Association of Preterm Birth with Inflammatory Bowel Disease and Salivary Gland Disease: Machine Learning Analysis Using National Health Insurance Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Variables
2.2. Analysis
3. Results
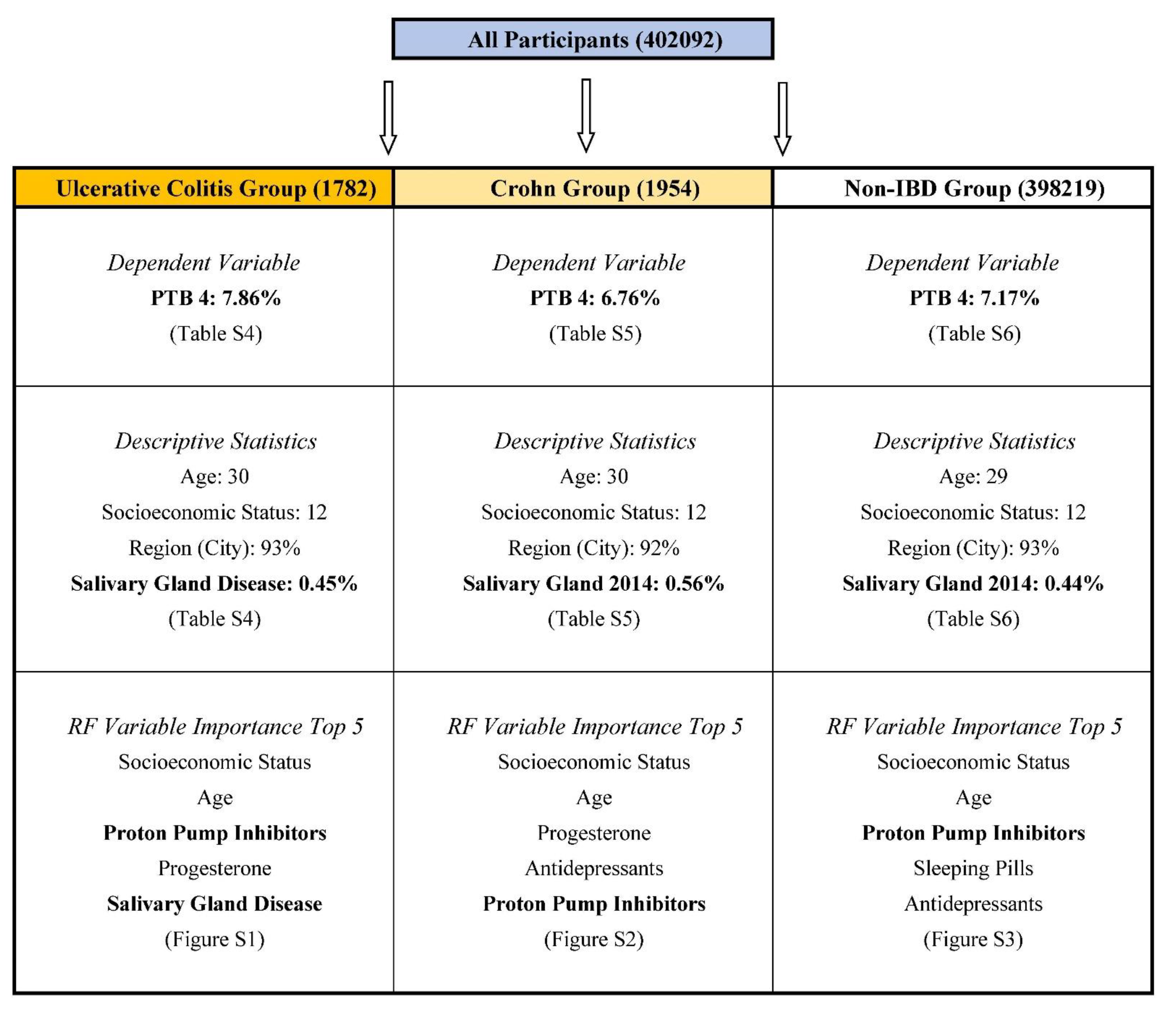
3.1. Descriptive Statistics
3.2. Random Forest Variable Importance
3.3. Logistic Regression Coefficient Estimated
4. Discussion
4.1. Findings of Study
4.2. Contributions of Study
4.3. Limitations of Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, L.; Oza, S.; Hogan, D.; Chu, Y.; Perin, J.; Zhu, J.; Lawn, J.E.; Cousens, S.; Mathers, C.; Black, R.E. Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 2016, 388, 3027–3035. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. News: Preterm Birth. Available online: http://www.who.int/news-room/fact-sheets/detail/preterm-birth (accessed on 1 December 2020).
- Magro Malosso, E.R.; Saccone, G.; Simonetti, B.; Squillante, M.; Berghella, V. US trends in abortion and preterm birth. J. Matern. Fetal Neonatal Med. 2018, 31, 2463–2467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harrison, M.S.; Goldenberg, R.L. Global burden of prematurity. Semin. Fetal Neonatal Med. 2016, 21, 74–79. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 Inflammatory Bowel Disease Collaborators. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2020, 5, 17–30. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.J.; Kim, M.S.; Kim, E.S.; Lee, J.; Lee, J.M.; Choi, H.S.; Kim, C.D. Higher risk of tuberculosis in combination therapy for inflammatory bowel disease: A nationwide population-based cohort study in South Korea. Medicine 2020, 99, e22897. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K.; Ha, H.J.; Oh, S.J.; Kim, J.; Lee, J.K.; Kim, H.; Yoon, S.M.; Kang, S.; Kim, E.S.; Kim, T.O.; et al. Nationwide validation study of diagnostic algorithms for inflammatory bowel disease in Korean National Health Insurance Service database. J. Gastroenterol. Hepatol. 2020, 35, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Y.; Park, S.J.; Jung, E.S.; Jung, S.-A.; Moon, C.M.; Chun, J.; Park, J.J.; Kim, E.S.; Park, Y.; Kim, T.-I.; et al. Genotype-based treatment with thiopurine reduces incidence of myelosuppression in patients with inflammatory bowel diseases. Clin. Gastroenterol. Hepatol. 2020, 18, 2010–2018.e2. [Google Scholar] [CrossRef] [PubMed]
- Goldinova, A.; Tan, C.X.; Bouma, G.; Duijvestein, M.; Brand, H.S.; de Boer, N.K. Oral health and salivary function in ulcerative colitis patients. United Eur. Gastroenterol. J. 2020, 8, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Song, I.S.; Kim, E.S.; Ahn, K.H. Determinants of spontaneous preterm labor and birth including gastroesophageal reflux disease and periodontitis. J. Korean Med. Sci. 2020, 35, e105. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, K.S.; Ahn, K.H. Application of artificial intelligence in early diagnosis of spontaneous preterm labor and birth. Diagnostics 2020, 10, 733. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.-S.; Kim, H.-I.; Kim, H.; Cho, G.; Hong, S.; Oh, M.; Kim, H.; Ahn, K. Association of preterm birth with depression and particulate matter: Machine learning analysis using national health insurance data. Diagnostics 2021, 11, 555. [Google Scholar] [CrossRef] [PubMed]
- Ouh, Y.-T.; Lee, K.-M.; Ahn, K.H.; Hong, S.-C.; Oh, M.-J.; Kim, H.-J.; Han, S.W.; Cho, G.J. Predicting peripartum blood transfusion: Focusing on pre-pregnancy characteristics. BMC Pregnancy Childbirth 2019, 19, 477. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, M.A.; Magee, L.A.; Kenny, L.C.; Karumanchi, S.A.; McCarthy, F.P.; Saito, S.; Hall, D.R.; Warren, C.E.; Adoyi, G.; Ishaku, S.; et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 2018, 72, 24–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baird, D.D.; Narendranathan, M.; Sandler, R.S. Increased risk of preterm birth for women with inflammatory bowel disease. Gastroenterology 1990, 99, 987–994. [Google Scholar] [CrossRef]
- Getahun, D.; Fassett, M.J.; Longstreth, G.F.; Koebnick, C.; Langer-Gould, A.M.; Strickland, D.; Jacobsen, S.J. Association between maternal inflammatory bowel disease and adverse perinatal outcomes. J. Perinatol. 2014, 34, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Wispelwey, B.P.; Sheiner, E. Inflammatory bowel disease and preterm delivery. Arch. Gynecol. Obstet. 2013, 288, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.K.; O’Brien, L.; Einarson, T.R.; Koren, G. The safety of proton pump inhibitors (PPIs) in pregnancy: A meta-analysis. Am. J. Gastroenterol. 2009, 104, 1541–1545. [Google Scholar] [CrossRef] [PubMed]
- Li, C.M.; Zhernakova, A.; Engstrand, L.; Wijmenga, C.; Brusselaers, N. Systematic review with meta-analysis: The risks of proton pump inhibitors during pregnancy. Aliment. Pharmacol. Ther. 2020, 51, 410–420. [Google Scholar] [CrossRef] [PubMed]
- Jackson, M.A.; Goodrich, J.K.; Maxan, M.-E.; Freedberg, D.E.; Abrams, J.A.; Poole, A.; Sutter, J.L.; Welter, D.; Ley, R.; Bell, J.; et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut 2016, 65, 749–756. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Model | Accuracy | AUCa | ||||||
|---|---|---|---|---|---|---|---|---|
| PTB 1 b | PTB 2 | PTB 3 | PTB 4 | PTB 1 | PTB 2 | PTB 3 | PTB 4 | |
| UlcerativeColitis | ||||||||
| Logistic Regression | 0.9238 | 0.9704 | 0.9064 | 0.9140 | 0.5783 | 0.6645 | 0.5334 | 0.5117 |
| Artificial Neural Network | 0.9390 | 0.9586 | 0.9232 | 0.9215 | 0.5000 | 0.5377 | 0.5000 | 0.5000 |
| Random Forest | 0.9390 | 0.9724 | 0.9232 | 0.9215 | 0.5444 | 0.5854 | 0.5783 | 0.5551 |
| Crohn | ||||||||
| Logistic Regression | 0.9478 | 0.9715 | 0.9096 | 0.9216 | 0.5607 | 0.6082 | 0.5142 | 0.5290 |
| Artificial Neural Network | 0.9513 | 0.9715 | 0.9334 | 0.9319 | 0.5000 | 0.6276 | 0.5000 | 0.5000 |
| Random Forest | 0.9513 | 0.9750 | 0.9334 | 0.9319 | 0.5709 | 0.5915 | 0.5946 | 0.5896 |
| Non-IBDc | ||||||||
| Logistic Regression | 0.9450 | 0.9767 | 0.9308 | 0.9283 | 0.5501 | 0.5905 | 0.5516 | 0.5562 |
| Artificial Neural Network | 0.9450 | 0.9767 | 0.9308 | 0.9283 | 0.5350 | 0.5873 | 0.5000 | 0.5558 |
| Random Forest | 0.9450 | 0.9767 | 0.9308 | 0.9283 | 0.5092 | 0.5161 | 0.5110 | 0.5153 |
| Determinant | PTB 1a | PTB 2 | PTB 3 | PTB 4 |
|---|---|---|---|---|
| Age | 1.0098 | 0.9382 | 1.0247 | 0.9892 |
| Antidepressant | 0.7931 | 0.3366 * | 0.9351 | 1.3572 |
| Benzodiazepine | 1.9445 * | 2.3187 | 1.8857 * | 1.6705 * |
| Calcium Channel Blocker | 6.7194 ** | 3.4212 | 2.1308 | 3.297 * |
| Diabetes_2002 | 0.0000 | 6.4689 | 3.0649 | 4.1871 |
| Diabetes_2003 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2004 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2005 | 4.7304 | 1.2090 | 0.0000 | 0.8411 |
| Diabetes_2006 | 2.7319 | 8.602 ** | 2.7566 | 3.9118 * |
| Diabetes_2007 | 1.4627 | 2.8207 | 0.8961 | 1.4748 |
| Diabetes_2008 | 0.8738 | 0.0000 | 0.6597 | 0.5084 |
| Diabetes_2009 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2010 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2011 | 1.7329 | 0.0000 | 0.0000 | 4.5494 * |
| Diabetes_2012 | 1.1298 | 0.0000 | 0.8382 | 0.0000 |
| Diabetes_2013 | 3.4178 * | 0.0000 | 4.0511 * | 2.9241 |
| Diabetes_2014 | 0.0000 | 1.0787 | 0.8086 | 0.1108 |
| Hypertension_2002 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Hypertension_2003 | 0.0000 | 0.0000 | M | 0.0000 |
| Hypertension_2004 | 0.0000 | 27.688 ** | 3.4349 | 3.0957 |
| Hypertension_2005 | 0.0000 | 1.3907 | 0.0000 | 1.4404 |
| Hypertension_2006 | 7.3522 | M | M | 5.5124 |
| Hypertension_2007 | 0.4594 | 0.0000 | 0.0000 | 0.0000 |
| Hypertension_2008 | 35.6946 ** | 69.4079 | M | M |
| Hypertension_2009 | 12.9229 ** | 5.7489 | 4.3275 | 16.7433 ** |
| Hypertension_2010 | 0.0000 | 0.0000 | 0.0000 | 0.1630 |
| Hypertension_2011 | 2.0824 | 0.0000 | 3.2252 | 0.0000 |
| Hypertension_2012 | 4.6089 | 0.0000 | 13.9992 * | 2.1780 |
| Hypertension_2013 | 2.2349 | 0.0000 | 0.2329 | 0.0000 |
| Hypertension_2014 | 1.7902 | 0.0000 | 1.0933 | 0.0000 |
| Myoma Uteri | 0.5859 | 0.4173 | 1.1059 | 0.9930 |
| Nitrate | 40.813 ** | 0.0914 | 8.1989 ** | 7.0922 ** |
| Prior Cone | 8.2979 * | 0.0000 | 13.5855 * | 0.0000 |
| Progesterone | 1.1946 | 0.9761 | 1.2636 | 1.0069 |
| Proton Pump Inhibitor | 1.0064 | 2.3587 ** | 0.9217 | 0.9230 |
| Region (City) in 2014 | 0.8083 | 0.4475 | 0.6042 | 0.6428 |
| Salivary Gland_2002 | 0.2207 | 0.0000 | 0.0000 | 0.5387 |
| Salivary Gland_2003 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2004 | 0.0000 | 0.0601 | 0.0000 | 0.0000 |
| Salivary Gland_2005 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2006 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2007 | 0.0000 | 4.7351 | 0.0000 | 1.4178 |
| Salivary Gland_2008 | 0.0000 | 4.8404 | 0.0000 | 3.1393 |
| Salivary Gland_2009 | 0.0000 | 0.0000 | 1.8714 | 1.9864 |
| Salivary Gland_2010 | 5.8416 | 10.7941 | 2.6198 | 2.9447 |
| Salivary Gland_2011 | 5.8416 | 0.0000 | 4.7588 | 1.4743 |
| Salivary Gland_2012 | 6.8483 | 0.0000 | 0.0000 | 2.1834 |
| Salivary Gland_2013 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2014 | 26.1017 ** | 7.1278 | 3.2970 | 43.5539 ** |
| Sleeping Pills | 0.8594 | 1.0148 | 1.1157 | 0.6741 |
| Socioeconomic Status | 1.0009 | 0.9781 | 0.9951 | 0.9870 |
| Determinant | PTB 1a | PTB 2 | PTB 3 | PTB 4 |
|---|---|---|---|---|
| Age | 0.9612 | 0.9182 | 0.9529 | 0.9483 |
| Antidepressant | 1.4643 | 0.9280 | 1.2048 | 1.0858 |
| Benzodiazepine | 1.1167 | 0.5946 | 1.0122 | 0.9757 |
| Calcium Channel Blocker | 3.1582 | 1.2433 | 5.8533 ** | 2.2185 |
| Diabetes_2002 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2003 | 9.8355 * | 0.0000 | 7.9486 * | 19.4796 ** |
| Diabetes_2004 | 0.0000 | 8.1336 | 3.0526 | 2.9233 |
| Diabetes_2005 | 0.0000 | 5.3495 | 19.0678 ** | 2.3422 |
| Diabetes_2006 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2007 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2008 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2009 | 1.5868 | 8.3228 * | 3.7584 | 0.9326 |
| Diabetes_2010 | 0.0000 | 6.2651 * | 0.0000 | 2.9998 |
| Diabetes_2011 | 10.7725 * | 7.0006 | 14.1682 ** | 3.3617 |
| Diabetes_2012 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2013 | 0.9761 | 0.0000 | 0.0000 | 0.0000 |
| Diabetes_2014 | 0.9794 | 6.1411 ** | 0.6349 | 3.3018 * |
| Hypertension_2002 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Hypertension_2003 | 0.0000 | 4.9828 | 7.5157 | 3.6272 |
| Hypertension_2004 | 0.0000 | 4.1829 | 0.0000 | 1.9322 |
| Hypertension_2005 | 2.0247 | 3.5431 | 1.6596 | 2.5593 |
| Hypertension_2006 | 3.1614 | 0.0379 | 1.8278 | 1.1823 |
| Hypertension_2007 | 0.0000 | 3.3974 | 0.0000 | 0.2921 |
| Hypertension_2008 | 3.4834 | 1.5947 | 0.0000 | 0.5604 |
| Hypertension_2009 | 7.5233 * | 1.8647 | 5.1141 | 4.3998 |
| Hypertension_2010 | 0.0000 | 0.8326 | 0.0000 | 1.8357 |
| Hypertension_2011 | 0.0000 | 8.7583 | 0.0000 | 15.6653 |
| Hypertension_2012 | 0.0000 | 0.9981 | 0.0000 | 0.1479 |
| Hypertension_2013 | 0.0000 | 0.2764 | 0.0000 | 0.6883 |
| Hypertension_2014 | 0.0000 | 4.8163 | 0.5982 | 1.6377 |
| Myoma Uteri | 0.7619 | 1.3336 | 1.5456 | 1.4259 |
| Nitrate | 2.0865 | 0.0000 | 1.8746 | 1.8284 |
| Prior Cone | NA | 0.0000 | NA | 0.0000 |
| Progesterone | 2.0049 ** | 1.8662 | 1.8207 ** | 2.2548 ** |
| Proton Pump Inhibitor | 0.7541 | 1.2072 | 1.1347 | 0.9458 |
| Region (City) in 2014 | 1.2852 | 0.4652 | 0.5451 * | 0.9668 |
| Salivary Gland_2002 | NA | 0.0000 | NA | 0.0000 |
| Salivary Gland_2003 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2004 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2005 | 0.9406 | 0.0000 | 189519030.0742 | 56.6879 ** |
| Salivary Gland_2006 | 2.7456 | 0.0000 | 1.9636 | 1.4216 |
| Salivary Gland_2007 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2008 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2009 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2010 | 0.0000 | 0.0000 | 0.0000 | 11.644 ** |
| Salivary Gland_2011 | 5.7892 | 0.0000 | 3.7886 | 3.9478 |
| Salivary Gland_2012 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2013 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Salivary Gland_2014 | 0.0000 | 0.0000 | 0.0000 | 0.0000 |
| Sleeping Pills | 0.7012 | 1.1153 | 0.9745 | 0.6289 |
| Socioeconomic Status | 1.0056 | 1.0578 | 1.0169 | 0.9893 |
| Determinant | PTB 1a | PTB 2 | PTB 3 | PTB 4 |
|---|---|---|---|---|
| Age | 0.9864 ** | 0.9493 ** | 0.9812 ** | 0.9803 ** |
| Antidepressant | 1.1138 ** | 1.0266 | 1.0942 ** | 1.0697 ** |
| Benzodiazepine | 1.0398 ** | 1.0190 | 1.0379 ** | 1.0369 ** |
| Calcium Channel Blocker | 1.0493 | 1.2628 ** | 1.1522 * | 1.1525 * |
| Diabetes_2002 | 1.1609 | 1.0846 | 1.1331 | 1.0639 |
| Diabetes_2003 | 1.0182 | 1.1752 | 1.1132 | 1.2316 |
| Diabetes_2004 | 1.0051 | 1.3507 | 0.9219 | 1.0140 |
| Diabetes_2005 | 1.0878 | 1.0050 | 1.0904 | 1.1378 |
| Diabetes_2006 | 1.1391 | 1.1016 | 1.1480 | 0.9728 |
| Diabetes_2007 | 1.0264 | 1.0572 | 1.0508 | 1.0159 |
| Diabetes_2008 | 1.1334 | 1.0637 | 1.0121 | 0.9703 |
| Diabetes_2009 | 1.0951 | 1.2045 | 1.0927 | 1.1808 * |
| Diabetes_2010 | 1.1063 | 1.0970 | 1.0954 | 1.1200 |
| Diabetes_2011 | 0.8018 * | 0.9057 | 0.9544 | 0.9632 |
| Diabetes_2012 | 1.1889 * | 1.1856 | 1.1403 | 1.1347 |
| Diabetes_2013 | 0.9975 | 1.0221 | 0.9668 | 1.0445 |
| Diabetes_2014 | 1.1579 ** | 1.7234 ** | 1.4539 ** | 1.3475 ** |
| Hypertension_2002 | 0.5747 ** | 0.7868 | 0.6063 ** | 0.6404 ** |
| Hypertension_2003 | 1.1511 | 0.6140 | 1.2541 | 1.2604 |
| Hypertension_2004 | 0.7358 | 0.8369 | 0.7422 | 0.6295 ** |
| Hypertension_2005 | 1.0448 | 0.9915 | 0.9587 | 1.0616 |
| Hypertension_2006 | 1.4625 ** | 1.1043 | 1.4599 ** | 1.3316 ** |
| Hypertension_2007 | 1.0695 | 1.0451 | 0.9113 | 0.9915 |
| Hypertension_2008 | 1.0781 | 1.2240 | 1.1505 | 1.0758 |
| Hypertension_2009 | 0.9630 | 1.0183 | 1.0273 | 0.8976 |
| Hypertension_2010 | 1.3628 ** | 1.0213 | 1.1403 | 1.317 ** |
| Hypertension_2011 | 0.8217 | 0.8861 | 0.8902 | 1.0492 |
| Hypertension_2012 | 0.9502 | 0.8388 | 0.9512 | 0.9595 |
| Hypertension_2013 | 0.8954 | 1.4962 ** | 1.1539 | 1.1752 |
| Hypertension_2014 | 1.2071 | 1.6816 ** | 1.3486 ** | 1.2994 ** |
| Myoma Uteri | 1.2391 ** | 1.5687 ** | 1.3566 ** | 1.3618 ** |
| Nitrate | 1.0039 | 1.1597 | 1.0187 | 1.1300 |
| Prior Cone | 2.0277 ** | 0.7387 | 1.2255 | 1.3424 |
| Progesterone | 1.2098 ** | 1.5060 ** | 1.2892 ** | 1.3095 ** |
| Proton Pump Inhibitor | 1.0587 ** | 0.9969 | 1.0481 ** | 1.0401 ** |
| Region (City) in 2014 | 1.0875 ** | 0.8727 ** | 1.0417 | 1.0673 ** |
| Salivary Gland_2002 | 1.1365 | 1.9245 ** | 1.0864 | 0.8633 |
| Salivary Gland_2003 | 0.9571 | 0.6351 | 0.9949 | 1.0453 |
| Salivary Gland_2004 | 0.8617 | 0.6470 | 0.5500 ** | 0.5602 ** |
| Salivary Gland_2005 | 1.1713 | 1.1267 | 0.9054 | 1.0701 |
| Salivary Gland_2006 | 1.2927 | 1.1820 | 1.4859 ** | 1.1396 |
| Salivary Gland_2007 | 0.7483 | 0.9624 | 0.7269 * | 0.8904 |
| Salivary Gland_2008 | 1.0409 | 0.9801 | 0.9911 | 1.0023 |
| Salivary Gland_2009 | 1.4634 ** | 1.1146 | 1.3290 ** | 1.2896 ** |
| Salivary Gland_2010 | 0.6818 ** | 0.9678 | 0.9079 | 0.9039 |
| Salivary Gland_2011 | 1.0066 | 0.9210 | 0.9264 | 1.0570 |
| Salivary Gland_2012 | 0.9522 | 0.9528 | 0.9342 | 0.9912 |
| Salivary Gland_2013 | 1.0885 | 0.8104 | 0.8957 | 0.9630 |
| Salivary Gland_2014 | 1.0097 | 0.5847 ** | 0.9340 | 0.9446 |
| Sleeping Pills | 0.9502 | 1.0534 | 0.9805 | 0.9992 |
| Socioeconomic Status | 1.0020 | 1.0043 | 1.0027 * | 1.0022 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.-S.; Kim, E.S.; Song, I.-S.; Kim, H.-I.; Ahn, K.H. Association of Preterm Birth with Inflammatory Bowel Disease and Salivary Gland Disease: Machine Learning Analysis Using National Health Insurance Data. Int. J. Environ. Res. Public Health 2022, 19, 3056. https://doi.org/10.3390/ijerph19053056
Lee K-S, Kim ES, Song I-S, Kim H-I, Ahn KH. Association of Preterm Birth with Inflammatory Bowel Disease and Salivary Gland Disease: Machine Learning Analysis Using National Health Insurance Data. International Journal of Environmental Research and Public Health. 2022; 19(5):3056. https://doi.org/10.3390/ijerph19053056
Chicago/Turabian StyleLee, Kwang-Sig, Eun Sun Kim, In-Seok Song, Hae-In Kim, and Ki Hoon Ahn. 2022. "Association of Preterm Birth with Inflammatory Bowel Disease and Salivary Gland Disease: Machine Learning Analysis Using National Health Insurance Data" International Journal of Environmental Research and Public Health 19, no. 5: 3056. https://doi.org/10.3390/ijerph19053056
APA StyleLee, K.-S., Kim, E. S., Song, I.-S., Kim, H.-I., & Ahn, K. H. (2022). Association of Preterm Birth with Inflammatory Bowel Disease and Salivary Gland Disease: Machine Learning Analysis Using National Health Insurance Data. International Journal of Environmental Research and Public Health, 19(5), 3056. https://doi.org/10.3390/ijerph19053056








