Impact of Pesticides on Human Health in the Last Six Years in Brazil
Abstract
1. Introduction
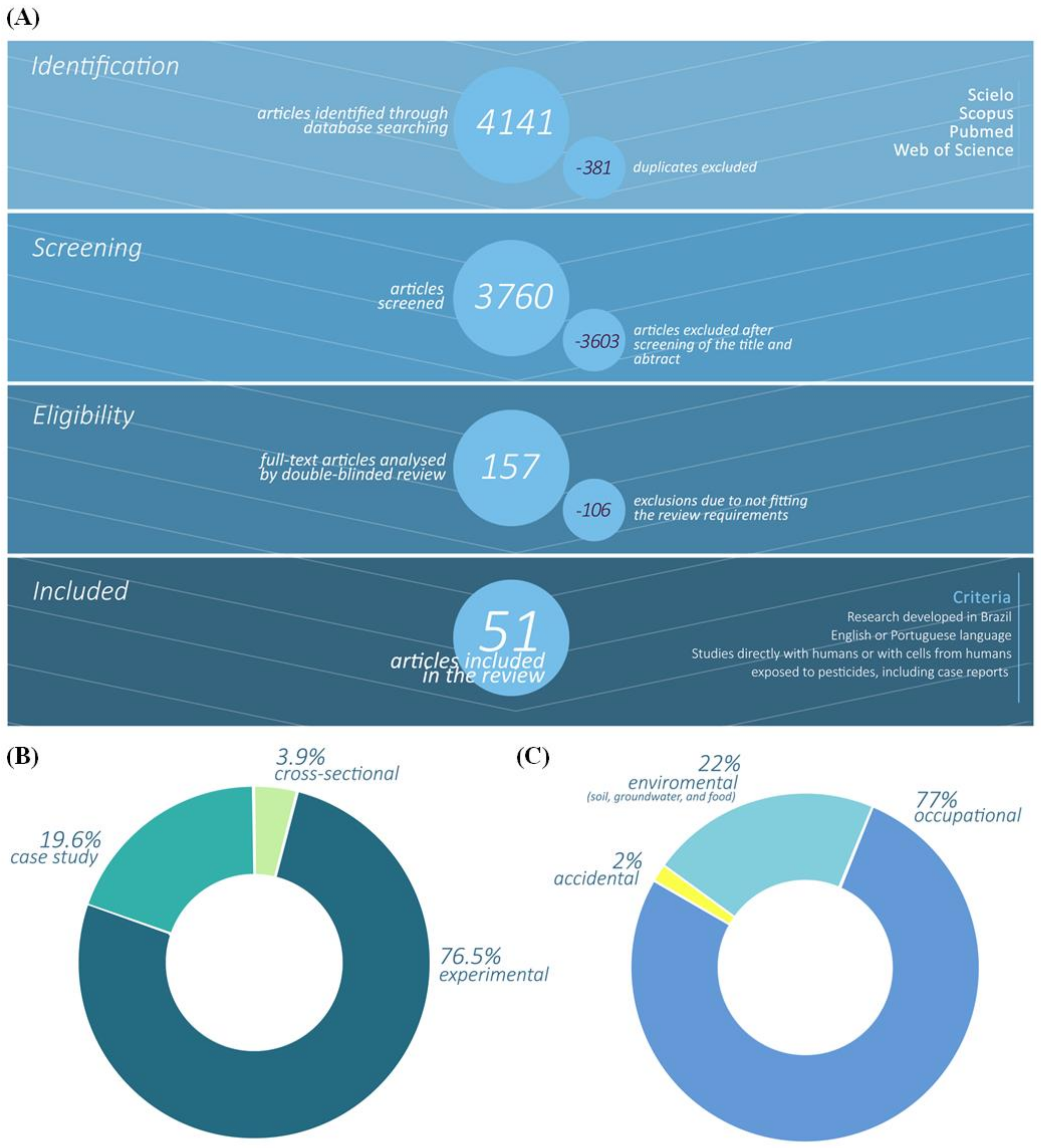
2. Methods
2.1. Data Sources
2.2. Studies Selection
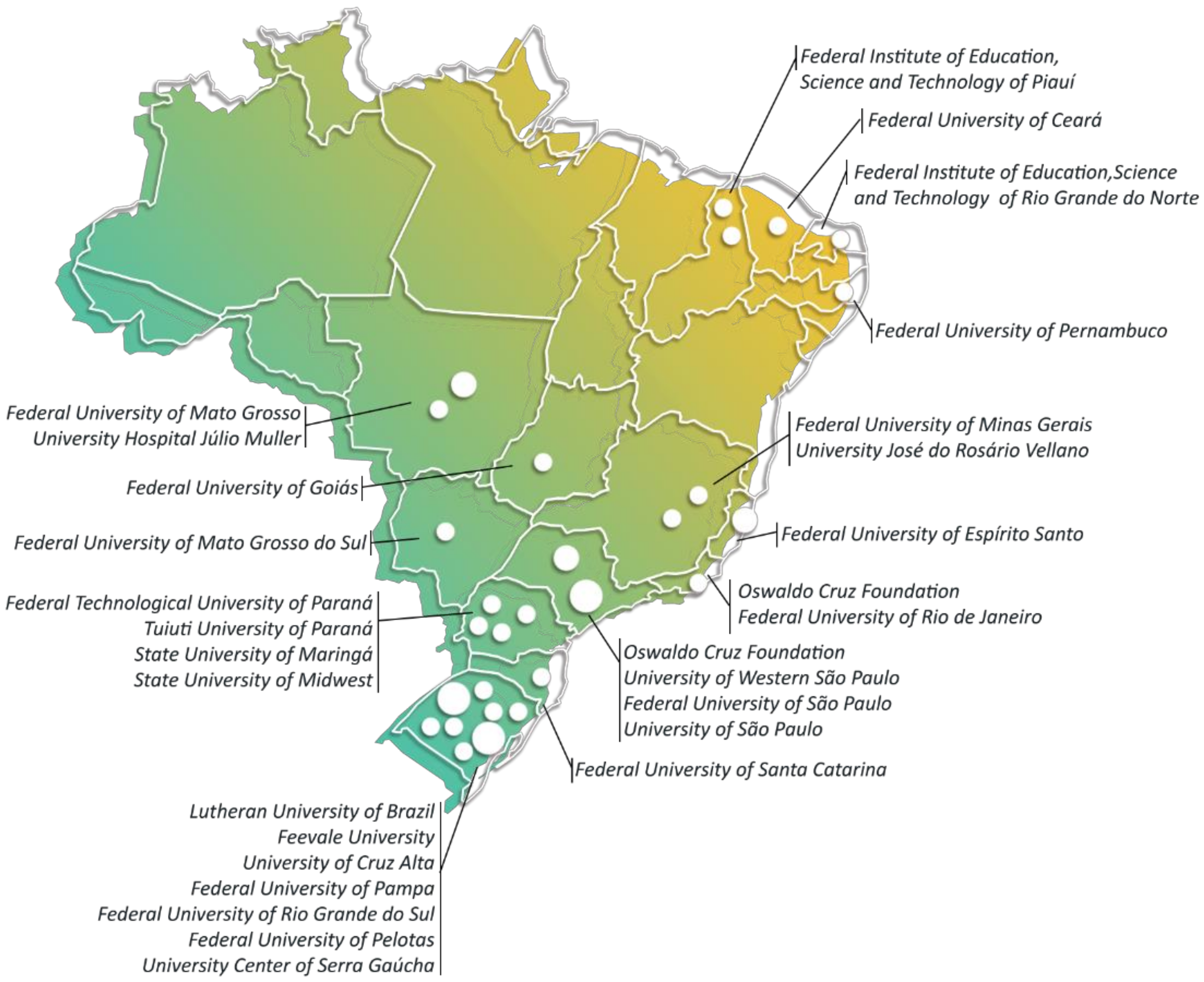
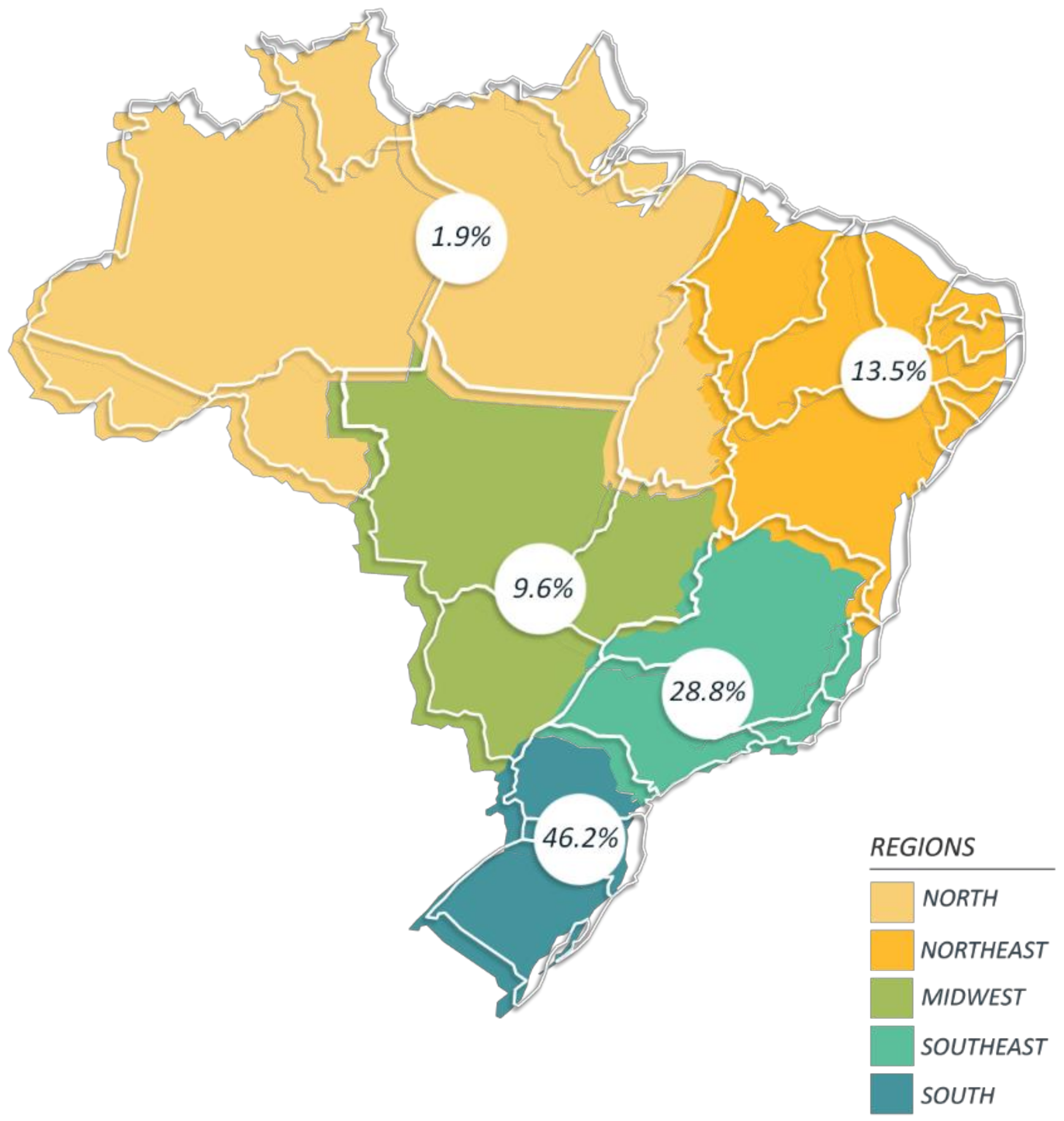
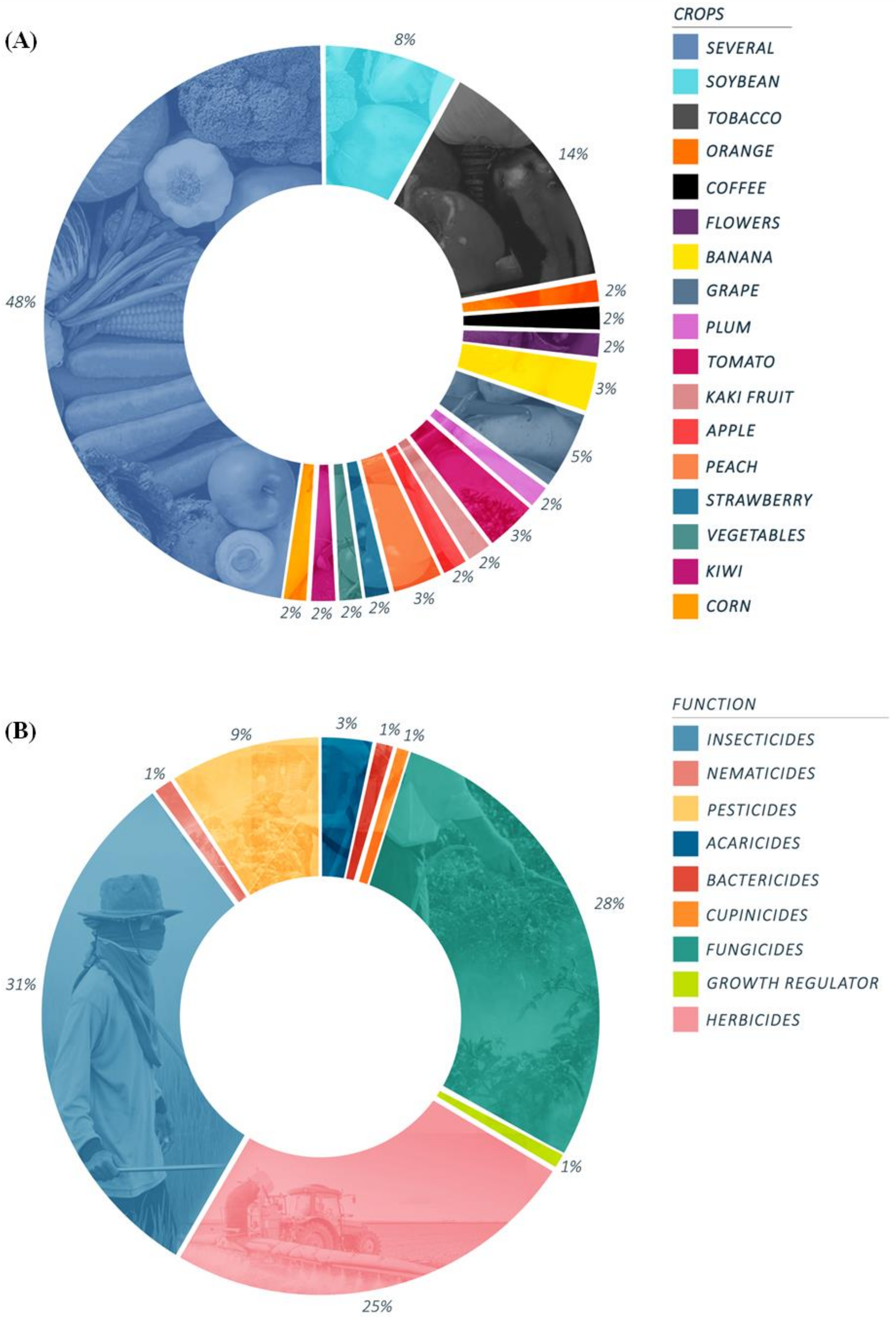
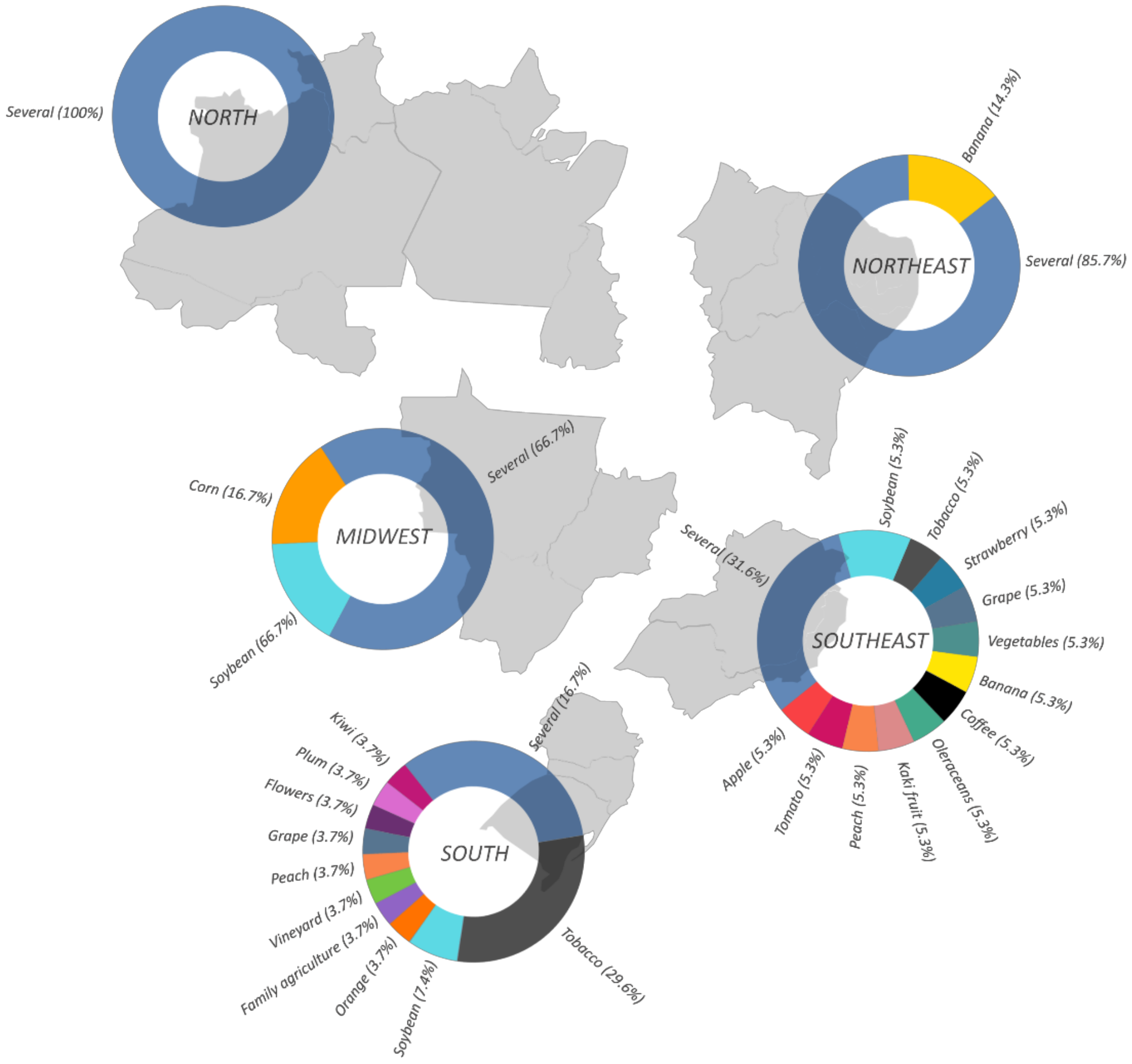
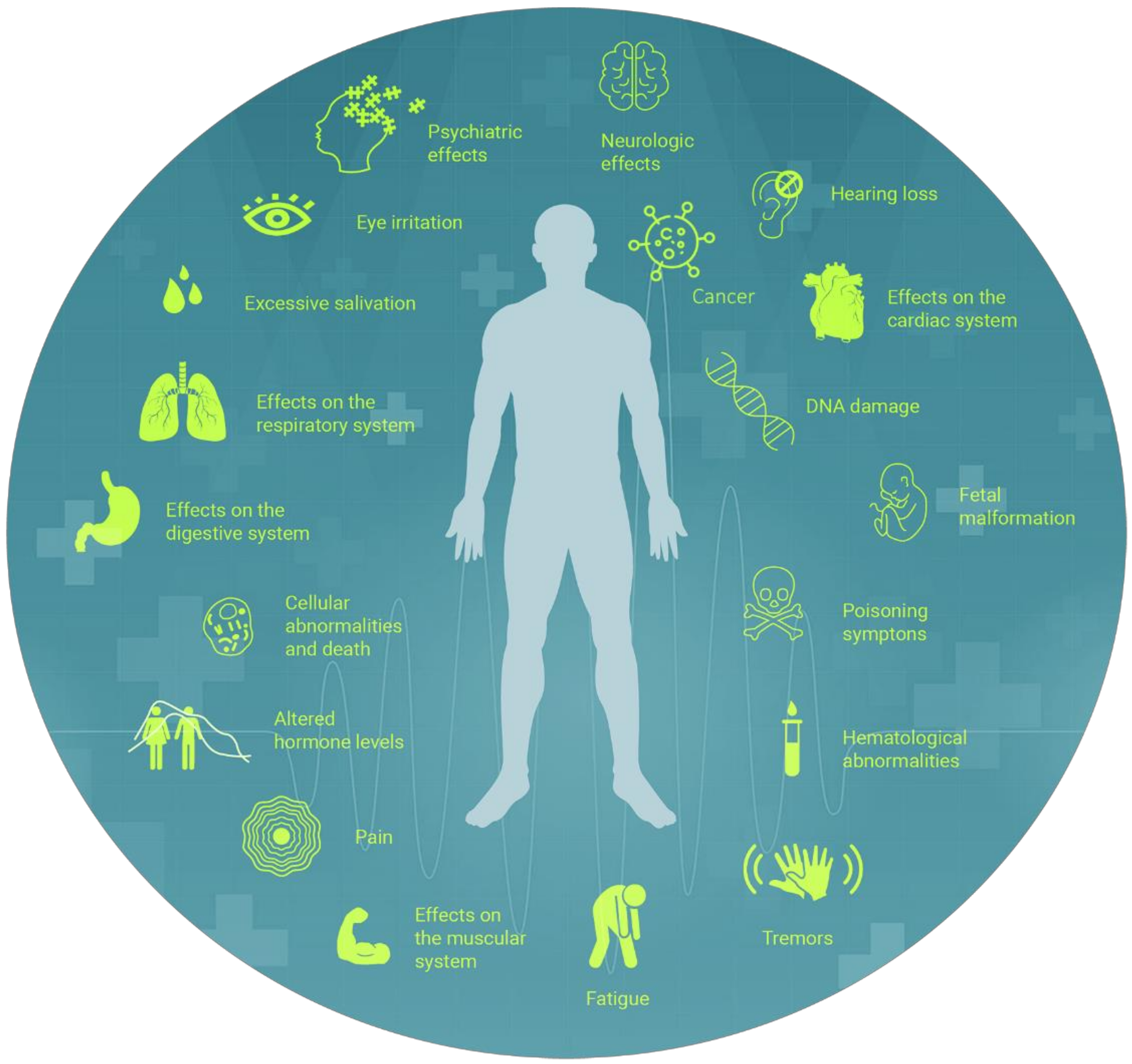
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Castro, N.R.; Spolador, H.F.S.; Marin, F.R. Assessing the economy–climate relationships for Brazilian agriculture. Empir. Econ. 2020, 59, 1161–1188. [Google Scholar] [CrossRef]
- de Souza Ramser, C.A.; Souza, A.M.; Souza, F.M.; da Veiga, C.P.; da Silva, W.V. The importance of principal components in studying mineral prices using vector autoregressive models: Evidence from the Brazilian economy. Resour. Policy 2019, 62, 9–21. [Google Scholar] [CrossRef]
- Brasil, Ministério da Agricultura, P. e A. de D.A. Portaria No. 43, de 21 de Fevereiro de 2020. Available online: http://www.agricultura.gov.br/assuntos/insumos-agropecuarios/insumos-agricolas/agrotoxicos/informacoes-tecnicas (accessed on 21 February 2020).
- Centro de Estudos Avançados em Economia Aplicada/Escola Superior de Agricultura “Luiz de Queiroz” PIB do Agronegócio Brasileiro. Available online: https://www.cepea.esalq.usp.br/br/pib-do-agronegocio-brasileiro.aspx (accessed on 27 November 2019).
- Eloy, L.; Aubertin, C.; Toni, F.; Lúcio, S.L.B.; Bosgiraud, M. On the margins of soy farms: Traditional populations and selective environmental policies in the Brazilian Cerrado. J. Peasant Stud. 2016, 43, 494–516. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística. Condições de Vida Desigualdade e Pobreza Condições de Vida, Desigualdade e Pobreza. Available online: https://www.ibge.gov.br/estatisticas/multidominio/condicoes-de-vida-desigualdade-e-pobreza.html (accessed on 1 June 2021).
- Wittman, H.; Desmarais, A.; Wiebe, N. Food Sovereignty: Reconnecting Food, Nature and Community. Environ. Soc. Res. 2010, 2, 87–105. [Google Scholar]
- Alimentar, N.B.C.N.; de Lei, S. Cria o Sistema Nacional de Segurança Alimentar e Nutricional-SISAN com vistas em assegurar o direito humano à alimentação adequada e dá outras providências. Diário Oficial da Uniāo 2006. Available online: http://www.planalto.gov.br/ccivil_03/_ato2004-2006/2006/lei/l11346.htm (accessed on 26 September 2021).
- Ribeiro, H.; Jaime, P.C.; Ventura, D. Alimentação e sustentabilidade. Estud. Avançados 2017, 31, 185–198. [Google Scholar] [CrossRef]
- Sauer, S. Agricultura Familiar versus Agronegócio: A Dinâmica Sociopolítica do Campo Brasileiro; Embrapa Informação Tecnológica: Rio de Janeiro, Brazil, 2006. [Google Scholar]
- Safety, F. Farm to Fork Strategy. Available online: https://ec.europa.eu/info/strategy/priorities-2019-2024/european-green-deal/actions-being-taken-eu/farm-fork_en (accessed on 1 June 2021).
- FAOSTAT International Code of Conduct on the Distribution and Use of Pesticides. Available online: https://apps.who.int/iris/bitstream/handle/10665/70293/WHO_HTM_NTD_WHOPES_2010.7_eng.pdf (accessed on 1 June 2020).
- FAOSTAT Definitions and Standards Used in FAOSTAT. Available online: http://www.fao.org/faostat/en/#definitions (accessed on 1 June 2020).
- Brasil Ato No. 91. 26 December 2019. Available online: http://www.in.gov.br/web/dou/-/ato-n-91-de-26-de-dezembro-de-2019-235559622 (accessed on 28 February 2020).
- ANVISA Programa de Análise de Resíduos de Agrotóxicos-Relatório 2017 e 2018. Available online: https://www.gov.br/anvisa/pt-br/centraisdeconteudo/publicacoes/agrotoxicos/programa-de-analise-de-residuos-de-agrotoxicos-relatorio-2017-e-2018.pdf/view (accessed on 10 February 2020).
- Hess, S.C.; Nodari, R.O.; Lopes-Ferreira, M. Agrotóxicos: Críticas à regulação que permite o envenenamento do país. Agron. Tempos Colapso Planet. Abordagens Crit. 2021, 57, 105–134. [Google Scholar] [CrossRef]
- Friedrich, K.; da Silveira, G.R.; Amazonas, J.C.; do Gurgel, A.M.; de Almeida, V.E.S.; Sarpa, M. Situação regulatória internacional de agrotóxicos com uso autorizado no Brasil: Potencial de danos sobre a saúde e impactos ambientais. Cad. Saude Publica 2021, 37. [Google Scholar] [CrossRef]
- Monneret, C. What is an endocrine disruptor? Comptes Rendus Biol. 2017, 340, 403–405. [Google Scholar] [CrossRef]
- Gundogan, K.; Donmez-Altuntas, H.; Hamurcu, Z.; Akbudak, I.H.; Sungur, M.; Bitgen, N.; Baskol, G.; Bayram, F. Evaluation of chromosomal DNA damage, cytotoxicity, cytostasis, oxidative DNA damage and their relationship with endocrine hormones in patients with acute organophosphate poisoning. Mutat. Res. Toxicol. Environ. Mutagen. 2018, 825, 1–7. [Google Scholar] [CrossRef]
- Jokanović, M. Neurotoxic effects of organophosphorus pesticides and possible association with neurodegenerative diseases in man: A review. Toxicology 2018, 410, 125–131. [Google Scholar] [CrossRef]
- Elgueta, S.; Valenzuela, M.; Fuentes, M.; Ulloa, P.; Ramos, C.; Correa, A.; Molinett, S. Analysis of multi-pesticide residues and dietary risk assessment in fresh tomatoes (Lycopersicum esculentum) from local supermarkets of the metropolitan region, Chile. Toxics 2021, 9, 249. [Google Scholar] [CrossRef]
- World Health Organization Pesticide Residues in Food. Available online: https://www.who.int/en/news-room/fact-sheets/detail/pesticide-residues-in-food (accessed on 12 January 2019).
- World Health Organization Health Topics-Pesticides. Available online: https://www.who.int/topics/pesticides/en/ (accessed on 20 February 2020).
- Agência Nacional de Vigilância Sanitária Relatório do Plano Plurianual 2017–2020–Ciclo 2017/2018. Available online: http://portal.anvisa.gov.br/programa-de-analise-de-registro-de-agrotoxicos-para (accessed on 10 February 2020).
- Ferreira, V.B.; Estrella, L.F.; Alves, M.G.R.; Gallistl, C.; Vetter, W.; Silva, T.T.C.; Malm, O.; Torres, J.P.M.; Abadio Finco, F.D.B. Residues of legacy organochlorine pesticides and DDT metabolites in highly consumed fish from the polluted Guanabara Bay, Brazil: Distribution and assessment of human health risk. J. Environ. Sci. Health Part B 2020, 55, 30–41. [Google Scholar] [CrossRef]
- Da Silva, H.C.M.P.; Bedor, D.C.G.; Cunha, A.N.; dos Rodrigues, H.O.S.; Telles, D.L.; Araújo, A.C.P.; de Santana, D.P. Ethephon and fosetyl residues in fruits from São Francisco Valley, Brazil. Food Addit. Contam. Part B 2020, 13, 16–24. [Google Scholar] [CrossRef]
- Pedon de Araujo Cardoso, T.; Viturino da Silva, J.W.; Kishishita, J.; Galindo Bedor, C.N.; Galindo Bedor, D.C.; Pereira de Santana, D.; Bastos Leal, L. Pesticide dermal absorption: Case study x in vitro study. Environ. Toxicol. Pharmacol. 2020, 75, 103313. [Google Scholar] [CrossRef]
- Associação Brasileira de Saúde Coletiva Dossiê Agrotóxicos. Available online: https://abrasco.org.br/dossieagrotoxicos/ (accessed on 1 June 2021).
- Stillerman, K.P.; Mattison, D.R.; Giudice, L.C.; Woodruff, T.J. Environmental exposures and adverse pregnancy outcomes: A review of the science. Reprod. Sci. 2008, 15, 631–650. [Google Scholar] [CrossRef]
- Mavoungou, S.; Rios, P.; Pacquement, H.; Nolla, M.; Rigaud, C.; Simonin, M.; Bertrand, Y.; Lambilliotte, A.; Faure, L.; Orsi, L.; et al. Maternal exposure to pesticides and risk of childhood lymphoma in France: A pooled analysis of the ESCALE and ESTELLE studies (SFCE). Cancer Epidemiol. 2020, 68, 101797. [Google Scholar] [CrossRef]
- Criswell, R.; Crawford, K.A.; Bucinca, H.; Romano, M.E. Endocrine-disrupting chemicals and breastfeeding duration: A review. Curr. Opin. Endocrinol. Diabetes Obes. 2020, 27, 388–395. [Google Scholar] [CrossRef]
- Helou, K.; Matta, J.; Harmouche-Karaki, M.; Sayegh, N.; Younes, H.; Mahfouz, Y.; Mahfouz, M.; Karake, S.; Finan, R.; Abi-Tayeh, G.; et al. Maternal and cord serum levels of polychlorinated biphenyls (PCBs) and organochlorine pesticides (OCPs) among Lebanese pregnant women and predictors of exposure. Chemosphere 2021, 266, 129211. [Google Scholar] [CrossRef]
- Cruz, F.O. Coleção Saúde, Ambiente e Sustentabilidade-Capítulo 2-Agrotóxicos. Available online: https://portal.fiocruz.br/sites/portal.fiocruz.br/files/documentos/02_agrotoxicos.pdf (accessed on 1 June 2021).
- Queiroz, P.R.; Lima, K.C.; de Oliveira, T.C.; dos Santos, M.M.; Jacob, J.F.; de Oliveira, A.M.B.M. Sistema de Informação de Agravos de Notificação e as intoxicações humanas por agrotóxicos no Brasil. Rev. Bras. Epidemiol. 2019, 22, e190033. [Google Scholar] [CrossRef]
- Menck, V.F.; Serafim, M.P.; Oliveira, J.M. Intoxicação do(a) trabalhador(a) rural por agrotóxicos: (Sub)notificação e (in)visibilidade nas políticas públicas de 2001 a 2015. Segur. Aliment. Nutr. 2019, 26, e019001. [Google Scholar] [CrossRef][Green Version]
- Faria, N.M.X.; Fassa, A.G.; Facchini, L.A. Intoxicação por agrotóxicos no Brasil: Os sistemas oficiais de informação e desafios para realização de estudos epidemiológicos. Ciênc. Saúde Colet. 2007, 12, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Buralli, R.J.; Ribeiro, H.; Iglesias, V.; Muñoz-Quezada, M.T.; Leão, R.S.; Marques, R.C.; de Almeida, M.M.C.; Guimarães, J.R.D. Occupational exposure to pesticides and health symptoms among family farmers in Brazil. Rev. Saude Publica 2020, 54, 133. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, C.L.F.; Volcão, L.M.; Ramires, P.F.; De Moura, R.R.; Da Silva Júnior, F.M.R. Distribution of pesticides in agricultural and urban soils of Brazil: A critical review. Environ. Sci. Process. Impacts 2020, 22, 256–270. [Google Scholar] [CrossRef]
- Hess, S.C. Ensaios Sobre Poluição e Doenças no Brasil. Available online: https://repositorio.ufsc.br/bitstream/handle/123456789/187660/LIVRO.pdf?sequence=1&isAllowed=y (accessed on 1 June 2021).
- Neves, P.D.M.; Mendonça, M.R.; Bellini, M.; Pôssas, I.B. Intoxicação por agrotóxicos agrícolas no estado de Goiás, Brasil, de 2005–2015: Análise dos registros nos sistemas oficiais de informação. Ciênc. Saúde Colet. 2020, 25, 2743–2754. [Google Scholar] [CrossRef]
- Silvério, A.C.P.; Martins, I.; Nogueira, D.A.; Mello, M.A.S.; de Loyola, E.A.C.; de Graciano, M.M.C. Assessment of Primary Health Care for rural workers exposed to pesticides. Rev. Saude Publica 2020, 54, 9. [Google Scholar] [CrossRef]
- Lovison Sasso, E.; Cattaneo, R.; Rosso Storck, T.; Spanamberg Mayer, M.; Sant’Anna, V.; Clasen, B. Occupational exposure of rural workers to pesticides in a vegetable-producing region in Brazil. Environ. Sci. Pollut. Res. 2021, 28, 25758–25769. [Google Scholar] [CrossRef]
- Freire, C.; Koifman, R.J.; Koifman, S. Serum levels of organochlorine pesticides in blood donors: A biomonitoring survey in the North of Brazil, 2010–2011. Sci. Total Environ. 2017, 598, 722–732. [Google Scholar] [CrossRef]
- Yanai, A.M.; de Graça, P.M.L.A.; Escada, M.I.S.; Ziccardi, L.G.; Fearnside, P.M. Deforestation dynamics in Brazil’s Amazonian settlements: Effects of land-tenure concentration. J. Environ. Manag. 2020, 268, 110555. [Google Scholar] [CrossRef]
- Instituto Nacional de Pesquisas Espaciais Plataforma Terra Brasilis. Available online: http://terrabrasilis.dpi.inpe.br/app/map/deforestation?hl=pt-br (accessed on 24 June 2020).
- Nepstad, D.; McGrath, D.; Stickler, C.; Alencar, A.; Azevedo, A.; Swette, B.; Bezerra, T.; DiGiano, M.; Shimada, J.; da Motta, R.; et al. Slowing Amazon deforestation through public policy and interventions in beef and soy supply chains. Science 2014, 344, 1118–1123. [Google Scholar] [CrossRef]
- Kurwadkar, S. Groundwater Pollution and Vulnerability Assessment. Water Environ. Res. 2017, 89, 1561–1579. [Google Scholar] [CrossRef]
- Introduction to OECD Test Guidelines on Pesticide Residues Chemistry-Section 5 Part A; OECD Guidelines for the Testing of Chemicals, Section 5; OECD: Paris, France, 2013; ISBN 9789264203761.
- Rose, C.; Coupe, R.; Capel, P.; Webb, R. Holistic assessment of occurrence and fate of metolachlor within environmental compartments of agricultural watersheds. Sci. Total Environ. 2017, 612, 708–719. [Google Scholar] [CrossRef]
- de Castro Lima, J.A.M.; Labanowski, J.; Bastos, M.C.; Zanella, R.; Prestes, O.D.; de Vargas, J.P.R.; Mondamert, L.; Granado, E.; Tiecher, T.; Zafar, M.; et al. “Modern agriculture” transfers many pesticides to watercourses: A case study of a representative rural catchment of southern Brazil. Environ. Sci. Pollut. Res. 2020, 27, 10581–10598. [Google Scholar] [CrossRef]
- Guarda, P.M.; Pontes, A.M.S.; de Domiciano, R.S.; da Gualberto, L.S.; Mendes, D.B.; Guarda, E.A.; da Silva, J.E.C. Assessment of Ecological Risk and Environmental Behavior of Pesticides in Environmental Compartments of the Formoso River in Tocantins, Brazil. Arch. Environ. Contam. Toxicol. 2020, 79, 524–536. [Google Scholar] [CrossRef]
- Rocha, G.H.O.; Lini, R.S.; Barbosa, F.J.; Batista, B.L.; de Oliveira Souza, V.C.; Nerilo, S.B.; Bando, E.; Mossini, S.A.G.; Nishiyama, P. Exposure to heavy metals due to pesticide use by vineyard farmers. Int. Arch. Occup. Environ. Health 2015, 88, 875–880. [Google Scholar] [CrossRef]
- Kahl, V.F.S.; da Silva, J.; da Silva, F.R. Influence of exposure to pesticides on telomere length in tobacco farmers: A biology system approach. Mutat. Res. 2016, 791, 19–26. [Google Scholar] [CrossRef]
- Carvalho, D.F.P.; Meire, R.O.; Guimarães, M.T.; Pereira, L.A.A.; Braga, A.L.F.; Bernardo, R.R.; Torres, J.P.M.; Malm, O. Determination of Environmental Exposure to DDT by Human Hair Analysis in Santos and São Vicente Estuary, São Paulo, Brazil. Orbital Electron. J. Chem. 2018, 10, 308–319. [Google Scholar] [CrossRef]
- Brito, J.G.; de Martins, C.B.G. Accidental intoxication of the infant-juvenile population in households: Profiles of emergency care. Rev. Esc. Enferm. USP 2015, 49, 373–380. [Google Scholar] [CrossRef]
- Cezar-Vaz, M.R.; Bonow, C.A.; Piexak, D.R.; Kowalczyk, S.; Vaz, J.C.; Borges, A.M. Skin cancer in rural workers: Nursing knowledge and intervention. Rev. Esc. Enferm. USP 2015, 49, 0564–0571. [Google Scholar] [CrossRef]
- Rocha, T.A.L.C.G.; de Oliveira, F.N. Segurança e Saúde do Trabalho: Vulnerabilidade e percepção de riscos relacionados ao uso de agroquímicos em um pólo de fruticultura irrigada do Rio Grande do Norte. Gest. Prod. 2016, 23, 600–611. [Google Scholar] [CrossRef][Green Version]
- Pignati, W.; Lima, F.; Lara, S.; Correa, M.; Barbosa, J.; Leão, L.; Pignatti, M. Distribuição espacial do uso de agrotóxicos no Brasil: Uma ferramenta para a Vigilância em Saúde. Ciênc. Saúde Colet. 2017, 22, 3281–3293. [Google Scholar] [CrossRef] [PubMed]
- Leão, R.S.; Marques, R.C.; Buralli, R.J.; Silva, D.S.; Guimarães, J.R.D. Public health assessment of agrochemicals exposure: An experience with family farming in the northwest of Rio de Janeiro|Avaliação de saúde pública por exposição a agroquímicos: Uma experiência com a agricultura familiar no noroeste do Rio de Janeiro. Sustentab. Debate 2018, 9, 81–94. [Google Scholar] [CrossRef]
- Bortolotto, C.C.; Hirschmann, R.; Martins-Silva, T.; Facchini, L.A. Exposição a agrotóxicos: Estudo de base populacional em zona rural do sul do Brasil. Rev. Bras. Epidemiol. 2020, 23, e200027. [Google Scholar] [CrossRef] [PubMed]
- Simas, J.M.M.; Yamauchi, L.Y.; do Alencar, M.C.B. de Risk factors associated among respiratory health and banana farming. Arch. Environ. Occup. Health 2021, 76, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Bombardi, L.M. Geografia do Uso de Agrotóxicos no Brasil e Conexões com a União Europeia. São Paulo; Faculdade de Filosofia Letras e Ciências Humanas da Universidade de São Paulo: São Paulo, Brazil, 2017. [Google Scholar]
- Brasil Ato no. 58, de 27 de Agosto de 2019: Altera as Classificações Toxicológicas dos Produtos Formulados Agrotóxicos. Brasília, Brazil. Available online: https://www.in.gov.br/web/dou/-/ato-n-58-de-27-de-agosto-de-2019-213474289 (accessed on 29 November 2021).
- Agência Nacional de Vigilância Sanitária Nota Técnica No. 23/2018. Apresenta a Nota Técnica Preliminar Sobre as Conclusões da Reavaliação do Glifosato. Available online: http://portal.anvisa.gov.br/documents/10181/5344168/1.+Nota+Técnica+Glifosato.pdf/d071af2d-5cb4-4443-b210-4bc43f2216b8 (accessed on 15 January 2020).
- Ministério da Indústria Comércio Exterior e Serviços Exportação Mercado de Commodities. Available online: http://www.mdic.gov.br/sistemas_web/aprendex/cooperativismo/index/conteudo/id/304 (accessed on 21 February 2020).
- Ramos, J.S.A.; Pedroso, T.M.A.; Godoy, F.R.; Batista, R.E.; de Almeida, F.B.; Francelin, C.; Ribeiro, F.L.; Parise, M.R.; de Melo e Silva, D. Multi-biomarker responses to pesticides in an agricultural population from Central Brazil. Sci. Total Environ. 2021, 754, 141893. [Google Scholar] [CrossRef] [PubMed]
- Pérez, G.; Vera, M.; Miranda, L. Effects of Herbicide Glyphosate and Glyphosate-Based Formulations on Aquatic Ecosystems. In Herbicides and Environment; BoD—Books on Demand: Norderstedt, Germany, 2011; pp. 343–368. ISBN 978-953-307-476-4. [Google Scholar]
- de Castilhos Ghisi, N.; Zuanazzi, N.R.; Fabrin, T.M.C.; Oliveira, E.C. Glyphosate and its toxicology: A scientometric review. Sci. Total Environ. 2020, 733, 139359. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, J.P.; Bleak, T.C.; Calaf, G.M. Glyphosate and the key characteristics of an endocrine disruptor: A review. Chemosphere 2021, 270, 128619. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro do Meio Ambiente e dos Recursos Naturais Relatórios de Comercialização de Agrotóxicos. Available online: http://ibama.gov.br/agrotoxicos/relatorios-de-comercializacao-de-agrotoxicos (accessed on 28 November 2019).
- Brasil. Ministério da Saúde. Secretaria de Vigilânica em Saúde. Coordenação-Geral de Vigilância em Saúde Ambiental. Portaria MS n.º 518/2004/Ministério da Saúde, Secretaria de Vigilância em Saúde, CoordenaçãoGeral de Vigilância em Saúde Ambiental–Brasília; Editora do Ministério da Saúde: Brasilia, Brazil, 2005.
- Persch, T.S.P.; da Silva, P.R.; dos Santos, S.H.D.; de Freitas, B.S.; Oliveira, G.T. Changes in intermediate metabolism and oxidative balance parameters in sexually matured three-barbeled catfishes exposed to herbicides from rice crops (Roundup®, Primoleo® and Facet®). Environ. Toxicol. Pharmacol. 2018, 58, 170–179. [Google Scholar] [CrossRef]
- Masood, M.I.; Naseem, M.; Warda, S.A.; Tapia-Laliena, M.Á.; Rehman, H.; Nasim, M.J.; Schäfer, K.H. Environment permissible concentrations of glyphosate in drinking water can influence the fate of neural stem cells from the subventricular zone of the postnatal mouse. Environ. Pollut. 2021, 270, 116179. [Google Scholar] [CrossRef]
- Tsai, W.-T. Trends in the Use of Glyphosate Herbicide and Its Relevant Regulations in Taiwan: A Water Contaminant of Increasing Concern. Toxics 2019, 7, 4. [Google Scholar] [CrossRef]
- Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde Relatório Nacional de Vigilância em Saúde de Populações Expostas a Agrotóxicos. Available online: https://bvsms.saude.gov.br/bvs/publicacoes/relatorio_nacional_vigilancia_populacoes_expostas_agrotoxicos.pdf (accessed on 1 June 2021).
- Brasil. Ministério da Saúde. Casos Notificados de Intoxicações Exógenas Relacionados ao Glifosato no Brasil, no Período de 2007 a 2016. Available online: http://portalarquivos2.saude.gov.br/images/pdf/2018/dezembro/04/BE-2018-31-Glifosato.pdf (accessed on 1 June 2021).
- Disner, G.R.; Falcão, M.A.P.; Andrade-Barros, A.I.; Leite dos Santos, N.V.; Soares, A.B.S.; Marcolino-Souza, M.; Gomes, K.S.; Lima, C.; Lopes-Ferreira, M. The Toxic Effects of Glyphosate, Chlorpyrifos, Abamectin, and 2,4-D on Animal Models: A Systematic Review of Brazilian Studies. Integr. Environ. Assess. Manag. 2021, 17, 507–520. [Google Scholar] [CrossRef]
- Sergievich, A.A.; Khoroshikh, P.P.; Artemenko, A.F.; Zakharenko, A.M.; Chaika, V.V.; Kodintsev, V.V.; Stroeva, O.A.; Lenda, E.G.; Tsatsakis, A.; Burykina, T.I.; et al. Behavioral impacts of a mixture of six pesticides on rats. Sci. Total Environ. 2020, 727, 138491. [Google Scholar] [CrossRef]
- Bonner, M.R.; Freeman, L.E.B.; Hoppin, J.A.; Koutros, S.; Sandler, D.P.; Lynch, C.F.; Hines, C.J.; Thomas, K.; Blair, A.; Alavanja, M.C.R. Occupational Exposure to Pesticides and the Incidence of Lung Cancer in the Agricultural Health Study. Environ. Health Perspect. 2017, 125, 544–551. [Google Scholar] [CrossRef]
- Dutra, L.S.; Ferreira, A.P.; Horta, M.A.P.; Palhares, P.R. Uso de agrotóxicos e mortalidade por câncer em regiões de monoculturas. Saúde Debate 2020, 44, 1018–1035. [Google Scholar] [CrossRef]
- Calaf, G.; Ponce-Cusi, R.; Aguayo, F.; Muñoz, J.; Bleak, T. Endocrine disruptors from the environment affecting breast cancer (Review). Oncol. Lett. 2020, 20, 19–32. [Google Scholar] [CrossRef]
- Guida, Y.; de Carvalho, G.O.; Capella, R.; Pozo, K.; Lino, A.S.; Azeredo, A.; Carvalho, D.F.P.; Braga, A.L.F.; Torres, J.P.M.; Meire, R.O. Atmospheric Occurrence of Organochlorine Pesticides and Inhalation Cancer Risk in Urban Areas at Southeast Brazil. Environ. Pollut. 2021, 271, 116359. [Google Scholar] [CrossRef]
- Rede Nacional de Atenção Integral à Saúde do Trabalhador Agência da OMS Divulga Publicação Sobre a Relação Entre Organofosforados e Câncer. (Grupo 2A). Available online: https://renastonline.ensp.fiocruz.br/noticias/agencia-oms-divulga-publicacao-sobre-relacao-entre-organofosforados-cancer#:~:text=Recentemente%2CaIARCdivulgouo,parahumanos (accessed on 1 June 2021).
- Costa, M.B.; Farias, I.R.; da Silva Monte, C.; Filho, L.I.P.F.; de Paula Borges, D.; de Oliveira, R.T.G.; Ribeiro-Junior, H.L.; Magalhães, S.M.M.; Pinheiro, R.F. Chromosomal abnormalities and dysregulated DNA repair gene expression in farmers exposed to pesticides. Environ. Toxicol. Pharmacol. 2021, 82, 103564. [Google Scholar] [CrossRef]
- Dos Santos, N.F.; Contrera, L.; Teston, E.F.; Kawakame, P.M.G.; Reis, L.E.A.; de Amarilha, K.J.O. Evidências dos efeitos neurotóxicos por exposição ao agrotóxico: Uma revisão integrativa/evidence of neurotoxic effects by exposure to pesticide. Braz. J. Dev. 2020, 6, 102160–102170. [Google Scholar] [CrossRef]
- Bonvoisin, T.; Utyasheva, L.; Knipe, D.; Gunnell, D.; Eddleston, M. Suicide by pesticide poisoning in India: A review of pesticide regulations and their impact on suicide trends. BMC Public Health 2020, 20, 251. [Google Scholar] [CrossRef]
- Dardiotis, E.; Aloizou, A.-M.; Sakalakis, E.; Siokas, V.; Koureas, M.; Xiromerisiou, G.; Petinaki, E.; Wilks, M.; Tsatsakis, A.; Hadjichristodoulou, C.; et al. Organochlorine pesticide levels in Greek patients with Parkinson’s disease. Toxicol. Rep. 2020, 7, 596–601. [Google Scholar] [CrossRef]
- Schneider Medeiros, M.; Reddy, S.P.; Socal, M.P.; Schumacher-Schuh, A.F.; Mello Rieder, C.R. Occupational pesticide exposure and the risk of death in patients with Parkinson’s disease: An observational study in southern Brazil. Environ. Health 2020, 19, 68. [Google Scholar] [CrossRef]
- Green, M.P.; Harvey, A.J.; Finger, B.J.; Tarulli, G.A. Endocrine disrupting chemicals: Impacts on human fertility and fecundity during the peri-conception period. Environ. Res. 2021, 194, 110694. [Google Scholar] [CrossRef] [PubMed]
- Kahn, L.G.; Philippat, C.; Nakayama, S.F.; Slama, R.; Trasande, L. Endocrine-disrupting chemicals: Implications for human health. Lancet Diabetes Endocrinol. 2020, 8, 703–718. [Google Scholar] [CrossRef]
- Kassotis, C.D.; Vandenberg, L.N.; Demeneix, B.A.; Porta, M.; Slama, R.; Trasande, L. Endocrine-disrupting chemicals: Economic, regulatory, and policy implications. Lancet Diabetes Endocrinol. 2020, 8, 719–730. [Google Scholar] [CrossRef]
- Zhang, C.; Schilirò, T.; Gea, M.; Bianchi, S.; Spinello, A.; Magistrato, A.; Gilardi, G.; Di Nardo, G. Molecular Basis for Endocrine Disruption by Pesticides Targeting Aromatase and Estrogen Receptor. Int. J. Environ. Res. Public Health 2020, 17, 5664. [Google Scholar] [CrossRef]
- Petrakis, D.; Vassilopoulou, L.; Mamoulakis, C.; Psycharakis, C.; Anifantaki, A.; Sifakis, S.; Docea, A.O.; Tsiaoussis, J.; Makrigiannakis, A.; Tsatsakis, A.M. Endocrine Disruptors Leading to Obesity and Related Diseases. Int. J. Environ. Res. Public Health 2017, 14, 1282. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Ni, Y.; Jin, Y.; Fu, Z. Pesticides-induced energy metabolic disorders. Sci. Total Environ. 2020, 729, 139033. [Google Scholar] [CrossRef]
- de Adad, L.M.M.; Andrade, H.H.R.; Kvitko, K.; Lehmann, M.; Cavalcante, A.A.M.C.; Dihl, R.R. Occupational exposure of workers to pesticides: Toxicogenetics and susceptibility gene polymorphisms. Genet. Mol. Biol. 2015, 38, 308–315. [Google Scholar] [CrossRef]
- Kahl, V.F.S.; da Silva, F.R.; Alves, J.D.S.; da Silva, G.F.; Picinini, J.; Dhillon, V.S.; Fenech, M.; Souza, M.R.; Dias, J.F.; de Souza, C.T.; et al. Role of PON1, SOD2, OGG1, XRCC1, and XRCC4 polymorphisms on modulation of DNA damage in workers occupationally exposed to pesticides. Ecotoxicol. Environ. Saf. 2018, 159, 164–171. [Google Scholar] [CrossRef]
- Kahl, V.F.S.; Dhillon, V.S.; Simon, D.; da Silva, F.R.; Salvador, M.; Branco, C.D.S.; Cappetta, M.; Martínez-López, W.; Thiesen, F.V.; Dias, J.F.; et al. Chronic occupational exposure endured by tobacco farmers from Brazil and association with DNA damage. Mutagenesis 2018, 33, 119–128. [Google Scholar] [CrossRef]
- Marcelino, A.F.; Wachtel, C.C.; Ghisi, N.D.; Marcelino, A.F.; Wachtel, C.C.; de Ghisi, N.C. Are Our Farm Workers in Danger? Genetic Damage in Farmers Exposed to Pesticides. Int. J. Environ. Res. Public Health 2019, 16, 358. [Google Scholar] [CrossRef]
- Oliveira, S.E.; Costa, P.M.; Nascimento, S.B.; Castro, W.V.; de Ribeiro, R.I.M.A.; Santos, H.B.; Thomé, R.G. Atrazine promotes immunomodulation by melanomacrophage centre alterations in spleen and vascular disorders in gills from Oreochromis niloticus. Aquat. Toxicol. 2018, 202, 57–64. [Google Scholar] [CrossRef]
- Bernieri, T.; Rodrigues, D.R.; Randon Barbosa, I.; Perassolo, M.S.; Grolli Ardenghi, P.; da Barros Silva, L. Effect of pesticide exposure on total antioxidant capacity and biochemical parameters in Brazilian soybean farmers. Drug Chem. Toxicol. 2021, 44, 170–176. [Google Scholar] [CrossRef]
- Mori, N.C.; Horn, R.C.; Oliveira, C.; Leal, P.A.P.; Golle, D.P.; Koefender, J.; Bortolotto, J.; Dias, H.M. Alterações bioquímicas e toxicológicas de agricultores familiares da região do Alto Jacuí, Rio Grande do Sul. Sci. Med. 2015, 25, 20999. [Google Scholar] [CrossRef]
- Wilhelm, C.M.; Calsing, A.K.; da Silva, L.B. Assessment of DNA damage in floriculturists in southern Brazil. Environ. Sci. Pollut. Res. Int. 2015, 22, 8182–8189. [Google Scholar] [CrossRef]
- Alves, J.S.; DA Silva, F.R.; DA Silva, G.F.; Salvador, M.; Kvitko, K.; Rohr, P.; DOS Santos, C.E.I.; DIAS, J.F.; Henriques, J.A.P.; Silva, J. DA Investigation of potential biomarkers for the early diagnosis of cellular stability after the exposure of agricultural workers to pesticides. An. Acad. Bras. Ciênc. 2016, 88, 349–360. [Google Scholar] [CrossRef]
- Cattelan, M.D.P.; Maurer, P.; Garcia, F.; Berro, L.F.; Machado, M.M.; Manfredini, V.; da Piccoli, J.C.E. Occupational exposure to pesticides in family agriculture and the oxidative, biochemical and hematological profile in this agricultural model. Life Sci. 2018, 203, 177–183. [Google Scholar] [CrossRef]
- Jacobsen-Pereira, C.H.; Cardoso, C.C.; Gehlen, T.C.; Regina Dos Santos, C.; Santos-Silva, M.C. Immune response of Brazilian farmers exposed to multiple pesticides. Ecotoxicol. Environ. Saf. 2020, 202, 110912. [Google Scholar] [CrossRef]
- Smith, M.T.; Guyton, K.Z.; Gibbons, C.F.; Fritz, J.M.; Portier, C.J.; Rusyn, I.; DeMarini, D.M.; Caldwell, J.C.; Kavlock, R.J.; Lambert, P.F.; et al. Key Characteristics of Carcinogens as a Basis for Organizing Data on Mechanisms of Carcinogenesis. Environ. Health Perspect. 2016, 124, 713–721. [Google Scholar] [CrossRef]
- Extra Classe Pesquisas Associam Câncer ao Uso Intensivo de Agrotóxicos nas Lavouras. Available online: https://www.extraclasse.org.br/saude/2018/05/pesquisas-associam-cancer-ao-uso-intensivo-de-agrotoxicos-nas-lavouras/#:~:text=Pesquisasassociamcânceraousointensivodeagrotóxicosnaslavouras,-PorTomBelmonte&text=AagricultoraFabianeLange%2C35,pe (accessed on 1 June 2021).
- Instituto Nacional do Câncer Agrotóxicos. Available online: https://www.inca.gov.br/exposicao-no-trabalho-e-no-ambiente/agrotóxicos (accessed on 1 June 2021).
- G1 MP Apura Presença de 27 Agrotóxicos que Causam Câncer e Malformação Fetal na Água que Abastece Cuiabá. Available online: https://g1.globo.com/mt/mato-grosso/noticia/2019/05/13/mp-apura-presenca-de-27-agrotoxicos-que-causam-cancer-e-malformacao-fetal-na-agua-que-abastece-cuiaba.ghtml (accessed on 3 May 2021).
- Mokarizadeh, A.; Faryabi, M.R.; Rezvanfar, M.A.; Abdollahi, M. A comprehensive review of pesticides and the immune dysregulation: Mechanisms, evidence and consequences. Toxicol. Mech. Methods 2015, 25, 258–278. [Google Scholar] [CrossRef]
- dos Santos Mendonça, J.; Vieira, L.G.; Valdes, S.A.C.; Vilca, F.Z.; Tornisielo, V.L.; Santos, A.L.Q. Effects of the exposure to atrazine on bone development of Podocnemis expansa (Testudines, Podocnemididae). Ecotoxicology 2016, 25, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Daisley, B.A.; Trinder, M.; McDowell, T.W.; Welle, H.; Dube, J.S.; Ali, S.N.; Leong, H.S.; Sumarah, M.W.; Reid, G. Neonicotinoid-induced pathogen susceptibility is mitigated by Lactobacillus plantarum immune stimulation in a Drosophila melanogaster model. Sci. Rep. 2017, 7, 2703. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Briguglio, G.; Catanoso, R.; Giambò, F.; Polito, I.; Teodoro, M.; Fenga, C. New perspectives on cytokine pathways modulation by pesticide exposure. Curr. Opin. Toxicol. 2020, 19, 99–104. [Google Scholar] [CrossRef]
- Giambò, F.; Teodoro, M.; Costa, C.; Fenga, C. Toxicology and Microbiota: How Do Pesticides Influence Gut Microbiota? A Review. Int. J. Environ. Res. Public Health 2021, 18, 5510. [Google Scholar] [CrossRef]
- Akdis, C.A. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat. Rev. Immunol. 2021, 21, 739–751. [Google Scholar] [CrossRef]
- Blacher, E.; Bashiardes, S.; Shapiro, H.; Rothschild, D.; Mor, U.; Dori-Bachash, M.; Kleimeyer, C.; Moresi, C.; Harnik, Y.; Zur, M.; et al. Potential roles of gut microbiome and metabolites in modulating ALS in mice. Nature 2019, 572, 474–480. [Google Scholar] [CrossRef]
- Dalbo, J.; Filgueiras, L.A.; Mendes, A.N.; Dalbo, J.; Filgueiras, L.A.; Mendes, A.N. Effects of pesticides on rural workers: Haematological parameters and symptomalogical reports. Ciênc. Saúde Colet. 2019, 24, 2569–2582. [Google Scholar] [CrossRef]
- Piccoli, C.; Cremonase, C.; Koifman, R.; Koifman, S.; Freire, C. Occupational exposure to pesticides and hematological alterations: A survey of farm residents in the south of brazil | Exposição ocupacional a agrotóxicos e alterações hematológicas: Estudo transversal em moradores rurais do Sul do Brasil. Ciênc. Saude Colet. 2019, 24, 2325–2340. [Google Scholar] [CrossRef]
- Cestonaro, L.V.; Garcia, S.C.; Nascimento, S.; Gauer, B.; Sauer, E.; Göethel, G.; Peruzzi, C.; Nardi, J.; Fão, N.; Piton, Y.; et al. Biochemical, hematological and immunological parameters and relationship with occupational exposure to pesticides and metals. Environ. Sci. Pollut. Res. 2020, 27, 29291–29302. [Google Scholar] [CrossRef]
- Pizzatti, L.; Kawassaki, A.C.B.; Fadel, B.; Nogueira, F.C.S.; Evaristo, J.A.M.; Woldmar, N.; Teixeira, G.T.; Da Silva, J.C.; Scandolara, T.B.; Rech, D.; et al. Toxicoproteomics Disclose Pesticides as Downregulators of TNF-α, IL-1β and Estrogen Receptor Pathways in Breast Cancer Women Chronically Exposed. Front. Oncol. 2020, 10, 1698. [Google Scholar] [CrossRef]
- Tichati, L.; Trea, F.; Ouali, K. Potential Role of Selenium against Hepatotoxicity Induced by 2,4-Dichlorophenoxyacetic Acid in Albino Wistar Rats. Biol. Trace Elem. Res. 2020, 194, 228–236. [Google Scholar] [CrossRef]
- Bernieri, T.; Rodrigues, D.; Barbosa, I.R.; Ardenghi, P.G.; Basso da Silva, L. Occupational exposure to pesticides and thyroid function in Brazilian soybean farmers. Chemosphere 2019, 218, 425–429. [Google Scholar] [CrossRef]
- Bernieri, T.; Moraes, M.F.; Ardenghi, P.G.; Basso da Silva, L. Assessment of DNA damage and cholinesterase activity in soybean farmers in southern Brazil: High versus low pesticide exposure. J. Environ. Sci. Health Part B 2020, 55, 355–360. [Google Scholar] [CrossRef]
- Lermen, J.; Bernieri, T.; Rodrigues, I.S.; Suyenaga, E.S.; Ardenghi, P.G. Pesticide exposure and health conditions among orange growers in Southern Brazil. J. Environ. Sci. Health Part B 2018, 53, 215–221. [Google Scholar] [CrossRef]
- do Nascimento, F.P.; Kuno, R.; Lemes, V.R.R.; Kussumi, T.A.; Nakano, V.E.; Rocha, S.B.; de Oliveira, M.C.C.; de Albuquerque Kimura, I.; Gouveia, N. Organochlorine pesticides levels and associated factors in a group of blood donors in São Paulo, Brazil. Environ. Monit. Assess. 2017, 189, 380. [Google Scholar] [CrossRef]
- Sifakis, S.; Androutsopoulos, V.P.; Tsatsakis, A.M.; Spandidos, D.A. Human exposure to endocrine disrupting chemicals: Effects on the male and female reproductive systems. Environ. Toxicol. Pharmacol. 2017, 51, 56–70. [Google Scholar] [CrossRef]
- Hernández, A.F.; Parrón, T.; Tsatsakis, A.M.; Requena, M.; Alarcón, R.; López-Guarnido, O. Toxic effects of pesticide mixtures at a molecular level: Their relevance to human health. Toxicology 2013, 307, 136–145. [Google Scholar] [CrossRef]
- De Silva, H.J.; Samarawickrema, N.A.; Wickremasinghe, A.R. Toxicity due to organophosphorus compounds: What about chronic exposure? Trans. R. Soc. Trop. Med. Hyg. 2006, 100, 803–806. [Google Scholar] [CrossRef]
- Perry, M.J.; Venners, S.A.; Chen, X.; Liu, X.; Tang, G.; Xing, H.; Barr, D.B.; Xu, X. Organophosphorous pesticide exposures and sperm quality. Reprod. Toxicol. 2011, 31, 75–79. [Google Scholar] [CrossRef]
- Yucra, S.; Rubio, J.; Gasco, M.; Gonzales, C.; Steenland, K.; Gonzales, G.F. Semen quality and reproductive sex hormone levels in Peruvian pesticide sprayers. Int. J. Occup. Environ. Health 2006, 12, 355–361. [Google Scholar] [CrossRef]
- Cremonese, C.; Piccoli, C.; Pasqualotto, F.; Clapauch, R.; Koifman, R.J.; Koifman, S.; Freire, C. Occupational exposure to pesticides, reproductive hormone levels and sperm quality in young Brazilian men. Reprod. Toxicol. 2017, 67, 174–185. [Google Scholar] [CrossRef] [PubMed]
- Santos, R.; Piccoli, C.; Cremonese, C.; Freire, C. Thyroid and reproductive hormones in relation to pesticide use in an agricultural population in Southern Brazil. Environ. Res. 2019, 173, 221–231. [Google Scholar] [CrossRef] [PubMed]
- Peiris-John, R.J.; Wickremasinghe, R. Impact of low-level exposure to organophosphates on human reproduction and survival. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Selevan, S.G.; Kimmel, C.A.; Mendola, P. Identifying critical windows of exposure for children’s health. Environ. Health Perspect. 2000, 108, 451–455. [Google Scholar] [CrossRef]
- Ueker, M.E.; Silva, V.M.; Moi, G.P.; Pignati, W.A.; Mattos, I.E.; Silva, A.M.C. Parenteral exposure to pesticides and occurence of congenital malformations: Hospital-based case-control study. BMC Pediatr. 2016, 16, 125. [Google Scholar] [CrossRef]
- Sena, T.R.R.; Dourado, S.S.F.; Lima, L.V.; Antoniolli, Â.R. The hearing of rural workers exposed to noise and pesticides. Noise Health 2018, 20, 23–26. [Google Scholar]
- Sena, T.R.; Dourado, S.; Antoniolli, Â. Audição em altas frequências em trabalhadores rurais expostos a agrotóxicos. Ciênc. Saúde Colet. 2019, 24, 3923–3932. [Google Scholar] [CrossRef]
- Mattiazzi, Â.L.; Caye, J.L.; Frank, J.G.; Endruweit Battisti, I.D. Hearing screening and cholinesterase activity among rural workers exposed to pesticides. Rev. Bras. Med. Trab. 2019, 17, 239–246. [Google Scholar] [CrossRef]
- Cazé, A.; Lacerda, A.; Lüders, D.; Conto, J.; Marques, J.; Leroux, T. Perception of the Quality of Life of Tobacco Growers Exposed to Pesticides: Emphasis on Health, Hearing, and Working Conditions. Int. Arch. Otorhinolaryngol. 2019, 23, 50–59. [Google Scholar] [CrossRef]
- Milani, P.; Franca, D.; Balieiro, A.G.; Faez, R.; Milani, P.; Franca, D.; Balieiro, A.G.; Faez, R. Polymers and its applications in agriculture. Polim. E Tecnol. 2017, 27, 256–266. [Google Scholar] [CrossRef]
- Tomiazzi, J.S.; Pereira, D.R.; Judai, M.A.; Antunes, P.A.; Favareto, A.P.A. Performance of machine-learning algorithms to pattern recognition and classification of hearing impairment in Brazilian farmers exposed to pesticide and/or cigarette smoke. Environ. Sci. Pollut. Res. Int. 2019, 26, 6481–6491. [Google Scholar] [CrossRef]
- Muñoz-Quezada, M.T.; Lucero, B.A.; Barr, D.B.; Steenland, K.; Levy, K.; Ryan, P.B.; Iglesias, V.; Alvarado, S.; Concha, C.; Rojas, E.; et al. Neurodevelopmental effects in children associated with exposure to organophosphate pesticides: A systematic review. Neurotoxicology 2013, 39, 158–168. [Google Scholar] [CrossRef]
- Roberts, J.R.; Dawley, E.H.; Reigart, J.R. Children’s low-level pesticide exposure and associations with autism and ADHD: A review. Pediatr. Res. 2019, 85, 234–241. [Google Scholar] [CrossRef]
- Ross, S.M.; McManus, I.C.; Harrison, V.; Mason, O. Neurobehavioral problems following low-level exposure to organophosphate pesticides: A systematic and meta-analytic review. Crit. Rev. Toxicol. 2013, 43, 21–44. [Google Scholar] [CrossRef]
- Mostafalou, S.; Abdollahi, M. Pesticides: An update of human exposure and toxicity. Arch. Toxicol. 2017, 91, 549–599. [Google Scholar] [CrossRef]
- Blair, A.; Ritz, B.; Wesseling, C.; Beane Freeman, L. Pesticides and human health. Occup. Environ. Med. 2015, 72, 81–82. [Google Scholar] [CrossRef]
- Campos, É.; Freire, C.; Novaes, C.O.; Koifman, R.; Koifman, S. Exposure to organochloride pesticides and the cognitive development of children and adolescents living in a contaminated area in brazil|Exposição a pesticidas organoclorados e desenvolvimento cognitivo em crianças e adolescentes residentes em uma area c. Rev. Bras. Saúde Matern. Infant. 2015, 15, 105–120. [Google Scholar] [CrossRef]
- De Azevedo, M.F.A.; Meyer, A. Tremor essencial em guardas de endemias expostos a agrotóxicos: Estudo caso-controle. Cad. Saude Publica 2017, 33, e00194915. [Google Scholar] [CrossRef]
- World Health Organization. The WHO Recommended Classification of Pesticides by Hazard and Guidelines to Classification. Available online: https://apps.who.int/iris/handle/10665/44271 (accessed on 15 September 2021).
- Gunnell, D.; Knipe, D.; Chang, S.-S.; Pearson, M.; Konradsen, F.; Lee, W.J.; Eddleston, M. Prevention of suicide with regulations aimed at restricting access to highly hazardous pesticides: A systematic review of the international evidence. Lancet Glob. Health 2017, 5, e1026–e1037. [Google Scholar] [CrossRef]
- Chowdhury, F.R.; Dewan, G.; Verma, V.R.; Knipe, D.W.; Isha, I.T.; Faiz, M.A.; Gunnell, D.J.; Eddleston, M. Bans of WHO Class I Pesticides in Bangladesh-suicide prevention without hampering agricultural output. Int. J. Epidemiol. 2018, 47, 175–184. [Google Scholar] [CrossRef]
- Cha, E.S.; Chang, S.-S.; Gunnell, D.; Eddleston, M.; Khang, Y.-H.; Lee, W.J. Impact of paraquat regulation on suicide in South Korea. Int. J. Epidemiol. 2016, 45, 470–479. [Google Scholar] [CrossRef]
- Knipe, D.W.; Chang, S.-S.; Dawson, A.; Eddleston, M.; Konradsen, F.; Metcalfe, C.; Gunnell, D. Suicide prevention through means restriction: Impact of the 2008-2011 pesticide restrictions on suicide in Sri Lanka. PLoS ONE 2017, 12, e0172893. [Google Scholar] [CrossRef]
- da Silva, V.D.; de Mello, M.S.; Otero, U.B. Exposure to pesticides and mental disorders in a rural population of Southern Brazil. Neurotoxicology 2016, 56, 7–16. [Google Scholar]
- Gondim, A.P.; Nogueira, R.R.; Lima, J.G.B.; Lima, R.A.C.; Albuquerque, P.L.M.M.; do Veras, M.S.B.; Ferreira, M.A.D. Tentativas de suicídio por exposição a agentes tóxicos registradas em um Centro de Informação e Assistência Toxicológica em Fortaleza, Ceará, 2013|Suicide attempts by exposure to toxic agents registered in a Toxicological Information and Assistance Cent. Epidemiol. Serv. Saúde 2017, 26, 109–119. [Google Scholar] [CrossRef]
- Conti, C.L.; Barbosa, W.M.; Simão, J.B.P.; Álvares-da-Silva, A.M. Pesticide exposure, tobacco use, poor self-perceived health and presence of chronic disease are determinants of depressive symptoms among coffee growers from Southeast Brazil. Psychiatry Res. 2018, 260, 187–192. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopes-Ferreira, M.; Maleski, A.L.A.; Balan-Lima, L.; Bernardo, J.T.G.; Hipolito, L.M.; Seni-Silva, A.C.; Batista-Filho, J.; Falcao, M.A.P.; Lima, C. Impact of Pesticides on Human Health in the Last Six Years in Brazil. Int. J. Environ. Res. Public Health 2022, 19, 3198. https://doi.org/10.3390/ijerph19063198
Lopes-Ferreira M, Maleski ALA, Balan-Lima L, Bernardo JTG, Hipolito LM, Seni-Silva AC, Batista-Filho J, Falcao MAP, Lima C. Impact of Pesticides on Human Health in the Last Six Years in Brazil. International Journal of Environmental Research and Public Health. 2022; 19(6):3198. https://doi.org/10.3390/ijerph19063198
Chicago/Turabian StyleLopes-Ferreira, Monica, Adolfo Luis Almeida Maleski, Leticia Balan-Lima, Jefferson Thiago Gonçalves Bernardo, Lucas Marques Hipolito, Ana Carolina Seni-Silva, Joao Batista-Filho, Maria Alice Pimentel Falcao, and Carla Lima. 2022. "Impact of Pesticides on Human Health in the Last Six Years in Brazil" International Journal of Environmental Research and Public Health 19, no. 6: 3198. https://doi.org/10.3390/ijerph19063198
APA StyleLopes-Ferreira, M., Maleski, A. L. A., Balan-Lima, L., Bernardo, J. T. G., Hipolito, L. M., Seni-Silva, A. C., Batista-Filho, J., Falcao, M. A. P., & Lima, C. (2022). Impact of Pesticides on Human Health in the Last Six Years in Brazil. International Journal of Environmental Research and Public Health, 19(6), 3198. https://doi.org/10.3390/ijerph19063198








