Sex and Economic Disparity Related to Reperfusion Therapies for Patients with Acute Ischemic Stroke in South Korea across a 10-Year Period: A Nationwide Population-Based Study Using the National Health Insurance Database
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Identification of Patients with AIS
2.2. Variables and Statistical Analysis
3. Results
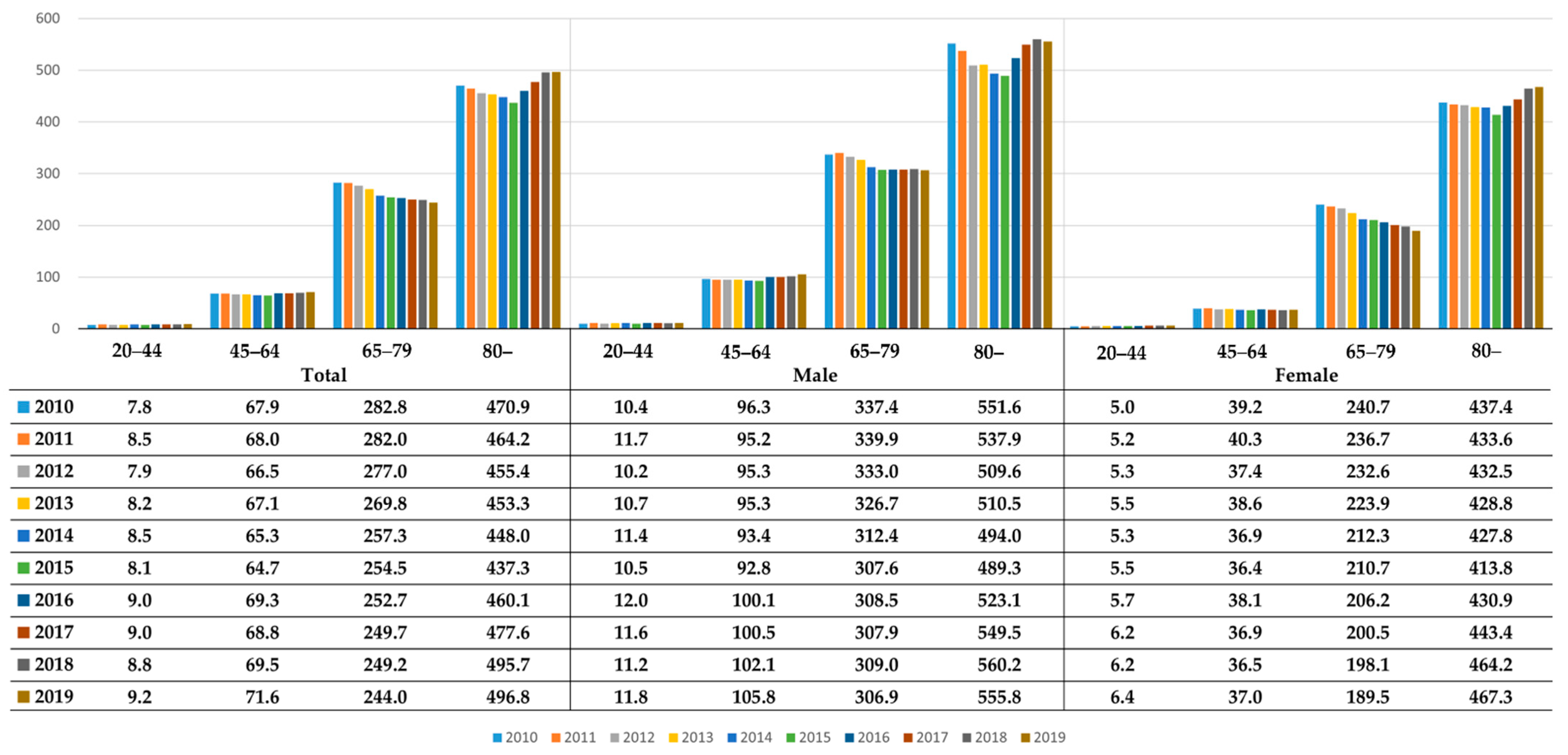
3.1. Demographic Trends for AIS in South Korea from 2010 to 2019
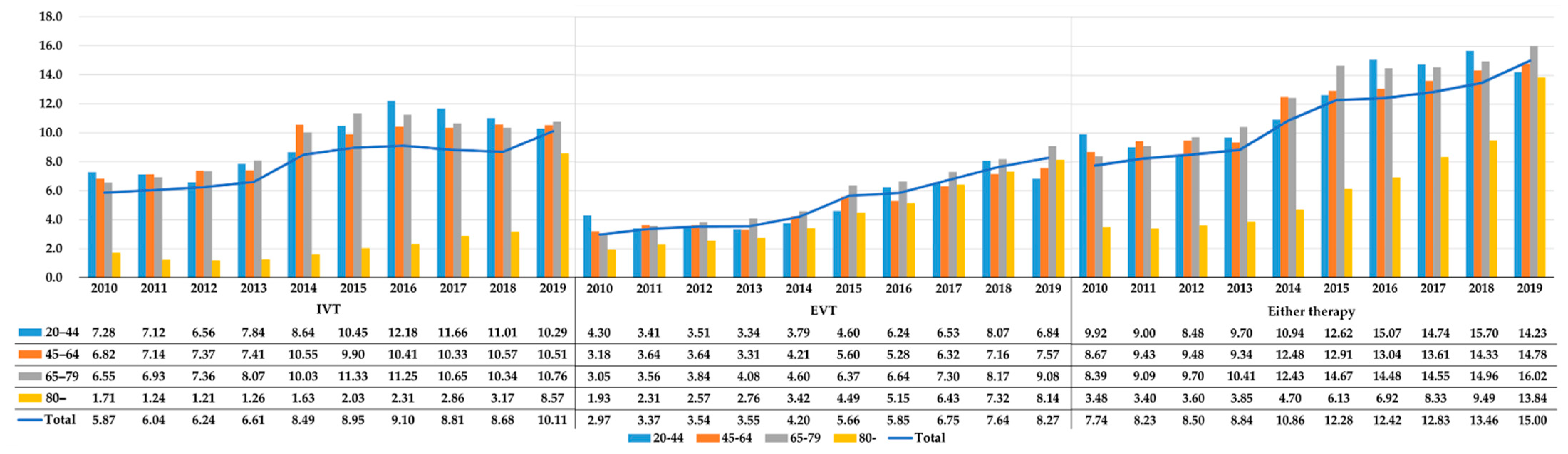
3.2. Reperfusin Therapy Disparity by Age in AIS
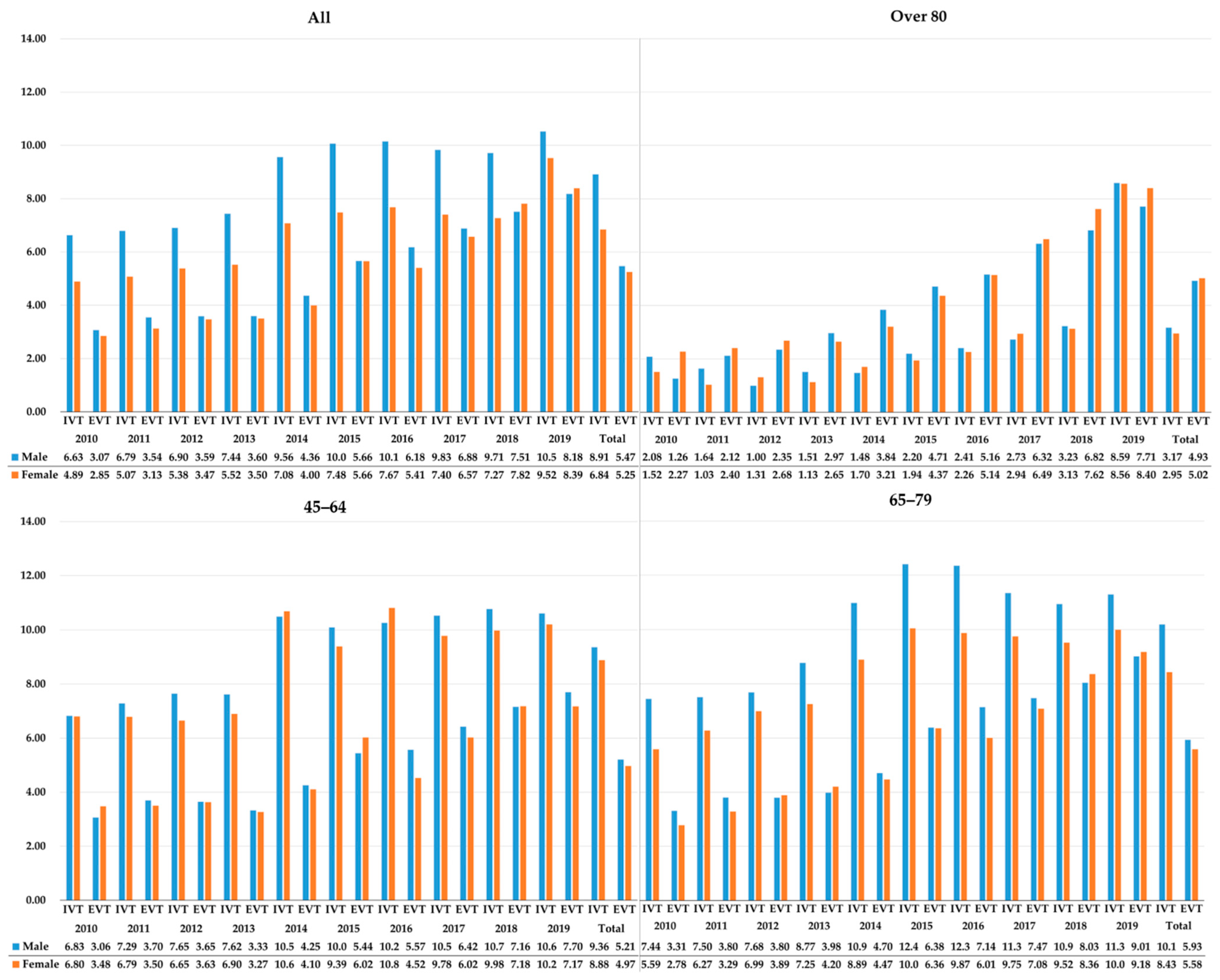
3.3. Sex and Economic Disparity in Reperfusion Therapies for 10 Years
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| ≥80 | <80 | OR (95% CI) | ||
|---|---|---|---|---|
| Total | IVT | 3.03 | 9.33 | 0.30 (0.29–0.32) |
| EVT | 4.99 | 5.48 | 0.91 (0.87–0.94) | |
| Either therapy | 7.17 | 12.33 | 0.55 (0.53–0.57) | |
| Male | IVT | 3.17 | 9.76 | 0.30 (0.28–0.33) |
| EVT | 4.93 | 5.55 | 0.88 (0.83–0.94) | |
| Either therapy | 7.28 | 12.81 | 0.53 (0.51–0.56) | |
| Female | IVT | 2.95 | 8.60 | 0.32 (0.30–0.34) |
| EVT | 5.02 | 5.35 | 0.94 (0.89–0.99) | |
| Either therapy | 7.11 | 11.51 | 0.59 (0.56–0.61) |
References
- Berkowitz, A.L.; Mittal, M.K.; Mclane, H.C.; Shen, G.C.; Muralidharan, R.; Lyons, J.L.; Shinohara, R.T.; Shuaib, A.; Mateen, F.J. Worldwide Reported Use of IV Tissue Plasminogen Activator for Acute Ischemic Stroke. Int. J. Stroke 2014, 9, 349–355. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kang, K.; Kang, J.; Koo, J.; Kim, D.H.; Kim, B.J.; Kim, W.J.; Kim, E.G.; Kim, J.G.; Kim, J.M.; et al. Executive Summary of Stroke Statistics in Korea 2018: A Report from the Epidemiology Research Council of the Korean Stroke Society. J. Stroke 2019, 21, 42–59. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Yan, S.; Song, X.; Gong, Y.; Li, W.; Wang, M.; Yin, X.; Hu, B.; Lu, Z. Intravenous Thrombolytic Therapy for Acute Ischemic Stroke in Hubei, China: A Survey of Thrombolysis Rate and Barriers. BMC Neurol. 2019, 19, 202. [Google Scholar] [CrossRef] [PubMed]
- Reeves, M.; Bhatt, A.; Jajou, P.; Brown, M.; Lisabeth, L. Sex Differences in the Use of Intravenous Rt-Pa Thrombolysis Treatment for Acute Ischemic Stroke: A Meta-Analysis. Stroke 2009, 40, 1743–1749. [Google Scholar] [CrossRef] [PubMed]
- Faigle, R.; Urrutia, V.C.; Cooper, L.A.; Gottesman, R.F. Individual and System Contributions to Race and Sex Disparities in Thrombolysis Use for Stroke Patients in the United States. Stroke 2017, 48, 990–997. [Google Scholar] [CrossRef]
- Kimball, M.M.; Neal, D.; Waters, M.F.; Hoh, B.L. Race and Income Disparity in Ischemic Stroke Care: Nationwide Inpatient Sample Database, 2002 to 2008. J. Stroke Cerebrovasc. Dis. 2014, 23, 17–24. [Google Scholar] [CrossRef]
- Choi, J.C.; Kim, J.G.; Kang, C.H.; Joon, H.; Kang, J.; Lee, S.J.; Park, J.M.; Park, T.H.; Cho, Y.J.; Lee, K.B.; et al. Effect of Transport Time on the Use of Reperfusion Therapy for Patients with Acute Ischemic Stroke in Korea. J. Korean Med. Sci. 2021, 36, e77. [Google Scholar] [CrossRef]
- Gwak, B.C.; Kim, G.Y.; Park, H.J.; Kwon, S.M.; Kim, D.H.; Jeong, J.H.; Cha, J.K. Sex Disparity in Acute Ischemic Stroke Outcomes in Korea. J. Neurocritical Care 2019, 12, 92–97. [Google Scholar] [CrossRef]
- Park, H.; Choi, J. Long-Term Trends in Living Alone among Korean Adults: Age, Gender, and Educational Differences. Demogr. Res. 2015, 32, 1177–1208. [Google Scholar] [CrossRef]
- Cho, K.-H.; Ko, S.-B.; Kim, D.-H.; Park, H.-K.; Cho, A.-H.; Hong, K.-S.; Yu, K.-H.; Heo, J.H.; Kwon, S.-U.; Bae, H.-J.; et al. Focused Update of Korean Clinical Practice Guidelines for the Thrombolysis in Acute Stroke Management. Korean J. Stroke 2012, 14, 95–105. [Google Scholar] [CrossRef][Green Version]
- Kang, D.-H.; Hwang, Y.-H.; Kim, Y.-S.; Park, J.; Kwon, O.; Jung, C. Direct Thrombus Retrieval Using the Reperfusion Catheter of the Penumbra System: Forced-Suction Thrombectomy in Acute Ischemic Stroke. Am. J. Neuroradiol. 2011, 32, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Menon, B.K.; van Zwam, W.H.; Dippel, D.W.J.; Mitchell, P.J.; Demchuk, A.M.; Dávalos, A.; Majoie, C.B.L.M.; van der Lugt, A.; de Miquel, M.A.; et al. Endovascular Thrombectomy after Large-Vessel Ischaemic Stroke: A Meta-Analysis of Individual Patient Data from Five Randomised Trials. Lancet 2016, 387, 1723–1731. [Google Scholar] [CrossRef]
- Hong, K.-S.; Ko, S.-B.; Yu, K.-H.; Jung, C.; Park, S.Q.; Kim, B.M.; Chang, C.-H.; Bae, H.-J.; Heo, J.H.; Oh, C.W.; et al. Update of the Korean Clinical Practice Guidelines for Endovascular Recanalization Therapy in Patients with Acute Ischemic Stroke. J. Stroke 2016, 18, 102–113. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, R.G.; Jadhav, A.P.; Haussen, D.C.; Bonafe, A.; Budzik, R.F.; Bhuva, P.; Yavagal, D.R.; Ribo, M.; Cognard, C.; Hanel, R.A.; et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N. Engl. J. Med. 2018, 378, 11–21. [Google Scholar] [CrossRef]
- Song, Y.J. The South Korean Health Care System. Jpn. Med. Assoc. J. 2009, 52, 206–209. [Google Scholar]
- Bahk, J.; Kang, H.-Y.; Khang, Y.-H. Trends in Life Expectancy among Medical Aid Beneficiaries and National Health Insurance Beneficiaries in Korea between 2004 and 2017. BMC Public Health 2019, 19, 1137. [Google Scholar] [CrossRef]
- Jeong, S.; Cho, S.I.; Kong, S.Y. Long-Term Effect of Income Level on Mortality after Stroke: A Nationwide Cohort Study in South Korea. Int. J. Environ. Res. Public Health 2020, 17, 8348. [Google Scholar] [CrossRef]
- Lattanzi, S.; Coccia, M.; Pulcini, A.; Cagnetti, C.; Galli, F.L.; Villani, L.; Campa, S.; Dobran, M.; Polonara, G.; Ceravolo, M.G.; et al. Endovascular Treatment and Cognitive Outcome after Anterior Circulation Ischemic Stroke. Sci. Rep. 2020, 10, 18524. [Google Scholar] [CrossRef]
- Fredwall, M.; Sternberg, S.; Blackhurst, D.; Lee, A.; Leacock, R.; Nathaniel, T.I. Gender Differences in Exclusion Criteria for Recombinant Tissue-Type Plasminogen Activator. J. Stroke Cerebrovasc. Dis. 2016, 25, 2569–2574. [Google Scholar] [CrossRef]
- Rudd, A.G.; Hoffman, A.; Grant, R.; Campbell, J.T.; Lowe, D.; Intercollegiate Working Party for Stroke. Stroke Thrombolysis in England, Wales and Northern Ireland: How Much Do We Do and How Much Do We Need? J. Neurol. Neurosurg. Psychiatry 2011, 82, 14. [Google Scholar] [CrossRef]
- Reeves, M.J.; Prager, M.; Fang, J.; Stamplecoski, M.; Kapral, M.K. Impact of Living Alone on the Care and Outcomes of Patients with Acute Stroke. Stroke 2014, 45, 3083–3085. [Google Scholar] [CrossRef] [PubMed]
- Foerch, C.; Misselwitz, B.; Humpich, M.; Steinmetz, H.; Neumann-Haefelin, T.; Sitzer, M. Sex Disparity in the Access of Elderly Patients to Acute Stroke Care. Stroke 2007, 38, 2123–2126. [Google Scholar] [CrossRef] [PubMed]
- Berglund, A.; Schenck-Gustafsson, K.; Euler, M. von Sex Differences in the Presentation of Stroke. Maturitas 2017, 99, 47–50. [Google Scholar] [CrossRef]
- Hong, K.-S.; Bang, O.Y.; Kang, D.-W.; Yu, K.-H.; Bae, H.-J.; Lee, J.S.; Heo, J.H.; Kwon, S.U.; Oh, C.W.; Lee, B.-C.; et al. Stroke Statistics in Korea: Part I. Epidemiology and Risk Factors: A Report from the Korean Stroke Society and Clinical Research Center for Stroke. J. Stroke 2013, 15, 2. [Google Scholar] [CrossRef] [PubMed]
- Korea, S. Population and Housing Census. 2019. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1PL1509&conn_path=I2 (accessed on 20 December 2021).
- Mainz, J.; Andersen, G.; Valentin, J.B.; Gude, M.F.; Johnsen, S.P. Disentangling Sex Differences in Use of Reperfusion Therapy in Patients with Acute Ischemic Stroke. Stroke 2020, 51, 2332–2338. [Google Scholar] [CrossRef] [PubMed]
- Bray, B.D.; Paley, L.; Hoffman, A.; James, M.; Gompertz, P.; Wolfe, C.D.A.; Hemingway, H.; Rudd, A.G.; Collaboration, S. Socioeconomic Disparities in First Stroke Incidence, Quality of Care, and Survival: A Nationwide Registry-Based Cohort Study of 44 Million Adults in England. Lancet Public Health 2018, 3, e185–e193. [Google Scholar] [CrossRef]
- Langagergaard, V.; Palnum, K.H.; Mehnert, F.; Ingeman, A.; Krogh, B.R.; Bartels, P.; Johnsen, S.P. Socioeconomic Differences in Quality of Care and Clinical Outcome After Stroke. Stroke 2011, 42, 2896–2902. [Google Scholar] [CrossRef] [PubMed]
- Stecksén, A.; Glader, E.-L.; Asplund, K.; Norrving, B.; Eriksson, M. Education Level and Inequalities in Stroke Reperfusion Therapy. Stroke 2018, 45, 2762–2768. [Google Scholar] [CrossRef]
- Sjölander, M.; Eriksson, M.; Asplund, K.; Norrving, B.; Glader, E.-L. Socioeconomic Inequalities in the Prescription of Oral Anticoagulants in Stroke Patients With Atrial Fibrillation. Stroke 2015, 46, 2220–2225. [Google Scholar] [CrossRef]
- Jaja, B.N.R.; Saposnik, G.; Nisenbaum, R.; Schweizer, T.A.; Reddy, D.; Thorpe, K.E.; Macdonald, R.L. Effect of Socioeconomic Status on Inpatient Mortality and Use of Postacute Care After Subarachnoid Hemorrhage. Stroke 2013, 44, 2842–2847. [Google Scholar] [CrossRef]
- Korea, S. Distribution of Households by Income by Household Characteristics of South Korea. 2020. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1HDAB03&conn_path=I2 (accessed on 20 December 2021).
- Kim, J.; Hwang, Y.-H.; Kim, J.-T.; Choi, N.-C.; Kang, S.-Y.; Cha, J.-K.; Ha, Y.S.; Shin, D.-I.; Kim, S.; Lim, B.-H. Establishment of Government-Initiated Comprehensive Stroke Centers for Acute Ischemic Stroke Management in South Korea. Stroke 2014, 45, 2391–2396. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.-H.; Yang, J.Y.; Cha, J.-K.; Kim, D.-H.; Nah, H.-W.; Kang, M.-J.; Choi, J.-H.; Huh, J.-T. Feasibility of a Pre-Hospital Notification System Using Direct Calls from Paramedics of 119 EMS Ambulances for Acute Stroke Patients: Accuracy of Diagnosis and Efficacy of Shortening of Door-to-Imaging Time. J. Neurocritical. Care 2015, 8, 98–102. [Google Scholar] [CrossRef]
- Kang, J.; Kim, S.-E.; Park, H.-K.; Cho, Y.-J.; Kim, J.Y.; Lee, K.-J.; Park, J.-M.; Park, K.-Y.; Lee, K.B.; Lee, S.J.; et al. Routing to Endovascular Treatment of Ischemic Stroke in Korea: Recognition of Need for Process Improvement. J. Korean Med. Sci. 2020, 35, e347. [Google Scholar] [CrossRef] [PubMed]
| Age | Male | Female | OR (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| IVT | EVT | Either Therapy | IVT | EVT | Either Therapy | IVT | EVT | Either Therapy | |
| 20–44 | 9.48 | 5.28 | 12.24 | 9.05 | 4.70 | 11.79 | 0.95 (0.85–1.07) | 0.89 (0.76–1.03) | 0.96 (0.86–1.06) |
| 45–64 | 9.36 | 5.21 | 12.22 | 8.88 | 4.97 | 11.47 | 0.94 (0.90–0.99) | 0.95 (0.89–1.01) | 0.93 (0.89–0.97) |
| 65–79 | 10.19 | 5.93 | 13.49 | 8.43 | 5.58 | 11.51 | 0.81 (0.78–0.84) | 0.94 (0.90–0.98) | 0.83 (0.81–0.86) |
| 80– | 3.17 | 4.93 | 7.28 | 2.95 | 5.02 | 7.11 | 0.93 (0.85–1.02) | 1.02 (0.95–1.10) | 0.98 (0.92–1.04) |
| Total | 8.91 | 5.47 | 12.1 | 6.84 | 5.25 | 10.14 | 0.75 (0.73–0.77) | 0.96 (0.93–0.99) | 0.82 (0.80–0.84) |
| Medical Aid Beneficiaries | NHI Beneficiaries | OR (95% CI) | ||
|---|---|---|---|---|
| Total | IVT | 7.45 | 8.10 | 0.91 (0.88–0.95) |
| EVT | 5.07 | 5.42 | 0.93 (0.89–0.98) | |
| Either therapy | 10.56 | 11.36 | 0.92 (0.90–0.95) | |
| Male | IVT | 8.10 | 9.01 | 0.89 (0.84–0.94) |
| EVT | 5.21 | 5.50 | 0.94 (0.88–1.01) | |
| Either therapy | 11.24 | 12.21 | 0.91 (0.87–0.95) | |
| Female | IVT | 6.75 | 6.86 | 0.98 (0.92–1.05) |
| EVT | 4.92 | 5.30 | 0.92 (0.86–0.99) | |
| Either therapy | 9.83 | 10.19 | 0.96 (0.91–1.01) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moon, J.; Shin, J.; Lee, J.; Jeong, H.J.; Kim, H.; An, J.; Jo, S.H.; Ko, K.-P.; Choi, J. Sex and Economic Disparity Related to Reperfusion Therapies for Patients with Acute Ischemic Stroke in South Korea across a 10-Year Period: A Nationwide Population-Based Study Using the National Health Insurance Database. Int. J. Environ. Res. Public Health 2022, 19, 3050. https://doi.org/10.3390/ijerph19053050
Moon J, Shin J, Lee J, Jeong HJ, Kim H, An J, Jo SH, Ko K-P, Choi J. Sex and Economic Disparity Related to Reperfusion Therapies for Patients with Acute Ischemic Stroke in South Korea across a 10-Year Period: A Nationwide Population-Based Study Using the National Health Insurance Database. International Journal of Environmental Research and Public Health. 2022; 19(5):3050. https://doi.org/10.3390/ijerph19053050
Chicago/Turabian StyleMoon, Jusun, Jinyoung Shin, Jeehye Lee, Ho Jin Jeong, Hyeongsu Kim, Jaehyeong An, Sung Hyun Jo, Kwang-Pil Ko, and Jeoungbin Choi. 2022. "Sex and Economic Disparity Related to Reperfusion Therapies for Patients with Acute Ischemic Stroke in South Korea across a 10-Year Period: A Nationwide Population-Based Study Using the National Health Insurance Database" International Journal of Environmental Research and Public Health 19, no. 5: 3050. https://doi.org/10.3390/ijerph19053050
APA StyleMoon, J., Shin, J., Lee, J., Jeong, H. J., Kim, H., An, J., Jo, S. H., Ko, K.-P., & Choi, J. (2022). Sex and Economic Disparity Related to Reperfusion Therapies for Patients with Acute Ischemic Stroke in South Korea across a 10-Year Period: A Nationwide Population-Based Study Using the National Health Insurance Database. International Journal of Environmental Research and Public Health, 19(5), 3050. https://doi.org/10.3390/ijerph19053050









