Pediatric Dental Emergency Visits and Treatment during Lockdown in the COVID-19 Pandemic: A Retrospective Study
Abstract
:1. Introduction
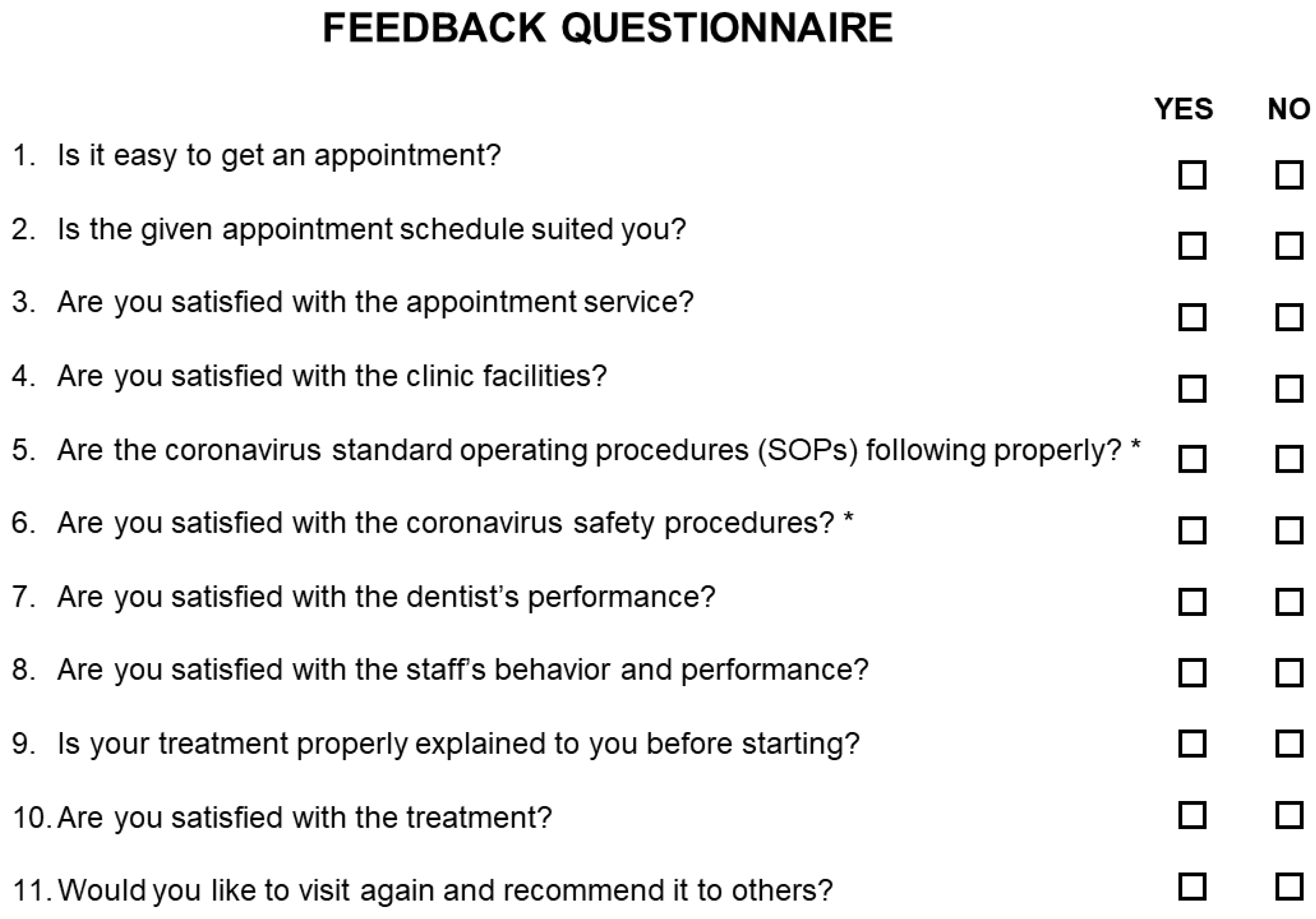
2. Methods
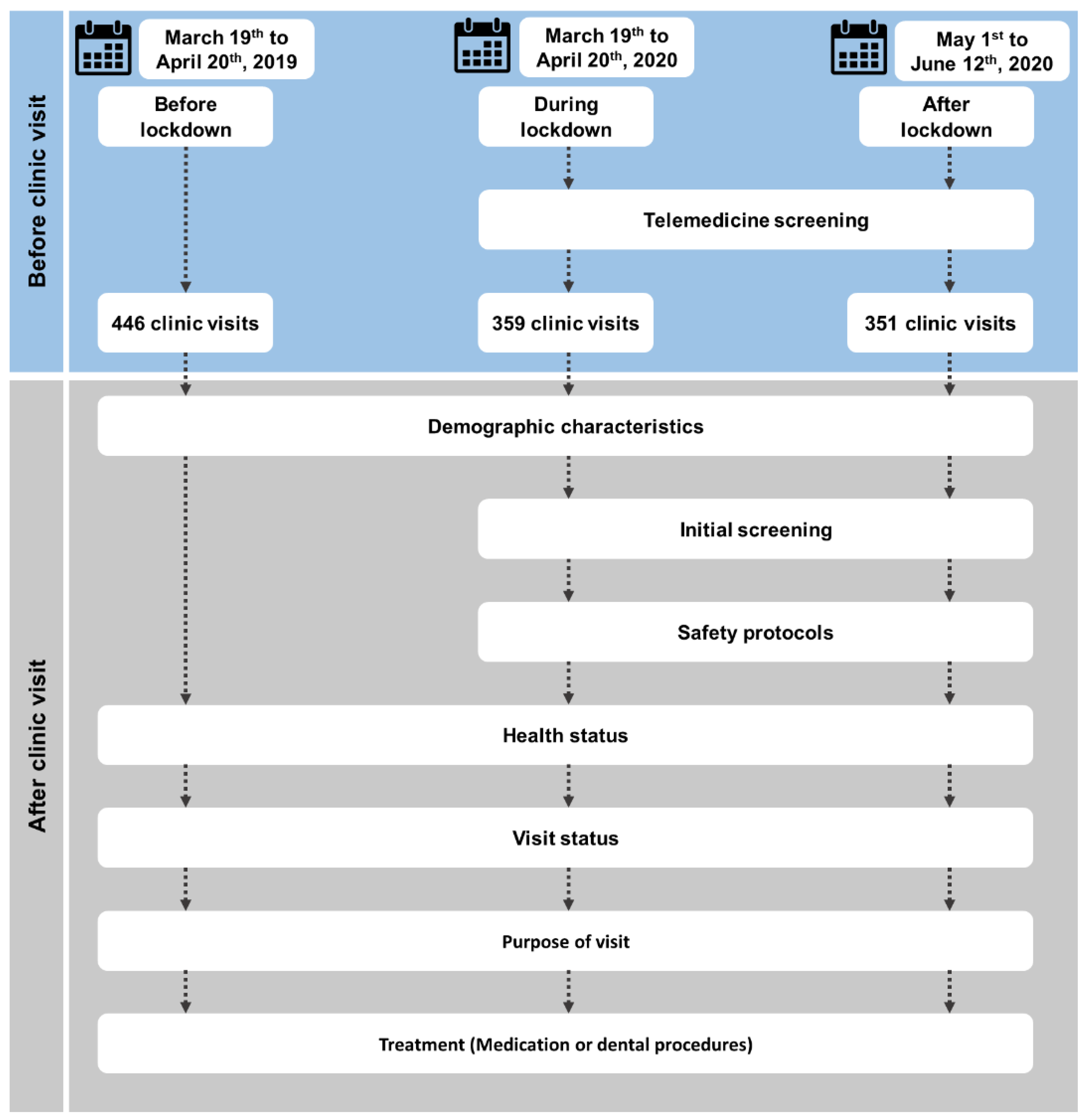
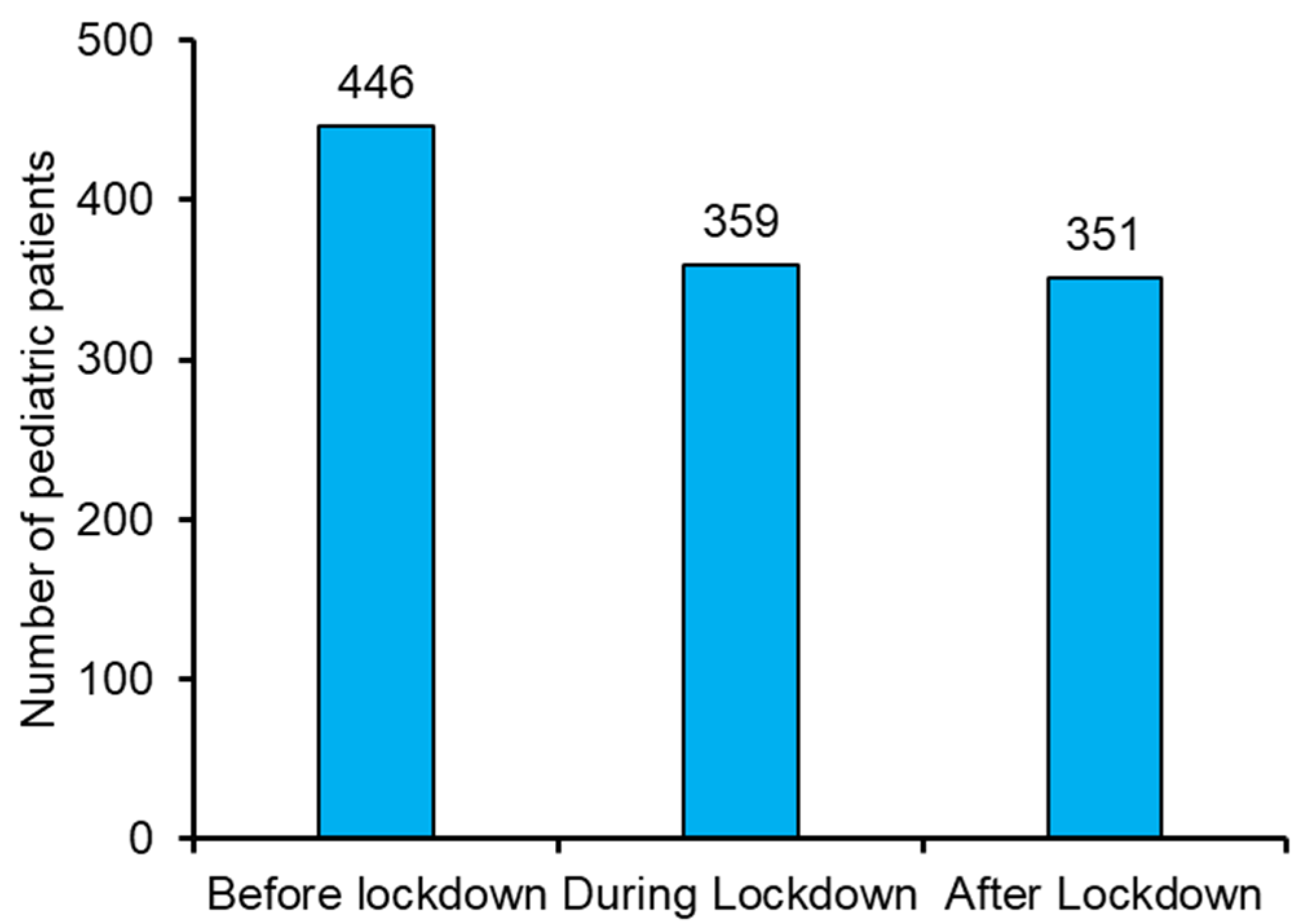
2.1. Study Design
2.1.1. Selection Criteria and Telemedicine Services
2.1.2. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Demographic Characteristics
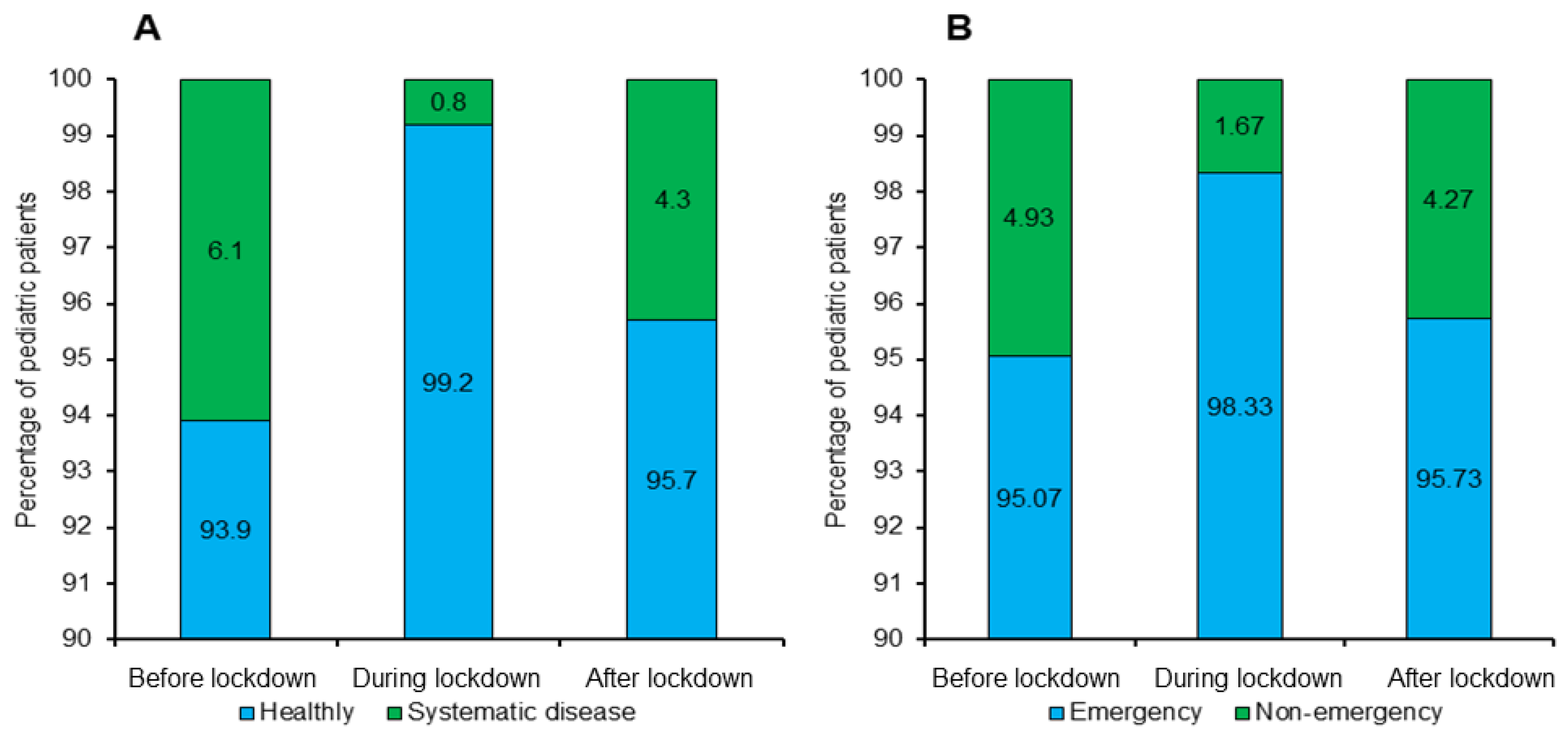
3.2. Health and Visit Status
3.3. Purpose of Visits
3.4. Treatment
3.4.1. Medication
3.4.2. Procedures
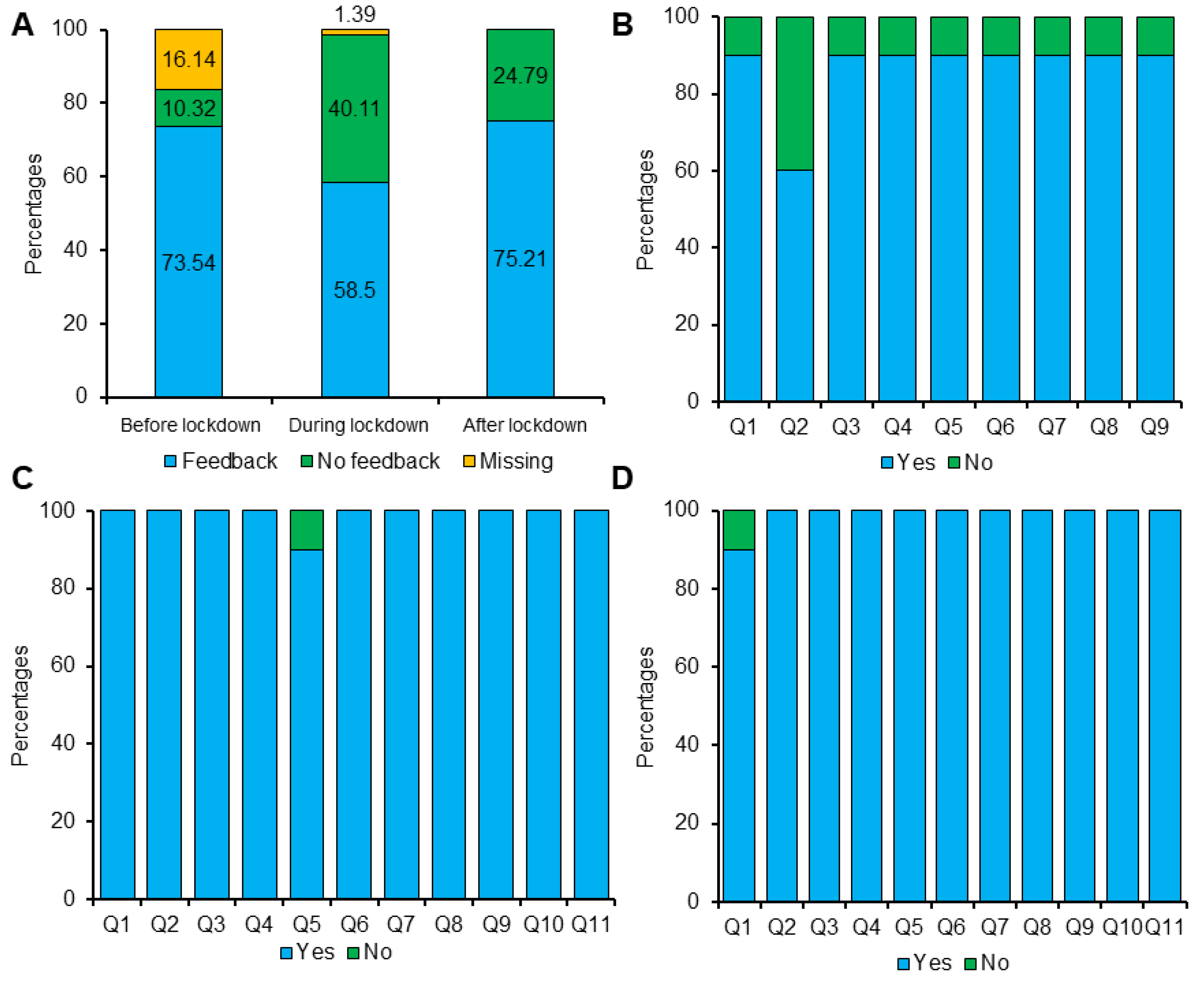
3.5. Feedback
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization Timeline of Response to COVID-19. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed on 15 January 2022).
- WHO WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 15 January 2022).
- Israel COVID: Worldometer. Available online: https://www.worldometers.info/coronavirus/country/israel/ (accessed on 15 January 2022).
- Last, M. The first wave of COVID-19 in Israel—Initial analysis of publicly available data. PLoS ONE 2020, 15, e0240393. [Google Scholar] [CrossRef] [PubMed]
- Cagetti, M.G.; Balian, A.; Camoni, N.; Campus, G. Influence of the covid-19 pandemic on dental emergency admissions in an urgent dental care service in North Italy. Int. J. Environ. Res. Public Health 2021, 18, 1812. [Google Scholar] [CrossRef] [PubMed]
- Dattner, I.; Goldberg, Y.; Katriel, G.; Yaari, R.; Gal, N.; Miron, Y.; Ziv, A.; Sheffer, R.; Hamo, Y.; Huppert, A. The role of children in the spread of COVID-19: Using household data from Bnei Brak, Israel, to estimate the relative susceptibility and infectivity of children. PLoS Comput. Biol. 2021, 17, e1008559. [Google Scholar] [CrossRef]
- Khoury Absawi, M.; Fahoum, K.; Costa, L.; Dror, A.A.; Bernfeld, N.M.; Oren, D.; Einy, S.; Kablan, F.; Srouji, S. COVID-19 induced stress among dentists affecting pediatric cooperation and alter treatment of choice. Adv. Oral Maxillofac. Surg. 2022, 5, 100212. [Google Scholar] [CrossRef]
- Ather, A.; Patel, B.; Ruparel, N.B.; Diogenes, A.; Hargreaves, K.M. Coronavirus Disease 19 (COVID-19): Implications for Clinical Dental Care. J. Endod. 2020, 46, 584–595. [Google Scholar] [CrossRef]
- Barranco, R.; Du Tremoul, L.V.B.; Ventura, F. Hospital-acquired sars-cov-2 infections in patients: Inevitable conditions or medical malpractice? Int. J. Environ. Res. Public Health 2021, 18, 489. [Google Scholar] [CrossRef]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef]
- Parvaie, P.; Osmani, F. Dentistry during COVID-19: Patients’ knowledge and satisfaction toward health protocols COVID-19 during dental treatment. Eur. J. Med. Res. 2022, 27, 3. [Google Scholar] [CrossRef]
- ADA Coronavirus (COVID-19) Center for Dentists. Available online: https://www.ada.org/resources/coronavirus (accessed on 15 January 2022).
- NHS. Novel Coronavirus (COVID-19) Standard Operating Procedure: Community Health Services. Available online: https://www.england.nhs.uk/wp-content/uploads/2020/02/20200305-COVID-19-PRIMARY-CARE-SOP-COMM-PHARM-PUBLICATION-V1 (accessed on 15 January 2022).
- Meng, L.; Hua, F.; Bian, Z. Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine. J. Dent. Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [Green Version]
- Obeidat, L.; Masarwa, N.; AlWarawreh, A.; El-Naji, W. Dental Treatments During the COVID-19 Pandemic in Three Hospitals in Jordan: Retrospective Study. Interact. J. Med. Res. 2020, 9, e24371. [Google Scholar] [CrossRef]
- What Constitutes a Dental Emergency? Available online: http://success.ada.org/~/media/CPS/Files/OpenFiles/ADA_COVID19_Dental_Emergency_DDS.pdf (accessed on 16 January 2022).
- Levit, M.; Levit, L. Infection Risk of COVID-19 in Dentistry Remains Unknown: A Preliminary Systematic Review. Infect. Dis. Clin. Pract. 2021, 29, e70–e77. [Google Scholar] [CrossRef] [PubMed]
- Froum, S.; Froum, S. Incidence of COVID-19 Virus Transmission in Three Dental Offices: A 6-Month Retrospective Study. Int. J. Periodontics Restor. Dent. 2020, 40, 853–859. [Google Scholar] [CrossRef]
- Medscape in Memoriam Healthcare Workers Who Have Died of COVID-19. Available online: https://www.medscape.com/viewarticle/927976#vp_1 (accessed on 16 January 2022).
- Statista Number of Male Dentists by Age Group in Italy 2019. Available online: https://www.statista.com/statistics/983852/Number-of-male-dentists-by-age-group-in-italy/ (accessed on 16 January 2022).
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020, 99, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Aldahlawi, S.A.; Afifi, I.K. COVID-19 in Dental Practice: Transmission Risk, Infection Control Challenge, and Clinical Implications. Open Dent. J. 2020, 14, 348–354. [Google Scholar] [CrossRef]
- Ashtiani, R.E.; Tehrani, S.; Revilla-León, M.; Zandinejad, A. Reducing the Risk of COVID-19 Transmission in Dental Offices: A Review. J. Prosthodont. 2020, 29, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Sergis, A.; Wade, W.G.; Gallagher, J.E.; Morrell, A.P.; Patel, S.; Dickinson, C.M.; Nizarali, N.; Whaites, E.; Johnson, J.; Addison, O.; et al. Mechanisms of Atomization from Rotary Dental Instruments and Its Mitigation. J. Dent. Res. 2021, 100, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Kumar, U.; Gupta, A.; Goyal, A.; Gauba, K. Impact of covid-19 pandemic on characteristics of dental emergencies and treatment services at tertiary care centre. Saudi Dent. J. 2021, 33, 1018–1023. [Google Scholar] [CrossRef]
- Nandlal, B.; Singh, B.; Gopi, A. Impact on Utilization and Shift in Treatment Needs Post-COVID Lockdown of Pediatric Dentistry in a Tertiary Care Hospital. Front. Dent. Med. 2021, 2, 722292. [Google Scholar] [CrossRef]
- Liu, C.; Zhang, S.; Zhang, C.; Tai, B.; Jiang, H.; Du, M. The impact of coronavirus lockdown on oral healthcare and its associated issues of pre-schoolers in China: An online cross-sectional survey. BMC Oral Health 2021, 21, 54. [Google Scholar] [CrossRef]
- Yang, J.; Yang, G.; Jin, R.; Song, G.; Yuan, G. Changes in paediatric dental clinic after reopening during COVID-19 pandemic in Wuhan: A retrospective study. BMJ Open 2022, 12, e048430. [Google Scholar] [CrossRef]
- Üstün, N.; Akgöl, B.B.; Bayram, M. Influence of COVID-19 pandemic on paediatric dental attendance. Clin. Oral Investig. 2021, 25, 6185–6191. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention; Division of Oral Health. Infection Prevention & Control in Dental Settings. Available online: https://www.cdc.gov/oralhealth/infectioncontrol/index.html (accessed on 21 January 2022).
- Docimo, R.; Costacurta, M.; Gualtieri, P.; Pujia, A.; Leggeri, C.; Attinà, A.; Cinelli, G.; Giannattasio, S.; Rampello, T.; Di Renzo, L. Cariogenic risk and COVID-19 lockdown in a paediatric population. Int. J. Environ. Res. Public Health 2021, 18, 7558. [Google Scholar] [CrossRef] [PubMed]
- Gao, X.; Ding, M.; Xu, M.; Wu, H.; Zhang, C.; Wang, X.; Feng, X.; Tai, B.; Hu, D.; Lin, H.; et al. Utilization of dental services and associated factors among preschool children in China. BMC Oral Health 2020, 20, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ghai, S. Teledentistry during COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 933–935. [Google Scholar] [CrossRef]
- Deshpande, S.; Patil, D.; Dhokar, A.; Bhanushali, P.; Katge, F. Teledentistry: A Boon Amidst COVID-19 Lockdown-A Narrative Review. Int. J. Telemed. Appl. 2021, 2021, 8859746. [Google Scholar] [CrossRef]
- Fux-Noy, A.; Mattar, L.; Shmueli, A.; Halperson, E.; Ram, D.; Moskovitz, M. Oral Health Care Delivery for Children During COVID-19 Pandemic—A Retrospective Study. Front. Public Health 2021, 9, 637351. [Google Scholar] [CrossRef]
- Samuel, S.R.; Mathew, M.G.; Suresh, S.G.; Varma, S.R.; Elsubeihi, E.S.; Arshad, F.; Elkareimi, Y.; Elsahn, N.A.; Khalil, E. Pediatric dental emergency management and parental treatment preferences during COVID-19 pandemic as compared to 2019. Saudi J. Biol. Sci. 2021, 28, 2591–2597. [Google Scholar] [CrossRef]
- Guo, H.; Zhou, Y.; Liu, X.; Tan, J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J. Dent. Sci. 2020, 15, 564–567. [Google Scholar] [CrossRef]
- Tobias, G. Dental Emergencies during the COVID-19 No Aversion Therapy Centers. Open Access J. Dent. Sci. 2020, 5, 265. [Google Scholar] [CrossRef]
- Limbu, S.; Dikshit, P.; Malla, M.; Verma, L.; Khapung, A. Pediatric Dental Emergency Pattern and Dental Care Provided during COVID-19 Pandemic Lockdown at a Tertiary Care Center in Kathmandu, Nepal. J. Nepal. Assoc. Pediatr. Dent. 2021, 2, 3–11. [Google Scholar] [CrossRef]
- Wu, K.; Li, C.; Yang, Z.; Yang, S.; Yang, W.; Hua, C. Changes in the characteristics of dental emergencies under the influence of SARS-CoV-2 pandemic: A retrospective study. BMC Oral Heal. 2021, 21, 174. [Google Scholar] [CrossRef] [PubMed]
- Sharma, H.; Suprabha, B.S.; Rao, A. Teledentistry and its applications in paediatric dentistry: A literature review. Pediatr. Dent. J. 2021, 31, 203–215. [Google Scholar] [CrossRef] [PubMed]

| Demographic Characteristics | Before Lockdown n = 446 (100%) | During Lockdown n = 359 (100%) | After Lockdown n = 351 (100%) | p-Value |
|---|---|---|---|---|
| Gender | ||||
| Male | 234 (52.5) | 178 (49.58) | 187 (53.28) | <0.01 |
| Female | 212 (47.5) | 181 (50.42) | 164 (46.72) | 0.879 |
| Age | ||||
| Range | 1–17 | 1–18 | 1–16 | |
| Mean + SD | 7.9 + 4.16 | 8.51+ 4.18 | 7.14 + 2.62 | |
| Median | 7 | 8 | 7 | |
| ≤6 | 156 (34.98) | 111 (30.92) | 110 (31.34) | <0.001 |
| 7–12 | 241 (54.04) | 161 (44.85) | 172 (49) | <0.001 |
| 13–18 | 49 (10.99) | 87 (24.23) | 69 (19.66) | <0.01 |
| Visit Purposes | Before Lockdown | During Lockdown | After Lockdown | p-Value | Pearson’s Correlation |
|---|---|---|---|---|---|
| 1 Trauma, n = 73, (100%) | 37 (50.7) | 18 (24.7) | 18 (24.7) | <0.01 | 1 vs. 2 (p < 0.001) |
| 2 Infection, n = 109, (100%) | 51 (46.8) | 31 (28.4) | 27 (24.8) | 0.01 | |
| 3 Pain, n = 861, (100%) | 307 (35.7) | 281 (32.6) | 273 (31.7) | 0.33 | |
| 4 Treatment continuation, n = 34, (100%) | 12 (35.3) | 7 (20.6) | 15 (44.1) | 0.23 | 4 vs. 5 (p < 0.001) |
| 5 Defective treatment, n = 36, (100%) | 17 (47.2) | 16 (44.4) | 3 (8.3) | <0.01 |
| Demographic Characteristics | Trauma n (%) | Infection n (%) | Pain n (%) | Treatment Continuation n (%) | Defective Treatment n (%) | p-Value |
|---|---|---|---|---|---|---|
| Before lockdown, n = 424, (100%) | ||||||
| Gender | ||||||
| Male | 12 (2.83) | 24 (5.66) | 169 (39.85) | 8 (1.89) | 10 (2.35) | 0.07 |
| Female | 25 (5.9) | 27 (6.36) | 138 (32.54) | 4 (0.94) | 7 (1.65) | |
| Age groups | ||||||
| ≤6 | 5 (1.18) a | 150 (35.37) a | <0.001 | |||
| 7–12 | 30 (7.07) a | 43 (10.14) a | 146 (34.43) a | 1 (0.23) a | 12 (2.83) | |
| 13–18 | 7 (1.65) a | 3 (0.7) | 11 (2.6) a | 11 (2.6) a | 5 (1.18) a | |
| Health Status | ||||||
| Healthy | 37 (8.72) | 51 (12.03) | 307 (72.4) a | 12 (2.83) | 12 (2.83) a | <0.001 |
| Systemic Disease | 5 (1.18) a | |||||
| Treatment | ||||||
| Medication | 21 (4.95) | 16 (3.77) | 167 (39.38) | <0.001 | ||
| Procedures | 16 (3.77) | 35 (8.25) | 140 (33.01) | 12 (2.7) | 17 (3.81) | |
| During lockdown, n = 353, (100%) | ||||||
| Gender | ||||||
| Male | 10 (2.83) | 11 (3.11) | 142 (40.22) | 3 (0.85) | 10 (2.83) | 0.405 |
| Female | 8 (2.26) | 20 (5.66) | 139 (39.37) | 4 (1.13) | 6 (1.7) | |
| Age groups | ||||||
| ≤6 | 4 (1.13) | 12 (3.4) | 85 (24.08) | 7 (2.00) | 0.409 | |
| 7–12 | 11 (3.11) | 13 (3.68) | 125 (35.41) | 4 (1.13) | 7 (2.00) | |
| 13–18 | 3 (0.8) | 6 (1.7) | 71 (20.11) | 3 (0.85) | 2 (0.56) | |
| Health Status | ||||||
| Healthy | 18 (5.1) | 31 (8.78) | 281 (79.6) | 7 (2.00) | 16 (4.53) | |
| Treatment | ||||||
| Medication | 80 (22.66) a | <0.001 | ||||
| Procedures | 18 (5.1) | 31 (8.78) a | 201 (56.94) a | 7 (2.00) | 16 (4.53) | |
| After lockdown, n = 336, (100%) | ||||||
| Gender | ||||||
| Male | 11 (3.27) | 15 (4.46) | 143 (42.56) | 7 (2.08) | 1 (0.3) | 0.865 |
| Female | 7 (2.08) | 12 (3.57) | 130 (38.7) | 8 (2.38) | 2 (0.6) | |
| Age groups | ||||||
| ≤6 | 2 (0.6) | 86 (25.5) | 15 (4.46) a | 1 (0.3) | <0.001 | |
| 7–12 | 13 (3.86) | 2 (0.6) a | 152 (45.23) a | 1 (0.3) | ||
| 13–18 | 5 (1.49) | 23 (6.84) a | 35 (10.41) a | 1 (0.3) | ||
| Health Status | ||||||
| Healthy | 18 (5.35) | 27 (8.03) | 273 (81.25) | 15 (4.46) | 3 (0.9) | |
| Treatment | ||||||
| Medication | 11 (3.27) | 18 (5.35) | 129 (38.39) | 7 (2.08) | 0.104 | |
| Procedures | 7 (2.08) | 9 (2.67) | 144 (42.85) | 8 (2.38) | 3 (0.9) | |
| Treatment Procedures | Before Lockdown | During Lockdown | After Lockdown | p-Value | Pearson’s Correlation |
|---|---|---|---|---|---|
| 1 Crown, n = 67, (100%) | 41 (61.2) | 4 (6) | 22(32.8) | <0.001 | 1 vs. 3 (p < 0.001) |
| 2 Extraction, n = 195, (100%) | 70 (35.9) | 81 (41.5) | 44 (22.6) | <0.01 | 2 vs. 3 (p < 0.001) |
| 3 Filling, n = 166, (100%) | 36 (21.7) | 84 (50.6) | 46 (27.7) | <0.001 | 3 vs. 5 (p < 0.001) |
| 4 Fluoride, n = 14, (100%) | 1 (7.1) | 13 (92.9) | 0.001 | ||
| 5 Pulp treatment, n = 216, (100%) | 68 (31.5) | 92 (42.6) | 56 (25.9) | <0.01 | 5 vs. 2 (p < 0.001) |
| 6 Sealant, n = 2, (100%) | 2 (100) | ||||
| 7 Space maintainers, n = 3, (100%) | 2 (66.7) | 1 (33.3) | 0.564 | ||
| 8 Tooth fixation, n = 2, (100%) | 2 (100) |
| Demographic Characteristics | Crown n (%) | Extraction n (%) | Filling n (%) | Fluoride n (%) | Pulp Treatment n (%) | Sealant n (%) | Space Maintainer n (%) | Tooth Fixation n (%) | p-Value |
|---|---|---|---|---|---|---|---|---|---|
| Before lockdown, n = 220, (100%) | |||||||||
| Gender | |||||||||
| Male | 25 (11.36) | 37 (16.81) | 15 (6.81) | 35 (15.9) | 1 (0.45) | 1 (0.45) | 0.68 | ||
| Female | 16 (7.27) | 33 (15) | 21 (9.54) | 1 (0.45) | 33 (15) | 1 (0.45) | 1 (0.45) | ||
| Age | |||||||||
| ≤6 | 15 (6.81) | 22 (10) | 6 (2.72) | 16 (7.27) | 1 (0.45) | 1 (0.45) | 0.776 | ||
| 7–12 | 23 (10.45) | 38 (17.27) | 26 (11.81) | 1 (0.45) | 43 (19.54) | 1 (0.45) | 1 (0.45) | ||
| 13–18 | 3 (1.36) | 10 (4.54) | 4 (1.81) | 9 (4.09) | |||||
| Health status | |||||||||
| Healthy | 40 (18.18) | 69 (31.36) | 35 (15.9) | 1 (0.45) | 66 (30) | 2 (0.9) | 2 (0.9) | 0.998 | |
| Systemic Disease | 1 (0.45) | 1 (0.45) | 1 (0.45) | 2 (0.9) | |||||
| Purpose of visits | |||||||||
| Trauma | 1 (0.45) | 7 (3.18) | 2 (0.9) | 6 (2.72) | 0.98 | ||||
| Infection | 6 (2.72) | 11 (5) | 6 (2.72) | 12 (5.45) | |||||
| Pain | 31 (14.09) | 40 (18.18) | 23 (10.45) | 1 (0.45) | 41 (18.63) | 2 (0.9) | 2 (0.9) | ||
| Treatment continuation | 1 (0.45) | 7 (3.18) | 1 (0.45) | 3 (1.36) | |||||
| Defective Treatment | 2 (0.9) | 5 (2.27) | 4 (1.81) | 6 (2.72) | |||||
| During lockdown, n = 274, (100%) | |||||||||
| Gender | |||||||||
| Male | 2 (0.73) | 35 (12.77) | 49 (17.88) | 7 (2.55) | 44 (16.06) | 0.429 | |||
| Female | 2 (0.73) | 45 (16.42) | 35 (12.77) | 6 (2.19) | 48 (17.51) | ||||
| Age | |||||||||
| ≤6 | 1 (0.36) | 24 (8.76) | 33 (12.04) | 5 (1.82) | 20 (7.3) | 0.066 | |||
| 7–12 | 3 (1.1) | 40 (14.6) | 34 (12.4) | 2 (0.73) | 49 (17.88) | ||||
| 13–18 | 16 (5.84) | 17 (6.2) | 6 (2.19) | 23 (8.4) | |||||
| Health status | |||||||||
| Healthy | 4 (1.46) | 80 (29.19) | 84 (30.65) | 13 (4.74) | 92 (33.57) | ||||
| Purpose of visits | |||||||||
| Trauma | 7 (2.55) | 5 (1.82) | 6 (2.19) | 0.12 | |||||
| Infection | 12 (4.38) | 8 (3.00) a | 5 (1.82) | 6 (2.19) | |||||
| Pain | 4 (1.46) | 54 (19.7) | 66 (24.08) | 6 (2.19) | 71 (25.91) | ||||
| Treatment continuation | 3 (1.1) | 4 (1.46) | |||||||
| Defective Treatment | 4 (1.46) | 5 (1.82) | 2 (0.73) | 5 (1.82) | |||||
| After lockdown, n = 171, (100%) | |||||||||
| Gender | |||||||||
| Male | 11 (6.43) | 21 (12.28) | 25 (14.62) | 32 (18.71) | 1 (0.58) | 0.865 | |||
| Female | 11 (6.43) | 23 (13.45) | 21 (12.28) | 24 (14.03) | 1 (0.58) | 1 (0.58) | |||
| Age | |||||||||
| ≤6 | 9 (5.26) | 14 (8.18) | 17 (9.94) | 22 (12.86) | 0.012 | ||||
| 7–12 | 11 (6.43) | 25 (14.61) | 24 (14.03) | 28 (16.37) | |||||
| 13–18 | 2 (1.17) | 5 (2.92) | 5 (2.92) | 6 (3.5) | 1 (0.58) | 2 (1.17) | |||
| Health status | |||||||||
| Healthy | 22 (12.86) | 44 (25.73) | 46 (26.9) | 56 (32.74) | 1 (0.58) | 2 (1.17) | |||
| Purpose of visits | |||||||||
| Trauma | 2 (1.17) | 3 (1.75) | 2 (1.17) | 0.002 | |||||
| Infection | 1 (0.58) | 3 (1.75) | 1 (0.58) | 2 (1.17) | 2 (1.17) | ||||
| Pain | 19 (11.1) | 36 (21.05) | 40 (23.4) | 48 (28.07) | 1 (0.58) | ||||
| Treatment continuation | 2 (1.17) | 1 (0.58) | 2 (1.17) | 3 (1.75) | |||||
| Defective Treatment | 2 (1.17) | 1 (0.58) | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elalouf, A.; Moran, R.; Yaron, B.; Oman, M. Pediatric Dental Emergency Visits and Treatment during Lockdown in the COVID-19 Pandemic: A Retrospective Study. Int. J. Environ. Res. Public Health 2022, 19, 3774. https://doi.org/10.3390/ijerph19073774
Elalouf A, Moran R, Yaron B, Oman M. Pediatric Dental Emergency Visits and Treatment during Lockdown in the COVID-19 Pandemic: A Retrospective Study. International Journal of Environmental Research and Public Health. 2022; 19(7):3774. https://doi.org/10.3390/ijerph19073774
Chicago/Turabian StyleElalouf, Amir, Rubanenko Moran, Bernstein Yaron, and Michal Oman. 2022. "Pediatric Dental Emergency Visits and Treatment during Lockdown in the COVID-19 Pandemic: A Retrospective Study" International Journal of Environmental Research and Public Health 19, no. 7: 3774. https://doi.org/10.3390/ijerph19073774
APA StyleElalouf, A., Moran, R., Yaron, B., & Oman, M. (2022). Pediatric Dental Emergency Visits and Treatment during Lockdown in the COVID-19 Pandemic: A Retrospective Study. International Journal of Environmental Research and Public Health, 19(7), 3774. https://doi.org/10.3390/ijerph19073774






