A Critical Analysis of the COVID-19 Hospitalization Network in Countries with Limited Resources
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Collection
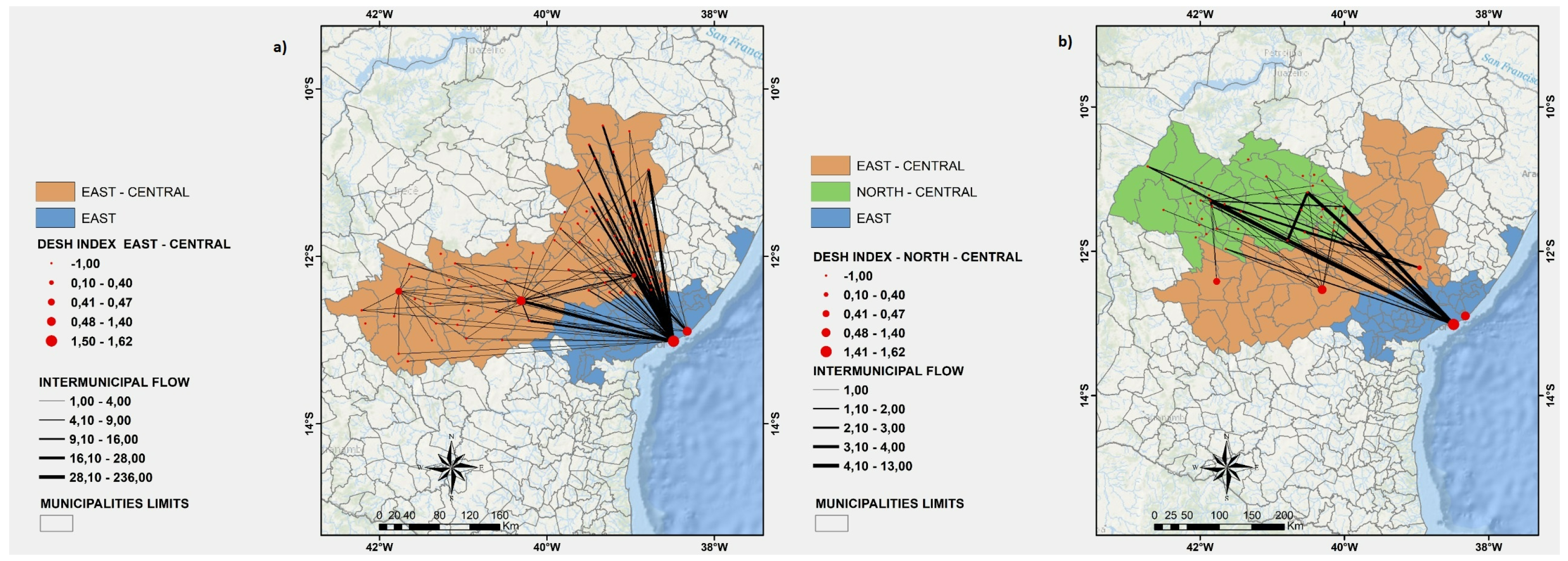
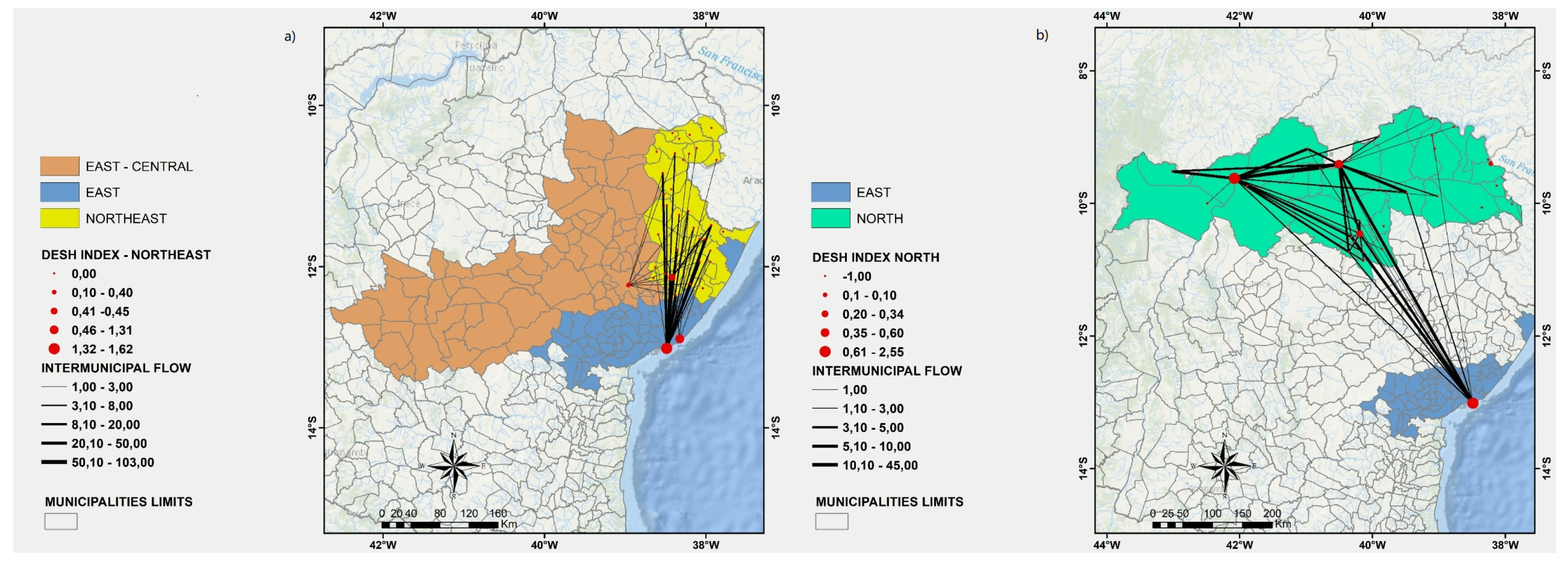
2.2. Hospitalization Network
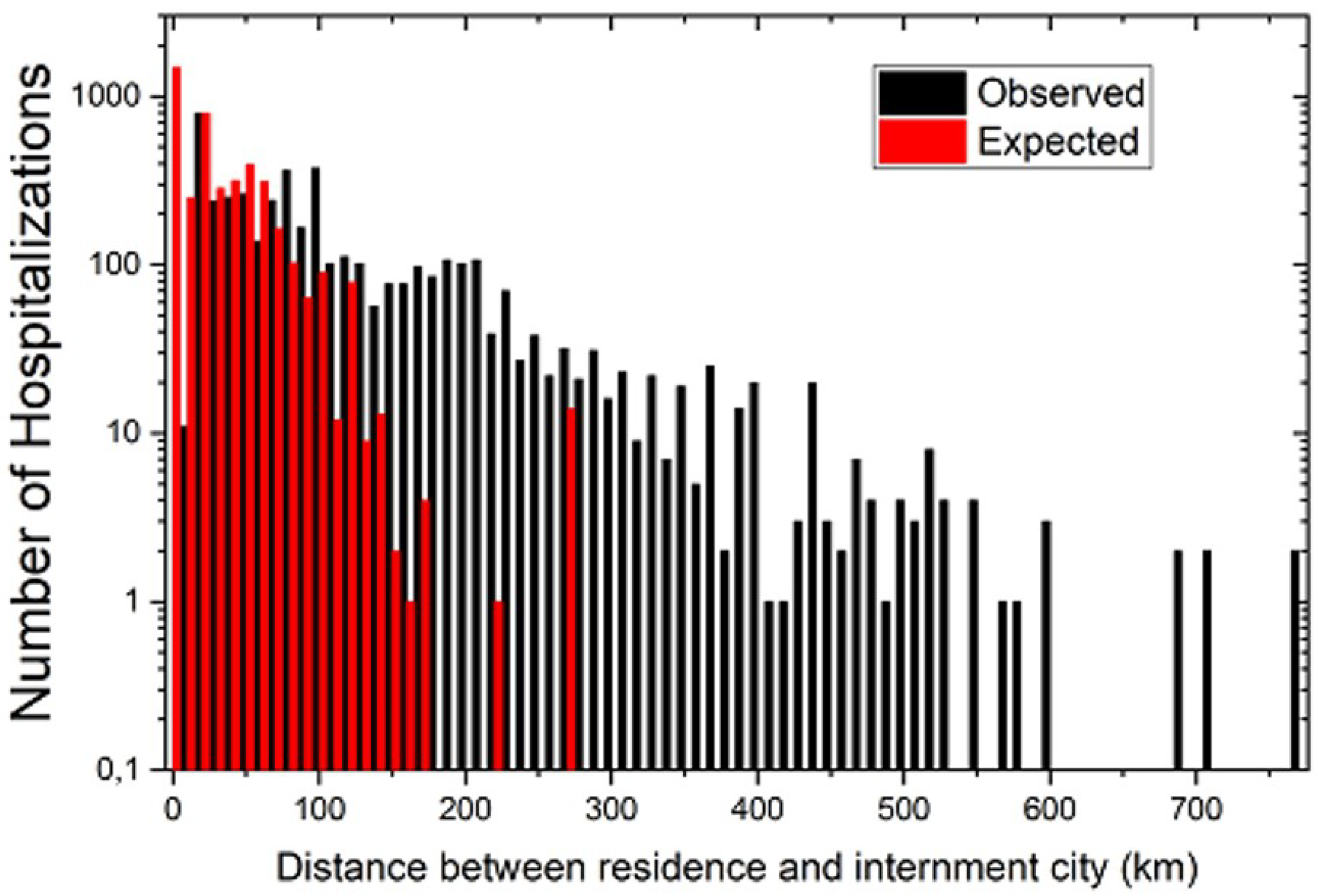
2.3. Simulation of the Expected Network
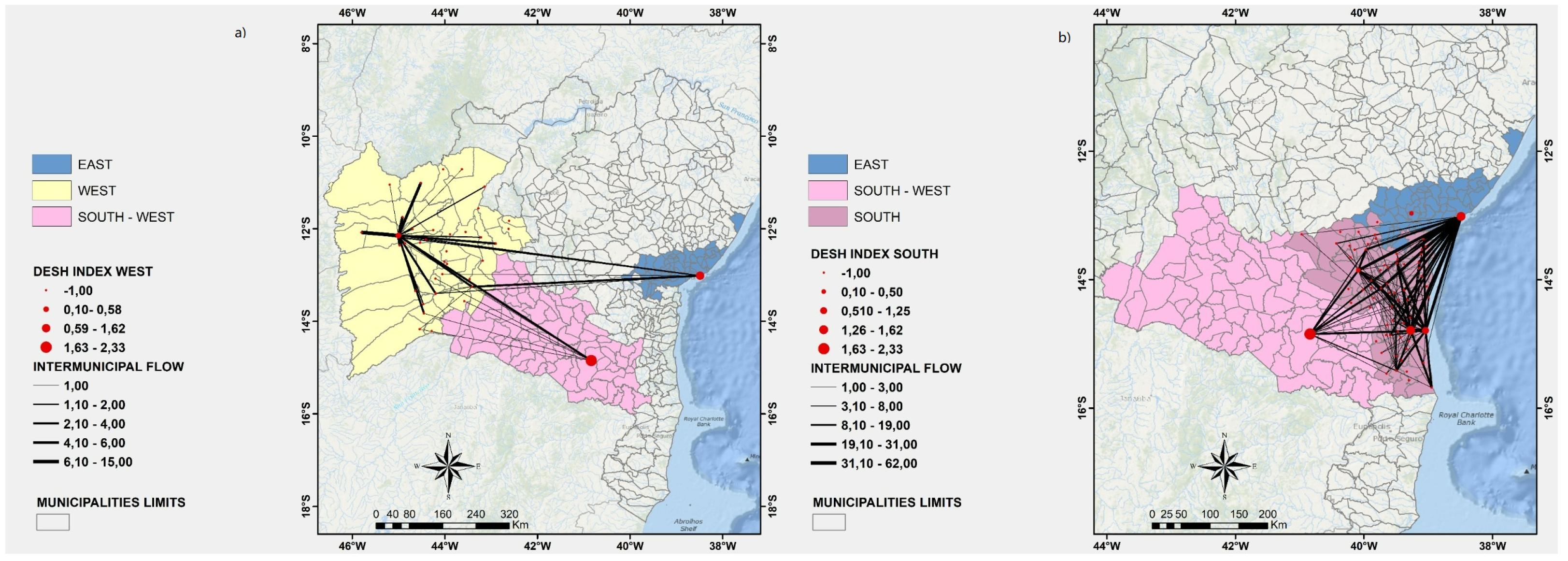
2.4. DESH (Degree of External Search for Hospitalization) Index
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CNPq | National Council for Scientific and Technological Development |
| COVID-19 | Coronavirus Disease 2019 |
| DESH | Degree of External Search for Hospitalization |
| FAPESB | The Foundation for Research Support of the State of Bahia |
| HDI | Human Development Index |
| SESAB | Health Secretary of the State of Bahia |
| SUS | Brazilian National Health System |
| WHO | World Health Organization |
References
- Brazilian Institute of Geography and Statistics. Estimated Population in Bahia, Brazil. Available online: https://cidades.ibge.gov.br/brasil/ba/panorama (accessed on 20 November 2021).
- World Health Organization. Considerations for Quarantine of Individuals in the Context of Containment for Coronavirus Disease (COVID-19): Interim Guidance; No. WHO/2019-nCov/IHR_Quarantine/2020.1; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Tanaka, O.Y.; Oliveira, V.E. Reforms and organization of the British National Health System: Lessons to the Brazilian National Health System. Saúde Soc. 2007, 16, 7–17. [Google Scholar] [CrossRef][Green Version]
- Constitution of the Federative Republic of Brazil. Available online: http://www.planalto.gov.br/ccivil_03/constituicao/constituicao.htm (accessed on 20 November 2021).
- Lei Orgânica de Saúde. Lei n° 8.080; 1990. Available online: http://www.planalto.gov.br/ccivil_03/leis/l8080.htm (accessed on 20 November 2021).
- Massuda, A.; Hone, T.; Leles, F.A.G.; De Castro, M.C.; Atun, R. The Brazilian health system at crossroads: Progress, crisis and resilience. BMJ Global Health 2018, 3, e000829. [Google Scholar] [PubMed]
- Punnakitikashem, P.; Hallinger, P. Bibliometric review of the knowledge base on healthcare management for sustainability, 1994–2018. Sustainability 2019, 12, 205. [Google Scholar] [CrossRef]
- Nuti, S.; Vainieri, M.; Bonini, A. Disinvestment for re-allocation: A process to identify priorities in healthcare. Health Policy 2010, 95, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Park, H.A.; Kim, S.; Ha, S.O.; Han, S.; Lee, C. Effect of Designating Emergency Medical Centers for Critical Care on Emergency Medical Service Systems during the COVID-19 Pandemic: A Retrospective Observational Study. J. Clin. Med. 2022, 11, 906. [Google Scholar] [CrossRef] [PubMed]
- Katayama, Y.; Tanaka, K.; Kitamura, T.; Takeuchi, T.; Nakao, S.; Nitta, M.; Iwami, T.; Fujimi, S.; Uejima, T.; Miyamoto, Y.; et al. Incidence and Mortality of Emergency Patients Transported by Emergency Medical Service Personnel during the Novel Corona Virus Pandemic in Osaka Prefecture, Japan: A Population-Based Study. J. Clin. Med. 2021, 10, 5662. [Google Scholar] [CrossRef] [PubMed]
- Health Secretary of the State of Bahia. Plano Estadual de Contingências Para Enfrentamento do Novo Coronavírus—SARS—CoV—2. Available online: http://www.saude.ba.gov.br/wp-content/uploads/2020/06/Plano-de-Continge%CC%82ncia-Coronav%C3%ADrus-Bahia-2020-2606.pdf (accessed on 20 November 2021).
- Health Secretary of the State of Bahia. Central Integrada de Comando e Controle de Saúde—COVID-19. Available online: https://bi.saude.ba.gov.br/transparencia/ (accessed on 20 January 2022).
- Health Secretary of the State of Bahia. Regulation System. Available online: http://www.saude.ba.gov.br/atencao-a-saude/comofuncionaosus/sistema-de-regulacao/ (accessed on 5 February 2022).
- Saba, H.; Vale, V.C.; Moret, M.A.; Miranda, J.C.V. Spatio-temporal correlation networks of dengue in the state of Bahia. BMC Public Health 2014, 14, 1085. [Google Scholar]
- Saba, H.; Moret, M.A.; Barreto, F.R.; Araujo, M.L.V.; Jorge, E.M.F.; Filho, A.S.N.F.; Miranda, J.G.V. Relevance of transportation to correlations among criticality, physical means of propagation, and distribution of dengue fever cases in the state of Bahia. Sci. Total Environ. 2018, 618, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Tiracini, A.; Cats, O. COVID-19 and public transportation: Current assessment, prospects, and research needs. J. Public Trans. 2020, 22, 1. [Google Scholar] [CrossRef]
- Zheng, R.; Xu, Y.; Wang, W.; Ning, G.; Bi, Y. Spatial transmission of COVID-19 via public and private transportation in China. Travel. Med. Infect. Dis. 2020, 34, 101626. [Google Scholar]
- Du, Z.; Wang, L.; Cauchemez, S.; Xu, X.; Wang, X.; Cowling, B.J.; Meyers, L.A. Risk for Transportation of Coronavirus Disease from Wuhan to Other Cities in China. Emerg. Infect. Dis. 2020, 26, 1049. Available online: https://wwwnc.cdc.gov/eid/article/26/5/20-0146_article (accessed on 20 November 2021). [PubMed]
- Wei, J.T.; Liu, Y.X.; Zhu, Y.C.; Qian, J.; Ye, R.Z.; Li, C.Y.; Ji, X.K.; Li, H.K.; Qi, C.; Wang, Y.; et al. Impacts of transportation and meteorological factors on the transmission of COVID-19. Int. J. Hyg. Environ. Health 2020, 230, 113610. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Park, S.J.; Lee, G.R.; Kim, J.E.; Lee, J.H.; Jung, Y.; Nam, E.W. The relationship between trends in COVID-19 prevalence and traffic levels in South Korea. Int. J. Infect. Dis. 2020, 96, 399–407. [Google Scholar] [CrossRef] [PubMed]
- Carmo, R.F.; Nunes, B.E.B.R.; Machado, M.F.; Armstrong, A.C.; Souza, C.D.F. Expansion of COVID-19 within Brazil: The importance of highways. J. Travel. Med. 2020, 27, taaa106. [Google Scholar] [CrossRef] [PubMed]
- Zhong, P.; Guo, S.; Chen, T. Correlation between travellers departing from Wuhan before the Spring Festival and subsequent spread of COVID-19 to all provinces in China. J. Travel. Med. 2020, 27, taaa036. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Lin, H.; Wang, J.; Xu, C.; Tatem, A.J.; Meng, B.; Zhang, X.; Liu, Y.; Wang, P.; Wu, G.; et al. The risk of COVID-19 transmission in train passengers: An epidemiological and modelling study. Clin. Infect. Dis. 2020, 72, 604–610. [Google Scholar] [CrossRef]
- Bajardi, P.; Poletto, C.; Ramasco, J.J.; Tizzoni, M.; Colizza, V.; Vespignani, A. Human Mobility Networks, Travel Restrictions, and the Global Spread of 2009 H1N1 Pandemic. PLoS ONE 2011, 6, e16591. [Google Scholar] [CrossRef]
- Liew, M.F.; Siow, W.T.; Yau, Y.W.; See, K.C. Safe patient transport for COVID-19. Crit. Care 2020, 24, 1–13. [Google Scholar]
- Brown, A.S.; Hustey, F.M.; Reddy, A.J. Interhospital transport of patients with COVID-19: Cleveland Clinic approach. Cleve Clin. J. Med. 2020. [Google Scholar] [CrossRef]
- Macedo, M.C.; Pinheiro, I.M.; Carvalho, C.J.; Fraga, H.C.; Araujo, I.P.; Montes, S.S.; Araujo, O.A.; Alves, L.A.; Saba, H.; Araújo, M.L.; et al. Correlation between hospitalized patients’ demographics, symptoms, comorbidities, and COVID-19 pandemic in Bahia, Brazil. PLoS ONE 2020, 15, e0243966. [Google Scholar] [CrossRef]
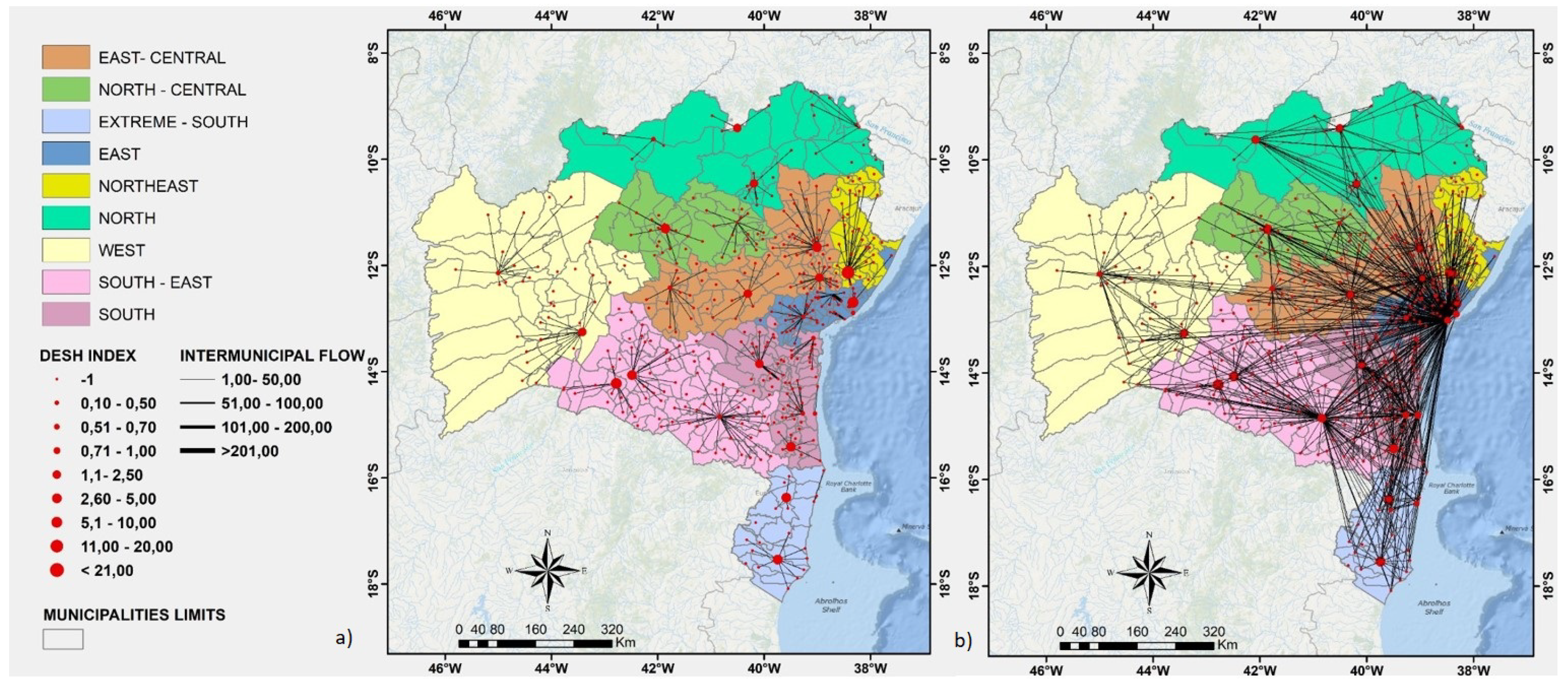

| Region | Patients That Live in That Region | Patients Imported from Other Regions | Patients Exported to Other Regions |
|---|---|---|---|
| North | 158 (81.9%) | 0 (0.0%) | 35 (18.1%) |
| Northeast | 11 (3.7%) | 0 (0.0%) | 290 (96.3%) |
| North-Central | 12 (12.9%) | 2 (2.2%) | 79 (84.9%) |
| East-Central | 77 (10.7%) | 70 (9.7%) | 571 (79.5%) |
| East | 1686 (54.9%) | 1369 (44.6%) | 14 (0.5%) |
| West | 62 (67.4%) | 0 (0.0%) | 30 (32.6%) |
| Southwest | 263 (54.3%) | 140 (28.9%) | 81 (16.7%) |
| South | 401 (47.3%) | 61 (7.2%) | 385 (45.5%) |
| Extreme-South | 74 (31.8%) | 1 (0.4%) | 158 (67.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araujo, M.L.V.; Miranda, J.G.V.; Vasconcelos, R.N.; Cambui, E.C.B.; Rosário, R.S.; Macedo, M.C.F.; Bandeira, A.C.; Souza, M.S.P.L.; Silva, A.C.F.N.; Filho, A.S.N.; et al. A Critical Analysis of the COVID-19 Hospitalization Network in Countries with Limited Resources. Int. J. Environ. Res. Public Health 2022, 19, 3872. https://doi.org/10.3390/ijerph19073872
Araujo MLV, Miranda JGV, Vasconcelos RN, Cambui ECB, Rosário RS, Macedo MCF, Bandeira AC, Souza MSPL, Silva ACFN, Filho ASN, et al. A Critical Analysis of the COVID-19 Hospitalization Network in Countries with Limited Resources. International Journal of Environmental Research and Public Health. 2022; 19(7):3872. https://doi.org/10.3390/ijerph19073872
Chicago/Turabian StyleAraujo, Marcio L. V., José G. V. Miranda, Rodrigo N. Vasconcelos, Elaine C. B. Cambui, Raphael S. Rosário, Márcio C. F. Macedo, Antonio C. Bandeira, Márcia S. P. L. Souza, Ana C. F. N. Silva, Aloisio S. Nascimento Filho, and et al. 2022. "A Critical Analysis of the COVID-19 Hospitalization Network in Countries with Limited Resources" International Journal of Environmental Research and Public Health 19, no. 7: 3872. https://doi.org/10.3390/ijerph19073872
APA StyleAraujo, M. L. V., Miranda, J. G. V., Vasconcelos, R. N., Cambui, E. C. B., Rosário, R. S., Macedo, M. C. F., Bandeira, A. C., Souza, M. S. P. L., Silva, A. C. F. N., Filho, A. S. N., Murari, T. B., Jorge, E. M. F., & Saba, H. (2022). A Critical Analysis of the COVID-19 Hospitalization Network in Countries with Limited Resources. International Journal of Environmental Research and Public Health, 19(7), 3872. https://doi.org/10.3390/ijerph19073872










