The Utility of Ambulance Dispatch Call Syndromic Surveillance for Detecting and Assessing the Health Impact of Extreme Weather Events in England
Abstract
:1. Introduction
2. Materials and Methods
3. Results
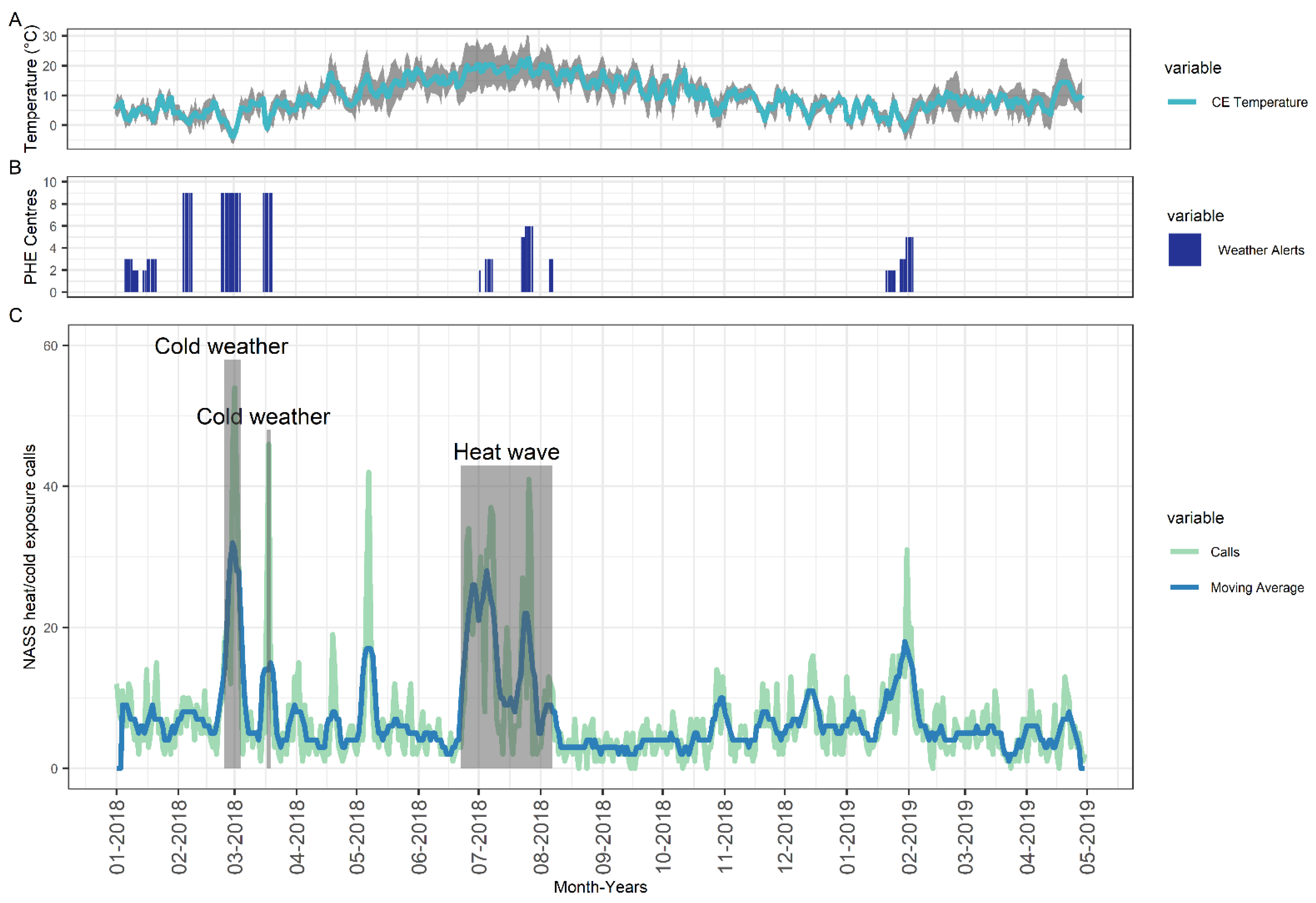
3.1. System Description
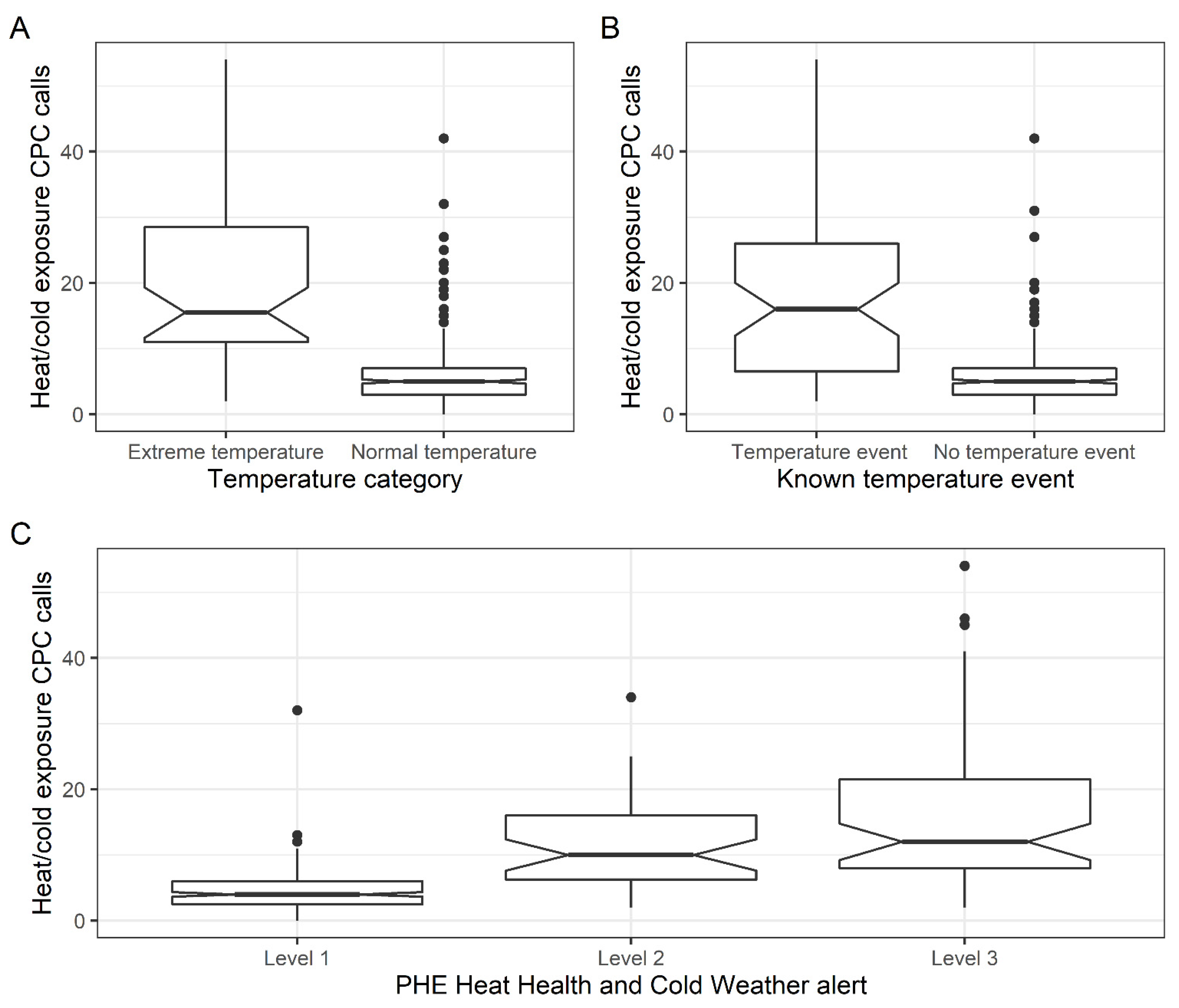
3.2. NASS Heat and Cold Exposure CPC Relationship with Extreme Temperature
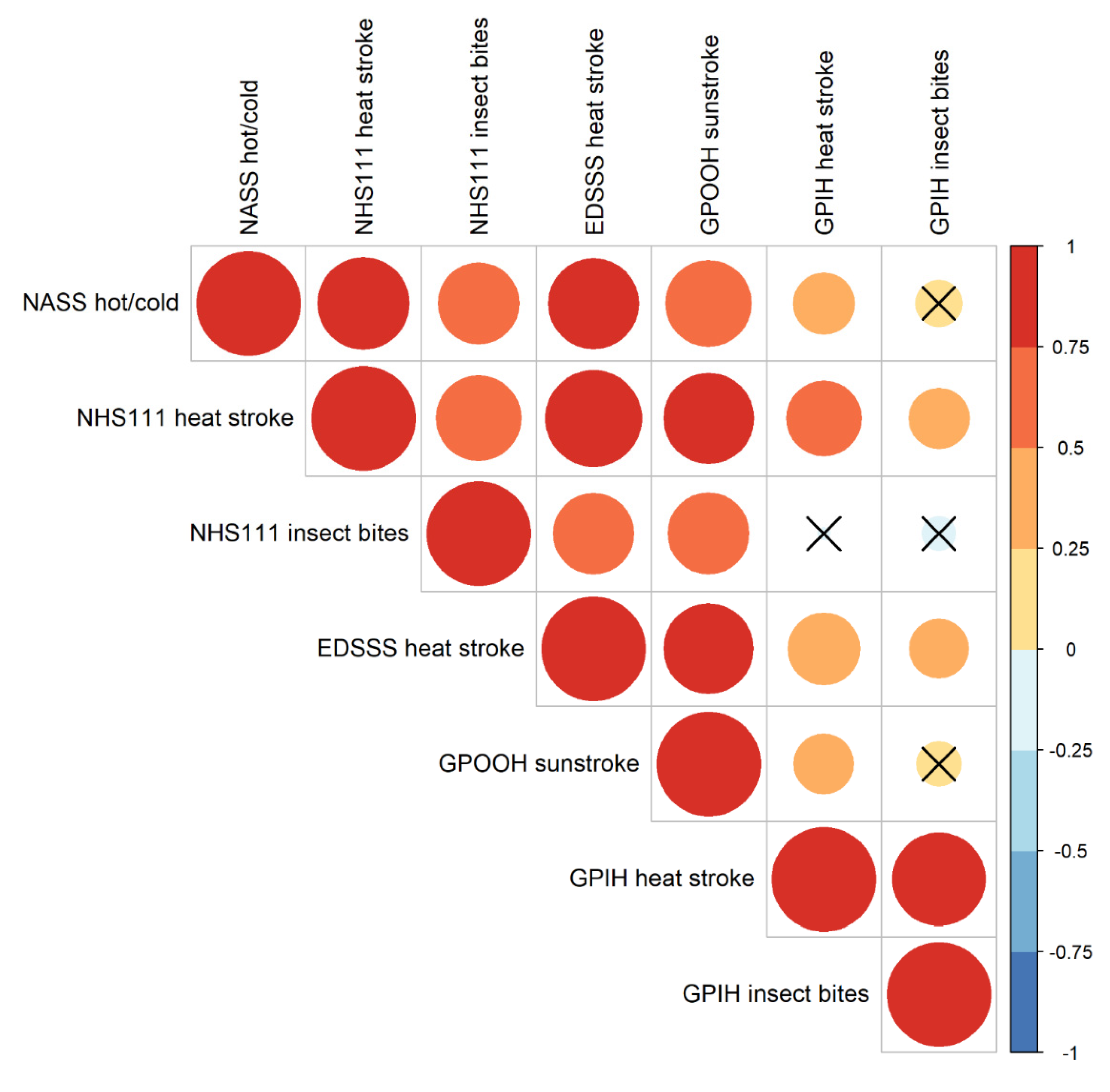
3.3. NASS Heat and Cold Exposure CPC Relationship with Other Syndromic Surveillance Systems
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Climate Change and Human Health: Risks and Responses; World Health Organization: Geneva, Switzerland, 2003; ISBN 9241590815. [Google Scholar]
- Melillo, J.M.; Richmond, T.; Yohe, G.W. Climate Change Impacts in the United States: The Third National Climate Assessment; U.S. Global Change Research Program: Washington, DC, USA, 2014. [Google Scholar]
- Doherty, R.M.; Heal, M.R.; Wilkinson, P.; Pattenden, S.; Vieno, M.; Armstrong, B.; Atkinson, R.; Chalabi, Z.; Kovats, S.; Milojevic, A.; et al. Current and future climate- and air pollution-mediated impacts on human health. Environ. Health 2009, 8, S8. [Google Scholar] [CrossRef] [Green Version]
- Whitman, S.; Good, G.; Donoghue, E.R. Mortality in Chicago attributed to the July 1995 heat wave. Am. J. Public Health 1997, 87, 1515–1518. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fouillet, A.; Rey, G.; Laurent, F.; Pavillon, G.; Bellec, S.; Guihenneuc-Jouyaux, C.; Clavel, J.; Jougla, E.; Hémon, D. Excess mortality related to the August 2003 heat wave in France. Int. Arch. Occup. Environ. Health 2006, 80, 16–24. [Google Scholar] [CrossRef] [Green Version]
- Kyselý, J.; Kim, J. Mortality during heat waves in South Korea, 1991 to 2005: How exceptional was the 1994 heat wave? Clim. Res. 2009, 38, 105–116. [Google Scholar]
- Johnson, H.; Kovats, R.S.; McGregor, G.; Stedman, J.; Gibbs, M.; Walton, H. The impact of the 2003 heat wave on daily mortality in England and Wales and the use of rapid weekly mortality estimates. Euro Surveill. 2005, 10, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, T.; Hu, M.; Zeng, W.; Zhang, Y.; Rutherford, S.; Lin, H.; Xiao, J.; Yin, P.; Liu, J.; et al. The impact of cold spells on mortality and effect modification by cold spell characteristics. Sci. Rep. 2016, 6, 38380. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Public Health England. Heatwave Plan for England. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/888668/Heatwave_plan_for_England_2020.pdf (accessed on 1 December 2021).
- Public Health England. The Cold Weather Plan for England. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1031106/UKHSA_Cold_Weather_Plan_for_England.pdf (accessed on 1 December 2021).
- Elliot, A.J.; Hughes, H.E.; Hughes, T.C.; Locker, T.E.; Shannon, T.; Heyworth, J.; Wapling, A.; Catchpole, M.; Ibbotson, S.; McCloskey, B.; et al. Establishing an emergency department syndromic surveillance system to support the London 2012 Olympic and Paralympic Games. Emerg. Med. J. 2012, 29, 954–960. [Google Scholar] [CrossRef] [PubMed]
- Elliot, A.J.; Hughes, H.E.; Hughes, T.C.; Locker, T.E.; Brown, R.; Sarran, C.; Clewlow, Y.; Murray, V.; Bone, A.; Catchpole, M.; et al. The impact of thunderstorm asthma on emergency department attendances across London during July 2013. Emerg. Med. J. 2014, 31, 675–678. [Google Scholar] [CrossRef] [PubMed]
- Paterson, B.J.; Durrheim, D.N. The remarkable adaptability of syndromic surveillance to meet public health needs. J. Epidemiol. Glob. Health 2013, 3, 41–47. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duijster, J.W.; Doreleijers, S.D.A.; Pilot, E.; van der Hoek, W.; Kommer, G.J.; van der Sande, M.A.B.; Krafft, T.; van Asten, L.C.H.I. Utility of emergency call centre, dispatch and ambulance data for syndromic surveillance of infectious diseases: A scoping review. Eur. J. Public Health 2020, 30, 639–647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubman, D.I.; Matthews, S.; Heilbronn, C.; Killian, J.J.; Ogeil, R.P.; Lloyd, B.; Witt, K.; Crossin, R.; Smith, K.; Bosley, E.; et al. The National Ambulance Surveillance System: A novel method for monitoring acute alcohol, illicit and pharmaceutical drug related-harms using coded Australian ambulance clinical records. PLoS ONE 2020, 15, e0228316. [Google Scholar] [CrossRef]
- Todkill, D.; Loveridge, P.; Elliot, A.J.; Morbey, R.A.; Edeghere, O.; Rayment-Bishop, T.; Rayment-Bishop, C.; Thornes, J.E.; Smith, G. Utility of Ambulance Data for Real-Time Syndromic Surveillance: A Pilot in the West Midlands Region, United Kingdom. Prehosp. Disaster Med. 2017, 32, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Elliot, A.J.; Harcourt, S.E.; Hughes, H.E.; Loveridge, P.; Morbey, R.A.; Smith, S.; Soriano, A.; Bains, A.; Smith, G.E.; Edeghere, O.; et al. The COVID-19 pandemic: A new challenge for syndromic surveillance. Epidemiol. Infect. 2020, 148, e122. [Google Scholar] [CrossRef] [PubMed]
- Morbey, R.A.; Elliot, A.J.; Charlett, A.; Verlander, N.Q.; Andrews, N.; Smith, G.E. The application of a novel “rising activity, multi-level mixed effects, indicator emphasis” (RAMMIE) method for syndromic surveillance in England. Bioinformatics 2015, 31, 3660–3665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wei, T.; Simko, V. R Package “corrplot”: Visualization of a Correlation Matrix; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Harrell, F.E. [R] Hmisc: Harrell Miscellaneous. Available online: https://cran.r-project.org/package=Hmisc (accessed on 1 December 2021).
- R Core Team, R. A Language and Environment for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 1 December 2021).
- Curtis, S.; Fair, A.; Wistow, J.; Val, D.V.; Oven, K. Impact of extreme weather events and climate change for health and social care systems. Environ. Health 2017, 16, 128. [Google Scholar] [CrossRef] [Green Version]
- Harcourt, S.E.; Morbey, R.A.; Loveridge, P.; Carrilho, L.; Baynham, D.; Povey, E.; Fox, P.; Rutter, J.; Moores, P.; Tiffen, J.; et al. Developing and validating a new national remote health advice syndromic surveillance system in England. J. Public Health 2016, 39, fdw013. [Google Scholar] [CrossRef] [Green Version]
- Harcourt, S.E.; Fletcher, J.; Loveridge, P.; Bains, A.; Morbey, R.; Yeates, A.; McCloskey, B.; Smyth, B.; Ibbotson, S.; Smith, G.E.; et al. Developing a new syndromic surveillance system for the London 2012 Olympic and Paralympic Games. Epidemiol. Infect. 2012, 140, 2152–2156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith, G.E.; Elliot, A.J.; Ibbotson, S.; Morbey, R.; Edeghere, O.; Hawker, J.; Catchpole, M.; Endericks, T.; Fisher, P.; McCloskey, B. Novel public health risk assessment process developed to support syndromic surveillance for the 2012 Olympic and Paralympic Games. J. Public Health 2017, 39, e111–e117. [Google Scholar] [CrossRef] [Green Version]
- Lubman, D.I.; Heilbronn, C.; Ogeil, R.P.; Killian, J.J.; Matthews, S.; Smith, K.; Bosley, E.; Carney, R.; McLaughlin, K.; Wilson, A.; et al. National Ambulance Surveillance System: A novel method using coded Australian ambulance clinical records to monitor self-harm and mental health-related morbidity. PLoS ONE 2020, 15, e0236344. [Google Scholar] [CrossRef]
- Dirmyer, V.F. Using Real-Time Syndromic Surveillance to Analyze the Impact of a Cold Weather Event in New Mexico. J. Environ. Public Health 2018, 2018, 2185704. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Level 1 | Percentage | Level 2 | Percentage | Level 3 | Percentage | Total | |
|---|---|---|---|---|---|---|---|
| No NASS Alarm | 245 | 80% | 30 | 10% | 31 | 10% | 306 |
| NASS Alarm | 2 | 5% | 12 | 29% | 28 | 67% | 42 |
| Total | 247 | 71% | 42 | 12% | 59 | 17% | 348 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Packer, S.; Loveridge, P.; Soriano, A.; Morbey, R.; Todkill, D.; Thompson, R.; Rayment-Bishop, T.; James, C.; Pillin, H.; Smith, G.; et al. The Utility of Ambulance Dispatch Call Syndromic Surveillance for Detecting and Assessing the Health Impact of Extreme Weather Events in England. Int. J. Environ. Res. Public Health 2022, 19, 3876. https://doi.org/10.3390/ijerph19073876
Packer S, Loveridge P, Soriano A, Morbey R, Todkill D, Thompson R, Rayment-Bishop T, James C, Pillin H, Smith G, et al. The Utility of Ambulance Dispatch Call Syndromic Surveillance for Detecting and Assessing the Health Impact of Extreme Weather Events in England. International Journal of Environmental Research and Public Health. 2022; 19(7):3876. https://doi.org/10.3390/ijerph19073876
Chicago/Turabian StylePacker, Simon, Paul Loveridge, Ana Soriano, Roger Morbey, Dan Todkill, Ross Thompson, Tracy Rayment-Bishop, Cathryn James, Hilary Pillin, Gillian Smith, and et al. 2022. "The Utility of Ambulance Dispatch Call Syndromic Surveillance for Detecting and Assessing the Health Impact of Extreme Weather Events in England" International Journal of Environmental Research and Public Health 19, no. 7: 3876. https://doi.org/10.3390/ijerph19073876
APA StylePacker, S., Loveridge, P., Soriano, A., Morbey, R., Todkill, D., Thompson, R., Rayment-Bishop, T., James, C., Pillin, H., Smith, G., & Elliot, A. J. (2022). The Utility of Ambulance Dispatch Call Syndromic Surveillance for Detecting and Assessing the Health Impact of Extreme Weather Events in England. International Journal of Environmental Research and Public Health, 19(7), 3876. https://doi.org/10.3390/ijerph19073876






