Does Treatment Readiness Shape Service-Design Preferences of Gay, Bisexual, and Other Men Who Have Sex with Men Who Use Crystal Methamphetamine? A Cross Sectional Study
Abstract
1. Introduction
2. Material and Methods
2.1. Protocol
2.2. Variables
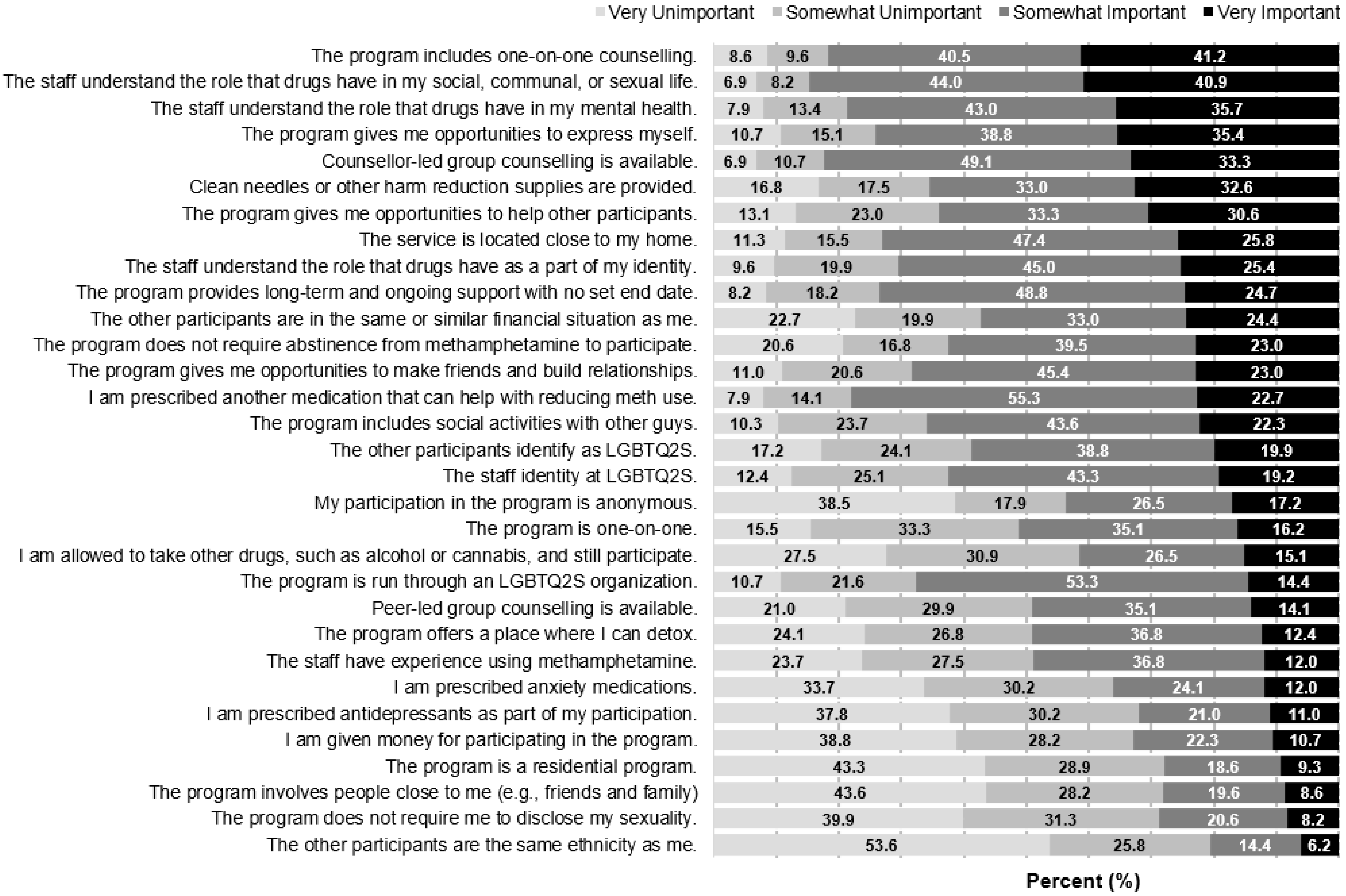
2.2.1. Service Design Preferences
2.2.2. Readiness to Change
2.2.3. Demographic and Behavioural Characteristics
2.3. Data Analysis
2.4. Ethical Approval
3. Results
3.1. Sample Description
3.2. Preferred Program Characteristics and Association with SOCRATES Subscale Scores
3.2.1. Staff Characteristics
3.2.2. Participant Characteristics
3.2.3. Host Organization Characteristics
3.2.4. Privacy and Disclosure Characteristics
3.2.5. Intervention Characteristics
3.2.6. Ideal Session Time, Frequency, and Duration
3.2.7. Benefits of Participation
3.2.8. Willingness to Participate
4. Discussion
4.1. Key Findings
4.2. Implications
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Demant, D.; Hides, L.; Kavanagh, D.J.; White, K.M.; Winstock, A.R.; Ferris, J. Differences in substance use between sexual orientations in a multi-country sample: Findings from the Global Drug Survey 2015. J. Public Health 2017, 39, 532–541. [Google Scholar] [CrossRef] [PubMed]
- Green; Halkitis, P.N. Crystal methamphetamine and sexual sociality in an urban gay subculture: An elective affinity. Cult. Health Sex. 2006, 8, 317–333. [Google Scholar] [CrossRef]
- Watt, M.H.; Myers, B.; Towe, S.L.; Meade, C.S. The mental health experiences and needs of methamphetamine users in Cape Town: A mixed methods study. S. Afr. Med. J. Suid-Afr. Tydskr. Vir Geneeskd. 2015, 105, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Knight, R.; Karamouzian, M.; Carson, A.; Edward, J.; Carrieri, P.; Shoveller, J.; Fairbairn, N.; Wood, E.; Fast, D. Interventions to address substance use and sexual risk among gay, bisexual and other men who have sex with men who use methamphetamine: A systematic review. Drug Alcohol. Depend. 2019, 194, 410–429. [Google Scholar] [CrossRef]
- Lea, T.; Kolstee, J.; Lambert, S.; Ness, R.; Hannan, S.; Holt, M. Methamphetamine treatment outcomes among gay men attending a LGBTI-specific treatment service in Sydney, Australia. PLoS ONE 2017, 12, e0172560. [Google Scholar] [CrossRef] [PubMed]
- Allen, R.S.; Olson, B.D. Predicting Attrition in the Treatment of Substance Use Disorders. J. Addict. Res. Ther. 2015, 6, 728–742. [Google Scholar] [CrossRef]
- Ciketic, S.; Hayatbakhsh, M.R.; Doran, C.M.; Najman, J.M.; McKetin, R. A review of psychological and pharmacological treatment options for methamphetamine dependence. J. Subst. Use 2012, 17, 363–383. [Google Scholar] [CrossRef]
- Hansten, M.L.; Downey, L.; Rosengren, D.B.; Donovan, D.M. Relationship between follow-up rates and treatment outcomes in substance abuse research: More is better but when is “enough” enough? Addiction 2000, 95, 1403–1416. [Google Scholar] [CrossRef]
- Harley, M.; Pit, S.W.; Rees, T.; Thomas, S. Completion rates and psychosocial intervention effectiveness in an Australian substance use therapeutic community. Subst. Abuse Treat. Prev. Policy 2018, 13, 33. [Google Scholar] [CrossRef] [PubMed]
- Loveland, D.; Driscoll, H. Examining attrition rates at one specialty addiction treatment provider in the United States: A case study using a retrospective chart review. Subst. Abuse Treat. Prev. Policy 2014, 9, 41. [Google Scholar] [CrossRef] [PubMed]
- Ronsley, C.; Nolan, S.; Knight, R.; Hayashi, K.; Klimas, J.; Walley, A.; Wood, E.; Fairbairn, N. Treatment of stimulant use disorder: A systematic review of reviews. PLoS ONE 2020, 15, 0234809. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, R.; Brown, L.; Shattell, M.; Wright, T.; Lewallen, L. Harm Reduction: Compassionate Care Of Persons with Addictions. Medsurg Nurs. Off. J. Acad. Med.-Surg. Nurses 2013, 22, 349–358. [Google Scholar]
- Green, A.I. “chem friendly”: The institutional basis of “club-drug” use in a sample of urban gay men. Deviant Behav. 2003, 24, 427–447. [Google Scholar] [CrossRef]
- Bryant, J.; Hopwood, M.; Dowsett, G.W.; Aggleton, P.; Holt, M.; Lea, T.; Drysdale, K.; Treloar, C. The rush to risk when interrogating the relationship between methamphetamine use and sexual practice among gay and bisexual men. Int. J. Drug Policy 2018, 55, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Marchand, K.; Beaumont, S.; Westfall, J.; MacDonald, S.; Harrison, S.; Marsh, D.C.; Schechter, M.T.; Oviedo-Joekes, E. Conceptualizing patient-centered care for substance use disorder treatment: Findings from a systematic scoping review. Subst. Abuse Treat. Prev. Policy 2019, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Steinka-Fry, K.T.; Tanner-Smith, E.E.; Dakof, G.A.; Henderson, C. Culturally sensitive substance use treatment for racial/ethnic minority youth: A meta-analytic review. J. Subst. Abuse Treat. 2017, 75, 22–37. [Google Scholar] [CrossRef]
- Knight, R. Investments in implementation science are needed to address the harms associated with the sexualized use of substances among gay, bisexual and other men who have sex with men. J. Int. AIDS Soc. 2018, 21, e25141. [Google Scholar] [CrossRef]
- Harawa, N.T.; Williams, J.K.; Ramamurthi, H.C.; Manago, C.; Avina, S.; Jones, M. Sexual Behavior, Sexual Identity, and Substance Abuse among Low-Income Bisexual and Non-Gay-Identifying African American Men Who Have Sex with Men. Arch. Sex. Behav. 2008, 37, 748–762. [Google Scholar] [CrossRef]
- Alexander, A.C.; Obong’o, C.O.; Chavan, P.P.; Dillon, P.J.; Kedia, S.K. Addicted to the ‘life of methamphetamine’: Perceived barriers to sustained methamphetamine recovery. Drugs Educ. Prev. Policy 2018, 25, 241–247. [Google Scholar] [CrossRef]
- Herbeck, D.M.; Brecht, M.-L.; Christou, D.; Lovinger, K. A Qualitative Study of Methamphetamine Users’ Perspectives on Barriers and Facilitators of Drug Abstinence. J. Psychoact. Drugs 2014, 46, 215–225. [Google Scholar] [CrossRef]
- Vayr, F.; Herin, F.; Jullian, B.; Soulat, J.M.; Franchitto, N. Barriers to seeking help for physicians with substance use disorder: A review. Drug Alcohol. Depend. 2019, 199, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Tonigan, J.S. Assessing drinkers’ motivation for change: The Stages of Change Readiness and Treatment Eagerness Scale (SOCRATES). Psychol. Addict. Behav. 1996, 10, 81–89. [Google Scholar] [CrossRef]
- Compton, W.M.; Jones, C.M.; Underwood, N. Reducing negative consequences from use of methamphetamine. Addiction 2020, 115, 1190–1191. [Google Scholar] [CrossRef] [PubMed]
- Pinkham, S.; Stone, K. A Global Review of the Harm Reduction Response to Amphetamines: A 2015 Update; International Harm Reduction Association: London, UK, 2015. [Google Scholar]
- McGuire, M.; Card, K.G.; Lachowsky, N.J. The Crystal Methamphetamine Project: Understanding the Need for Culturally-Safe Supports and Services Addressing Crystal Methamphetamine Use among Gay, Bi, and Queer Men (Both Cis and Trans); Community-Based Research Centre: Vancouver, BC, Canada, 2020. [Google Scholar]
- Abiola, T.; Udofia, O.; Sheikh, T.L.; Sanni, K. Assessing Change Readiness and Treatment Eagerness among Psychoactive Substance Users in Northern Nigeria. J. Subst. Abuse Treat. 2015, 58, 72–77. [Google Scholar] [CrossRef]
- Bertholet, N.; Dukes, K.; Horton, N.J.; Palfai, T.P.; Pedley, A.; Saitz, R. Factor structure of the SOCRATES questionnaire in hospitalized medical patients. Addict. Behav. 2009, 34, 568–572. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mitchell, D.; Angelone, D.J. Assessing the validity of the Stages of Change Readiness and Treatment Eagerness Scale with treatment-seeking military service members. Mil. Med. 2006, 171, 900–904. [Google Scholar] [CrossRef] [PubMed]
- Napper, L.E.; Wood, M.M.; Jaffe, A.; Fisher, D.G.; Reynolds, G.L.; Klahn, J.A. Convergent and discriminant validity of three measures of stage of change. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav. 2008, 22, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Carey, K.B.; Maisto, S.A.; Carey, M.P.; Purnine, D.M. Measuring readiness-to-change substance misuse among psychiatric outpatients: I. Reliability and validity of self-report measures. J. Stud. Alcohol. 2001, 62, 79–88. [Google Scholar] [CrossRef][Green Version]
- Nanín, J.E.; Parsons, J.T.; Bimbi, D.S.; Grov, C.; Brown, J.T. Community Reactions to Campaigns Addressing Crystal Methamphetamine Use among Gay and Bisexual Men in New York City. J. Drug Educ. 2006, 36, 297–315. [Google Scholar] [CrossRef] [PubMed]
- Hughes, R.A.; Heron, J.; Sterne, J.A.C.; Tilling, K. Accounting for missing data in statistical analyses: Multiple imputation is not always the answer. Int. J. Epidemiol. 2019, 48, 1294–1304. [Google Scholar] [CrossRef] [PubMed]
- Burrow-Sánchez, J.J.; Corrales, C.; Totsky, J. Predictive Validity of the SOCRATES in a Clinical Sample of Latina/o Adolescents. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav. 2019, 33, 171–177. [Google Scholar] [CrossRef]
- Brecht, M.-L.; Anglin, M.D.; Dylan, M. Coerced treatment for methamphetamine abuse: Differential patient characteristics and outcomes. Am. J. Drug Alcohol Abuse 2005, 31, 337–356. [Google Scholar] [CrossRef] [PubMed]
- Van Horn, D.H.A.; Drapkin, M.; Lynch, K.G.; Rennert, L.; Goodman, J.D.; Thomas, T.; Ivey, M.; McKay, J.R. Treatment choices and subsequent attendance by substance-dependent patients who disengage from intensive outpatient treatment. Addict. Res. Theory 2015, 23, 391–403. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Martos, A.J.; Wilson, P.A.; Meyer, I.H. Lesbian, gay, bisexual, and transgender (LGBT) health services in the United States: Origins, evolution, and contemporary landscape. PLoS ONE 2017, 12, e0180544. [Google Scholar] [CrossRef] [PubMed]
- Race, K.; Murphy, D.; Pienaar, K.; Lea, T. Injecting as a sexual practice: Cultural formations of ‘slamsex’. Sexualities 2021, 1, 1–18. [Google Scholar] [CrossRef]
- Souleymanov, R.; Brennan, D.J.; Logie, C.; Allman, D.; Craig, S.L.; Halkitis, P.N. Pleasure and HIV biomedical discourse: The structuring of sexual and drug-related risks for gay and bisexual men who Party-n-Play. Int. J. Drug Policy 2019, 74, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Braine, N.; Acker, C.J.; van Sluytman, L.; Friedman, S.; Des Jarlais, D.C. Drug Use, Community Action, and Public Health: Gay Men and Crystal Meth in NYC. Subst. Use Misuse 2011, 46, 368–380. [Google Scholar] [CrossRef] [PubMed]
- Green, K.E.; Feinstein, B.A. Substance Use in Lesbian, Gay, and Bisexual Populations: An Update on Empirical Research and Implications for Treatment. Psychol. Addict. Behav. 2012, 26, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Mericle, A.A.; de Guzman, R.; Hemberg, J.; Yette, E.; Drabble, L.; Trocki, K. Delivering LGBT-sensitive substance use treatment to sexual minority women. J. Gay Lesbian Soc. Serv. 2018, 30, 393–408. [Google Scholar] [CrossRef] [PubMed]
- Crescenzo, F.D.; Ciabattini, M.; D’Alò, G.L.; Giorgi, R.D.; Giovane, C.D.; Cassar, C.; Janiri, L.; Clark, N.; Ostacher, M.J.; Cipriani, A. Comparative efficacy and acceptability of psychosocial interventions for individuals with cocaine and amphetamine addiction: A systematic review and network meta-analysis. PLoS Med. 2018, 15, e1002715. [Google Scholar] [CrossRef] [PubMed]
- Benishek, L.A.; Dugosh, K.L.; Kirby, K.C.; Matejkowski, J.; Clements, N.T.; Seymour, B.L.; Festinger, D.S. Prize-based contingency management for the treatment of substance abusers: A meta-analysis. Addict. Abingdon Engl. 2014, 109, 1426–1436. [Google Scholar] [CrossRef]
- McPherson, S.M.; Burduli, E.; Smith, C.L.; Herron, J.; Oluwoye, O.; Hirchak, K.; Orr, M.F.; McDonell, M.G.; Roll, J.M. A review of contingency management for the treatment of substance-use disorders: Adaptation for underserved populations, use of experimental technologies, and personalized optimization strategies. Subst. Abuse Rehabil. 2018, 9, 43–57. [Google Scholar] [CrossRef] [PubMed]
- Menza, T.W.; Jameson, D.R.; Hughes, J.P.; Colfax, G.N.; Shoptaw, S.; Golden, M.R. Contingency management to reduce methamphetamine use and sexual risk among men who have sex with men: A randomized controlled trial. BMC Public Health 2010, 10, 774. [Google Scholar] [CrossRef]
- Carrico, A.W.; Gómez, W.; Siever, M.D.; Discepola, M.V.; Dilworth, S.E.; Moskowitz, J.T. Pilot randomized controlled trial of an integrative intervention with methamphetamine-using men who have sex with men. Arch. Sex. Behav. 2015, 44, 1861–1867. [Google Scholar] [CrossRef] [PubMed]
- Reback, C.J.; Shoptaw, S. Development of an evidence-based, gay-specific cognitive behavioral therapy intervention for methamphetamine-abusing gay and bisexual men. Addict. Behav. 2014, 39, 1286–1291. [Google Scholar] [CrossRef] [PubMed]
- Shoptaw, S.; Reback, C.J.; Peck, J.A.; Yang, X.; Rotheram-Fuller, E.; Larkins, S.; Veniegas, R.C.; Freese, T.E.; Hucks-Ortiz, C. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug Alcohol. Depend. 2005, 78, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Johnson, T.P. Sources of Error in Substance Use Prevalence Surveys. Int. Sch. Res. Not. 2014, 2014, 923290. [Google Scholar] [CrossRef] [PubMed]
- Salway, T.J.; Morgan, J.; Ferlatte, O.; Hawkins, B.; Lachowsky, N.J.; Gilbert, M. A Systematic Review of Characteristics of Nonprobability Community Venue Samples of Sexual Minority Individuals and Associated Methods for Assessing Selection Bias. LGBT Health 2019, 6, 205–215. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (%)/Median (Q1–Q3) |
|---|---|
| Age | 41 (34–51) |
| Person of Colour | |
| Yes | 83 (28.5) |
| No | 208 (71.5) |
| Gender | |
| Cisgender | 269 (92.4) |
| Trans/Non-binary | 22 (7.6) |
| Sexual Identity | |
| Gay | 231 (79.4) |
| Bisexual | 34 (11.7) |
| Other | 26 (8.9) |
| Province | |
| Atlantic and Eastern Canada | 155 (53.3) |
| The Prairies | 32 (11.0) |
| Western Canada | 104 (35.7) |
| Person Living with HIV | |
| Yes | 107 (36.8) |
| No | 184 (63.2) |
| Annual Income (CAD) | |
| Less than $29,999 | 100 (34.4) |
| $30,000–$59,000 | 99 (34.0) |
| $60,000–$89,999 | 52 (17.9) |
| $90,000 or more | 40 (13.7) |
| Frequency of CM Use in P6M | |
| Daily or Almost Daily | 102 (35.1) |
| Weekly | 48 (16.5) |
| Monthly | 49 (16.8) |
| Once or Twice | 92 (31.6) |
| Self-reported Readiness to take action on CM Use | |
| No perceived problem with CM Use | 113 (38.7) |
| Not ready to take action on CM Use | 57 (19.5) |
| Ready to take action on CM Use | 291 (41.7) |
| SOCRATES Subscales | |
| Contemplativeness (Range 4–20) | 12 (9–15) |
| Readiness (Range 4–35) | 21 (14–26) |
| Action-taking (Range 8–40) | 24 (18–29) |
| Outcome Variable | Average Rating (1–4) | Primary Explanatory Variable | ||
|---|---|---|---|---|
| Contemplativeness | Readiness | Action-Taking | ||
| aOR (95%CI) | aOR (95%CI) | aOR (95%CI) | ||
| Staff Characteristics | ||||
| The staff identity as LGBTQ2S. A | 2.62 | 1.07 (1.01, 1.13) | 1.02 (0.99, 1.06) | 1.02 (0.99, 1.05) |
| The staff have experience using methamphetamine. A | 2.22 | 1.03 (0.97, 1.09) | 1.02 (0.99, 1.06) | 1.02 (0.99, 1.05) |
| The staff understand the role that drugs have in my social, communal, or sexual life. A | 3.14 | 1.09 (1.03, 1.16) | 1.06 (1.02, 1.10) | 1.06 (1.02, 1.09) |
| The staff understand the role that drugs have as a part of my identity. A | 2.86 | 1.11 (1.05, 1.18) | 1.07 (1.03, 1.10) | 1.05 (1.02, 1.09) |
| The staff understand the role that drugs have in my mental health. A | 3.09 | 1.10 (1.03, 1.16) | 1.09 (1.05, 1.12) | 1.04 (1.01, 1.07) |
| Program Participant Characteristics | ||||
| The other participants are in the same or similar financial situation as me. A | 2.81 | 1.04 (0.98, 1.10) | 1.01 (0.98, 1.04) | 0.98 (0.95, 1.01) |
| The other participants are the same ethnicity as me. A | 1.73 | 0.99 (0.94, 1.05) | 0.99 (0.96, 1.03) | 1.00 (0.97, 1.03) |
| The other participants identify as LGBTQ2S. A | 2.65 | 1.04 (0.98, 1.10) | 1.01 (0.98, 1.05) | 1.01 (0.98, 1.05) |
| The program involves people close to me. A | 1.94 | 1.06 (1.00, 1.12) | 1.03 (1.00, 1.07) | 1.02 (1.00, 1.05) |
| The program includes social activities with other guys. A | 2.69 | 1.08 (1.02, 1.15) | 1.04 (1.01, 1.07) | 1.04 (1.01, 1.07) |
| The program gives me opportunities to help other participants. A | 2.90 | 1.07 (1.01, 1.13) | 1.06 (1.03, 1.10) | 1.04 (1.01, 1.07) |
| The program gives me opportunities to make friends and build relationships. A | 2.78 | 1.14 (1.08, 1.21) | 1.08 (1.05, 1.12) | 1.07 (1.03, 1.10) |
| Host Organization Characteristics | ||||
| The program is run through an LGBTQ2S organization. A | 2.37 | 1.07 (1.01, 1.13) | 1.02 (0.98, 1.05) | 1.00 (0.97, 1.03) |
| The service is located close to my home. A | 2.88 | 1.05 (0.99, 1.11) | 1.02 (0.98, 1.05) | 1.02 (0.99, 1.05) |
| Privacy and Disclosure Characteristics | ||||
| My participation in the program is anonymous. A | 2.59 | 1.04 (0.99, 1.10) | 1.03 (0.99, 1.06) | 1.01 (0.99, 1.04) |
| The program does not require me to disclose my sexuality. A | 1.93 | 1.06 (1.00, 1.12) | 1.00 (0.97, 1.03) | 1.03 (1.00, 1.06) |
| The program is one-on-one. A | 2.52 | 1.05 (0.99, 1.11) | 1.02 (0.99, 1.05) | 1.01 (0.98, 1.04) |
| Intervention Characteristics | ||||
| The program gives me opportunities to express myself. A | 3.07 | 1.07 (1.01, 1.13) | 1.05 (1.02, 1.09) | 1.03 (1.00, 1.06) |
| The program is a residential program. A | 1.97 | 1.12 (1.06, 1.19) | 1.08 (1.05, 1.12) | 1.03 (1.00, 1.07) |
| The program offers a place where I can detox. A | 2.29 | 1.09 (1.03, 1.15) | 1.07 (1.03, 1.10) | 1.02 (1.00, 1.05) |
| The program includes one-on-one counselling. A | 3.19 | 1.13 (1.07, 1.20) | 1.08 (1.05, 1.12) | 1.04 (1.01, 1.08) |
| Counsellor-led group counselling is available. A | 2.99 | 1.10 (1.04, 1.16) | 1.07 (1.04, 1.11) | 1.04 (1.01, 1.07) |
| Peer-led group counselling is available. A | 2.37 | 1.10 (1.04, 1.17) | 1.07 (1.03, 1.11) | 1.06 (1.03, 1.10) |
| Harm Reduction Characteristics | ||||
| The program provides long-term and ongoing support with no set end date. A | 2.81 | 1.12 (1.05, 1.18) | 1.07 (1.04, 1.11) | 1.04 (1.01, 1.07) |
| The program does not require abstinence from methamphetamine to participate. A | 2.80 | 1.00 (0.95, 1.06) | 0.99 (0.96, 1.03) | 1.00 (0.97, 1.03) |
| I am allowed to take other drugs, such as alcohol or cannabis, and still participate. A | 2.42 | 0.98 (0.93, 1.04) | 0.98 (0.95, 1.02) | 0.99 (0.96, 1.02) |
| Clean needles or other harm reduction supplies are provided. A | 2.93 | 1.04 (0.99, 1.10) | 1.01 (0.98, 1.04) | 1.01 (0.98, 1.04) |
| Ideal Session Time, Frequency, and Duration | ||||
| Program Duration (In Number of Sessions) B | - | 1.01 (1.00, 1.02) | 1.02 (1.02, 1.03) | 1.01 (1.01, 1.02) |
| Program Duration (In Weeks) B | - | 1.01 (1.00, 1.02) | 1.01 (1.01, 1.02) | 1.02 (1.01, 1.02) |
| Session Time Commitment (In Hours) A | - | 1.11 (1.05, 1.17) | 1.06 (1.02, 1.09) | 1.06 (1.02, 1.09) |
| Session Frequency A | - | 1.05 (1.00, 1.12) | 1.08 (1.04, 1.11) | 1.03 (1.00, 1.06) |
| Ideal Benefits of Participation | ||||
| Session Honorarium Amount (CAD/visit) B | - | 0.95 (0.95, 0.96) | 0.99 (0.99, 0.99) | 0.97 (0.97, 0.97) |
| I am given money for participating in the program. A | 2.05 | 0.99 (0.93, 1.04) | 1.00 (0.96, 1.03) | 1.00 (0.97, 1.03) |
| I am prescribed antidepressants as part of my participation. A | 2.05 | 1.11 (1.05, 1.18) | 1.06 (1.03, 1.10) | 1.04 (1.01, 1.07) |
| I am prescribed anxiety medications as part of my participation. A | 2.14 | 1.08 (1.02, 1.14) | 1.07 (1.04, 1.11) | 1.03 (1.00, 1.06) |
| I am prescribed another medication that can help with reducing MA use. A | 2.71 | 1.10 (1.04, 1.17) | 1.07 (1.03, 1.10) | 1.04 (1.01, 1.07) |
| Willingness to Participate in a… | ||||
| Program Designed to Help Participants Quit using MA C | - | 1.20 (1.12, 1.28) | 1.13 (1.09, 1.19) | 1.10 (1.06, 1.14) |
| Program Designed to Help Participants Control MA use C | - | 1.17 (1.09, 1.27) | 1.12 (1.06, 1.18) | 1.08 (1.04, 1.12) |
| Program Designed to Help Participants Stop using MA Temporarily C | - | 1.18 (1.10, 1.27) | 1.14 (1.09, 1.20) | 1.10 (1.06, 1.14) |
| In a Placebo-Controlled RCT testing a Pharmacological Intervention C | - | 1.16 (1.08, 1.25) | 1.09 (1.05, 1.15) | 1.06 (1.02, 1.10) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Card, K.G.; McGuire, M.; Berlin, G.W.; Wells, G.A.; Fulcher, K.; Nguyen, T.; Hart, T.A.; Skakoon Sparling, S.; Lachowsky, N.J. Does Treatment Readiness Shape Service-Design Preferences of Gay, Bisexual, and Other Men Who Have Sex with Men Who Use Crystal Methamphetamine? A Cross Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 3458. https://doi.org/10.3390/ijerph19063458
Card KG, McGuire M, Berlin GW, Wells GA, Fulcher K, Nguyen T, Hart TA, Skakoon Sparling S, Lachowsky NJ. Does Treatment Readiness Shape Service-Design Preferences of Gay, Bisexual, and Other Men Who Have Sex with Men Who Use Crystal Methamphetamine? A Cross Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(6):3458. https://doi.org/10.3390/ijerph19063458
Chicago/Turabian StyleCard, Kiffer G., Madison McGuire, Graham W. Berlin, Gordon A. Wells, Karyn Fulcher, Tribesty Nguyen, Trevor A. Hart, Shayna Skakoon Sparling, and Nathan J. Lachowsky. 2022. "Does Treatment Readiness Shape Service-Design Preferences of Gay, Bisexual, and Other Men Who Have Sex with Men Who Use Crystal Methamphetamine? A Cross Sectional Study" International Journal of Environmental Research and Public Health 19, no. 6: 3458. https://doi.org/10.3390/ijerph19063458
APA StyleCard, K. G., McGuire, M., Berlin, G. W., Wells, G. A., Fulcher, K., Nguyen, T., Hart, T. A., Skakoon Sparling, S., & Lachowsky, N. J. (2022). Does Treatment Readiness Shape Service-Design Preferences of Gay, Bisexual, and Other Men Who Have Sex with Men Who Use Crystal Methamphetamine? A Cross Sectional Study. International Journal of Environmental Research and Public Health, 19(6), 3458. https://doi.org/10.3390/ijerph19063458






