Effects of a Worksite-Based Self-Management Program in Traditional Retail Market Workers: Longitudinal Associations with Metabolic Parameters
Abstract
1. Introduction
2. Materials and Methods
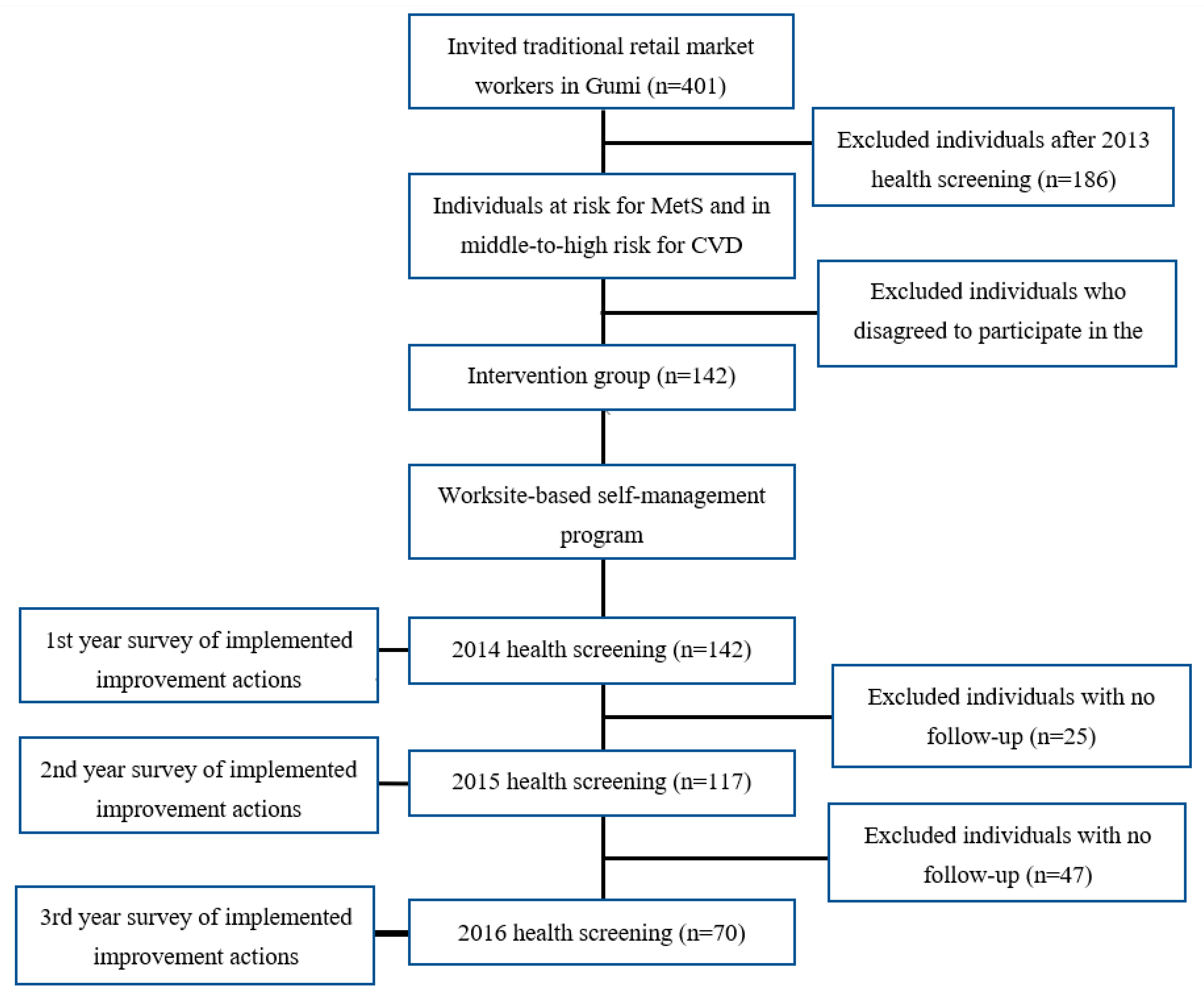
2.1. Participants and Procedures
2.2. Development of an Intervention Program
2.2.1. Development of the Action Checklist
2.2.2. Counseling and Setting Action Plans
2.3. Measurements
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. General Characteristics
3.2. Proposed and Implemented Action Plans during 3 Years
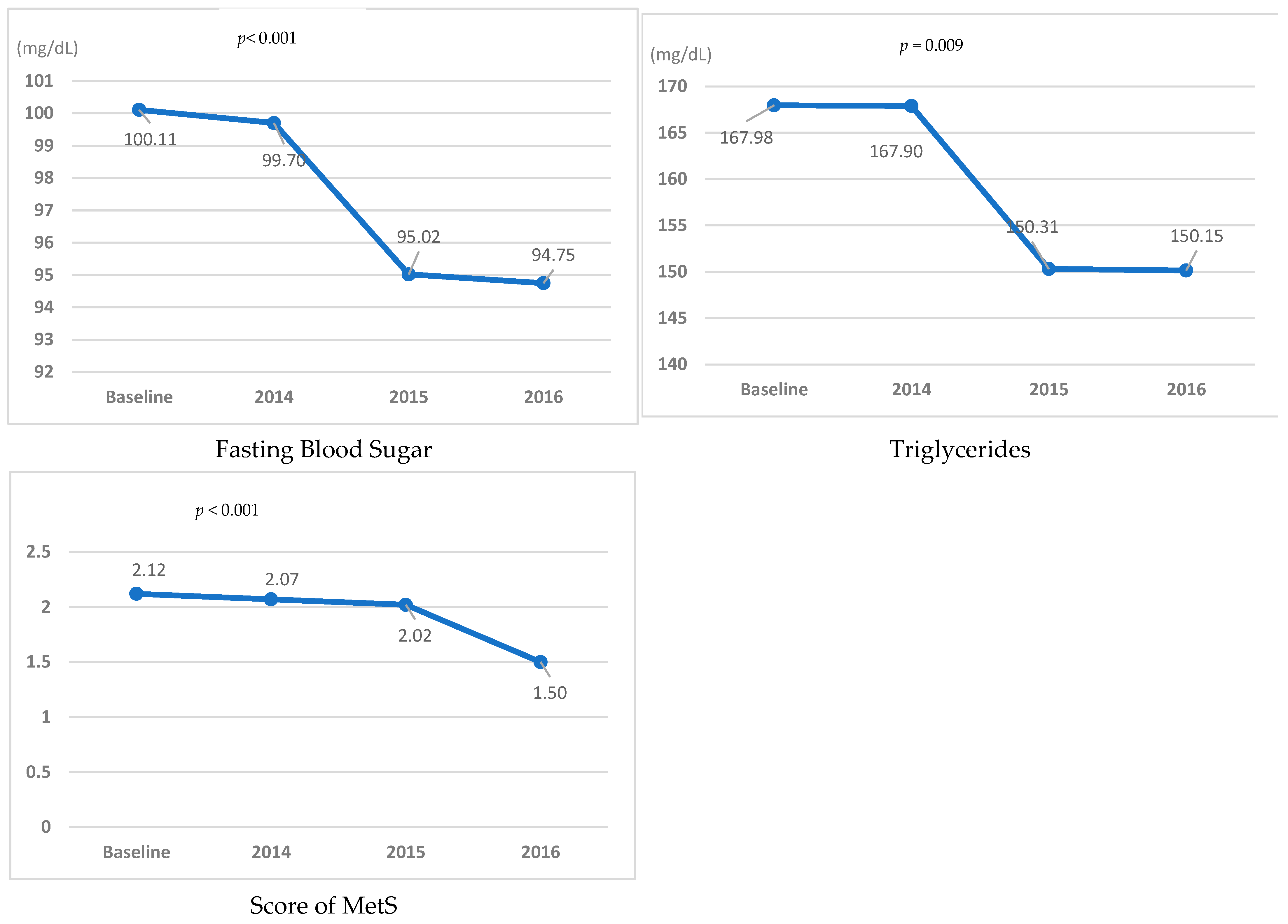
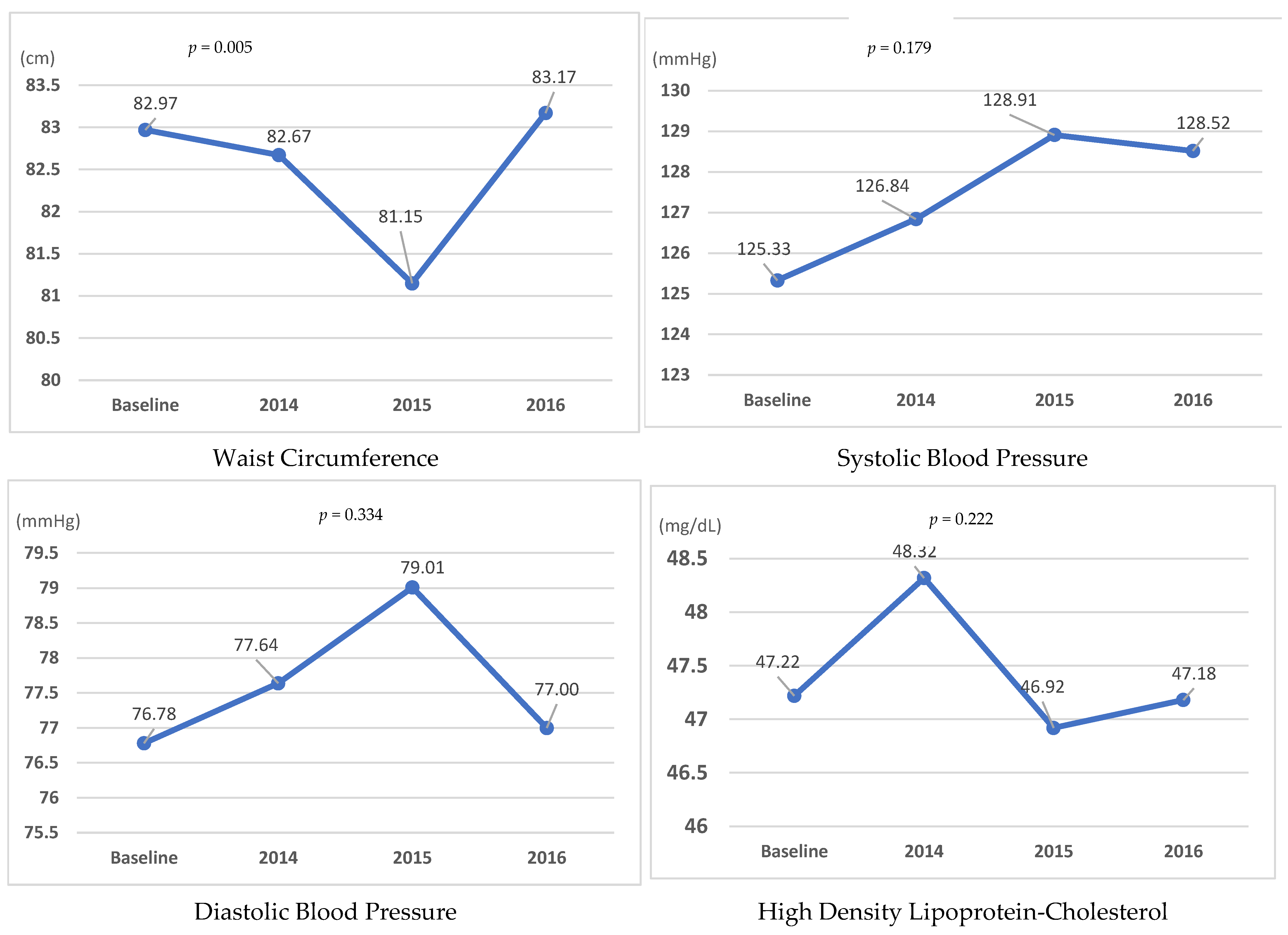
3.3. Follow-Up Results of MetS Risk Components during 3 Years of Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arbel, Y.; Havakuk, O.; Halkin, A.; Revivo, M.; Berliner, S.; Herz, I.; Weiss-Meilik, A.; Sagy, Y.; Keren, G.; Finkelstein, A.; et al. Relation of metabolic syndrome with long-term mortality in acute and stable coronary disease. Am. J. Cardiol. 2015, 115, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Saboya, P.P.; Bodanese, L.C.; Zimmermann, P.R.; Gustavo, A.D.; Macagnan, F.E.; Feoli, A.P.; Oliveira, M.D. Lifestyle intervention on metabolic syndrome and its impact on quality of life: A randomized controlled trial. Arq. Bras. Cardiol. 2017, 108, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Huh, J.H.; Kang, D.R.; Jang, J.Y.; Shin, J.H.; Kim, J.Y.; Choi, S.; Cho, E.J.; Park, J.S.; Sohn, I.S.; Jo, S.H.; et al. Metabolic syndrome epidemic among Korean adults: Korean survey of Cardiometabolic Syndrome. Atherosclerosis 2018, 277, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.Y.; Yun, J.M. Analysis of the association between health-related and work-related factors among workers and metabolic syndrome using data from the Korean National Health and Nutrition Examination Survey (2016). Nutr. Res. Pract. 2019, 13, 444–451. [Google Scholar] [CrossRef]
- Kwon, L.S.; Lee, S.H. Environmental factors related factors of metabolic syndrome of Korean adults-focused on the fourth term Korea National Health & Nutrition Examination Survey. J. Korean Soc. Living Environ. Syst. 2012, 19, 676–688. [Google Scholar]
- Ryu, J.Y.; Hong, S.; Kim, C.H.; Lee, S.; Kim, J.H.; Lee, J.T.; Kim, D.H. Prevalence of the metabolic syndrome among Korean workers by occupational group: Fifth Korean National Health and Nutrition Examination Survey (KNHANES) 2010. Ann. Occup. Environ. Med. 2013, 25, 13. [Google Scholar] [CrossRef]
- Hozawa, H.; Takeuchi, A.; Oguma, Y. Prevalence of metabolic syndrome and lifestyle characteristics by business type among Japanese workers in small- and medium-sized enterprises. Keio J. Med. 2019, 68, 54–67. [Google Scholar] [CrossRef]
- Statistics Korea. Micro-Enterprises Statistics Survey; 2019. Available online: https://www.narastat.kr/metasvc/index.do?confmNo=920022&inputYear=2019 (accessed on 28 December 2021).
- Small Enterprise and Market Service (SEMAS). Report of Actual Condition of the Traditional Market and Store. 2017. Available online: https://www.sbiz.or.kr/sup/custcenter/report/1201860_1716.jsp (accessed on 2 August 2021).
- Lee, S.J.; Park, S.K.; Kim, H.C.; Lee, D.H.; Kim, G.W.; Leem, J.H.; Jeon, S.H.; Heo, Y.S. The relationship between job stress and the will to cease tobacco smoking for small and medium scale industry male workers. Korean J. Occup. Environ. Med. 2012, 24, 33–39. [Google Scholar] [CrossRef]
- Alexander, J.A.; Hearld, L.R.; Mittler, J.N.; Harvey, J. Patient-physician role relationships and patient activation among individuals with chronic illness. Health Sev. Res. 2012, 47, 1201–1223. [Google Scholar] [CrossRef]
- Kazutaka, K. Roles of participatory action-oriented programs in promoting safety and health at work. Safe Health Work 2012, 3, 155–165. [Google Scholar] [CrossRef]
- Warner, G.; Packer, T.; Villeneuve, M.; Audulv, A.; Versnel, J. A systematic review of the effectiveness of stroke self-management programs for improving function and participation outcomes: Self-management programs for stroke survivors. Disabil. Rehabil. 2015, 37, 2141–2163. [Google Scholar] [CrossRef] [PubMed]
- Augustine, H.; Roberts, J.; Packer, T. Everyday participation: Important outcomes for people with chronic conditions. Occup. Ther. 2011, 13, 8–10. [Google Scholar]
- Kim, Y.H.; Yoshikawa, E.; Yoshikawa, T.; Kogi, K.; Jung, M.H. Utility of action checklists as a consensus building tool. Ind. Health 2015, 53, 85–94. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Baydur, H.; Ergör, A.; Demiral, Y.; Akalı, E. Effects of participatory ergonomic intervention on the development of upper extremity musculoskeletal disorders and disability in office employees using a computer. J. Occup. Health 2016, 58, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.; Kim, S.L.; Jung, H.S.; Koo, J.W.; Woo, K.H.; Kim, M.Y. Participatory action oriented training for hospital nurses (PAOTHN) program to prevent musculoskeletal disorders. J. Occup. Health 2009, 51, 370–376. [Google Scholar] [CrossRef]
- Tsutsumi, A.; Nagami, M.; Yoshikawa, T.; Kogi, K.; Kawakami, N. Participatory intervention for workplace improvements on mental health and job performance among blue-collar workers: A cluster randomized controlled trial. J. Occup. Environ. Med. 2009, 51, 554–563. [Google Scholar] [CrossRef]
- Yoshikawa, T.; Kidouchi, K.; Kimura, S.; Okubo, T.; Perry, J.; Jagger, J. Needlestick injuries to the feet of Japanese healthcare workers: A culture-specific exposure risk. Infect. Control Hosp. Epidemiol. 2007, 2, 215–218. [Google Scholar] [CrossRef]
- Lee, J.; Kam, S.; Yoon, S. Effectiveness of participatory action-oriented training (PAOT) methods for the management metabolic syndrome in Korean manufacture workers for three-years. Korean J. Occup. Health Nurs. 2016, 25, 384–393. [Google Scholar] [CrossRef][Green Version]
- Yoon, S.Y.; Woo, K.H.; Kim, H.S.; Kim, Y.B.; Kim, J.S.; Jo, S.Y.; Lee, S.S. The Effect of Metabolic syndrome management program applying participatory action-oriented training principle. Korean J. Health Educ. Promot. 2014, 12, 81–95. [Google Scholar] [CrossRef]
- Yoon, S.Y.; Kam, S.; Kim, J.S.; Jo, S.Y.; Kwon, Y.J.; Song, I.W.; Woo, K.H. The effect of participatory approach program for cardiovascular disease prevention in the workplace. Korean J. Occup. Environ. Med. 2012, 24, 133–144. [Google Scholar] [CrossRef]
- National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef] [PubMed]
- Korea Occupational Safety and Health Agency. GUIDElines for Assessment and Management of Cardiovascular Disease Risk at Workplace;Report No.: KOSHA GUIDE H-1-2010; Korea Occupational Safety and Health Agency: 2010; pp. 1–16. (In Korean). Available online: https://www.kosha.or.kr/kosha/data/guidanceH.do (accessed on 28 December 2021).
- Kim, J.S.; Yoon, S.Y.; Cho, S.Y.; Kim, S.K.; Chung, I.S.; Shin, H.S. Effectiveness of participatory training for the promotion of work-related health and safety among Korean farmers. Ind. Health 2017, 55, 391–401. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maruyama, C.; Kimura, C.; Okumura, H.; Hayashi, K.; Arao, T. Effect of a worksite-based intervention program on metabolic parameters in middle-aged male white-collar workers: A randomized controlled trial. Prev. Med. 2010, 51, 11–17. [Google Scholar] [CrossRef]
- Gupta, N.; Wahlin-Jacobsen, C.D.; Henriksen, L.N.; Abildgaard, J.S.; Nielsen, K.; Holtermann, A. A participatory physical and psychosocial intervention for balancing the demands and resources among industrial workers (PIPPI): Study protocol of a cluster-randomized controlled trial. BMC Public Health 2015, 15, 274. [Google Scholar] [CrossRef] [PubMed]
- Balkau, B.; Picard, P.; Vol, S.; Fezeu, L.; Eschwège, E. Consequences of Change in Waist Circumference on Cardiometabolic Risk Factors Over 9 Years. Diabetes Care 2017, 30, 1901–1903. [Google Scholar] [CrossRef] [PubMed]
| 1. Hypertension management |
| 1-1. Self-measure and record blood pressure three times a weak |
| 1-2. Get out of bed slowly and try to relax before going to work |
| 1-3. Use a cart for heavy lifting and avoid maintaining the same working posture for a long time |
| 1-4. Avoid long-distance driving to prevent blood pressure increase |
| 1-5. Quit smoking and reduce alcohol drinking to prevent blood pressure increase |
| 1-6. Avoid overeating and heavy drinking to maintain a normal weight and waist circumference |
| 1-7. Maintain sleeping time more than 6 h per day |
| 1-8. Decrease physical and mental stress by stretching and bathing frequently to lower blood pressure |
| 1-9. Drink more than 1.5 L of water per day to prevent an elevated blood concentration |
| 1-10. Obtain regular checks for lipid and sugar blood levels and ophthalmic examinations |
| 2. Dyslipidemia management |
| 2-1. Know and maintain lipid levels in the normal range |
| 2-2. Cut fat off and eat only lean meat |
| 2-3. Avoid eating fried food and oily soup |
| 2-4. Reduce intake of processed products, convenient food, and junk food |
| 2-5. Eat food with unsaturated fatty acids and fiber (nuts, fish filled with omega-3, fruits, vegetables) |
| 2-6. Exercise for at least 30 min, three times a week to lower LDL cholesterol |
| 3. Diabetes management |
| 3-1. Monitor and maintain glucose levels in the normal range |
| 3-2. Check and record glucose level at least three times a week |
| 3-3. Eat a diet appropriate for diabetes |
| 3-4. Exercise for at least 30 min, three times a week to maintain glucose levels |
| 3-5. Undergo an ophthalmic examination and renal function test annually |
| 4. Alcohol drinking management |
| 4-1. Avoid keeping any liquor at home or at store |
| 4-2. Make your intentions known that you are not willing to drink alcohol |
| 4-3. Do not drink alcohol two days in a row or past your limit |
| 4-4. Drink after eating; do not drink alcohol on an empty stomach |
| 4-5. Drink less and more slowly by filling glasses half-full |
| 4-6. Drink water before, during, and after consuming alcohol to prevent dehydration |
| 4-7. Drink alcohol in a good mood; do not turn to alcohol after a stressful event |
| 4-8. Eat vegetables, low-sodium, and protein-rich foods; avoid fried, oily, salted, and spicy food while consuming alcohol |
| 5. Smoking habits management |
| 5-1. Make people know that you have quit smoking; try not to meet people for dinner as doing so can break the nonsmoking habit |
| 5-2. Throw away your cigarettes, cigarette lighters, and ashtrays |
| 5-3. Make a list of your personal reasons for quitting and display it prominently |
| 5-4. Wear a quit smoking badge so that everyone knows your intentions |
| 5-5. Motivate each other to quit smoking |
| 5-6. Practice refusal skills in case peers offer you a cigarette |
| 5-7. Use sugar-free gum or candy, breath mints, nuts etc., as a substitute for cigarettes |
| 5-8. Brush teeth and perform aerobic exercise right after eating a meal to resist the temptation to smoke |
| 5-9. Engage in a hobby or activity that you enjoy so that you can deal with stress |
| 5-10. Write out a list of good symptoms after quitting and display it prominently |
| 6. Exercise management |
| 6-1. Avoid prolonged postures and stretch every hour to improve impeded blood flow and stasis in veins |
| 6-2. Stretching should be carried out more often to get into the habit of doing it |
| 6-3. Sit and walk with a straight-spine posture to improve blood flow and burn calories |
| 6-4. Add movement to your daily life to improve blood flow and excrete metabolic waste |
| 6-5. Engage in at least 30 min of aerobic exercise and weight training three times a week to improve blood flow |
| 6-6. Perform light regular exercise every day, including dumbbells, yoga, Pilates, etc. |
| 6-7. Make people know that you are dieting and weigh yourself regularly |
| 7. Diet management |
| 7-1. Eat your vegetables first and avoid spicy and salted food |
| 7-2. Eat regular breakfast slowly and with less food |
| 7-3. Eat more fresh food and eat less processed, instant, fried, or salted food |
| 7-4. Avoid adding extra salt into food and try not to eat salty stews |
| 7-5. Eat fresh fruits and vegetables, take vitamin supplements, and avoid high-calorie food with large amounts of animal fats and oils |
| 7-6. Brush one’s teeth after a meal and take an after-meal walk |
| 7-7. Drink more than 1.5 L of water per day and avoid coffee, soda, and drinks added with artificial flavors |
| 7-8. Eat brown or multigrain rice to slow down digestion and metabolism |
| 8. Stress management |
| 8-1. Identify moments when you are under stress and improve your ability to cope |
| 8-2. Actively engage in a conversation and socializing with other merchants |
| 8-3. Have conversations with those with a relaxed and positive mind |
| 8-4. Have a big laugh for more than 10 s, three times a week |
| 8-5. Relax your body and psychological tension for a while every day. |
| 8-6. Release psychological tension by trying a life transition method or walking |
| 8-7. Release body tension by taking a bath, having a deep sleep, and drinking enough water |
| 8-8. Find ways to relieve your stress such as playing a sport, developing a hobby, or leading a religious life that can help you deal with your stress better |
| Variables | n (%), Mean ± SD | |
|---|---|---|
| Gender | Male | 21 (30.2) |
| Female | 49 (69.8) | |
| Age | 40–49 | 12 (17.1) |
| 50–59 | 28 (40.0) | |
| ≥60 | 30 (42.9) | |
| 60.15 ± 8.51 | ||
| Working time (hr) | <10 | 3 (5.1) |
| ≥10 | 67 (94.9) | |
| smoking | yes | 23 (32.5) |
| no | 47 (67.5) | |
| Drinking alcohol (days/week) | None | 47 (67.1) |
| 1–2 | 15 (21.4) | |
| ≥3 | 8 (11.4) | |
| Stress | Yes | 61 (87.2) |
| No | 9 (12.8) | |
| Occupation-related musculoskeletal pain | Yes | 38 (54.2) |
| No | 32 (45.8) |
| Variables | 1st Year | 2nd Year | 3rd Year |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Proposed action plans | 296 | 281 | 246 |
| Implemented action plans after 3 months | 245 (82.7) | 244 (86.8) | 190 (77.2) |
| Implemented action plans after 6 months | 182 (61.4) | 162 (57.6) | 131 (53.2) |
| MetS Components | B | 2014 | 2015 | 2016 | B–2014 | B–2015 | B–2016 | 2014–2015 | 2014–2016 | 2015–2016 | F/χ2 | p |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M ± SD | M ± SD | M ± SD | M ± SD | p | p | p | p | p | p | |||
| WC (cm) | 82.97 ± 8.20 | 82.67 ± 8.31 | 81.15 ± 8.76 | 83.17 ± 7.64 | 0.617 | 0.009 | 0.753 | 0.016 | 0.402 | 0.006 | 4.44 | 0.005 |
| SBP (mmHg) * | 125.33 ± 14.69 | 126.84 ± 16.47 | 128.91 ± 15.69 | 128.52 ± 13.96 | 0.375 | 0.022 | 0.038 | 0.418 | 0.408 | 0.937 | 4.90 | 0.179 |
| DBP (mmHg) * | 76.78 ± 7.69 | 77.64 ± 10.20 | 79.01 ± 9.67 | 77.00 ± 8.70 | 0.475 | 0.083 | 0.713 | 0.347 | 0.517 | 0.120 | 3.40 | 0.334 |
| FBS (mg/dL) * | 100.11 ± 24.03 | 99.70 ± 19.88 | 95.02 ± 18.14 | 94.75 ± 19.36 | 0.600 | 0.033 | 0.005 | 0.006 | <0.001 | 0.380 | 18.52 | <0.001 |
| TGL (mg/dL) * | 167.98 ± 114.33 | 167.90 ± 126.77 | 150.31 ± 128.57 | 150.15 ± 191.22 | 0.452 | 0.021 | 0.009 | 0.074 | 0.008 | 0.468 | 11.68 | 0.009 |
| HDL-C(mg/dL) * | 47.22 ± 10.82 | 48.32 ± 12.70 | 46.92 ± 11.13 | 47.18 ± 11.68 | 0.230 | 0.617 | 0.858 | 0.072 | 0.136 | 0.622 | 4.39 | 0.222 |
| Score of MetS * | 2.12 ± 1.41 | 2.07 ± 1.31 | 2.02 ± 1.28 | 1.50 ± 1.11 | 0.645 | 0.541 | <0.001 | 0.856 | 0.001 | 0.001 | 17.73 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.-H.; Yoon, S.-Y. Effects of a Worksite-Based Self-Management Program in Traditional Retail Market Workers: Longitudinal Associations with Metabolic Parameters. Int. J. Environ. Res. Public Health 2022, 19, 2854. https://doi.org/10.3390/ijerph19052854
Kim Y-H, Yoon S-Y. Effects of a Worksite-Based Self-Management Program in Traditional Retail Market Workers: Longitudinal Associations with Metabolic Parameters. International Journal of Environmental Research and Public Health. 2022; 19(5):2854. https://doi.org/10.3390/ijerph19052854
Chicago/Turabian StyleKim, Yeon-Ha, and Seong-Yong Yoon. 2022. "Effects of a Worksite-Based Self-Management Program in Traditional Retail Market Workers: Longitudinal Associations with Metabolic Parameters" International Journal of Environmental Research and Public Health 19, no. 5: 2854. https://doi.org/10.3390/ijerph19052854
APA StyleKim, Y.-H., & Yoon, S.-Y. (2022). Effects of a Worksite-Based Self-Management Program in Traditional Retail Market Workers: Longitudinal Associations with Metabolic Parameters. International Journal of Environmental Research and Public Health, 19(5), 2854. https://doi.org/10.3390/ijerph19052854






