Nature-Based Interventions for Psychological Wellbeing in Long-Term Conditions: A Systematic Review
Abstract
:1. Introduction
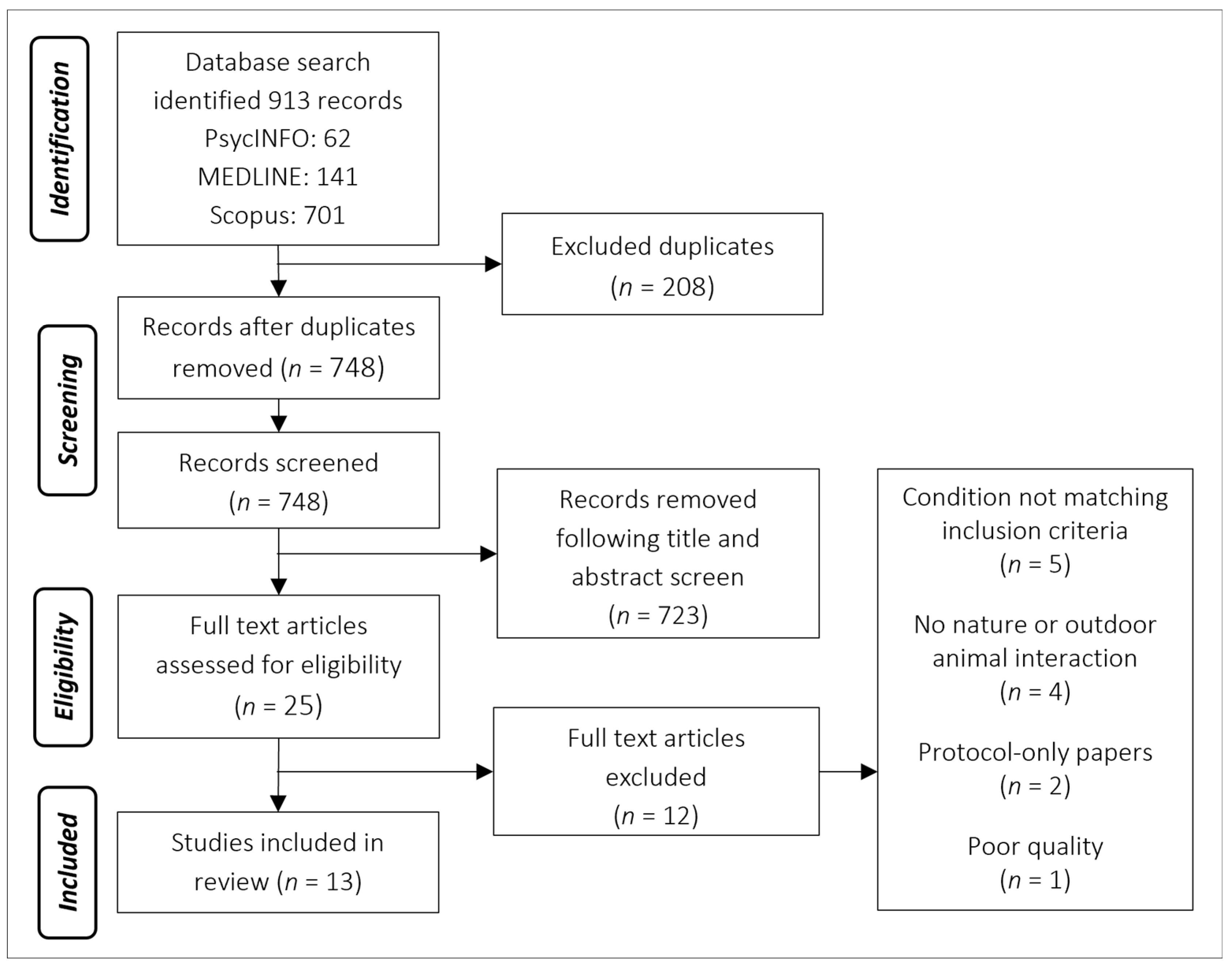
2. Materials and Methods
2.1. Study Selection
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
- Nature-based intervention conducted inside or outside or animal-based intervention conducted in outdoors environments;
- Involves an active intervention rather than just passive proximity to, e.g., greenspace;
- Studies with a minimum of 50% participants with at least one diagnosed long-term physical health condition, limited to cardiovascular disease, stroke, lung and liver disease, type II diabetes or chronic kidney disease, but not excluding other co-morbidities;
- Measuring psychometrically robust psychological outcomes, including (but not limited to) QoL.
2.2.2. Exclusion Criteria
- Not specific to long-term conditions listed above;
- Participants within end-of-life pathways (e.g., palliative care).
2.3. Search Strategy
2.4. Data Extraction
2.5. Quality Appraisal
3. Results
3.1. Study Characteristics
| Author (Year) | Research Design | Participants | Intervention | Control | Psychological Measurements | Psychological Outcomes | Physiological Measurements | Physiological Outcomes |
|---|---|---|---|---|---|---|---|---|
| Beinotti et al. (2013) [34] | Single-blind RCT | 20 patients (6 female) ≥1 year post-stroke Mean age 55.5 years | 16 weeks physio and horse-riding therapy (10 participants) Mean age 59 years | 16 weeks physio only (10 participants) Mean age 52 years | Medical Outcomes Study 36-item Short-Form health survey Measurements before and after the intervention | Significant improvement in functional capacity, physical aspects and mental health following horseback riding therapy compared to controls. No changes in general health state, vitality or emotional aspects | N/A | N/A |
| Chun et al. (2017) [45] | Two-sample randomised cohort | 59 participants (19 female) Mean age 60.8 years (SD 9.1) | Forest therapy programme (30 participants) 4-day trip involving meditation, experiencing the forest and walking | Urban comparison (29 participants) 4-day trip involving meditation and walking in the hotel | Beck Depression Inventory (BDI) Hamilton Depression Rating Scale (HAM-D17) Spielberger State-Trait Anxiety Inventory (STAI) Measurements before and after the intervention | Reduced BDI, HAM-D17 and STAI scores following forest therapy programme compared to baseline. Increased STAI scores in urban group following programme | Oxidative stress: total oxidant capacity and iron-reducing activity Measurements before and after the intervention | No significant differences between forest and urban groups |
| Pohl et al. (2018) [46] | Qualitative exploration | 18 participants (6 female) Mean age 60.3 1–5 years post-stroke | 12-week multi-modal intervention incorporating horseback riding | No comparison group | Individual face-to-face semi-structured interviews | Four themes identified: transformative experiences, human–horse interaction, togetherness and belonging, and the all-in-one solution | N/A | N/A |
| Jia et al. (2016) [47] | Two-sample randomised cohort | 20 COPD patients (6 female) Mean age 70.1 years | Forest walking (10 participants) Mean age 70.1 (range 67–77) 7 days at forest site with scheduled walking time, staying in a hotel | City walking (8 participants) Mean age 70 (range 61–79) 7 days at city site with scheduled walking time, staying in a hotel | Profile of Mood State (POMS) Measurements before and after the intervention | Lower POMS scores of “tension–anxiety”, “depression” and “anger–hostility” in forest but not city group | Lymphocytes: NK, NKT-like and CD8+ T-cells expression of intracellular perforin and granzyme B Pro-inflammatory cytokines: interferon-γ (IFN-γ), interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-1β (IL-1β), tumour necrosis factorα (TNF-α) and C-reactive protein (CRP) COPD-associated factors: pulmonary and activation-regulated chemokine (PARC/CCL-18), surfactant protein D (SP-D) and tissue inhibitor of metalloproteinase (TIMP-1) Stress hormones: serum cortisol and epinephrine Measurements before and after the intervention | Lymphocytes: no significant group difference in proportion of NK, NKT-like and CD8+ T-cells, nor their expression of granzyme B. Significant reduction of NK, NKT-like and CD8+ T-cell expression of intracellular perforin after forest bathing but not city group. Pro-inflammatory cytokines: significant reduction of IFN-γ, IL-6 and IL-8 after forest bathing but not city group. Slight decrease in IL-1β, TNF-α and CRP after forest bathing but not city group. COPD-associated factors: significant decrease in PARC/CCL-18 TIMP-1 after forest bathing but not city group. No significant change in SP-D in either group. Stress hormones: significant decrease in serum cortisol and epinephrine after forest bathing but not city group |
| Song et al. (2015) [52] | Two-sample randomised cross-over cohort study | 20 male participants with high-normal blood pressure (HNBP) or hypertension Mean age 58.0 years (SD 10.6) | Forest walking 17 min walk All participants completed both interventions on 2 consecutive days (10 in each group, counterbalanced: forest first vs urban first) | Urban walking 17 min walk | Semantic Differential (SD) method Profile of Mood State (POMS) Measurements taken at end of each walk | Increased SD scores of “comfortable”, “relaxed” and “natural” after waking in forest area compared with urban area. Reduced negative POMS scores of “tension–anxiety”, “depression”, “anger–hostility”, “fatigue” and “confusion”, with increased “vigour” after walking in forest area compared to urban area | Heart rate variability (HRV) and heart rate Measures collected at 1 min intervals and averaged over the 17 min course | Significantly higher parasympathetic activity during forest walking compared to urban walking. No significant difference in sympathetic nerve activity between groups. Significantly lower mean heart rate during forest walking compared to urban walking. Physiological measures were significantly related to the differences in air temperature and humidity between the forest and urban environments |
| Li et al. (2016) [53] | Single-sample cross-over cohort study | 19 male participants with high-normal blood pressure (HNBP) or hypertension Mean age 51.2 years (SD 8.8) | Forest walking Day trip All participants completed both interventions. Urban first | Urban walking Day trip | Profile of Mood State (POMS) Measurements taken before, during and after each intervention | Reduced POMS (D), (A), (F), (C) and increased (V) in forest walking but not city walking. City group also had increased (D) | Blood pressure and heart rate. Serum triglycerides, total cholesterol (Cho), low-density lipoprotein (LDL) Cho, high-density lipoprotein (HDL) Cho and remnant-like particles (RLP) Cho, serum adiponectin, blood glucose, serum insulin, serum dehydroepiandrosterone sulphate (DHEA-S), serum high-sensitivity C-reactive protein (hs-CRP). Urinary adrenaline, noradrenaline and dopamine (corrected for creatinine) Blood and urine collected in the morning before and after each day trip. Blood pressure and heart rate measured by an ambulatory monitor every 20 min | No significant difference in blood pressure between forest and urban day trips. Significant decrease in heart rate during forest walking compared to urban walking. No significant change in serum triglycerides, Cho, LDL Cho, HDL Cho, and RLP Cho, blood glucose, serum insulin, serum DHEA-S, or hs-CRP. Significant increase in serum adiponectin after forest but not urban day trips. Both forest and urban walking significantly reduced urinary noradrenaline. Non-significant decrease in urinary adrenaline after forest walking compared to urban walking. Significant decrease in urinary dopamine after forest walking compared to urban walking |
| Ochiai et al. (2015) [54] | Single-sample cohort | 9 male participants with high-normal blood pressure (HNBP) Mean age 56.0 years (SD 13.0) | Forest therapy 1-day programme involving walking, sitting and lying down | No comparison group | Semantic Differential (SD) method Profile of Mood State (POMS) combined POMS Total Mood Disturbance (TDM) Measurements before and after the intervention | Increased SD scores of “relaxed” and “natural” after forest therapy compared with baseline. Reduced negative POMS scores of “tension–anxiety”, “confusion” and “anger–hostility”, and TDM after forest therapy. | Blood pressure Urinary adrenaline (corrected for creatinine) Serum cortisol Blood pressure collected during intervention using portable device. Urine and blood samples collected in the afternoon before and after the intervention | Significant decrease in blood pressure after forest therapy. Significant decrease in urinary adrenaline and serum cortisol after forest therapy |
| Song et al. (2017) [55] | Two-sample, randomised cross-over cohort | 20 males with high-normal blood pressure or hypertension Mean age 58.0 years (SD 10.6) | Viewing forest landscape for 10 min while sitting (10 participants saw forest first, 10 saw urban first on 2 consecutive days) | Viewing urban landscape for 10 min while sitting | Modified semantic differential (SD) method completed after each viewing | Significantly increased scores of “comfortable”, “relaxed” and “natural” after viewing forest area compared to urban area | Heart rate variability (HRV) and heart rate collected at 1 min intervals and averaged across the 10 min period | Significantly increased high-frequency HRV during forest compared to urban viewing. No significant difference between high-frequency/low-frequency heart rate significantly lower during forest compared to urban viewing |
| Sung et al. (2012) [48] | Non-randomised controlled trial | 56 participants (22 female) with hypertension Mean age 64.5 years | 3-day CBT Forest Therapy programme including 2 recreational visits to forest sites (28 participants) Mean age 63 years (SD 11) 50% male | Provided with printed educational materials for hypertension management (28 participants) Mean age 66 years (SD 7) 28% male | QoL with 5 domains: General Health (GH), Physical Dimension (PD), Mental Dimension (MD), Social Dimension (SD and Hypertension-related Dimension (HTD). Measured at initial visit and at 8-week final visit | Forest group showed significantly increased total QoL scores after forest therapy. Increases in MD and HTD but not GH or SD. No significant change in control group | Blood pressure: measured at start and at end of 3-day program. Daily self-monitoring morning and evening from first until last day of study Salivary cortisol: collected at initial visit and 8-week final visit | Blood pressure: marginally significantly larger decrease in systolic blood pressure following forest therapy (at day 3). No change in diastolic blood pressure or either of self-measured at week 4 or 8. No significant longitudinal change in blood pressure in either group Salivary cortisol: significantly larger reduction following forest therapy and significant increase in control group |
| Wu et al. (2020) [49] | Two-sample randomised cohort | 31 participants (12 female) with hypertension Mean age 73.7 years | Forest walking (20 participants) 2 days at forest site with scheduled walking, rest and staying in a hotel | City walking (11 participants) 2 days at city site with scheduled walking, rest and staying in a hotel | Profile of Mood State (POMS) Measurements before and after the intervention | Reduced negative POMS scores of “tension–anxiety”, “depression”, “confusion” and “fatigue”, as well as increased “vigour” after forest bathing compared to city walking group. | Blood pressure, heart rate, oxygen saturation (SpO2%) and heart rate variability (HRV) Measurements taken in the morning before and after the intervention | Significant decrease in diastolic blood pressure, but not systolic blood pressure after forest bathing compared to controls Significant increase in SpO2% after forest bathing compared to controls No significant change in heart rate Significantly decreased in LF HRV and LF/HF HRV after forest bathing compared to controls. Significant increase in HF HRV after forest bathing compared to controls |
| Mao et al. (2012) [56] | Two-sample randomised cohort | 24 patients with essential hypertension (does not specify sex or age) | Forest walking (12 participants) 7 days at forest site with scheduled walking time, staying in a hotel | City walking (12 participants) 7 days at city site with scheduled walking time, staying in a hotel | Profile of Mood State (POMS) Measurements before and after the intervention. | Lower POMS scores of “depression”, “anger-hostility”, “fatigue” and “confusion”, with increased “vigour” in forest but not city group | Blood pressure and heart rate Cytokines: homocysteine (Hcy), constituents of the renin-angiotensin system (RAS) including renin, angiotensinogen (AGT), angiotensin II (Ang II), angiotensin II type 1 receptor (AT1), angiotensin II type 2 receptor (AT2) Cardiovascular disease-associated factors: serum interleukin-6 (IL-6), tumour necrosis factorα (TNF-α) and endothelin-1 (ET-1) Measurements taken in the morning before and after the intervention | Significant decrease in systolic and diastolic blood pressure after forest bathing compared to controls No significant change in heart rate Significant decrease in ET-1 and Hcy, RAS constituents including AGT, AT1, and AT2 after forest bathing compared to controls. Non-significant reduction in renin and Ang II after forest bathing compared to controls. Significant association between systolic blood pressure and Ang II, ET-1 and Hcy. Diastolic blood pressure was significantly associated with Ang II and ET-1. BP was poorly associated with the change in renin, AT1, and AGT Significant decrease in serum IL-6 after forest bathing compared to controlsNo significant change in TNF-α |
| Mao et al. (2017) [50] | Two-sample randomised cohort | 33 participants (14 female) with Chronic Heart Failure Mean age 71.8 years | Forest walking 23 participants 4-day trip | City walking 10 participants 4-day trip | Profile of Mood State (POMS) Measurements before and after the intervention. | Reduced negative POMS scores of “tension–anxiety”, “depression”, “anger–hostility” and “confusion” compared to baseline in forest group but not city group. | High-sensitive-reactive protein (hCRP) Bio-markers for heart failure: BNP and NT-ProBNP Cardiovascular disease-related factors: ET-1, constituents of the renin–angiotensin system (RAS) including renin, angiotensinogen (AGT), angiotensin II (Ang II), angiotensin II type 1 receptor (AT1), angiotensin II type 2 receptor (AT2) Pro-inflammatory cytokines: interleukin-6 (IL-6), tumour necrosis factorα (TNF-α) Oxidative indicators: activity for serum total SOD (T-SOD) and lipid peroxidation reflected by malondialdehyde (MDA) Measurements taken in the morning before and after the intervention | Significant decrease in BNP after forest bathing compared to baseline. No significant difference in controls. No significant difference in NT-ProBNP in either group. Significant decrease in ET-1 after forest bathing compared to controls. No change in ET-1 and the five RAS constituents in the city group compared to baseline. Significant increase in AT2 after forest bathing compared to baseline. No significant difference in controls Significant decrease in serum IL-6 after forest bathing compared to controls. No significant changes in TNF-α or high-sensitive-reactive protein (hCRP) Significant decrease in serum MDA and significant increase in T-SOD after forest bathing compared to controls. No significant difference in controls |
| Wichrowski et al. (2005) [51] | Two-sample cohort non-randomised | 107 participants (42 females) Inpatients on a phase I cardiac rehabilitation programme (does not specify age) | Horticultural therapy 59 participants single session | Patient education class 48 participants single session | Profile of Mood State (POMS) combined POMS Total Mood Disturbance (TDM) Measurements before and after the intervention | Reduced negative POMS scores of “tension”, “depression”, “anger”, “confusion” and “fatigue”, as well as increased “vigour” after horticultural therapy. TMD decreased after horticultural therapy. No changes following patient education class. | Heart rate before and after intervention | Significant decrease in heart rate following horticultural therapy, but no significant change following patient education class |
3.2. Psychological Outcomes
3.3. Physiological Outcomes
3.4. Qualitative Participant Experiences
3.5. Quality Appraisal
4. Discussion
4.1. Clinical Implications
4.2. Strengths and Limitations
4.3. Review Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- KingsFund. Long-Term Conditions and Multi-Morbidity|The King’s Fund. Available online: https://www.kingsfund.org.uk/projects/time-think-differently/trends-disease-and-disability-long-term-conditions-multi-morbidity (accessed on 31 January 2021).
- British Medical Association. Prevention before Cure. Securing the Long-Term Sustainability of the NHS; BMA: London, UK, 2018. [Google Scholar]
- Diabetes UK. Diabetes Prevalence 2019 | Diabetes UK. Available online: https://www.diabetes.org.uk/professionals/position-statements-reports/statistics/diabetes-prevalence-2019 (accessed on 2 March 2021).
- Kidney Care UK. Facts and Stats | Kidney Care UK. Available online: https://www.kidneycareuk.org/news-and-campaigns/facts-and-stats/ (accessed on 12 February 2021).
- Department of Health. Long Term Conditions Compendium of Information: Third Edition; Department of Health: London, UK, 2012. [Google Scholar]
- Gascon, M.; Triguero-Mas, M.; Martinez, D.; Dadvand, P.; Rojas-Rueda, D.; Plasencia, A.; Nieuwenhuijsen, M.J. Residential green spaces and mortality: A systematic review. Environ. Int. 2016, 86, 60–67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seo, S.; Choi, S.; Kim, K.; Kim, S.M.; Park, S.M. Association between urban green space and the risk of cardiovascular disease: A longitudinal study in seven Korean metropolitan areas. Environ. Int. 2019, 125, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Bauwelinck, M.; Casas, L.; Nawrot, T.S.; Nemery, B.; Trabelsi, S.; Thomas, I.; Aerts, R.; Lefebvre, W.; Vanpoucke, C.; Van Nieuwenhuyse, A.; et al. Residing in urban areas with higher green space is associated with lower mortality risk: A census-based cohort study with ten years of follow-up. Environ. Int. 2021, 148, 106365. [Google Scholar] [CrossRef] [PubMed]
- Paul, L.A.; Hystad, P.; Burnett, R.T.; Kwong, J.C.; Crouse, D.L.; van Donkelaar, A.; Tu, K.; Lavigne, E.; Copes, R.; Martin, R.V.; et al. Urban green space and the risks of dementia and stroke. Environ. Res. 2020, 186, 109520. [Google Scholar] [CrossRef] [PubMed]
- De la Fuente, F.; Saldías, M.A.; Cubillos, C.; Mery, G.; Carvajal, D.; Bowen, M.; Bertoglia, M.P. Green space exposure association with type 2 diabetes mellitus, physical activity, and obesity: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 97. [Google Scholar] [CrossRef] [PubMed]
- Twohig-Bennett, C.; Jones, A. The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environ. Res. 2018, 166, 628–637. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S. View through a window may influence recovery from surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef] [Green Version]
- Russell, R.; Guerry, A.D.; Balvanera, P.; Gould, R.K.; Basurto, X.; Chan, K.M.A.; Klain, S.; Levine, J.; Tam, J. Humans and nature: How knowing and experiencing nature affect well-being. Annu. Rev. Environ. Resour. 2013, 38, 473–502. [Google Scholar] [CrossRef]
- Kuo, M. How might contact with nature promote human health? Promising mechanisms and a possible central pathway. Front. Psychol. 2015, 6, 1093. [Google Scholar] [CrossRef]
- Wilson, E.O. Biophilia: The Human Bond with Other Species; Harvard University Press: Cambridge, MA, USA, 1984. [Google Scholar]
- Myers, O.G. The Biophilia Hypothesis. Environ. Ethics 1996, 18, 327–330. [Google Scholar] [CrossRef]
- Genter, C.; Roberts, A.; Richardson, J.; Sheaff, M. The contribution of allotment gardening to health and wellbeing: A systematic review of the literature. Br. J. Occup. Ther. 2015, 78, 593–605. [Google Scholar] [CrossRef]
- Cipriani, J.; Benz, A.; Holmgren, A.; Kinter, D.; McGarry, J.; Rufino, G. A Systematic Review of the Effects of Horticultural Therapy on Persons with Mental Health Conditions. Occup. Ther. Ment. Health 2017, 33, 47–69. [Google Scholar] [CrossRef]
- Wen, Y.; Yan, Q.; Pan, Y.; Gu, X.; Liu, Y. Medical empirical research on forest bathing (Shinrin-yoku): A systematic review. Environ. Health Prev. Med. 2019, 24, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Morimoto, K.; Nakadai, A.; Inagaki, H.; Katsumata, M.; Shimizu, T.; Hirata, Y.; Hirata, K.; Suzuki, H.; Miyazaki, Y.; et al. Forest bathing enhances human natural killer activity and expression of anti-cancer proteins. Int. J. Immunopathol. Pharmacol. 2007, 20, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Morimoto, K.; Kobayashi, M.; Inagaki, H.; Katsumata, M.; Hirata, Y.; Hirata, K.; Suzuki, H.; Li, Y.J.; Wakayama, Y.; et al. Visiting a forest, but not a city, increases human natural killer activity and expression of anti-cancer proteins. Int. J. Immunopathol. Pharmacol. 2008, 21, 117–127. [Google Scholar] [CrossRef] [PubMed]
- Tesler, R.; Endevelt, R.; Plaut, P. Urban Forest Health Intervention Program to promote physical activity, healthy eating, self-efficacy and life satisfaction: Impact on Israeli at-risk youth. Health Promot. Int. 2021, daab145. [Google Scholar] [CrossRef] [PubMed]
- Kabisch, N.; Püffel, C.; Masztalerz, O.; Hemmerling, J.; Kraemer, R. Physiological and psychological effects of visits to different urban green and street environments in older people: A field experiment in a dense inner-city area. Landsc. Urban Plan. 2021, 207, 103998. [Google Scholar] [CrossRef]
- Bailey, A.W.; Allen, G.; Herndon, J.; Demastus, C. Cognitive benefits of walking in natural versus built environments. World Leis. J. 2018, 60, 293–305. [Google Scholar] [CrossRef]
- Berman, M.G.; Kross, E.; Krpan, K.M.; Askren, M.K.; Burson, A.; Deldin, P.J.; Kaplan, S.; Sherdell, L.; Gotlib, I.H.; Jonides, J. Interacting with nature improves cognition and affect for individuals with depression. J. Affect. Disord. 2012, 140, 300–305. [Google Scholar] [CrossRef] [Green Version]
- Berget, B.; Braastad, B.O. Theoretical framework for animal-assisted interventions—Implications for practice. Ther. Communities 2008, 29, 323–337. [Google Scholar]
- Beetz, A.; Uvnäs-Moberg, K.; Julius, H.; Kotrschal, K. Psychosocial and psychophysiological effects of human-animal interactions: The possible role of oxytocin. Front. Psychol. 2012, 3, 234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matchock, R.L. Pet ownership and physical health. Curr. Opin. Psychiatry 2015, 28, 386–392. [Google Scholar] [CrossRef] [PubMed]
- Krause-Parello, C.A.; Gulick, E.E.; Basin, B. Loneliness, depression, and physical activity in older adults: The therapeutic role of human–animal interactions. Anthrozoos 2019, 32, 239–254. [Google Scholar] [CrossRef]
- McCune, S.; Kruger, K.A.; Griffin, J.A.; Esposito, L.; Freund, L.S.; Hurley, K.J.; Bures, R. Evolution of research into the mutual benefits of human-animal interaction. Anim. Front. 2014, 4, 49–58. [Google Scholar] [CrossRef] [Green Version]
- Sung, Y.-H.; Kim, C.-J.; Yu, B.-K.; Kim, K.-M. A hippotherapy simulator is effective to shift weight bearing toward the affected side during gait in patients with stroke. NeuroRehabilitation 2013, 33, 407–412. [Google Scholar] [CrossRef]
- Kim, Y.-N.; Lee, D.-K. Effects of horse-riding exercise on balance, gait, and activities of daily living in stroke patients. J. Phys. Ther. Sci. 2015, 27, 607–609. [Google Scholar] [CrossRef] [Green Version]
- Beinotti, F.; Correia, N.; Christofoletti, G.; Borges, G. Use of hippotherapy in gait training for hemiparetic post-stroke. Arq. Neuropsiquiatr. 2010, 68, 908–913. [Google Scholar] [CrossRef] [Green Version]
- Beinotti, F.; Christofoletti, G.; Correia, N.; Borges, G. Effects of horseback riding therapy on quality of life in patients post stroke. Top. Stroke Rehabil. 2013, 20, 226–232. [Google Scholar] [CrossRef]
- Håkanson, M.; Möller, M.; Lindström, I.; Mattsson, B. The horse as the healer-A study of riding in patients with back pain. J. Bodyw. Mov. Ther. 2009, 13, 43–52. [Google Scholar] [CrossRef]
- Lundquist Wanneberg, P. Disability, Riding, and Identity: A Qualitative Study on the Influence of Riding on the Identity Construction of People with Disabilities. Int. J. Disabil. Dev. Educ. 2014, 61, 67–79. [Google Scholar] [CrossRef] [Green Version]
- Schardt, C.; Adams, M.B.; Owens, T.; Keitz, S.; Fontelo, P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007, 7, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brooks, S.K.; Dunn, R.; Amlôt, R.; Greenberg, N.; James Rubin, G. Social and occupational factors associated with psychological distress and disorder among disaster responders: A systematic review. BMC Psychol. 2016, 4, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- BestBETs.org. BestBETs—BETs CA Worksheets. Available online: https://bestbets.org/links/BET-CA-worksheets.php (accessed on 22 February 2021).
- Marshall, C.; Sutton, A. Systematic Review Toolbox. Value Health 2016, 19, A398. [Google Scholar] [CrossRef]
- Booth, A.; Sutton, A.; Papaioannou, D. Systematic Approaches to a Successful Literature Review, 2nd ed.; SAGE: London, UK, 2016; ISBN 9780857021359. [Google Scholar]
- Sandelowski, M.; Barroso, J. Reading Qualitative Studies. Int. J. Qual. Methods 2002, 1, 74–108. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Throner, V.; Kirschneck, M.; Immich, G.; Frisch, D.; Schuh, A. The Psychological and Physical Effects of Forests on Human Health: A Systematic Review of Systematic Reviews and Meta-Analyses. Int. J. Environ. Res. Public Health 2021, 18, 1770. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Chun, M.H.; Chang, M.C.; Lee, S.J. The effects of forest therapy on depression and anxiety in patients with chronic stroke. Int. J. Neurosci. 2017, 127, 199–203. [Google Scholar] [CrossRef]
- Pohl, P.; Carlsson, G.; Käll, L.B.; Nilsson, M.; Blomstrand, C. A qualitative exploration of post-acute stroke participants’ experiences of a multimodal intervention incorporating horseback riding. PLoS ONE 2018, 13, e0203933. [Google Scholar] [CrossRef] [Green Version]
- Jia, B.B.; Yang, Z.X.; Mao, G.X.; Lyu, Y.D.; Wen, X.L.; Xu, W.H.; Lyu, X.L.; Cao, Y.B.; Wang, G.F. Health Effect of Forest Bathing Trip on Elderly Patients with Chronic Obstructive Pulmonary Disease. Biomed. Environ. Sci. 2016, 29, 212–218. [Google Scholar] [CrossRef]
- Sung, J.; Woo, J.M.; Kim, W.; Lim, S.K.; Chung, E.J. The effect of cognitive behavior therapy-based “forest therapy” program on blood pressure, salivary cortisol level, and quality of life in elderly hypertensive patients. Clin. Exp. Hypertens. 2012, 34, 1–7. [Google Scholar] [CrossRef]
- Wu, Q.; Ye, B.; Lv, X.; Mao, G.; Wang, S.; Chen, Z.; Wang, G. Adjunctive therapeutic effects of cinnamomum camphora forest environment on elderly patients with hypertension. Int. J. Gerontol. 2020, 14, 327–331. [Google Scholar] [CrossRef]
- Mao, G.; Cao, Y.; Wang, B.; Wang, S.; Chen, Z.; Wang, J.; Xing, W.; Ren, X.; Lv, X.; Dong, J.; et al. The Salutary Influence of Forest Bathing on Elderly Patients with Chronic Heart Failure. Int. J. Environ. Res. Public Health 2017, 14, 368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wichrowski, M.; Whiteson, J.; Haas, F.; Mola, A.; Rey, M.J. Effects of horticultural therapy on mood and heart rate in patients participating in an inpatient cardiopulmonary rehabilitation program. J. Cardiopulm. Rehabil. 2005, 25, 270–274. [Google Scholar] [CrossRef] [PubMed]
- Song, C.; Ikei, H.; Kobayashi, M.; Miura, T.; Taue, M.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; Miyazaki, Y. Effect of forest walking on autonomic nervous system activity in middle-aged hypertensive individuals: A pilot study. Int. J. Environ. Res. Public Health 2015, 12, 2687–2699. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Kobayashi, M.; Kumeda, S.; Ochiai, T.; Miura, T.; Kagawa, T.; Imai, M.; Wang, Z.; Otsuka, T.; Kawada, T. Effects of Forest Bathing on Cardiovascular and Metabolic Parameters in Middle-Aged Males. Evid.-Based Complement. Altern. Med. 2016, 2016, 2587381. [Google Scholar] [CrossRef]
- Ochiai, H.; Ikei, H.; Song, C.; Kobayashi, M.; Takamatsu, A.; Miura, T.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; et al. Physiological and psychological effects of forest therapy on middle-aged males with high-normal blood pressure. Int. J. Environ. Res. Public Health 2015, 12, 2532–2542. [Google Scholar] [CrossRef] [Green Version]
- Song, C.; Ikei, H.; Kobayashi, M.; Miura, T.; Li, Q.; Kagawa, T.; Kumeda, S.; Imai, M.; Miyazaki, Y. Effects of viewing forest landscape on middle-aged hypertensive men. Urban For. Urban Green. 2017, 21, 247–252. [Google Scholar] [CrossRef]
- Mao, G.-X.; Cao, Y.-B.; Lan, X.-G.; He, Z.-H.; Chen, Z.-M.; Wang, Y.-Z.; Hu, X.-L.; Lv, Y.-D.; Wang, G.-F.; Yan, J. Therapeutic effect of forest bathing on human hypertension in the elderly. J. Cardiol. 2012, 60, 495–502. [Google Scholar] [CrossRef] [Green Version]
- Bunketorp-Käll, L.; Lundgren-Nilsson, Å.; Blomstrand, C.; Pekna, M.; Pekny, M.; Nilsson, M. The effects of a rhythm and music-based therapy program and therapeutic riding in late recovery phase following stroke: A study protocol for a three-armed randomized controlled trial. BMC Neurol. 2012, 12, 141. [Google Scholar] [CrossRef] [Green Version]
- Bunketorp-Käll, L.; Pekna, M.; Pekny, M.; Blomstrand, C.; Nilsson, M. Effects of horse-riding therapy and rhythm and music-based therapy on functional mobility in late phase after stroke. NeuroRehabilitation 2019, 45, 483–492. [Google Scholar] [CrossRef] [Green Version]
- Pollock, V.; Cho, D.W.; Reker, D.; Volavka, J. Profile of Mood States: The Factors and Their Physiological Correlates. J. Nerv. Ment. Dis. 1979, 167, 612–614. [Google Scholar] [CrossRef] [PubMed]
- McHorney, C.A.; Ware, J.E.; Raczek, A.E. The MOS 36-item short-form health survey (Sf-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med. Care 1993, 31, 247–263. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Osgood, C.E.; Suci, G.J.; Tannenbaum, P. The Measurement of Meaning; University of Illinois Press: Urbana, IL, USA, 1957. [Google Scholar]
- Beck, A.T.; Steer, R.A.; Ball, R.; Ranieri, W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J. Personal. Assess. 1996, 67, 588–597. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. The Assessment of Anxiety States By Rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Barnes, L.L.B.; Harp, D.; Jung, W.S. Reliability Generalization of Scores on the Spielberger State-Trait Anxiety Inventory. Educ. Psychol. Meas. 2002, 62, 603–618. [Google Scholar] [CrossRef]
- Kim, K.Y.; Chun, B.Y.; Kam, S.; Lee, S.W.; Park, K.S.; Chae, S.C. Development of measurement scale for the quality of life in hypertensive patients. J. Prev. Med. Public Health 2005, 38, 61–70. [Google Scholar]
- Wang, Y.X.; Song, L.; Xing, A.J.; Gao, M.; Zhao, H.Y.; Li, C.H.; Zhao, H.L.; Chen, S.H.; Lu, C.Z.; Wu, S.L. Predictive Value of Cumulative Blood Pressure for All-Cause Mortality and Cardiovascular Events. Sci. Rep. 2017, 7, 41969. [Google Scholar] [CrossRef] [Green Version]
- Pugh, D.; Gallacher, P.J.; Dhaun, N. Management of Hypertension in Chronic Kidney Disease. Drugs 2019, 79, 365–379. [Google Scholar] [CrossRef] [Green Version]
- Howard, G.; Banach, M.; Cushman, M.; Goff, D.C.; Howard, V.J.; Lackland, D.T.; McVay, J.; Meschia, J.F.; Muntner, P.; Oparil, S.; et al. Is Blood Pressure Control for Stroke Prevention the Correct Goal?: The Lost Opportunity of Preventing Hypertension. Stroke 2015, 46, 1595–1600. [Google Scholar] [CrossRef] [Green Version]
- Han, M.; Chen, Q.; Liu, L.; Li, Q.; Ren, Y.; Zhao, Y.; Liu, D.; Zhang, D.; Liu, F.; Chen, X.; et al. Stage 1 hypertension by the 2017 American College of Cardiology/American Heart Association hypertension guidelines and risk of cardiovascular disease events: Systematic review, meta-analysis, and estimation of population etiologic fraction of prospective cohort studies. J. Hypertens. 2020, 38, 573–578. [Google Scholar] [CrossRef]
- Sunkara, N.; Ahsan, H.C. Hypertension in diabetes and the risk of cardiovascular disease. Cardiovasc. Endocrinol. 2017, 6, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Iwane, M.; Arita, M.; Tomimoto, S.; Satani, O.; Matsumoto, M.; Miyashita, K.; Nishio, I. Walking 10,000 steps/day or more reduces blood pressure and sympathetic nerve activity in mild essential hypertension. Hypertens. Res. 2000, 23, 573–580. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayashino, Y.; Jackson, J.L.; Fukumori, N.; Nakamura, F.; Fukuhara, S. Effects of supervised exercise on lipid profiles and blood pressure control in people with type 2 diabetes mellitus: A meta-analysis of randomized controlled trials. Diabetes Res. Clin. Pract. 2012, 98, 349–360. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.T.; Thompson, P.D. Walking versus running for hypertension, cholesterol, and diabetes mellitus risk reduction. Arterioscler. Thromb. Vasc. Biol. 2013, 33, 1085–1091. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.Z.A.; Karam, J.A.; Zeb, A.; Ullah, R.; Shah, A.; Haq, I.U.; Ali, I.; Darain, H.; Chen, H. Movement is Improvement: The Therapeutic Effects of Exercise and General Physical Activity on Glycemic Control in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Diabetes Ther. 2021, 12, 707–732. [Google Scholar] [CrossRef]
- Pedersen, B.K.; Saltin, B. Exercise as medicine—Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 2015, 25, 1–72. [Google Scholar] [CrossRef] [Green Version]
- Delaney, J.P.A.; Leong, K.S.; Watkins, A.; Brodie, D. The short-term effects of myofascial trigger point massage therapy on cardiac autonomic tone in healthy subjects. J. Adv. Nurs. 2002, 37, 364–371. [Google Scholar] [CrossRef]
- Park, B.J.; Tsunetsugu, Y.; Kasetani, T.; Kagawa, T.; Miyazaki, Y. The physiological effects of Shinrin-yoku (taking in the forest atmosphere or forest bathing): Evidence from field experiments in 24 forests across Japan. Environ. Health Prev. Med. 2010, 15, 18–26. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Tsunetsugu, Y.; Takayama, N.; Park, B.J.; Li, Q.; Song, C.; Komatsu, M.; Ikei, H.; Tyrväinen, L.; Kagawa, T.; et al. Influence of forest therapy on cardiovascular relaxation in young adults. Evid.-Based Complement. Altern. Med. 2014, 2014, 834360. [Google Scholar] [CrossRef]
- Dickerson, S.S.; Kemeny, M.E. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol. Bull. 2004, 130, 355–391. [Google Scholar] [CrossRef] [Green Version]
- Imperato, A.; Puglisi-Allegra, S.; Casolini, P.; Zocchi, A.; Angelucci, L. Stress-induced enhancement of dopamine and acetylcholine release in limbic structures: Role of corticosterone. Eur. J. Pharmacol. 1989, 165, 337–338. [Google Scholar] [CrossRef]
- Haraoui, B.; Liu, P.P.; Papp, K.A. Managing cardiovascular risk in patients with chronic inflammatory diseases. Clin. Rheumatol. 2012, 31, 585–594. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, L.; Urbanowicz, R.A.; Corne, J.; Lamb, J.R. Killer cells in chronic obstructive pulmonary disease. Clin. Sci. 2008, 114, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.A.; Kivimäki, M.; Bullmore, E.T.; Steptoe, A.; Carvalho, L.A.; Vértes, P.E.; Cardinal, R.; Richardson, S.; Leday, G.; Freeman, T.; et al. Repeated exposure to systemic inflammation and risk of new depressive symptoms among older adults. Transl. Psychiatry 2017, 7, e1208. [Google Scholar] [CrossRef] [PubMed]
- McEwan, K.; Giles, D.; Clarke, F.J.; Kotera, Y.; Evans, G.; Terebenina, O.; Minou, L.; Teeling, C.; Basran, J.; Wood, W.; et al. A pragmatic controlled trial of forest bathing compared with compassionate mind training in the UK: Impacts on self-reported wellbeing and heart rate variability. Sustainability 2021, 13, 1380. [Google Scholar] [CrossRef]
- Rainham, D.G.C.; Smoyer-Tomic, K.E. The role of air pollution in the relationship between a heat stress index and human mortality in Toronto. Environ. Res. 2003, 93, 9–19. [Google Scholar] [CrossRef]
- Woodhouse, P.R.; Khaw, K.; Plummer, M. Seasonal variation of blood pressure and its relationship to ambient temperature in an elderly population. J. Hypertens. 1993, 11, 1267–1274. [Google Scholar] [CrossRef]
- Shanahan, D.; Astell–Burt, T.; Barber, E.; Brymer, E.; Cox, D.; Dean, J.; Depledge, M.; Fuller, R.; Hartig, T.; Irvine, K.; et al. Nature–Based Interventions for Improving Health and Wellbeing: The Purpose, the People and the Outcomes. Sports 2019, 7, 141. [Google Scholar] [CrossRef] [Green Version]
- Ellingsen-Dalskau, L.H.; Morken, M.; Berget, B.; Pedersen, I. Autonomy support and need satisfaction in prevocational programs on care farms: The self-determination theory perspective. Work 2016, 53, 73–85. [Google Scholar] [CrossRef]
- Fortier, M.S.; Duda, J.L.; Guerin, E.; Teixeira, P.J. Promoting physical activity: Development and testing of self-determination theory-based interventions. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 20. [Google Scholar] [CrossRef] [Green Version]
- Moorthi, R.N.; Latham-Mintus, K. Social isolation in chronic kidney disease and the role of mobility limitation. Clin. Kidney J. 2019, 12, 602–610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chilcot, J.; Guirguis, A.; Friedli, K.; Almond, M.; Day, C.; Da Silva-Gane, M.; Davenport, A.; Fineberg, N.A.; Spencer, B.; Wellsted, D.; et al. Depression symptoms in haemodialysis patients predict all-cause mortality but not kidney transplantation: A cause-specific outcome analysis. Ann. Behav. Med. 2018, 52, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Litchman, M.L.; Oser, T.K.; Hodgson, L.; Heyman, M.; Walker, H.R.; Deroze, P.; Rinker, J.; Warshaw, H. In-Person and Technology-Mediated Peer Support in Diabetes Care: A Systematic Review of Reviews and Gap Analysis. Diabetes Educ. 2020, 46, 230–241. [Google Scholar] [CrossRef] [PubMed]
- Ghahramani, N.; Chinchilli, V.M.; Kraschnewski, J.L.; Lengerich, E.J.; Sciamanna, C.N. Effect of Peer Mentoring on Quality of Life among CKD Patients: Randomized Controlled Trial. Kidney Dis. 2021, 7, 323–334. [Google Scholar] [CrossRef]
- Basinger, E.D.; Farris, M.; Delaney, A.L. Investigating the Experience of Diabetes Stigma in Online Forums. South. Commun. J. 2019, 85, 43–57. [Google Scholar] [CrossRef]
- Jerpseth, H.; Knutsen, I.R.; Jensen, K.T.; Halvorsen, K. Mirror of shame: Patients experiences of late-stage COPD. A qualitative study. J. Clin. Nurs. 2021, 30, 2854–2862. [Google Scholar] [CrossRef]
- Kato, A.; Fujimaki, Y.; Fujimori, S.; Izumida, Y.; Suzuki, R.; Ueki, K.; Kadowaki, T.; Hashimoto, H. A qualitative study on the impact of internalized stigma on type 2 diabetes self-management. Patient Educ. Couns. 2016, 99, 1233–1239. [Google Scholar] [CrossRef]
- Brown, B. Shame resilience theory: A grounded theory study on women and shame. Fam. Soc. 2006, 87, 43–52. [Google Scholar] [CrossRef]
- Dayal, H.; Weaver, K.; Domene, J.F. From shame to shame resilience: Narratives of counselor trainees with eating issues. Qual. Health Res. 2015, 25, 153–167. [Google Scholar] [CrossRef]
- Gredig, D.; Bartelsen-Raemy, A. Diabetes-related stigma affects the quality of life of people living with diabetes mellitus in Switzerland: Implications for healthcare providers. Health Soc. Care Community 2017, 25, 1620–1633. [Google Scholar] [CrossRef]
- Woo, S.; Zhou, W.; Larson, J.L. Stigma experiences in people with chronic obstructive pulmonary disease: An integrative review. Int. J. Chronic Obstr. Pulm. Dis. 2021, 16, 1647–1659. [Google Scholar] [CrossRef] [PubMed]
- Cruwys, T.; Wakefield, J.R.H.; Sani, F.; Dingle, G.A.; Jetten, J. Social Isolation Predicts Frequent Attendance in Primary Care. Ann. Behav. Med. 2018, 52, 817–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bickerdike, L.; Booth, A.; Wilson, P.M.; Farley, K.; Wright, K. Social prescribing: Less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017, 7, e013384. [Google Scholar] [CrossRef]
- NHS. NHS England » Social Prescribing. Available online: https://www.england.nhs.uk/personalisedcare/social-prescribing/green-social-prescribing/ (accessed on 16 January 2022).
- Elston, J.; Gradinger, F.; Asthana, S.; Lilley-Woolnough, C.; Wroe, S.; Harman, H.; Byng, R. Does a social prescribing ‘holistic’ link-worker for older people with complex, multimorbidity improve well-being and frailty and reduce health and social care use and costs? A 12-month before-and-after evaluation. Prim. Health Care Res. Dev. 2019, 20, e135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lynch, M.; Jones, C. Social prescribing for frequent attenders: Findings from an innovative pilot intervention. Lancet 2019, 394, S69. [Google Scholar] [CrossRef] [Green Version]
- Bloomfield, D. What makes nature-based interventions for mental health successful? BJPsych. Int. 2017, 14, 82–85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoen, V.; Caputo, S.; Blythe, C. Valuing physical and social output: A rapid assessment of a London community garden. Sustainability 2020, 12, 5452. [Google Scholar] [CrossRef]
- Carrier, J.; Newbury, G. Managing long-term conditions in primary and community care. Br. J. Community Nurs. 2016, 21, 504–508. [Google Scholar] [CrossRef]
- Naylor, C.; Parsonage, M.; Mcdaid, D.; Knapp, M.; Fossey, M.; Galea, A. Long-Term Condition and Mental Health: The Cost of Co-Morbidities; King’s Fund: London, UK, 2012; pp. 1–32. [Google Scholar]
- Whicher, C.A.; O’Neill, S.; Holt, R.I.G. Diabetes in the UK: 2019. Diabet. Med. 2020, 37, 242–247. [Google Scholar] [CrossRef]
- Hurst, J.R.; Skolnik, N.; Hansen, G.J.; Anzueto, A.; Donaldson, G.C.; Dransfield, M.T.; Varghese, P. Understanding the impact of chronic obstructive pulmonary disease exacerbations on patient health and quality of life. Eur. J. Intern. Med. 2020, 73, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Song, F.; Parekh, S.; Hooper, L.; Loke, Y.K.; Ryder, J.; Sutton, A.J.; Hing, C.; Kwok, C.S.; Pang, C.; Harvey, I. Health Technology Assessment NIHR HTA programme www.hta.ac.uk Dissemination and publication of research findings: An updated review of related biases. Health Technol. Assess. 2010, 14. [Google Scholar] [CrossRef] [PubMed]
- Weldegiorgis, M.; Smith, M.; Herrington, W.G.; Bankhead, C.; Woodward, M. Socioeconomic disadvantage and the risk of advanced chronic kidney disease: Results from a cohort study with 1.4 million participants. Nephrol. Dial. Transplant. 2020, 35, 1562–1570. [Google Scholar] [CrossRef] [PubMed]
- Geronimus, A.T.; Hicken, M.; Keene, D.; Bound, J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am. J. Public Health 2006, 96, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Corazon, S.S.; Gramkow, M.C.; Poulsen, D.V.; Linlygum, V.; Zhang, G.; Stigsdotter, U.K. I would really like to visit the forest, but it is just too difficult: A qualitative study on mobility disability and green spaces. Scand. J. Disabil. Res. 2019, 21, 1–13. [Google Scholar] [CrossRef]
- Mayer, F.S.; Frantz, C.M.P. The connectedness to nature scale: A measure of individuals’ feeling in community with nature. J. Environ. Psychol. 2004, 24, 503–515. [Google Scholar] [CrossRef] [Green Version]
- Wilkie, S.; Davinson, N. Prevalence and effectiveness of nature-based interventions to impact adult health-related behaviours and outcomes: A scoping review. Landsc. Urban Plan. 2021, 214, 104166. [Google Scholar] [CrossRef]
- Mattila, O.; Korhonen, A.; Pöyry, E.; Hauru, K.; Holopainen, J.; Parvinen, P. Restoration in a virtual reality forest environment. Comput. Human Behav. 2020, 107, 106295. [Google Scholar] [CrossRef]
- Yu, C.P.; Lee, H.Y.; Luo, X.Y. The effect of virtual reality forest and urban environments on physiological and psychological responses. Urban For. Urban Green. 2018, 35, 106–114. [Google Scholar] [CrossRef]
- Salonen, K.; Hyvönen, K.; Paakkolanvaara, J.-V.; Korpela, K. Flow With Nature Treatment for Depression: Participants’ Experiences. Front. Psychol. 2022, 12, 768372. [Google Scholar] [CrossRef]
| PICO | |
|---|---|
| P—Population | People with long-term physical health conditions limited to cardiovascular disease, stroke, lung and liver disease, type II diabetes and chronic kidney disease |
| I—Intervention | Nature-, green- or outdoor animal-based interventions |
| C—Comparison | Treatment as usual, urban environments or no comparison |
| O—Outcome | Evaluation of effectiveness, as measured by improvements in psychological wellbeing and/or quality of life (QoL) |
| Search Terms | |
|---|---|
| Nature-based interventions | ((garden* OR green OR horticultur* OR “nature-based” OR “nature based”) N2 (therap* OR intervention* OR proximity)) OR ((healing OR restorative OR wander) N2 garden) OR “green prescri*” OR “social prescri*” OR “nature prescri*” OR “nature play” OR “park prescri*” OR “garden prescri*” OR “green space*” OR greenspace* OR “green exercise” OR “green infrastructure” OR “community garden*” OR “community allotment*” OR allotment* OR “outdoor exercise” OR “blue space*” OR “blue gym*” OR “green gym*” OR “park prescri*” OR “eco therapy” OR “eco-therapy” OR “wilderness therapy” OR “wilderness-therapy” OR “care-farming” OR “care farming” OR “farm therapy” OR “farm-therapy” OR “forest bathing” OR “forest-bathing” OR “environmental volunteering” OR “wild play” OR “nature play” OR “animal assisted therap*” or “animal-assisted therap*” OR “animal therap*” OR “pet therap*” or “pet-assisted therapy” OR “equine assisted therap*” OR “equine-assisted therap*” OR “canine assisted therap*” OR “canine-assisted therap*” |
| Long-term conditions | Cardiovascular or “cardiovascular disease” or Hypertension or “high blood pressure” or “Coronary Heart Disease” or “heart disease” or CHD or “Coronary Disease” or “vascular disease” or “Heart failure” or “Pulmonary Heart Disease” OR “Pulmonary disease” or “Respiratory disease” or Asthma or “Chronic Obstructive Pulmonary Disease” or COPD OR “Liver disease” or “Chronic liver disease” or “liver cirrhosis” or “Fatty Liver” or Hepatitis or “hepatic disease” OR “type II diabetes” or “type two diabetes” or “type 2 diabetes” or Diabetes or T2DM or “diabetes mellitus” OR “Kidney disease” or “Chronic kidney disease” or CKD or “renal insufficiency” or “chronic renal insufficiency” or “renal disease” or “chronic renal disease” or “kidney failure” or “renal failure” or AKI or “acute kidney injury” |
| Negative | Positive | |||||
|---|---|---|---|---|---|---|
| Author (Date) [Ref] | Tension-Anxiety | Depression | Anger-Hostility | Fatigue | Confusion | Vigour |
| Jia et al. (2016) [47] | + | + | + | |||
| Song et al. (2015) [52] | + | + | + | + | + | + |
| Li et al. (2016) [53] | + | + | + | + | + | |
| Ochiai et al. (2015) [54] | + | + | + | |||
| Wu et al. (2020) [49] | + | + | + | + | + | |
| Mao et al. (2012) [56] | + | + | + | + | + | |
| Mao et al. (2017) [50] | + | + | + | + | ||
| Wichrowski et al. (2005) [51] | + | + | + | + | + | + |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taylor, E.M.; Robertson, N.; Lightfoot, C.J.; Smith, A.C.; Jones, C.R. Nature-Based Interventions for Psychological Wellbeing in Long-Term Conditions: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 3214. https://doi.org/10.3390/ijerph19063214
Taylor EM, Robertson N, Lightfoot CJ, Smith AC, Jones CR. Nature-Based Interventions for Psychological Wellbeing in Long-Term Conditions: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(6):3214. https://doi.org/10.3390/ijerph19063214
Chicago/Turabian StyleTaylor, Eleanor M., Noelle Robertson, Courtney J. Lightfoot, Alice C. Smith, and Ceri R. Jones. 2022. "Nature-Based Interventions for Psychological Wellbeing in Long-Term Conditions: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 6: 3214. https://doi.org/10.3390/ijerph19063214
APA StyleTaylor, E. M., Robertson, N., Lightfoot, C. J., Smith, A. C., & Jones, C. R. (2022). Nature-Based Interventions for Psychological Wellbeing in Long-Term Conditions: A Systematic Review. International Journal of Environmental Research and Public Health, 19(6), 3214. https://doi.org/10.3390/ijerph19063214






