mutamba, B.B.; Nadkarni, A.; Pedersen, G.A.; Singla, D.R.; Patel, V. The Role of Communities in Mental Health Care in Low- and Middle-Income Countries: A Meta-Review of Components and Competencies. Int. J. Environ. Res. Public Health 2018, 15, 1279. [Google Scholar] [CrossRef] [Green Version]
- Lee, B.; Choi, M.; Choi, M. Evaluation of Individual and Community Factors Affecting Adolescents’ Mental Health: A Longitudinal Multilevel Analysis. Appl. Res. Qual. Life 2021, 16, 1187–1203. [Google Scholar] [CrossRef]
- Erskine, H.E.; Moffitt, T.E.; Copeland, W.E.; Costello, E.J.; Ferrari, A.J.; Patton, G.; Degenhardt, L.; Vos, T.; Whiteford, H.A.; Scott, J.G. A heavy burden on young minds: The global burden of mental and substance use disorders in children and youth. Psychol. Med. 2015, 45, 1551–1563. [Google Scholar] [CrossRef] [Green Version]
- Adolescent Mental Health: World Health Organization. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health (accessed on 8 August 2021).
- Malla, A.; Shah, J.; Iyer, S.; Boksa, P.; Joober, R.; Andersson, N.; Lal, S.; Fuhrer, R. Youth Mental Health Should Be a Top Priority for Health Care in Canada. Can. J. Psychiatry 2018, 63, 216–222. [Google Scholar] [CrossRef] [Green Version]
- Rosenberg, S.; Harvey, C. Mental Health in Australia and the Challenge of Community Mental Health Reform. Consort. Psychiatr. 2021, 2, 40–46. [Google Scholar] [CrossRef]
- National Mental Health Commission. Report of the National Review of Mental Health Programmes and Services; NMHC: Sydney, Australia, 2014. [Google Scholar]
- Groom, G.; Hickie, I.B.; Davenport, T. ‘Out of Hospital, Out of Mind!’: A Report Detailing Mental Health Services in Australia in 2002 and Community Priorities for National Mental Health Policy in 2003–2008; Mental Health Council of Australia: Canberra, Australia, 2003. [Google Scholar]
- Hickie, I.B.; Scott, E.M.; Cross, S.P.; Iorfino, F.; Davenport, T.A.; Guastella, A.J.; Naismith, S.L.; Carpenter, J.S.; Rohleder, C.; Crouse, J.J.; et al. Right care, first time: A highly personalised and measurement-based care model to manage youth mental health. Med. J. Aust. 2019, 211 (Suppl. 9), S3–S46. [Google Scholar] [CrossRef] [Green Version]
- Rosenberg, S.; Hickie Am, I. Making better choices about mental health investment: The case for urgent reform of Australia’s Better Access Program. Aust. N. Z. J. Psychiatry 2019, 53, 1052–1058. [Google Scholar] [CrossRef]
- Grace, F.C.; Meurk, C.S.; Head, B.W.; Hall, W.D.; Harris, M.G.; Whiteford, H.A. An analysis of policy success and failure in formal evaluations of Australia’s national mental health strategy (1992–2012). BMC Health Serv. Res. 2017, 17, 374. [Google Scholar] [CrossRef] [Green Version]
- Atkinson, J.-A.; Wells, R.; Page, A.; Dominello, A.; Haines, M.; Wilson, A. Applications of system dynamics modelling to support health policy. Public Health Res. Pract. 2016, 9, e2531531. [Google Scholar] [CrossRef]
- Occhipinti, J.A.; Skinner, A.; Iorfino, F.; Lawson, K.; Sturgess, J.; Burgess, W.; Davenport, T.; Hudson, D.; Hickie, I. Reducing youth suicide: Systems modelling and simulation to guide targeted investments across the determinants. BMC Med. 2021, 19, 61. [Google Scholar] [CrossRef]
- Atkinson, J.A.; Skinner, A.; Hackney, S.; Mason, L.; Heffernan, M.; Currier, D.; King, K.; Pirkis, J. Systems modelling and simulation to inform strategic decision making for suicide prevention in rural New South Wales (Australia). Aust. N. Z. J. Psychiatry 2020, 54, 892–901. [Google Scholar] [CrossRef]
- Atkinson, J.-A.; Skinner, A.; Lawson, K.; Rosenberg, S.; Hickie, I.B. Bringing new tools, a regional focus, resource-sensitivity, local engagement and necessary discipline to mental health policy and planning. BMC Public Health 2020, 20, 814. [Google Scholar] [CrossRef]
- Senge, P.M.; Sterman, J.D. Systems thinking and organizational learning: Acting locally and thinking globally in the organization of the future. Eur. J. Oper. Res. 1992, 59, 137–150. [Google Scholar] [CrossRef]
- Hoang, V.P.; Shanahan, M.; Shukla, N.; Perez, P.; Farrell, M.; Ritter, A. A systematic review of modelling approaches in economic evaluations of health interventions for drug and alcohol problems. BMC Health Serv. Res. 2016, 16, 127. [Google Scholar] [CrossRef] [Green Version]
- Long, K.M.; Meadows, G.N. Simulation modelling in mental health: A systematic review. J. Simul. 2018, 12, 76–85. [Google Scholar] [CrossRef]
- Rutter, H.; Savona, N.; Glonti, K.; Bibby, J.; Cummins, S.; Finegood, D.T.; Greaves, F.; Harper, L.; Hawe, P.; Moore, L.; et al. The need for a complex systems model of evidence for public health. Lancet 2017, 390, 2602–2604. [Google Scholar] [CrossRef] [Green Version]
- Waterlander, W.E.; Luna Pinzon, A.; Verhoeff, A.; den Hertog, K.; Altenburg, T.; Dijkstra, C.; Halberstadt, J.; Hermans, R.; Renders, C.; Seidell, J.; et al. A System Dynamics and Participatory Action Research Approach to Promote Healthy Living and a Healthy Weight among 10–14-Year-Old Adolescents in Amsterdam: The LIKE Programme. Int. J. Environ. Res. Public Health 2020, 17, 4928. [Google Scholar] [CrossRef]
- Occhipinti, J.-A.; Lawson, K.; Skinner, A.; Hickie, I. Road to Recovery, Part 2: Investing in Australia’s Mental Wealth; The University of Sydney: Sydney, Australia, 2020. [Google Scholar]
- Hamilton, S.H.; Fu, B.; Guillaume, J.H.; Badham, J.; Elsawah, S.; Gober, P.; Hunt, R.J.; Iwanaga, T.; Jakeman, A.J.; Ames, D.P.; et al. A framework for characterising and evaluating the effectiveness of environmental modelling. Environ. Model. Softw. 2019, 118, 83–98. [Google Scholar] [CrossRef] [Green Version]
- Hedelin, B.; Evers, M.; Alkan-Olsson, J.; Jonsson, A. Participatory modelling for sustainable development: Key issues derived from five cases of natural resource and disaster risk management. Environ. Sci. Policy 2017, 76, 185–196. [Google Scholar] [CrossRef]
- Voinov, A.; Bousquet, F. Modelling with stakeholders. Environ. Model. Softw. 2010, 25, 1268–1281. [Google Scholar] [CrossRef]
- Right Care, First Time, Where You Live. The University of Sydney. 2021. Available online: https://www.sydney.edu.au/brain-mind/our-research/youth-mental-health-and-technology/right-care-first-time-where-you-live-program.html (accessed on 8 August 2021).
- Occhipinti, J.A.; Skinner, A.; Freebairn, L.; Song, Y.J.; Ho, N.; Lawson, K.; Lee, G.Y.; Hickie, I.B. Which Social, Economic, and Health Sector Strategies Will Deliver the Greatest Impacts for Youth Mental Health and Suicide Prevention? Protocol for an Advanced, Systems Modelling Approach. Front. Psychiatry 2021, 12, 1760. [Google Scholar] [CrossRef]
- Freebairn, L.; Occhipinti, J.A.; Song, Y.J.; Skinner, A.; Lawson, K.; Lee, G.Y.; Hockey, S.J.; Huntley, S.; Hickie, I.B. Participatory Methods for Systems Modeling of Youth Mental Health: Implementation Protocol. JMIR Res. Protoc. 2022, 11, e32988. [Google Scholar] [CrossRef]
- Freebairn, L.; Atkinson, J.-A.; Kelly, P.M.; McDonnell, G.; Rychetnik, L. Decision makers’ experience of participatory dynamic simulation modelling: Methods for public health policy. BMC Med. Inf. Decis. Mak. 2018, 18, 131. [Google Scholar] [CrossRef]
- McTaggart, R. Principles for Participatory Action Research. Adult Educ. Q. 1991, 41, 168–187. [Google Scholar] [CrossRef]
- Freebairn, L. “Turning Mirrors into Windows”: A Study of Participatory Dynamic Simulation Modelling to Inform Health Policy Decisions; The University of Notre Dame Australia: Sydney, Australia, 2019. [Google Scholar]
- Holt, C.L.; Chambers, D.A. Opportunities and challenges in conducting community-engaged dissemination/implementation research. Transl. Behav. Med. 2017, 7, 389–392. [Google Scholar] [CrossRef] [Green Version]
- Murphy, J.; Qureshi, O.; Endale, T.; Esponda, G.M.; Pathare, S.; Eaton, J.; De Silva, M.; Ryan, G. Barriers and drivers to stakeholder engagement in global mental health projects. Int. J. Ment. Health Syst. 2021, 15, 30. [Google Scholar] [CrossRef]
- National Health and Medical Research Council. National Statement on Ethical Conduct in Human Research 2007 (Updated 2018); NHMRC: Canberra, Australia, 2018.
- The University of Sydney. Research Data Management Procedures 2015; The University of Sydney: Sydney, Australia, 2020. [Google Scholar]
- Cogniss Privacy Policy. Available online: https://www.cogniss.com/privacy-policy (accessed on 5 April 2021).
- National Health and Medical REsearch Council. Ethical Conduct in Research with Aboriginal and Torres Strait Islander Peoples and Communities: Guidelines for Researchers and Stakeholders; NHMRC: Canberra, Australia, 2018.
- Australian Institute of Aboriginal and Torres Strait Islander Studies. AIATSIS Code of Ethics for Aboriginal and Torres Strait Islander Research; AIATSIS: Canberra, Australia, 2020.
- The Productivity Commission. Indigenous Evaluation Strategy; Productivity Commission: Canberra, Australia, 2020.
- Butler, M.; McCreedy, E.; Schwer, N.; Burgess, D.; Call, K.; Przedworski, J. AHRQ Comparative Effectiveness Reviews. In Improving Cultural Competence to Reduce Health Disparities; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2016. [Google Scholar]
- Torrance, H. Triangulation, Respondent Validation, and Democratic Participation in Mixed Methods Research. J. Mix. Methods Res. 2012, 6, 111–123. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Appendix 4: Cognitive Testing Interview Guide; CDC: Atlanta, GA, USA.
- About Our Story: Cogniss n.d. Available online: https://www.cogniss.com/our-story (accessed on 5 April 2021).
- Harms, J.; Biegler, S.; Wimmer, C.; Kappel, K.; Grechenig, T. (Eds.) Gamification of Online Surveys: Design Process, Case Study, and Evaluation. In Human-Computer Interaction—INTERACT; Springer International Publishing: Cham, Switzerland, 2015; pp. 219–236. [Google Scholar]
- Lee, G.Y.; Hickie, I.B.; Occhipinti, J.; Song, Y.J.C.; Huntley, S.; Skinner, A.; Lawson, K.; Hockey, S.J.; Freebairn, L. Prototyping, developing, and iterating a gamified survey to evaluate participatory systems modelling for youth mental health: Quality assurance pilot. In Proceedings of the 24th International Congress on Modelling and Simulation, Sydney, Australia, 5–10 December 2021. [Google Scholar]
- Pagulayan, R.J.; Steury, K.R.; Fulton, B.; Romero, R.L. Designing for Fun: User-Testing Case Studies. In Funology 2 Human–Computer Interaction Series; Blythe, M.A., et al., Eds.; Springer: Dordrecht, The Netherlands, 2018. [Google Scholar] [CrossRef]
- North Carolina Prepardness and Emergency Response Research Center. Addressing Public Health Issues with Social Network Analysis; The University of North Carolina: Chapel Hill, NC, USA, 2011. [Google Scholar]
- Nicaise, P.; Tulloch, S.; Dubois, V.; Matanov, A.; Priebe, S.; Lorant, V. Using social network analysis for assessing mental health and social services inter-organisational collaboration: Findings in deprived areas in Brussels and London. Adm. Policy Ment. Health 2013, 40, 331–339. [Google Scholar] [CrossRef]
- Helms, C.; Gardner, A.; McInnes, E. The use of advanced web-based survey design in Delphi research. J. Adv. Nurs. 2017, 73, 3168–3177. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Clarke, V.; Braun, V. Successful Qualitative Research: A Practical Guide for Beginners; Sage: London, UK, 2013. [Google Scholar]
- Saldaña, J. Coding and Analysis Strategies In The Oxford Handbook of Qualitative Research, 1st ed.; Leavy, P., Ed.; Oxford University Press: London, UK, 2014. [Google Scholar] [CrossRef]
- Leppin, A.L.; Okamoto, J.M.; Organick, P.W.; Thota, A.D.; Barrera-Flores, F.J.; Wieland, M.L.; McCoy, R.G.; Bonacci, R.P.; Montori, V.M. Applying Social Network Analysis to Evaluate Implementation of a Multisector Population Health Collaborative That Uses a Bridging Hub Organization. Front. Public Health 2018, 6, 315. [Google Scholar] [CrossRef]
- National Center for Research in Advanced Information and Digital Technologies. Planning a Social Network Analysis; Digital Promise: Washington, DC, USA, 2018. [Google Scholar]
- Smajgl, A.; Ward, J. Evaluating participatory research: Framework, methods and implementation results. J. Environ. Manag. 2015, 157, 311–319. [Google Scholar] [CrossRef]
- Zare, F.; Guillaume, J.H.; ElSawah, S.; Croke, B.; Fu, B.; Iwanaga, T.; Merritt, W.; Partington, D.; Ticehurst, J.; Jakeman, A.J. A formative and self-reflective approach to monitoring and evaluation of interdisciplinary team research: An integrated water resource modelling application in Australia. J. Hydrol. 2021, 596, 126070. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V.; Boulton, E.; Davey, L.; McEvoy, C. The online survey as a qualitative research tool. Int. J. Soc. Res. Methodol. 2021, 24, 641–654. [Google Scholar] [CrossRef]
- Bakhanova, E.; Garcia, J.A.; Raffe, W.L.; Voinov, A. Targeting social learning and engagement: What serious games and gamification can offer to participatory modeling. Environ. Model. Softw. 2020, 134, 104846. [Google Scholar] [CrossRef]
- van der Lubbe, L.M.; Gerritsen, C.; Klein, M.C.A.; Hindriks, K.V. Empowering vulnerable target groups with serious games and gamification. Entertain. Comput. 2021, 38, 100402. [Google Scholar] [CrossRef]
- Maddox, K.; Baggetta, D.; Herout, J.; Ruark, K. Lessons Learned from Journey Mapping in Health Care. Proc. Int. Symp. Hum. Factors Ergon. Health Care 2019, 8, 105–109. [Google Scholar] [CrossRef]
- Tilleczek, K.C.; Bell, B.L.; Munro, M.A.; Gallant, S.D. Youth Journeys in Mental Health: Invoking Unique Patient Perspectives. Can. J. Community Ment. Health 2017, 36, 151–164. [Google Scholar] [CrossRef] [Green Version]
- MacDonald, C. Understanding participatory action research: A qualitative research methodology option. Can. J. Action Res. 2012, 13, 34–50. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).