The Transmission, Infection Prevention, and Control during the COVID-19 Pandemic in China: A Retrospective Study
Abstract
:1. Introduction
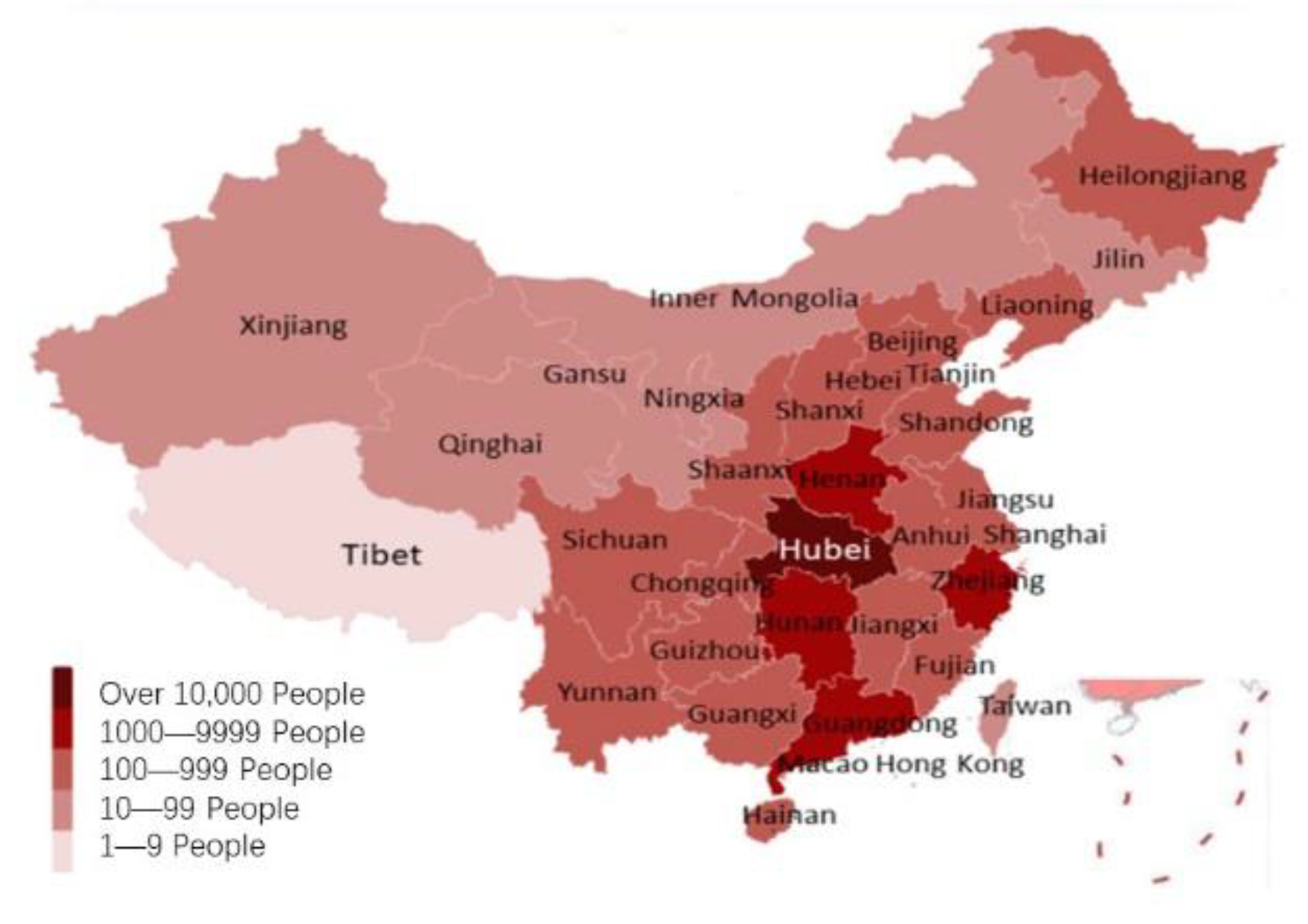
2. Materials and Methods
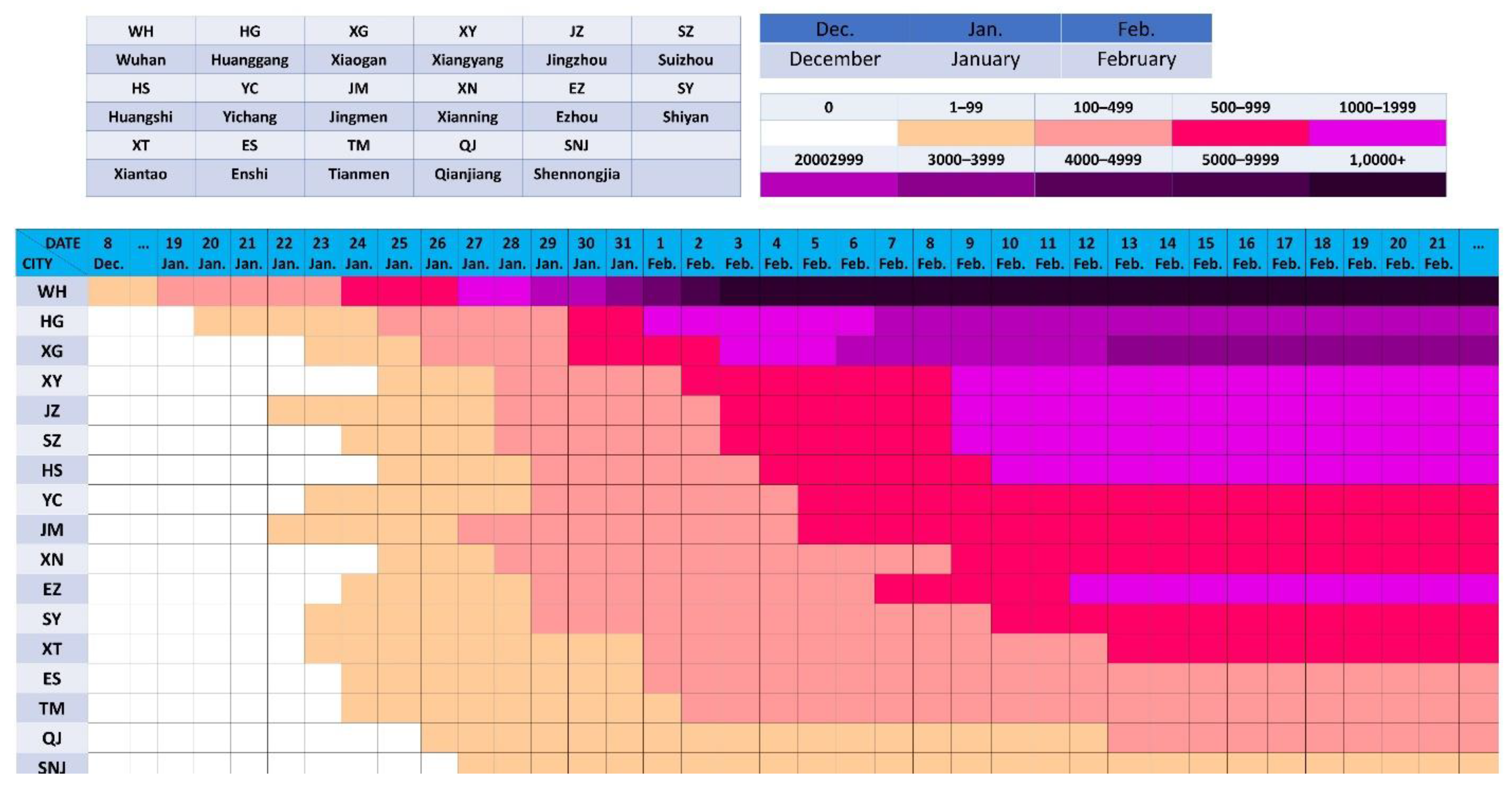
2.1. Routine Reports on the Pandemic
2.2. Transmission Stages
- (A)
- Explosive growth stage: There are new cases every day, and the increase rate is more than 0, i.e., exponential distribution or quasi-exponential distribution.
- (B)
- Stable growth stage: There are new cases every day, and the growth rate tends to 0 or fluctuates around 0.
- (C)
- Attenuated growth stage: There are new cases or zero growth of less than one transmission cycle every day, and the increase rate is negative, showing negative exponential or quasi-negative exponential distribution.
- (D)
- Sporadic growth stage: Zero cases occur in more than one transmission cycle, followed by a continuous period of zero or only sporadic confirmed cases.
2.3. Two Special Reports
2.4. IPC in China
3. Results
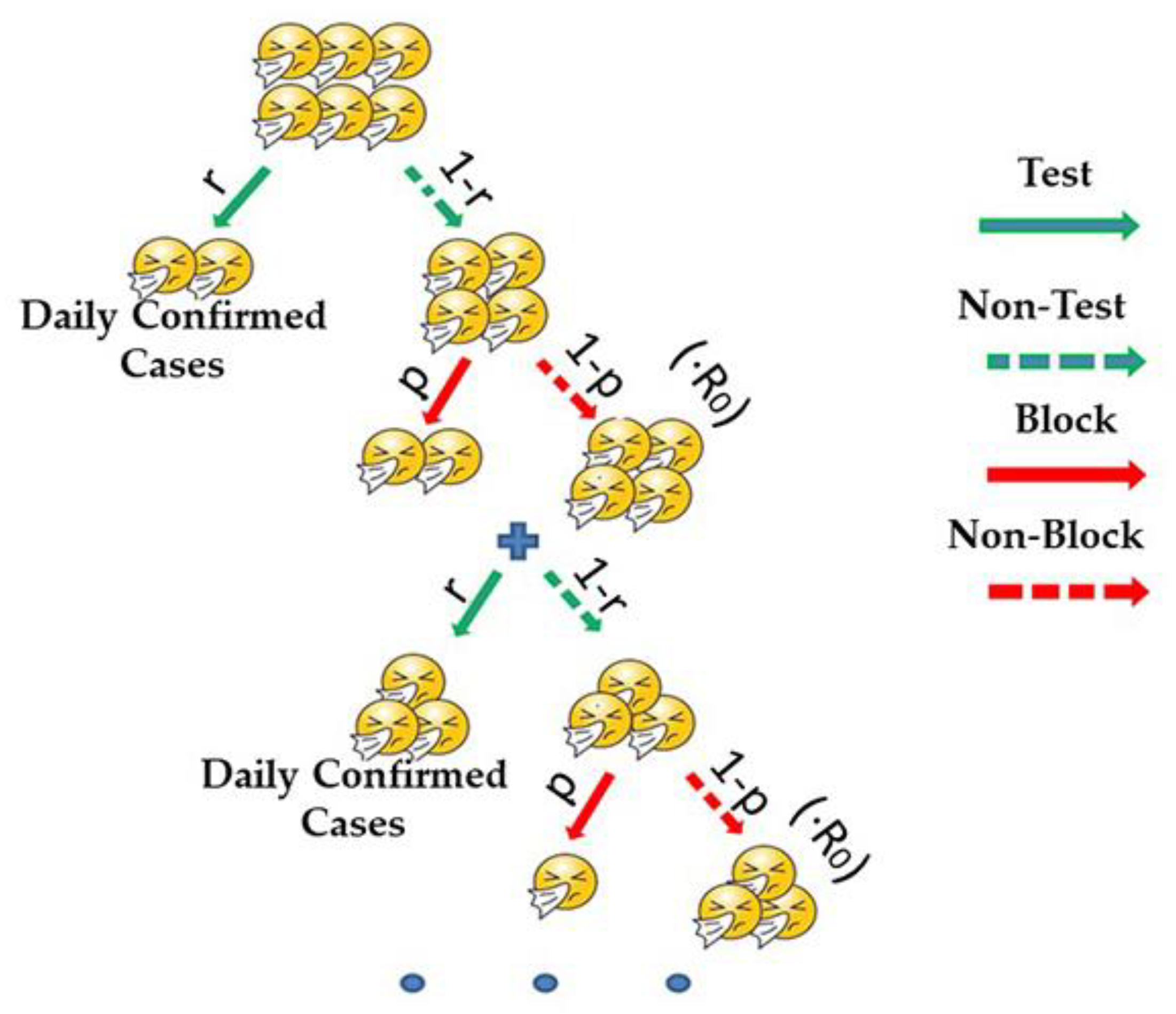
3.1. The Estimation of R0
- (a)
- Data were taken from the beginning of the outbreak.
- (b)
- Confirmed cases were sufficient.
- (c)
- All cases were tested in a timely manner.
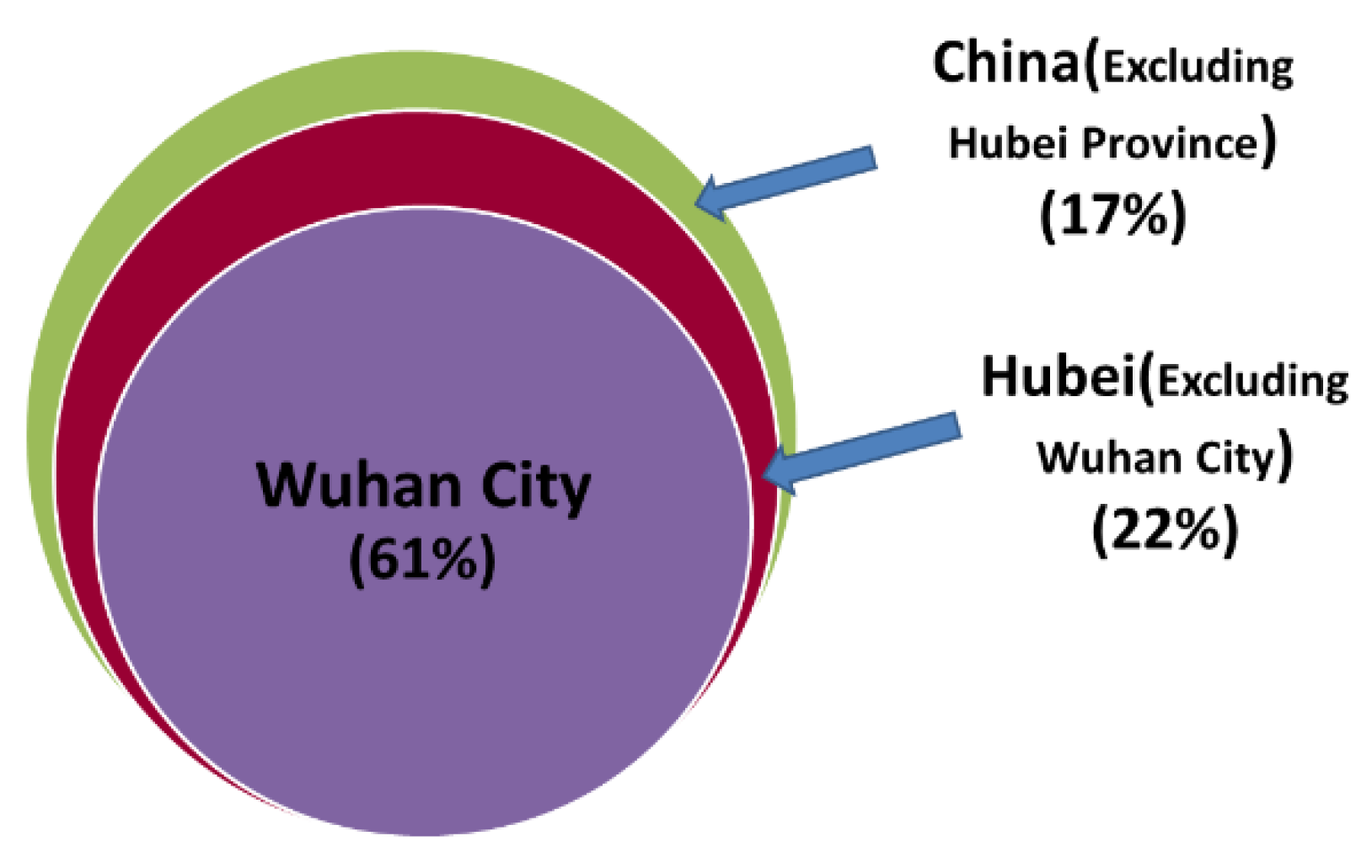
3.2. Study of the Transmission Model in Non-Wuhan Areas
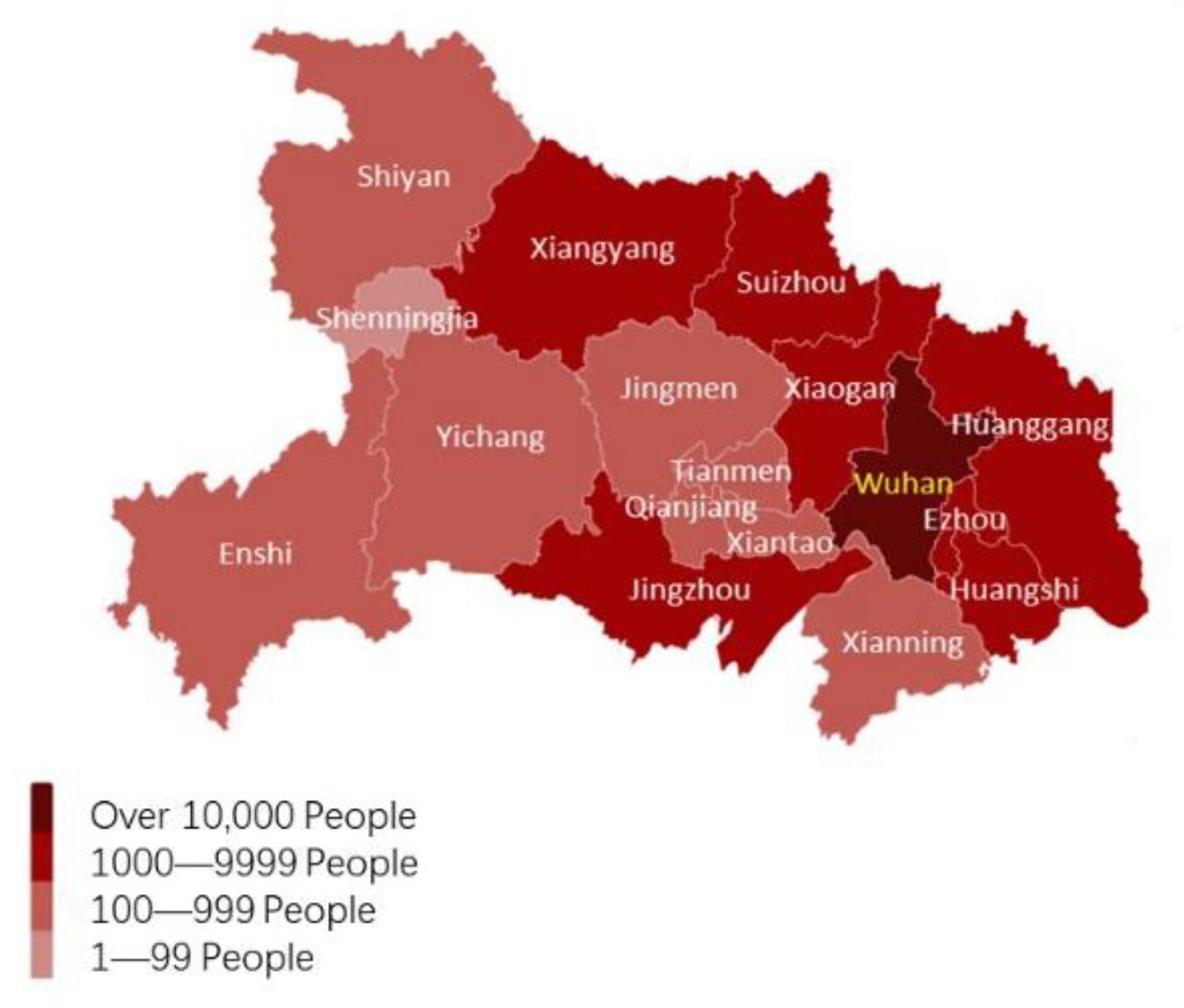
3.3. Study of the Transmission Model in Wuhan
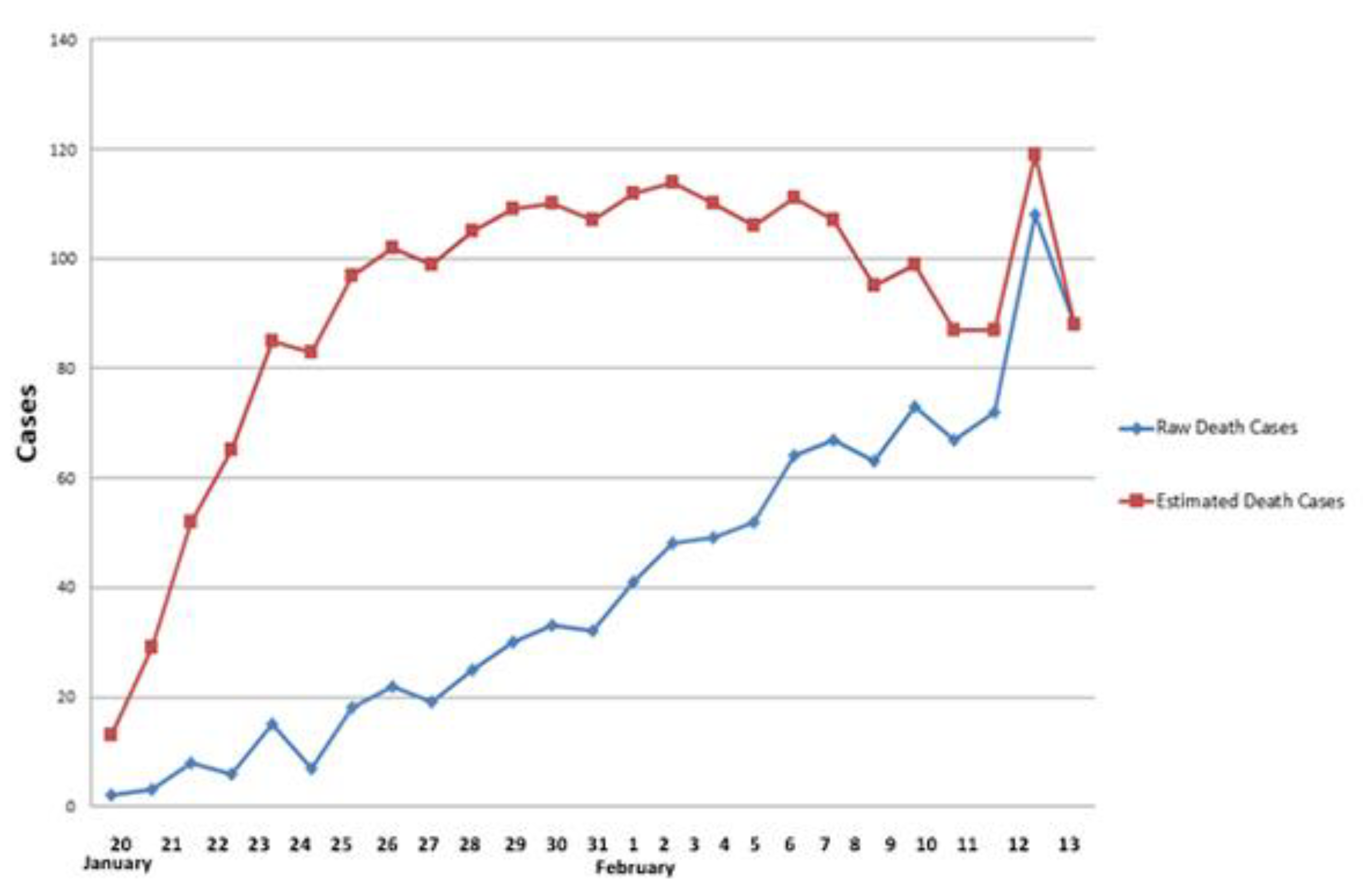
3.4. Revision and Estimate Based on Two Special Reports
3.5. Analysis of the Effect of IPC
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hui, D.S.; Azhar, E.I.; Madani, T.A.; Ntoumi, F.; Kock, R.; Dar, O.; Ippolito, G.; Mchugh, T.D.; Memish, Z.A.; Drosten, C.; et al. The continuing 2019-nCoV pandemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020, 91, 264–266. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR 2020, 69, 343–346. [Google Scholar]
- Rio, C.; Malani, P.N. COVID-19—New Insights on a Rapidly Changing Pandemic. JAMA 2020, 323, 1339–1340. [Google Scholar] [PubMed] [Green Version]
- Tang, Y.-W.; Schmitz, J.E.; Persing, D.H.; Stratton, C.W. The Laboratory Diagnosis of COVID-19 Infection: Current Issues and Challenges. J. Clin. Microbiol. 2020, 58, e00512-20. [Google Scholar] [CrossRef] [Green Version]
- Lu, J.; Gu, J.; Li, K.; Xu, C.; Su, W.; Lai, Z.; Zhou, D.; Yu, C.; Xu, B.; Yang, Z. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. Emerg. Infect. Dis. 2020, 26, 1628–1631. [Google Scholar] [CrossRef]
- Wang, J.; Du, G. COVID-19 may transmit through aerosol. Ir. J. Med Sci. 2020, 189, 1143–1144. [Google Scholar] [CrossRef] [Green Version]
- Zhang, H.; Kang, Z.; Gong, H.; Xu, D.; Wang, J.; Li, Z.; Li, Z.; Cui, X.; Xiao, J.; Zhan, J.; et al. Digestive system is a potential route of COVID-19: An analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut 2020, 69, 1010–1018. [Google Scholar] [CrossRef]
- Tian, Y.; Rong, L.; Nian, W.; He, Y. Review article: Gastrointestinal features in COVID-19 and the possibility of faecal transmis-sion. Aliment. Pharmacol. Ther. 2020, 51, 843–851. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 39, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Leo, D.; Trabucchi, M. COVID-19 and the Fears of Italian Senior Citizens. Int. J. Environ. Res. 2020, 17, 3572. [Google Scholar]
- Chan, J.F.-W.; Zhang, A.J.; Yuan, S.; Poon, V.K.-M.; Chan, C.C.-S.; Lee, A.C.-Y.; Chan, W.-M.; Fan, Z.; Tsoi, H.-W.; Wen, L.; et al. Simulation of the Clinical and Pathological Manifestations of Coronavirus Disease 2019 (COVID-19) in a Golden Syrian Hamster Model: Implications for Disease Pathogenesis and Transmissibility. Clin. Infect. Dis. 2020, 71, 2428–2446. [Google Scholar] [CrossRef] [PubMed]
- Brooke, J.; Jackson, D. Older people and COVID-19: Isolation, risk and ageism. J. Clin. Nurs. 2020, 29, 2044–2046. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Song, C.; Xu, C.; Jin, G.; Chen, Y.; Xu, X.; Ma, H.; Chen, W.; Lin, Y.; Zheng, Y.; et al. Clinical Characteristics of 24 Asymptomatic Infections with COVID-19 Screened among Close Contacts in Nanjing, China; Cold Spring Harbor Laboratory: Cold Spring Harbor, NY, USA, 2020; pp. 1–6. [Google Scholar]
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.Y.; Chen, L.; Wang, M. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA 2020, 323, 1406–1407. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishiura, H.; Kobayashi, T.; Miyama, T.; Suzuki, A.; Jung, S.-M.; Hayashi, K.; Kinoshita, R.; Yang, Y.; Yuan, B.; Akhmetzhanov, A.R.; et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int. J. Infect. Dis. 2020, 94, 154–155. [Google Scholar] [CrossRef]
- Karim, S.S.A.; Karim, O.A. Omicron SARS-CoV-2 variant: A new chapter in the COVID-19 pandemic. Lancet 2021, 398, 2126–2128. [Google Scholar] [CrossRef]
- World Health Organization. Infection Prevention and Control during Health Care When Novel Coronavirus (nCoV) Infection is Suspected. 2020. Available online: https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 (accessed on 26 January 2020).
- Coltart, C.E.M.; Johnson, A.M.; Whitty, C.J.M. Role of healthcare workers in early pandemic spread of Ebola: Policy implica-tions of prophylactic compared to reactive vaccination policy in outbreak prevention and control. BMC Med. 2015, 13, 271. [Google Scholar] [CrossRef] [Green Version]
- Lee, B.Y.; Brown, S.T.; Cooley, P.C.; Zimmerman, R.K.; Wheaton, W.D.; Zimmer, S.M.; Grefenstette, J.J.; Assi, T.M.; Furphy, T.J.; Wagener, D.K.; et al. A Computer Simulation of Employee Vaccination to Mitigate an Influenza Pandemic. Am. J. Prev. Med. 2010, 38, 247–257. [Google Scholar] [CrossRef] [Green Version]
- Niu, Y.; Xu, F. Deciphering the power of isolation in controlling COVID-19 outbreaks. Lancet Glob. Health 2020, 8, e452–e453. [Google Scholar] [CrossRef] [Green Version]
- Hellewell, J.; Abbott, S.; Gimma, A.; Bosse, N.I.; Jarvis, C.I.; Russell, T.W.; Munday, J.D.; Kucharski, A.J.; Edmunds, W.J.; Funk, S.; et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob. Health 2020, 8, e488–e496. [Google Scholar] [CrossRef] [Green Version]
- Berg-Weger, M.; Morley, J.E. Loneliness and Social Isolation in Older Adults during the COVID-19 Pandemic: Implications for Gerontological Social Work. J. Nutr. Health Aging 2020, 24, 456–458. [Google Scholar] [CrossRef] [Green Version]
- Koo, J.R.; Cook, A.R.; Park, M.; Sun, Y.; Sun, H.; Lim, J.T.; Tam, C.; Dickens, B.L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. Lancet Infect. Dis. 2020, 20, 678–688. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Wu, L.; Yuan, F.; Dou, J.; Miao, S. Mass human migration and Beijing’s urban heat island during the Chinese New Year holiday. Sci. Bull. 2015, 60, 1038–1041. [Google Scholar] [CrossRef]
- General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine. Notice on the Issuance of a Program for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infected Pneumonia (Trial Version 2). 2020. Available online: http://www.nhc.gov.cn/xcs/zhengcwj/202001/c67cfe29ecf1470e8c7fc47d3b751e88.shtml (accessed on 22 January 2020).
- General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine. Notice on the Issuance of a Program for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infected Pneumonia (Trial Version 3). 2020. Available online: http://www.nhc.gov.cn/xcs/zhengcwj/202001/470b128513fe46f086d79667db9f76a5.shtml (accessed on 22 January 2020).
- General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine. Notice on the Issuance of a Program for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infected Pneumonia (Trial Version 4). 2020. Available online: http://www.nhc.gov.cn/xcs/zhengcwj/202002/573340613ab243b3a7f61df260551dd4.shtml (accessed on 6 February 2020).
- General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine. Notice on the Issuance of a Program for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infected Pneumonia (Trial Version 5). 2020. Available online: http://www.nhc.gov.cn/xcs/zhengcwj/202002/a5d6f7b8c48c451c87dba14889b30147.shtml (accessed on 21 February 2020).
- General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine. Notice on the Issuance of a Program for the Diagnosis and Treatment of Novel Coronavirus (2019-nCoV) Infected Pneumonia (Trial Version 6). 2020. Available online: http://www.nhc.gov.cn/xcs/zhengcwj/202003/4856d5b0458141fa9f376853224d41d7.shtml (accessed on 7 March 2020).
- Health Commission of Hubei Province. Statement on the Revision of the COVID-19 Pandemic in Hubei Province on April 16, 2020. Available online: http://wjw.Hubei.gov.cn/fbjd/dtyw/202004/t20200417_2233509.shtml (accessed on 17 April 2020).
- China Publishes Timeline on COVID-19 Information Sharing, int’l Cooperation. 6 April 2020. Available online: http://www.gov.cn/xinwen/2020-04/06/content_5499625.htm (accessed on 6 April 2020).
- Liu, W.; Yue, X.-G.; Tchounwou, P.B. Response to the COVID-19 Epidemic: The Chinese Experience and Implications for Other Countries. Int. J. Environ. Res. Public Health 2020, 17, 2304. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Xu, X.; Cai, Y.; Ge, Q.; Zeng, G.; Li, X.; Zhang, W.; Ji, C.; Yang, L. Mining the Characteristics of COVID-19 Patients in China: Analysis of Social Media Posts. J. Med. Internet Res. 2020, 22, e19087. [Google Scholar] [CrossRef]
- Xu, X.; Han, M.; Li, T.; Sun, W.; Wang, D.; Fu, B.; Zhou, Y.; Zheng, X.; Yang, Y.; Li, X.; et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc. Natl. Acad. Sci. USA 2020, 117, 10970–10975. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.; Wang, Z.; Zhao, F.; Yang, Y.; Li, J.; Yuan, J.; Wang, F.; Li, D.; Yang, M.; Xing, L.; et al. Treatment of 5 Critically Ill Patients With COVID-19 With Convalescent Plasma. JAMA: J. Am. Med. Assoc. 2020, 323, 1582. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.-H.; Cai, L.; Cheng, Z.-S.; Cheng, H.; Deng, T.; Fan, Y.-P.; Fang, C.; Huang, D.; Huang, L.-Q.; Huang, Q.; et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil. Med. Res. 2020, 7, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorenzo, G.D.; Trolio, R.D. Coronavirus Disease (COVID-19) in Italy: Analysis of Risk Factors and Proposed Remedial Measures. Front. Med. 2020, 7, 140. [Google Scholar] [CrossRef] [Green Version]
- Delamater, P.L.; Street, E.J.; Leslie, T.F.; Yang, Y.T.; Jacobsen, K.H. Complexity of the Basic Reproduction Number (R0). Emerg. Infect. Dis. 2019, 25, 1–4. [Google Scholar] [CrossRef] [Green Version]
- Kelly, H.A.; Mercer, G.N.; Fielding, J.E.; Dowse, G.K.; Glass, K.; Carcione, D.; Grant, K.A.; Effler, P.V.; Lester, R.A. Pandemic (H1N1) 2009 Influenza Community Transmission Was Established in One Australian State When the Virus Was First Identified in North America. PLoS ONE 2010, 5, e11341. [Google Scholar] [CrossRef] [Green Version]
- Lauer, S.A.; Grantz, K.H.; Bi, Q.; Jones, F.K.; Zheng, Q.; Meredith, H.R.; Azman, A.S.; Reich, N.G.; Lessler, J. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann. Intern. Med. 2020, 172, 577–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, X.; Lau, E.H.Y.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X.; et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020, 26, 672–675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thompson, W.W.; Shay, D.; Weintraub, E.; Brammer, L.; Cox, N.; Anderson, L.J.; Fukuda, K. Mortality Associated with Influenza and Respiratory Syncytial Virus in the United States. JAMA: J. Am. Med. Assoc. 2003, 289, 179–186. [Google Scholar] [CrossRef]
- Sprenger, M.J.W.; Van Naelten, M.A.M.G.; Mulder, P.G.H.; Masurel, N. Influenza mortality and excess deaths in the elderly, 1967–1982. Epidemiol. Infect. 1989, 103, 633–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wong, C.; Chan, K.; Hedley, A.J.; Peiris, J.S.M. Influenza-Associated Mortality in Hong Kong. Clin. Infect. Dis. 2004, 39, 1611–1617. [Google Scholar] [CrossRef] [Green Version]
- Hao, X.; Cheng, S.; Wu, D.; Wu, T.; Lin, X.; Wang, C. Reconstruction of the full transmission dynamics of COVID-19 in Wuhan. Nature 2020, 584, 420–424. [Google Scholar] [CrossRef]
- Liu, L.; Iketani, S.; Guo, Y.; Chan, J.F.; Wang, M.; Liu, L.; Luo, Y.; Chu, H.; Huang, Y.; Nair, M.S.; et al. Striking antibody evasion manifested by the Omicron variant of SARS-CoV-2. Nature 2022, 602, 676–681. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Weekly Epidemiological Update: Omicron Variant of Concern (VOC)–Week 2 (Data as of 20 January 2022) EU/EEA. Available online: https://www.ecdc.europa.eu/en/news-events/weekly-epidemiological-update-omicron-variant-concern-voc-week-2-data-20-january-2022 (accessed on 21 January 2022).
- General Office of National Health Committee. Notice on the Issuance of Testing Technical Specification of Novel Coronavirus (2019-nCoV) for 10 in 1 Mixed Sampling. Available online: http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=fa5057afe4314ef8a9172edd6c65380e (accessed on 19 August 2020).
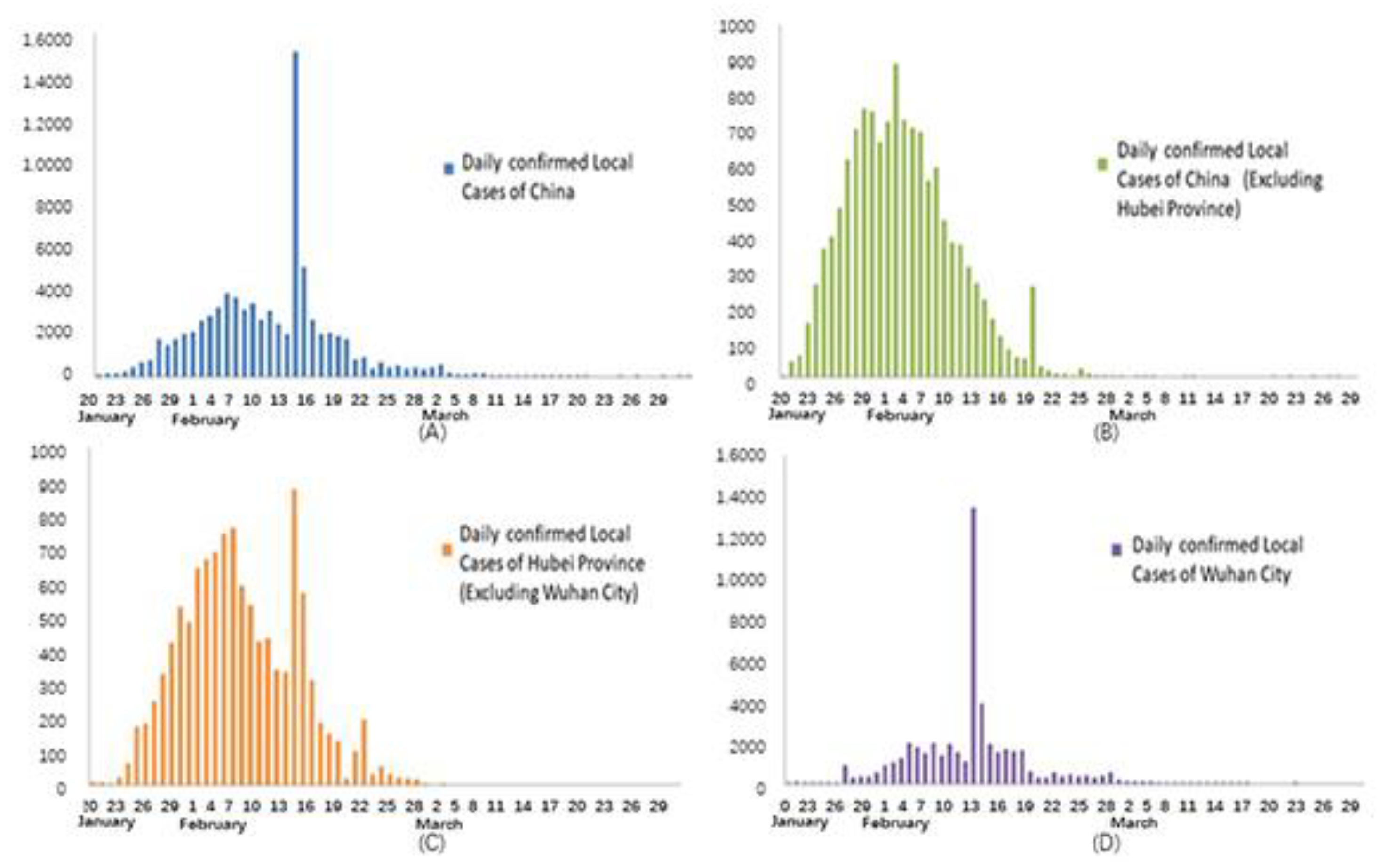





| Stage Area | Explosive Growth Stage | Stable Growth Stage | Attenuated Growth Stage | Sporadic Growth Stage |
|---|---|---|---|---|
| China | December 2019–4 February 2020 | 5 February–18 February 2020 | 19 February 2020– Present | Unknown |
| China (excluding Hubei Province) | 20 January–29 January 2020 | 30 January–8 February 2020 | 9 February–6 March 2020 | 7 March 2020–Present |
| Hubei Province (excluding Wuhan) | 21 January–4 February 2020 | 5 February–18 February 2020 | 19 February–3 March 2020 | 4 March 2020–Present |
| Wuhan | December 2019–2 February 2020 | 3 February–13 February 2020 | 14 February–17 March 2020 | 18 March 2020–Present |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, L.; Welsch, R.E.; Cao, Z. The Transmission, Infection Prevention, and Control during the COVID-19 Pandemic in China: A Retrospective Study. Int. J. Environ. Res. Public Health 2022, 19, 3074. https://doi.org/10.3390/ijerph19053074
Zhang L, Welsch RE, Cao Z. The Transmission, Infection Prevention, and Control during the COVID-19 Pandemic in China: A Retrospective Study. International Journal of Environmental Research and Public Health. 2022; 19(5):3074. https://doi.org/10.3390/ijerph19053074
Chicago/Turabian StyleZhang, Lifeng, Roy E. Welsch, and Zhi Cao. 2022. "The Transmission, Infection Prevention, and Control during the COVID-19 Pandemic in China: A Retrospective Study" International Journal of Environmental Research and Public Health 19, no. 5: 3074. https://doi.org/10.3390/ijerph19053074
APA StyleZhang, L., Welsch, R. E., & Cao, Z. (2022). The Transmission, Infection Prevention, and Control during the COVID-19 Pandemic in China: A Retrospective Study. International Journal of Environmental Research and Public Health, 19(5), 3074. https://doi.org/10.3390/ijerph19053074






