Prevalence and Numbers of Diabetes Patients with Elevated BMI in China: Evidence from a Nationally Representative Cross-Sectional Study
Abstract
:1. Introduction
2. Methods
2.1. Data Sources and Study Population
2.2. Blood Glucose Measurement and Definition
2.3. Elevated BMI
2.4. Statistical Analysis
3. Results
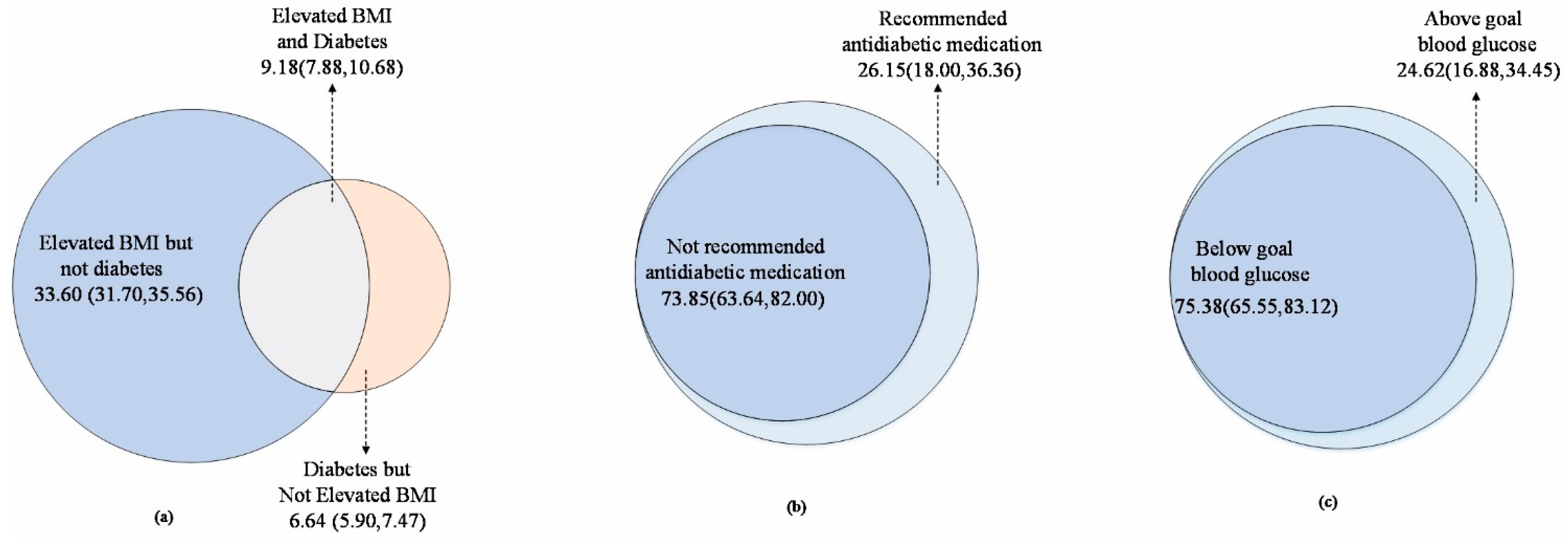
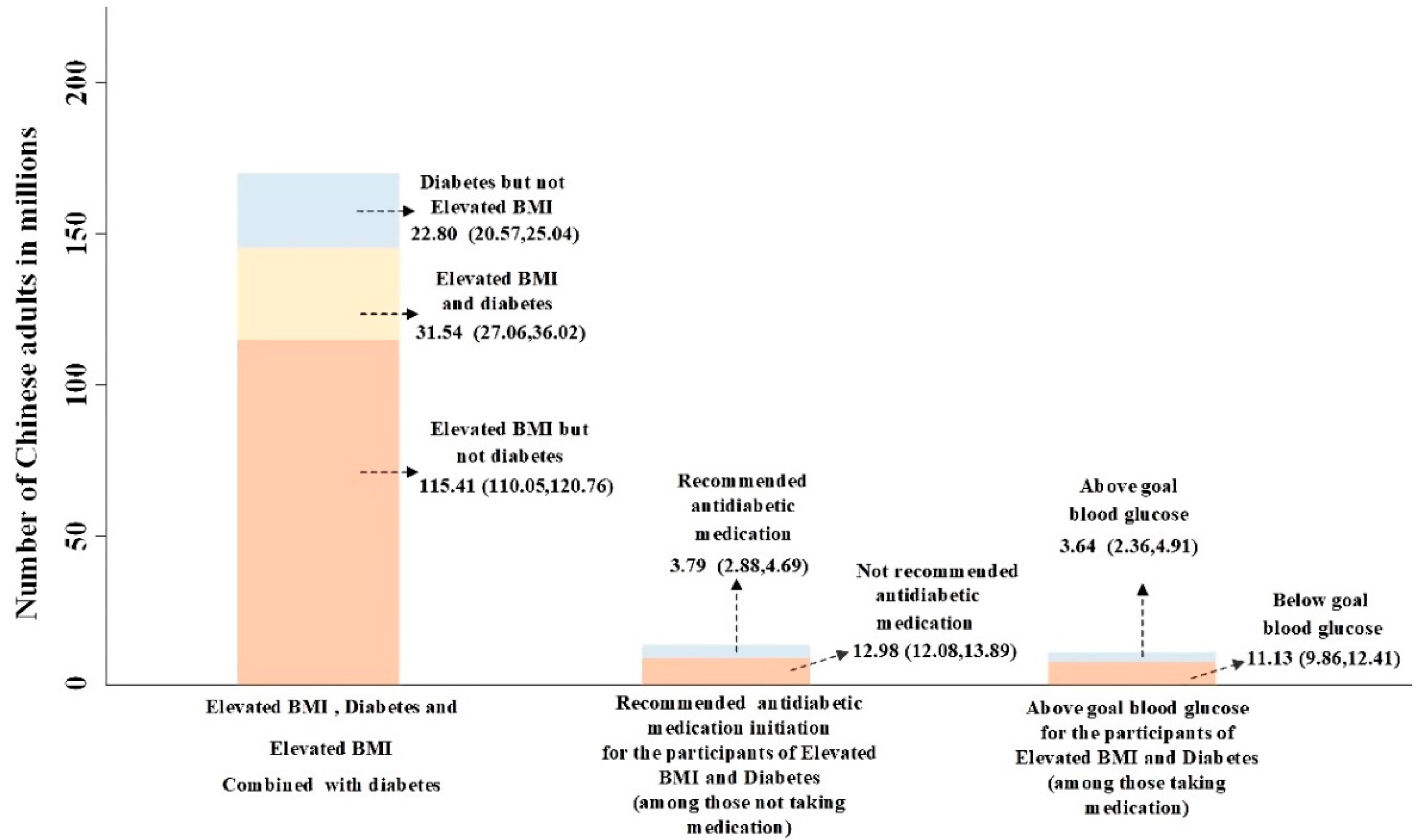
3.1. Prevalence and Numbers of Diabetes Patients with Elevated BMI, Recommended to Initiate Antidiabetic Medication, or above Goal Blood Glucose
3.2. Baseline Information of Participants Included in CHARLS 2011–2012 Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Description | Percentage (95% CI), % | Numbers (95% CI), Millions | |
|---|---|---|---|
| Total | Recommend antidiabetic medication | 26.15 | 3.79 |
| (18.00,36.36) | (2.88,4.69) | ||
| Not recommend antidiabetic medication | 73.84 | 12.98 | |
| (63.64,82.00) | (12.07,13.89) | ||
| Above goal blood glucose | 24.62 | 3.64 | |
| (16.88,34.45) | (2.36,4.91) | ||
| Below goal blood glucose | 75.38 | 11.13 | |
| (65.55,83.12) | (9.86,12.41) | ||
| Age < 65 | Recommend antidiabetic medication | 24.99 | 2.79 |
| (18.15,33.36) | (2.06,3.51) | ||
| Not recommend antidiabetic medication | 75.01 | 10.03 | |
| (66.46,81.85) | (9.30,10.75) | ||
| Above goal blood glucose | 26.39 | 2.84 | |
| (16.35,39.68) | (1.59,4.09) | ||
| Below goal blood glucose | 73.61 | 7.92 | |
| (60.32,83.65) | (6.67,9.16) | ||
| Age ≥ 65 | Recommend antidiabetic medication | 30.43 | 1.00 |
| (11.87,58.69) | (0.45,1.54) | ||
| Not recommend antidiabetic medication | 69.57 | 2.95 | |
| (41.31,88.13) | (2.41,3.50) | ||
| Above goal blood glucose | 19.90 | 0.80 | |
| (11.43,32.35) | (0.38,1.22) | ||
| Below goal blood glucose | 80.10 | 3.22 | |
| (67.65,88.87) | (2.79,3.64) | ||
| Male | Recommend antidiabetic medication | 23.17 | 1.55 |
| (14.09,35.66) | (0.95,2.15) | ||
| Not recommend antidiabetic medication | 76.83 | 6.12 | |
| (64.34,85.91) | (5.52,6.72) | ||
| Above goal blood glucose | 36.54 | 1.92 | |
| (24.34,50.74) | (1.25,2.59) | ||
| Below goal blood glucose | 63.46 | 3.34 | |
| (49.26,75.66) | (2.66,4.01) | ||
| Female | Recommend antidiabetic medication | 28.63 | 2.24 |
| (18.31,41.32) | (1.55,2.92) | ||
| Not recommend antidiabetic medication | 71.37 | 6.86 | |
| (58.68,81.39) | (6.18,7.55) | ||
| Above goal blood glucose | 18.05 | 1.72 | |
| (10.73,28.75) | (0.87,2.57) | ||
| Below goal blood glucose | 81.95 | 7.80 | |
| (71.25,89.27) | (6.95,8.65) | ||
| Continuous Variables | Obs | Mean | Std. Dev. | Min | Max |
| Age (years) | 9410 | 59.53 | 9.41 | 45.00 | 95.75 |
| Blood Glucose (mmol/L) | 9410 | 6.14 | 2.10 | 1.00 | 40.15 |
| HbA1c (%) | 9410 | 5.27 | 0.82 | 3.50 | 14.50 |
| BMI (Kg/m2) | 9410 | 23.52 | 3.95 | 5.39 | 71.29 |
| SBP (mmHg) | 9410 | 130.62 | 21.52 | 73.00 | 233.3 |
| DBP (mmHg) | 9410 | 75.77 | 12.13 | 35.33 | 142.7 |
| Categorical variables | Freq. | Percent (%) | Cum. (%) | ||
| Age (years) | |||||
| 45–59 | 5264 | 55.94 | 55.94 | ||
| 60–74 | 3468 | 36.85 | 92.79 | ||
| ≥75 | 678 | 7.21 | 100.00 | ||
| Gender | |||||
| Male | 4377 | 46.51 | 46.51 | ||
| Female | 5033 | 53.49 | 100.00 | ||
| BMI | |||||
| Normal BMI | 5562 | 59.11 | 59.11 | ||
| Elevated BMI | 3828 | 40.89 | 100.00 | ||
| Diabetes | |||||
| Yes | 1436 | 15.26 | 15.26 | ||
| No | 7974 | 84.74 | 100.00 | ||
| Educational level | |||||
| Illiterate | 2746 | 29.18 | 29.18 | ||
| Primary school | 3883 | 41.26 | 70.45 | ||
| Middle/High school | 2658 | 28.25 | 98.69 | ||
| Bachelor or above | 123 | 1.31 | 100.00 | ||
| Marital status | |||||
| Never | 66 | 0.70 | 0.70 | ||
| Married | 9344 | 99.30 | 100.00 | ||
| Registered residence | |||||
| Rural | 7795 | 82.86 | 82.86 | ||
| Urban | 1612 | 17.14 | 100.00 | ||
| Smoking status | |||||
| Non-smoker | 6543 | 69.53 | 69.53 | ||
| Smoker | 2867 | 30.47 | 100.00 | ||
| Drinking status | |||||
| Non-drinker | 6325 | 67.27 | 67.27 | ||
| Drinker | 3077 | 32.73 | 100.00 | ||
References
- Kharroubi, A.T.; Darwish, H.M. Diabetes mellitus: The epidemic of the century. World J. Diabetes 2015, 6, 850–867. [Google Scholar] [CrossRef] [PubMed]
- Deshpande, A.D.; Harris-Hayes, M.; Schootman, M. Epidemiology of diabetes and diabetes-related complications. Phys. Ther. 2008, 88, 1254–1264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacob, K.S. Non-communicable diseases from a public health perspective. Natl. Med. J. India 2019, 32, 193–196. [Google Scholar] [CrossRef]
- King, H.; Aubert, R.E.; Herman, W.H. Global burden of diabetes, 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care 1998, 21, 1414–1431. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.; Gao, P.; Zhang, M.; Huang, Z.; Zhang, D.; Deng, Q.; Li, Y.; Zhao, Z.; Qin, X.; Jin, D.; et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017, 317, 2515–2523. [Google Scholar] [CrossRef]
- Ma, S.; Xi, B.; Yang, L.; Sun, J.; Zhao, M.; Bovet, P. Trends in the prevalence of overweight, obesity, and abdominal obesity among Chinese adults between 1993 and 2015. Int. J. Obes. 2021, 45, 427–437. [Google Scholar] [CrossRef]
- Eckel, R.H.; Kahn, S.E.; Ferrannini, E.; Goldfine, A.B.; Nathan, D.M.; Schwartz, M.W.; Smith, R.J.; Smith, S.R. Obesity and type 2 diabetes: What can be unified and what needs to be individualized? J. Clin. Endocrinol. Metab. 2011, 96, 1654–1663. [Google Scholar] [CrossRef] [Green Version]
- Hossain, P.; Kawar, B.; El-Nahas, M. Obesity and diabetes in the developing world--a growing challenge. N. Engl. J. Med. 2007, 356, 213–215. [Google Scholar] [CrossRef] [Green Version]
- Mokdad, A.H.; Ford, E.S.; Bowman, B.A.; Dietz, W.H.; Vinicor, F.; Bales, V.S.; Marks, J.S. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 2003, 289, 76–79. [Google Scholar] [CrossRef]
- Xu, Y.; Wang, L.; He, J.; Bi, Y.; Li, M.; Wang, T.; Wang, L.; Jiang, Y.; Dai, M.; Lu, J.; et al. Prevalence and control of diabetes in Chinese adults. JAMA 2013, 310, 948–959. [Google Scholar] [CrossRef] [PubMed]
- Pan, X.R.; Yang, W.Y.; Li, G.W.; Liu, J. Prevalence of diabetes and its risk factors in China, 1994. National Diabetes Prevention and Control Cooperative Group. Diabetes Care 1997, 20, 1664–1669. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Lu, J.; Weng, J.; Jia, W.; Ji, L.; Xiao, J.; Shan, Z.; Liu, J.; Tian, H.; Ji, Q.; et al. Prevalence of diabetes among men and women in China. N. Engl. J. Med. 2010, 362, 1090–1101. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Xu, Q.; Han, L.; Wu, T.; Shi, X.; Ye, L.; Yao, G.; Li, X. Using real-world data to estimate the changing trends in the prevalence and incidence of type 2 diabetes mellitus in Xiamen of China from 2014 to 2019. BMC Endocr. Disord. 2021, 21, 92. [Google Scholar] [CrossRef]
- Zhu, S.; Hu, J.; McCoy, T.P.; Li, G.; Zhu, J.; Lei, M.; Yuan, J.; Peng, J.; Kong, L. Socioeconomic Status and the Prevalence of Type 2 Diabetes Among Adults in Northwest China. Diabetes Educ. 2015, 41, 599–608. [Google Scholar] [CrossRef]
- Chen, X.; Smith, J.; Strauss, J.; Wang, Y.; Zhao, Y. China Health and Retirement Longitudinal Study (CHARLS). In Encyclopedia of Geropsychology; Springer: Singapore, 2014; Volume 43, pp. 61–68. [Google Scholar] [CrossRef] [Green Version]
- Society, C.D. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin. J. Diabetes Mellitus 2021, 13, 317–411. [Google Scholar]
- He, W.; Li, Q.; Yang, M.; Jiao, J.; Ma, X.; Zhou, Y.; Song, A.; Heymsfield, S.B.; Zhang, S.; Zhu, S. Lower BMI cutoffs to define overweight and obesity in China. Obesity 2015, 23, 684–691. [Google Scholar] [CrossRef]
- Hou, X.; Lu, J.; Weng, J.; Ji, L.; Shan, Z.; Liu, J.; Tian, H.; Ji, Q.; Zhu, D.; Ge, J.; et al. Impact of waist circumference and body mass index on risk of cardiometabolic disorder and cardiovascular disease in Chinese adults: A national diabetes and metabolic disorders survey. PLoS ONE 2013, 8, e57319. [Google Scholar] [CrossRef]
- Abdullah, A.; Peeters, A.; de Courten, M.; Stoelwinder, J. The magnitude of association between overweight and obesity and the risk of diabetes: A meta-analysis of prospective cohort studies. Diabetes Res. Clin. Pract. 2010, 89, 309–319. [Google Scholar] [CrossRef]
- Al-Goblan, A.S.; Al-Alfi, M.A.; Khan, M.Z. Mechanism linking diabetes mellitus and obesity. Diabetes Metab. Syndr. Obes. 2014, 7, 587–591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leggio, M.; Lombardi, M.; Caldarone, E.; Severi, P.; D’Emidio, S.; Armeni, M.; Bravi, V.; Bendini, M.G.; Mazza, A. The relationship between obesity and hypertension: An updated comprehensive overview on vicious twins. Hypertens. Res. 2017, 40, 947–963. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, A.D.; Skerrett, P.J.; Manson, J.E. Obesity, diabetes, and coronary risk in women. J. Cardiovasc. Risk 2002, 9, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Huang, X.; You, C.; Li, J.; Hong, K.; Li, P.; Wu, Y.; Wu, Q.; Wang, Z.; Gao, R.; et al. Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. PLoS ONE 2017, 12, e0183934. [Google Scholar] [CrossRef] [PubMed]
- Ren, Q.; Wang, L.; Peng, D.; Guo, Y. Influence of awareness on the behaviors of Chinese adults with diabetes mellitus. Beijing Da Xue Xue Bao Yi Xue Ban 2017, 49, 451–454. [Google Scholar]
- Sapkota, R.P.; Upadhyaya, T.; Gurung, G.; Parker, M.; Raman, R.; Pardhan, S. Need to improve awareness and treatment compliance in high-risk patients for diabetic complications in Nepal. BMJ Open Diabetes Res. Care 2018, 6, e000525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Description | Normal 1 | Isolated Elevated BMI | Isolated Diabetes | Elevated BMI and Diabetes | ||||
|---|---|---|---|---|---|---|---|---|
| Percentage | Numbers (95% CI) | Percentage | Numbers (95% CI) | Percentage | Numbers (95% CI) | Percentage | Numbers (95% CI) | |
| Total | 50.57 | 173.68 | 33.60 | 115.41 | 6.64 | 22.80 | 9.18 | 31.54 |
| (48.30,52.84) | (168.07,179.30) | (31.70,35.56) | (110.05,120.76) | (5.90,7.47) | (20.57,25.04) | (7.88,10.68) | (27.06,36.02) | |
| Age < 65 | 48.66 | 121.50 | 36.31 | 90.65 | 5.59 | 13.96 | 9.44 | 23.57 |
| (46.23,51.10) | (116.62,126.38) | (34.52,38.13) | (86.02,95.28) | (4.91,6.36) | (12.34,15.58) | (7.86,11.31) | (19.43,27.71) | |
| Age ≥ 65 | 55.66 | 52.18 | 26.41 | 24.76 | 9.44 | 8.85 | 8.50 | 7.97 |
| (52.01,59.24) | (49.38,54.98) | (22.84,30.32) | 21.97,27.54) | (7.86,11.30) | (7.33,10.36) | (6.84,10.52) | (6.27,9.67) | |
| Male | 57.11 | 93.26 | 27.93 | 45.62 | 7.04 | 11.50 | 7.92 | 12.93 |
| (54.58,59.61) | (89.53,96.98) | (25.88,30.09) | (42.32,48.92) | (6.02,8.22) | (9.81,13.19) | (6.71,9.32) | (10.97,14.88) | |
| Female | 44.65 | 80.42 | 38.74 | 69.79 | 6.28 | 11.30 | 10.33 | 18.61 |
| (41.73,47.60) | (76.56,84.29) | (36.23,41.32) | (65.70,73.88) | (5.42,7.25) | (9.85,12.76) | (8.38,12.67) | (14.62,22.61) | |
| Normal | Isolated Elevated BMI | Isolated Diabetes | Elevated BMI and Diabetes | Total | p Value | |
|---|---|---|---|---|---|---|
| Number of participants | 4904 | 3070 | 658 | 778 | 9410 | |
| Age, mean ± SD | 60.47 ± 9.71 | 57.54 ± 8.73 | 62.19 ± 9.55 | 59.17 ± 8.48 | 59.53 ± 9.41 | <0.001 |
| Age | <0.001 | |||||
| 45–59 | 2582 (52.65) | 1943 (63.29) | 300 (45.59) | 439 (56.43) | 5264 (55.94) | |
| 60–74 | 1884 (38.42) | 1002 (32.64) | 279 (42.40) | 303 (38.95) | 3468 (36.85) | |
| ≥75 | 438 (8.93) | 125 (4.07) | 79 (12.01) | 36 (4.63) | 678 (7.21) | |
| Gender | <0.001 | |||||
| Male | 2576 (52.53) | 1157 (37.69) | 318 (48.33) | 326 (41.90) | 4377 (46.51) | |
| Female | 2328 (47.47) | 1913 (62.31) | 340 (51.67) | 452 (58.10) | 5033 (53.49) | |
| Educational level | <0.001 | |||||
| Illiterate | 1513 (30.85) | 814 (26.51) | 213 (32.37) | 206 (26.48) | 2746 (29.18) | |
| Primary school | 2095 (42.72) | 1198 (39.02) | 291 (44.22) | 299 (38.48) | 3883 (41.26) | |
| Middle/High school | 1248 (25.45) | 1004 (32.70) | 146 (22.19) | 260 (33.42) | 2658 (28.25) | |
| Bachelor or above | 48 (0.98) | 54 (1.76) | 8 (1.22) | 13 (1.67) | 123 (1.31) | |
| Marital status | ||||||
| Never | 51 (1.04) | 8 (0.26) | 5 (0.76) | 2 (0.26) | 66 (0.70) | <0.001 |
| Married | 4853 (98.96) | 3062 (99.74) | 653 (99.24) | 776 (99.74) | 9344 (99.30) | |
| Registered residence | <0.001 | |||||
| Rural | 4268 (87.05) | 2405 (78.39) | 548 (83.28) | 574 (73.78) | 7795 (82.86) | |
| Urban | 635 (12.95) | 663 (21.61) | 110 (16.72) | 204 (26.22) | 1612 (17.14) | |
| Smoking status | <0.001 | |||||
| Non-smoker | 3078 (62.77) | 2424 (78.96) | 438 (66.57) | 603 (77.51) | 6543 (69.53) | |
| Smoker | 1826 (37.23) | 646 (21.04) | 220 (33.43) | 175 (22.49) | 2867 (30.47) | |
| Drinking status | <0.001 | |||||
| Non-drinker | 3138 (64.07) | 2198 (71.60) | 430 (65.55) | 558 (71.85) | 6325 (67.27) | |
| Drinker | 1760 (35.93) | 872 (28.40) | 226 (34.45) | 219 (28.15) | 3077 (32.73) | |
| FBG (fasting blood-glucose), mean ± SD | 5.56 ± 0.78 | 5.71 ± 0.77 | 9.17 ± 4.30 | 8.99 ± 3.62 | 6.14 ± 2.11 | <0.001 |
| Glycated hemoglobin, mean ± SD | 5.08 ± 0.39 | 5.14 ± 0.40 | 6.13 ± 1.66 | 6.31 ± 1.50 | 5.27 ± 0.82 | <0.001 |
| BMI, mean ± SD | 20.97 ± 2.01 | 26.99 ± 3.00 | 21.32 ± 1.94 | 27.71 ± 3.85 | 23.52 ± 3.95 | <0.001 |
| SBP, mean ± SD | 127.46 ± 21.25 | 133.51 ± 21.21 | 131.83 ± 21.38 | 138.16 ± 21.00 | 130.62 ± 21.52 | <0.001 |
| DBP, mean ± SD | 73.49 ± 11.82 | 78.63 ± 12.14 | 74.42 ± 10.88 | 80.03 ± 11.51 | 75.77 ± 12.13 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Liang, X.; Zhou, Z.; Hou, Z.; Yang, J.; Gao, Y.; Yang, C.; Chen, T.; Li, C. Prevalence and Numbers of Diabetes Patients with Elevated BMI in China: Evidence from a Nationally Representative Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2989. https://doi.org/10.3390/ijerph19052989
Wang Y, Liang X, Zhou Z, Hou Z, Yang J, Gao Y, Yang C, Chen T, Li C. Prevalence and Numbers of Diabetes Patients with Elevated BMI in China: Evidence from a Nationally Representative Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(5):2989. https://doi.org/10.3390/ijerph19052989
Chicago/Turabian StyleWang, Yongjuan, Xuanyi Liang, Ziai Zhou, Zeyi Hou, Jinyu Yang, Yanpei Gao, Chenyu Yang, Tao Chen, and Chao Li. 2022. "Prevalence and Numbers of Diabetes Patients with Elevated BMI in China: Evidence from a Nationally Representative Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 5: 2989. https://doi.org/10.3390/ijerph19052989
APA StyleWang, Y., Liang, X., Zhou, Z., Hou, Z., Yang, J., Gao, Y., Yang, C., Chen, T., & Li, C. (2022). Prevalence and Numbers of Diabetes Patients with Elevated BMI in China: Evidence from a Nationally Representative Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(5), 2989. https://doi.org/10.3390/ijerph19052989






