Abstract
Purpose: The first coronavirus disease (COVID-19) spike and subsequent pandemic in South Korea were rapid and disruptive. Government response measures for disadvantaged groups against infectious disease should be prioritized based on evidence and affordability. We investigated whether COVID-19 infection, intensive care unit (ICU) care, and mortality from COVID-19 are related to social and medical vulnerability, including tuberculosis (TB). Patients and Methods: Using the National Health Insurance Service COVID-19 database in South Korea, we analyzed 129,128 patients, including controls, from 1 January to 30 May 2020, during the early stage of the COVID-19 epidemic. The relationship between health insurance premiums (representing socioeconomic status), the Charlson comorbidity index (CCI) score for the severity of the underlying disease, and additional TB diagnosis was analyzed using the chi-square test and logistic regression. Results: For the demographics, 3244 out of 51,783 men (6.3%) and 4836 out of 77,345 women (6.3%) were infected with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). COVID-19 infection, ICU care, and mortality were related to older age (p < 0.001) and lower health insurance premium levels (p < 0.05). Regarding the CCI score, the CCI score, COVID-19 infection, and mortality increased (p < 0.0001). In terms of premium level, the highest group showed a lower risk of infection (OR 0.52, 0.48-0.57, p = 0.004), ICU care (OR 0.59, 0.46-0.75, p < 0.001), and mortality (OR 0.51, 0.32-0.78, p = 0.016) than the medical aid group. TB was related to ICU care for COVID-19 (OR 4.27, 1.27-14.38, p = 0.018). Conclusion: In the early epidemic, SARS-CoV-2 infection, ICU admission, and mortality from COVID-19 increased in socioeconomically and physically vulnerable groups. However, the relationship between tuberculosis, COVID-19 and mortality was not definite because of the possible under-reporting of TB cases and the relatively small number of TB patients.
1. Introduction
The World Health Organization (WHO) declared the outbreak of the novel coronavirus disease (COVID-19) as a public health emergency of international concern on 30 January 2020, and recorded 209,876,613 cases and 4,400,284 deaths from COVID-19 by August 19 [1]. South Korea was one of the countries affected by COVID-19 in the initial epidemic; the first confirmed case was reported on 20 January 2020. As of 19 August 2021, there had been 232,859 confirmed cases of COVID-19 in South Korea, resulting in 2197 deaths (see the WHO COVID-19 Dashboard).
In many infectious diseases, including COVID-19, hygiene and environmental control are very important in order to block the infection connection chain, especially in socially and medically vulnerable groups [2]. Even though government response policies for disadvantaged groups should have been prioritized based on evidence and affordability, the initial COVID-19 surge and consecutive pandemic were abrupt and disruptive to the earlier-affected Asian countries [3]. Socially vulnerable groups such as intellectually disabled people were expected to be affected more seriously in the initial stage of the COVID-19 pandemic [4].
A consistent finding in this pandemic is that patients with comorbidities are more likely to be afflicted by the virus. A meta-analysis of eight studies and 46,248 patients with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection confirmed by molecular diagnostics showed that comorbidities were powerful predictors of the need for hospitalization and poor outcomes [5]. The suggested comorbidities are diabetes, cardiac disease, chronic renal disease, bronchiectasis, and obesity [6]. Given that most fatal cases develop from respiratory failure, such as adult respiratory distress syndrome (ARDS) requiring ventilator care or extracorporeal membrane oxygenation (ECMO), pre-existing or co-infected respiratory disease could critically influence the clinical course of COVID-19 [2].
Individuals with latent or active tuberculosis (TB) were more susceptible to SARS-CoV-2 infection, according to an observational study from Wuhan, the pandemic’s epicenter [7]. Infection with Mycobacterium tuberculosis was found to be a more common comorbidity in COVID-19 (36%) than diabetes (25%), hypertension (22%), ischemic heart disease (8%), and chronic obstructive lung disease and chronic obstructive pulmonary disease (COPD) (6%) in China. M. tuberculosis co-infection was also associated with more severe COVID-19 and more rapid progression. Therefore, considering the intermediate TB burden in the Republic of Korea (hereafter Korea), where 19,933 new TB cases (38.8 per 100,000 population) and 1600 TB-related deaths were reported in 2020 [8], the possible links between TB and COVID-19 should be clarified [9].
We aimed to investigate the ways in which infection with COVID-19, ICU care, and mortality from COVID-19 were related to social and medical vulnerabilities, as well as TB.
2. Material and Methods
2.1. Data Collection and Study Participants
The purpose of this study was to determine the severity of SARS-CoV-2 infection in the tuberculosis population compared to the total population, in order to evaluate the appropriateness of the recent government directives, by analyzing SARS-CoV-2 infection, intensive care unit (ICU) admission, and COVID-19 death rates. In Korea’s health insurance system, public insurance is operated and funded by a single insurer, the National Health Insurance Service (NHIS). In Korea, all patients with confirmed COVID-19 are hospitalized. Therefore, all medical claims, including those for COVID-19 patients, are collected from the NHIS. We used the NHIS-COVID database (DB) for this analysis, which is given by the NHIS to facilitate research investigations that are based on the evidence for coronavirus therapy and policy implementation. This national data includes one’s insurance status, insurance premiums, and medical examination results. The data source includes all medical records from January 2015 to July 2020 for COVID-19 patients and controls from January 1 to 30 May 2020. The control group was a stratified sample of patients without a history of COVID-19 testing on a scale 15 times that of the COVID-19 patients. Stratification factors including sex (male, female), age group (0–9, 10–19, 20–29, 30–39, 40–49, 50–59, 60–69, 70–79, 80+), and residence (Seoul, Daegu, Gyeonggi-do, Gyeongsangbuk-do, Others) were considered based on their high prevalence, and random samples were drawn within the same groups. In this study, 129,128 patients included in the NHIS-COVID DB were analyzed (Figure 1), of which 121,048 were not infected and 8080 were infected with SARS-CoV-2, and the association between TB and SARS-CoV-2 infection was analyzed, in addition to the effect of the presence of tuberculosis on ICU admission and mortality in COVID-19 patients.
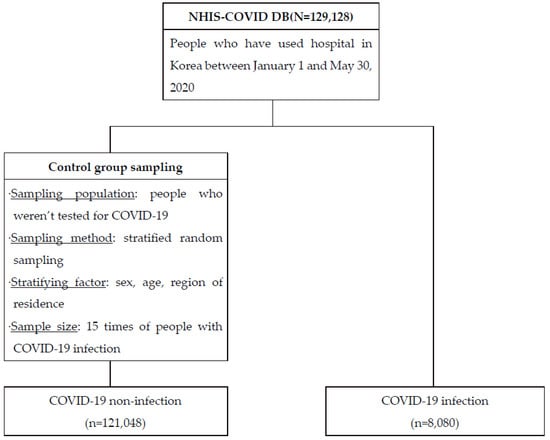
Figure 1.
Flow chart for people included in the analysis.
2.2. Statistical Analysis
A chi-square test was performed to confirm the association between TB diagnosis, SARS-CoV-2 infection, ICU admission, and COVID-19 death, and to examine the characteristics of patients that affected the outcome variables (Table 1). The variables reviewed for analysis were gender, age, residence, health insurance premium, Charlson comorbidity index (CCI) score, degree of disability, type of disability, disability, and tuberculosis diagnosis. The ages were categorized as 0–59, 60–69, 70–79, and 80+ years, and residence was classified based on regions with many COVID-19 confirmed cases (Seoul, Daegu, Gyeonggi-do, Gyeongsangbuk-do, and Others). The health insurance premium was used as a variable to reflect socioeconomic status, a main variable of interest in this study. In Korea, health insurance premiums are paid according to income level. Medical aid recipients fall under the low-income class, and do not pay health insurance premiums; those who do pay health insurance premiums are classified into the 1st quantile (lowest), 2nd quantile, 3rd quantile, 4th quantile, and 5th quantile (highest) according to the amount paid. The CCI score refers to the severity of the underlying disease, and the updated weights suggested by Quan et al. were assigned based on the 2019 medical records [10]. The characteristics of the people with disabilities were classified according to the degree of disability and type of disability. TB diagnosis was based on the medical record in 2019, and a history of TB as the main diagnosis or TB-related special calculation codes (‘R7860’, ‘V206’, ‘V246’, ‘V000’, ‘F009’, ‘F010’) were defined as a patient with TB. The ICD-10 codes for tuberculosis diagnosis were defined as ‘A15’, ‘A16’, ‘A17’, ‘A19’, ‘P370’, ‘U843’, and ‘U880’.

Table 1.
Baseline characteristics.
Logistic regression analysis was performed in order to analyze the effect of TB diagnosis on SARS-CoV-2 infection, ICU admission, and COVID-19 death. In the logistic regression model in which SARS-CoV-2 infection was set as an outcome variable, health insurance premiums, CCI scores, and disability were used as independent and adjustment variables. In the model that considered ICU admission and COVID-19 mortality due to SARS-CoV-2 infection as outcome variables, gender, age, region, CCI score, and disability were input as independent variables. The statistical analysis was performed using SAS 9.4, and statistical significance was set at p < 0.05.
2.3. Ethics Statement
This study followed Korean rules for de-identification of personal data and was accepted as a review-exempt study by Kyung Hee University’s Institutional Review Board (IRB No. KHSIRB-20-301(EA)). The board waived informed consent because the study used de-identified data.
3. Results
3.1. COVID-19 Patient Characteristics
The demographic characteristics of 8080 individuals with SARS-CoV-2 infections, 1020 ICU admissions, and 248 COVID-19 deaths are shown in Table 1. A Chi-square test was performed to compare the rates of SARS-CoV-2 infection, ICU admission, and COVID-19 death with the characteristics of the COVID-19 patients, and to determine the statistical significance. Looking at SARS-CoV-2 infections by demographic characteristics, 3244 out of 51,783 men (6.3%) and 4836 out of 77,345 women (6.3%) were infected with SARS-CoV-2. The infection rates according to health insurance premium levels were the highest for patients with medical benefits (10.9%). The higher the CCI score, the higher the SARS-CoV-2 infection rate (p < 0.001).
Approximately 12.6% of the patients were admitted to the ICU, and 3.1% of the patients died (p < 0.001). The intensive care unit admission and death rates were higher in male (15.9% and 4.2%, respectively) than in female patients. In ICU admission and COVID-19 death by age, the higher the age, the higher the ICU admission and COVID-19 death rate. However, the ICU admission rates for patients aged 0–9 years (12.3%) were higher than those for patients aged 40–49 years (10.2%). The ICU admission rate of COVID-19 patients was highest in the other areas (29.2%), while the COVID-19 mortality rate was higher in Gyeongsangbuk-do (5.8%). Patients with medical benefits (17.7%) had the highest ICU admission rates by health insurance premium level, and these rates increased as the health insurance premium level increased in general. The COVID-19 mortality rates showed a similar trend to the ICU admission rates. Higher CCI scores were associated with higher ICU admission and COVID-19 mortality rates.
3.2. TB and COVID-19 Infection, ICU Admission, and Mortality
3.3. Logistic Regression Analysis for SARS-CoV-2 Infection
Multivariate logistic regression analysis was performed in order to evaluate the impact of social factors on COVID-19 severity (Table 2). SARS-CoV-2 infection was used as the outcome variable in two logistic regression models, and the study revealed a link between SARS-CoV-2 infection and the most independent variables in the logistic regression model. Health insurance premiums, CCI scores, and tuberculosis were adjusted in multivariate model 1, and health insurance premiums, CCI scores, disability, and tuberculosis were adjusted in multivariate model 2. First, an analysis of the health insurance premium level of the COVID-19 patients showed that multivariate model 1 and multivariate model 2 were higher in patients with medical benefits. The higher the CCI score, the higher the risk of SARS-CoV-2 infection; this was statistically significant in models 1 and 2. However, statistical significance was not observed in patients with a CCI score of 1 compared with those with a CCI score of 0. The diagnosis of TB did not affect SARS-CoV-2 infection in either multivariate model 1 or 2.

Table 2.
Odds ratio for the risk of SARS-CoV-2 infection.
3.4. Logistic Regression Analysis for ICU Admission in COVID-19 Patients
Multivariate logistic regression analysis was performed in order to evaluate the impact of social factors on COVID-19 severity (Table 3). Two logistic regression models were created with ICU admission as the outcome variables, and the analysis showed an association between ICU admission and the most independent variables in the logistic regression model. Multivariate model 1 was adjusted for sex, age, region of residence, health insurance premium, CCI score, and tuberculosis, and multivariate model 2 was adjusted for sex, age, region of residence, health insurance premium, CCI score, disability, and tuberculosis. First, male patients had a higher probability of ICU admission. Patients under the age of 80 were at a lower probability of being admitted to the ICU. Patients aged 0–59 years had the lowest severity. By region, the risk of ICU admission was highest in the ‘Others’. However, statistical significance was not observed in patients who resided in Gyeonggi-do. The analysis of the health insurance premium level of ICU admission showed that multivariate models 1 and 2 were higher in patients with medical benefits. The higher the CCI score, the higher the risk of ICU admission, which was statistically significant. However, statistical significance was not observed in patients with a CCI score of 1 or 3+. The risk of ICU admission was higher in patients with tuberculosis according to multivariate model 1 (OR, 4.087; 95% CI, 1.223–13.663) and 2 (OR, 4.278; 95% CI, 1.272–14.386).

Table 3.
Odds ratio for the risk of ICU admission.
3.5. Logistic Regression Analysis for COVID-19 Death in COVID-19 Patients
Multivariate logistic regression analysis was performed in order to evaluate the impact of social factors on the death of COVID-19 patients (Table 4). Two logistic regression models were created with COVID-19 death as the outcome variables, and the analysis showed an association between COVID-19 death and the most independent variables in the logistic regression model. Sex, age, region of residence, health insurance premium, CCI score, disability, and tuberculosis were all adjusted in multivariate model 1, and sex, age, region of residence, health insurance premium, CCI score, disability, and TB were all adjusted in multivariate model 2. First, the risk of COVID-19 death was higher in male patients. Younger age groups were at a lower risk of COVID-19 death than patients over 80 years of age. Patients aged 0–59 years had the lowest severity. By region, the risk of COVID-19 death was highest in Gyeonggi-do. However, statistical significance was observed in patients who resided in Seoul and Gyeonggi-do. The analysis of the health insurance premium level of COVID-19 deaths showed that multivariate models 1 and 2 were higher in patients with medical benefits. The risk of COVID-19 death was the highest, with a CCI score of 1.

Table 4.
Odds ratio for the risk of COVID-19 death.
4. Discussion
In this study, we analyzed 129,128 people in the NHIS-COVID DB, including COVID-19 patients and controls, between 1 January and 30 May 2020, during the early stage of the COVID-19 epidemic in South Korea, when social distancing was not reinforced. Infection, ICU admission, and mortality due to COVID-19 increased in socioeconomically and physically vulnerable groups. However, the relationship between TB and SARS-CoV-2 infection and mortality was not evident, possibly owing to the small number of TB cases.
In the early phase of the epidemic, before the official announcement of social distancing from the Korean government, morbidity and death in the vulnerable group increased. Given that underserved populations were disproportionately affected by higher rates of both acute and chronic illness, received lower quality care, and experienced worse health-related outcomes [11], the patterns of SARS-CoV-2 infection seem to be similar in the early phase of the epidemic, when hospital beds were overwhelmed. Therefore, attention must be paid to the social needs of disadvantaged subpopulations that are not unnoticed during the COVID-19 pandemic [12].
Similarly to other reports, our study showed a higher rate of ICU admission and mortality in men and older adults [13]. In addition, the severity of underlying disease was related to SARS-CoV-2 infection and mortality, similarly to when the Charlson comorbidity index (CCI) was used as the comorbidity index [14], which means that higher mean CCI scores were associated with mortality [15]. However, the ICU admission rate was not related to the CCI score because the priority of ICU admission was not guided based on the COVID-19 severity score in the initial COVID-19 surge [15,16]. However, other comorbid conditions, such as obesity and peripheral vascular disease, must be investigated in order to determine their relationship with and influence on COVID-19 mortality.
TB was not related to COVID-19 infection, but was related to ICU admission after COVID-19 infection—excluding mortality from COVID-19—in our small dataset. Patients with COVID-19 who had recovered from TB seem to be devastated because of residual compromised lung function from TB sequelae [9]. Therefore, destructive changes in TB could contribute to respiratory failure with COPD symptoms, resulting in ICU admission [17]. In addition, as reported in the Philippines, time-to-recovery was reported to be significantly longer in COVID-19 patients with TB than in those without TB [18].
In our study, the included number of TB patients was only 216 patients for 5 months, which is a relatively low number compared with the average of 9925 patients for 5 months in 2019 [19].
The reduced reporting rate of TB could have resulted from decreased transmission associated with physical distancing and the increased use of face masks. In addition, the re-allocation of vacant human resources for TB contact investigation, the difficult accessibility of hospital clinics owing to COVID-19 pre-screening, and prioritized negative pressure units for admitted COVID-19 patients are influential reasons for the reduced TB reporting.
This study has several limitations. First, this study was performed based on the National Health Insurance System DB, without more accurate or precise clinical information in the early epidemic stage. Therefore, a more precise investigation with recent data in all regions in the midst of COVID-19 is warranted. Second, the reported TB numbers in this study are small; therefore, greater numbers of TB cases in the national TB control program DB should be joined with the COVID-19 DB in order to clarify the relationship between TB and SARS-CoV-2 infection. In addition, microbiologically confirmed TB cases excluding false positive diagnosis from imaging-only studies must be selected in order to decide the definite biological relationships between TB and COVID-19 infection. Lastly, because these data were taken before the settlement of triage for the intensive care unit capacity based on clinical severity score (Central Disease Control Headquarters, 2020) [20], an updated recent national analysis under the control of a governmental administrative order for ICU arrangement should be performed.
However, we concluded that—based on NHIS data in the early epidemic—SARS-CoV-2 infection, ICU admission, and mortality from COVID-19 were increased in socioeconomically and physically vulnerable groups. However, the relationship between TB and SARS-CoV-2 infection and mortality must be elucidated with a greater number of TB cases, revealing the possible underestimation of TB reporting in the COVID-19 pandemic era.
5. Conclusions
SARS-CoV-2 infection, ICU hospitalization, and COVID-19 mortality increased in socioeconomically and physically vulnerable populations during the early pandemic. However, because of suspected under-reporting of TB cases and the small number of TB patients, the link between tuberculosis, COVID-19, and death was not conclusive. With a larger number of TB cases, the connection between TB and SARS-CoV-2 infection and mortality can be better understood, exposing the potential underreporting of TB in the COVID-19 pandemic timeframe.
Author Contributions
Conceptualization: Y.W.L. and I.H.O. Data curation: J.Y.S. Formal analysis: J.Y.S. Methodology: Y.W.L. and J.Y.S. Writing—original draft: Y.W.L. Writing—review & editing: S.H.L. and I.H.O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI20C1068).
Institutional Review Board Statement
The Kyung Hee University Institutional Review Board (IRB No. KHSIRB-20-301(EA)) approved this study as a review-exempt study because it follows Korean guidelines for de-identification of personal data.
Informed Consent Statement
Because the study employed de-identified data, the board waived informed consent.
Data Availability Statement
The datasets generated and analyzed during the current study are not publicly available as the National Health Insurance Service (NHIS) kept the datasets for analysis within its closed network to prevent the leak of personal information.
Conflicts of Interest
There are no financial conflicts of interest to disclose. The author reports no conflicts of interest in this work.
References
- World Health Organization. Weekly Operational Update on COVID-19; World Health Organization (WHO): Geneva, Switzerland, 2021; Volume 53, pp. 1–10. [Google Scholar]
- World Health Organization. Rapid Communication on Forthcoming Changes to the Programmatic Management of Tuberculosis Preventive Treatment. Available online: http://apps.who.int/bookorders. (accessed on 21 March 2020).
- Lim, W.S.; Liang, C.K.; Assantachai, P.; Auyeung, T.W.; Kang, L.; Lee, W.J.; Lim, J.; Sugimoto, K.; Akishita, M.; Chia, S.; et al. COVID-19 and older people in Asia: Asian Working Group for Sarcopenia calls to actions. Geriatr. Gerontol. Int. 2020, 20, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Courtenay, K.; Perera, B. Courtenay and Perera, COVID-19 and people with intellectual disability: Impacts of a pandemic. Ir. J. Psychol. Med. 2020, 37, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.A.; Ahmed, Z.; Younas, S. COVID-19 and comorbidities: Deleterious impact on infected patients. J. Infect. Public Health 2020, 13, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wang, Y.; Fleming, J.; Yu, Y.; Gu, Y.; Liu, C.; Fan, L.; Wang, X.; Cheng, M.; Bi, L.; et al. Active or latent tuberculosis increases susceptibility to COVID-19 and disease severity. MedRxiv 2020, 165, 1–13. [Google Scholar]
- Korea Centers for Disease Control and Prevention. 2020 Annual Report on the Notified Tuberculosis in Korea. Available online: https://www.kdca.go.kr/board/board.es?mid=a20602010000&bid=0034&act=view&list_no=712904 (accessed on 1 September 2021).
- Udwadia, Z.F.; Vora, A.; Tripathi, A.R.; Malu, K.N.; Lange, C.; Raju, R.S. COVID-19 -Tuberculosis interactions: When dark forces collide. Indian J. Tuberc. 2020, 67, S155–S162. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grief, S.N.; Miller, J.P. Infectious Disease Issues in Underserved Populations. Prim. Care Clin. Off. Pr. 2017, 44, 67–85. [Google Scholar] [CrossRef] [PubMed]
- Quinn, S.C.; Kumar, S. Health Inequalities and Infectious Disease Epidemics: A Challenge for Global Health Security. Biosecurity Bioterrorism Biodefense Strategy Pract. Sci. 2014, 12, 263–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cannistraci, C.V.; Valsecchi, M.G.; Capua, I. Age-sex population adjusted analysis of disease severity in epidemics as a tool to devise public health policies for COVID-19. Sci. Rep. 2021, 11, 11787. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-Q.; Gou, R.; Diao, Y.-S.; Yin, Q.-H.; Fan, W.-X.; Liang, Y.-P.; Chen, Y.; Wu, M.; Zang, L.; Li, L.; et al. Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. J. Zhejiang Univ. Sci. B 2014, 15, 58–66. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuswardhani, R.T.; Henrina, J.; Pranata, R.; Lim, M.A.; Lawrensia, S.; Suastika, K. Charlson comorbidity index and a composite of poor outcomes in COVID-19 patients: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 2103–2109. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Park, S.Y.; Seon, J.Y.; Jeon, W.H.; Nam, S.I.; Park, J.H.; Park, J.S.; Kim, H.Y.; Thakkar, N.; Selvaraj, P.; et al. Intensive Care Unit Capacity and Its Associated Risk Factors During the COVID-19 Surge in the Republic of Korea: Analysis Using Nationwide Health Claims Data. Risk Manag. Healthc. Policy. 2020, 2020, 2571–2581. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarti, B.; Calverley, P.M.; Davies, P.D. Tuberculosis and its incidence, special nature, and relationship with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 2007, 2, 263–272. [Google Scholar] [PubMed]
- Sy, K.T.L.; Haw, N.J.L.; Uy, J. Previous and active tuberculosis increases risk of death and prolongs recovery in patients with COVID-19. Infect. Dis. 2020, 52, 902–907. [Google Scholar] [CrossRef] [PubMed]
- Korea Disease Control and Prevention Agency. 2019 Annual Report on the Notified Tuberculosis in Korea. 2019. Available online: https://nih.go.kr/board/board.es?mid=a40303030000&bid=0034&act=view&list_no=366715 (accessed on 1 September 2021).
- Central Disease Control Headquarters. 2020 Coronavirus Infectious Disease-19 Response Guidelines (7th Edition). 2020. Available online: https://www.kdca.go.kr/board/board.es?mid=a20507020000&bid=0019 (accessed on 1 September 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).